Abstract
Background
Family with sequence similarity 19 (chemokine (C-C motif)-like) member A5 (FAM19A5) is a newly identified adipokine. There is a limited number of studies linking FAM19A5 to metabolic disorders. In the current study, we aimed to explore if FAM19A5 is associated with nonalcoholic fatty liver disease (NAFLD). We also sought to determine the possibility of FAM19A5 association with subclinical atherosclerosis in NAFLD patients.
Methods
A total of 69 subjects including 37 NAFLD and 32 control subjects were included in this cross-sectional study. Plasma concentration of FAM19A5 was measured with the ELISA method. Carotid artery intima-media thickness (cIMT) was assessed by the ultrasonography.
Results
Plasma concentration of FAM19A5 in patients with NAFLD was significantly lower in NAFLD patients than controls. Moreover, we observed significant negative correlations between plasma level of FAM19A5 and body mass index (BMI), visceral fat, alanine amino transferase (ALT), aspartate amino transferase (AST), liver stiffness (LS), and cIMT. Following stepwise multiple linear regression analysis, ALT and cIMT were the only determinants of FAM19A5 level.
Conclusions
This is the first report to describe association of circulating FAM19A5 levels with NAFLD. Our findings provide further evidence showing relation of FAM19A5 with the risk of atherosclerosis. However, more studies are necessary to unravel the contribution of lower FAM19A5 levels to the NAFLD pathogenesis and the higher risk of atherosclerosis in these patients.
Similar content being viewed by others
Background
Non-alcoholic fatty liver disease (NAFLD) is the most common chronic liver disease with the prevalence of 25% in the general population [1]. NAFLD is closely associated with obesity and is regarded as the hepatic component of metabolic syndrome [2]. As one of the largest endocrine organs in the body, adipose tissue secrets a host of bioactive molecules, called adipokines [3]. Adipokines possess a wide spectrum of metabolic effects in the physiological and pathological processes [3]. Previous studies have reported the important roles of adipokines in the pathogenesis of NAFLD [4,5,6,7].
Family with sequence similarity 19 (chemokine (C-C motif)-like) member A5 (FAM19A5) belongs to a family with sequence similarity 19, which is composed of 5 highly homologous genes (FAM19A1–5). FAM19A5 is a secretory protein which is predominantly expressed in the brain and adipose tissues. It is first identified as an adipokine by Wang et al. [8]. They studied FAM19A5 expression in the epididymal adipose tissues of high-fat diet-induced obese and leptin receptor-deficient (db/db) mice. They observed reduced expression of FAM19A5 expression of the epididymal adipose tissues of obese mice [8]. In a recent clinical study, it has been indicated that circulating level of FAM19A5 is different in diabetic patients compared to controls. They also found association of FAM19A5 with the obesity and diabetes indicators [9].
Growing epidemiological evidence demonstrates association of NAFLD with subclinical atherosclerosis and increased prevalence of cardiovascular diseases [10,11,12]. Subclinical atherosclerosis is an early indicator of atherosclerotic risk which can predict future cardiovascular events. Subclinical atherosclerosis can be conveniently measured by carotid intima-media thickness (CIMT) [13,14,15]. Now NAFLD is considered as a potential independent risk factor for cardiovascular diseases [16]. Several studies reported greater carotid artery intimal medial thickness in ultrasound- diagnosed NAFLD patients [17,18,19,20]. Moreover, it has been revealed that adipokines contribute to the cardiovascular homeostasis which affects vessel remodeling [21]. Wang et al. showed FAM19A5 inhibits the vascular smooth muscle cells proliferation and ameliorates neointima formation in the injured rat carotid arteries [8]. Although several studies addressed contribution of FAM19A5 to neurological disorders [22,23,24,25,26], existing data on a relevant association of FAM19A5 and cardiac and metabolic disorders are very limited [8, 9]. To our knowledge, this is the first clinical observation pointing to the association of FAM19A5 with the pathogenesis of NAFLD.
The aim of this study was to compare the circulating levels of FAM19A5 in patients with NAFLD and controls and to investigate a potential association of FAM19A5 with fatty liver and atherosclerosis indices.
Methods
Study design and participants
A total of 69 subjects including 37 NAFLD and 32 control subjects were selected from Golestan Cohort Study [27]. This study was approved by the medical ethics committee of Semnan University of Medical Sciences, and the written informed consent was obtained from all participants according to the guidelines of Declaration of Helsinki. The diagnosis of NAFLD was established using ultasonography and fibroscan. All participants were male, aged 50–81 years old. The subjects were excluded if they had excessive alcohol consumption (> 30 g/d), diabetes, viral hepatitis, autoimmune liver disease, hemochromatosis, Wilson’s disease. None of the patients were taking medication that has been reported to cause steatosis.
Anthropometric and laboratory evaluation
Anthropometric parameters including age, height, weight, blood pressure (BP), waist circumference (WC) were measured in accordance with the standardized protocols. Body mass index (BMI) was calculated as body weight (kg) divided by the square of height (m2). WC was measured at the midpoint between the lowest rib and the iliac crest.
Plasma samples were collected from participants following an overnight fasting and stored at − 80 °C until analysis. Fasting blood glucose (FBG), serum total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and levels of alanine amino transferase (ALT), aspartate amino transferase (AST), gamma glutamyl transferase (GGT) were determined by automated enzymatic methods and commercial kits (Pars Azmoon, Iran).
Circulating level of FAM19A5 was measured with an enzyme linked immunosorbent assay (ELISA) with a minimum detectable concentration of 15 pg/ml, Intra assay CV of < 10% and Inter assay CV of < 12% (RayBiotech Inc., USA).
Ultrasonography and elastography
Ultrasound assessment was performed using Accuvix XQ ultrasound unit (Medison, South Korea) equipped with a 3–7 MHz curved-array and a 5–12 MHz linear-array transducer for the evaluation of liver, abdominal fat and carotid arteries as previously described [27]. Ultrasonographic scoring was used to determine fatty liver with specificity of 100% and sensitivity of 91.7%. In this protocol, ultrasonography results included vascular blurring (score 0 to 1), hepatorenal echo contrast and/or liver brightness (score 0 to 3) and deep attenuation (score 0 to 2). A total score of at least 2 was needed for the diagnosis of NAFLD [27].
Visceral Adipose Tissue thickness (VAT) was measured between the anterior wall of the aorta and the internal face of the rectus abdominis muscle perpendicular to the aorta. Ultrasonographic measurements have been shown to have strong correlations with the visceral fat area measured by the computed tomography [27].
Carotid Intima-Media Thickness (cIMT) was assessed as the distance between the lumen–intima interface and the media– adventitia interface, measured at its thickest point on the distal (far) wall of the common carotid arteries, 1.5–2 cm proximal to the carotid bulb. The average of right and left sides was used for cIMT analysis [27].
LS was measured by transient elastography using the FibroScan 502 machine (EchoSense, Paris, France, 5 MHz). According to the manufacturer’s guidelines the M probe was used for the subjects with thoracic perimeter less than 110 cm and the XL probe for 110 cm and above. At least 10 measurements were done for each patient and the median value was recorded. Values were considered valid if the inter-quartile range (IQR) was less than 30% of the median reading [27].
Statistical analyses
The sample size was calculated based on data from a previous study about circulating levels of FAM19A5 in the subjects with and without diabetes [9]. We calculated that 32 subjects in each group would provide 90% power to achieve a difference of 80% in the circulating levels of FAM19A5 between the studied groups assuming a 2-sided t-test with alpha of 0.05.
The Shapiro-Wilk test was applied to test the normal distribution of values. Non-pairwise comparisons of the concentrations of normally and non-normally distributed variables were performed between the two groups with the students t test and nonparametric Mann–Whitney test respectively. Binary logistic regression models were calculated to identify independent risk factors. Associations between the concentrations of FAM19A5 and other variables of interest were tested with the use of Pearson correlation coefficients after appropriate log-normalizations of the concentration values. Additionally, multivariate linear regressions with the stepwise variable selection were used to test for significant relations in continuous data with adjustment for possible confounders. We used two-tailed hypothesis tests and P-values < 0.05 were considered significant.
Results
The clinical and biochemical characteristics of the study subjects were summarized in Table 1. There were no significant differences between the two groups in terms of age. In the NAFLD group, BMI, waist circumference, FBG, TG, GFR, ALT, AST, GGT and LS were significantly higher than the control group. Whereas HDL-C, LDL-C, TC, creatinine, urea and cIMT were comparable in two groups.
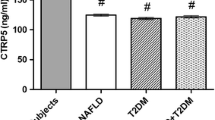
The plasma FAM19A5 concentration was significantly lower in NAFLD group compared to control group (Fig. 1).
Associations between FAM19A5 plasma levels and presence of NAFLD were assessed using binary logistic regression. FAM19A5 appeared to be negatively associated with presence of NAFLD (P = 0.019). This association remained significant after adjustment for age (P = 0.019). It disappeared after adjustment for BMI (P = 0.062). But the association of FAM19A5 with NAFLD remained significant after adjustment for the visceral fat (P = 0.025) (Table 2).
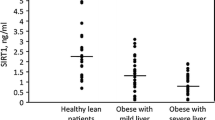
The associations between circulating FAM19A5 levels and clinical and biochemical variables were assessed and the data are summarized in Table 2. Plasma FAM19A5 level showed a significant negative correlation with serum levels of liver enzymes including ALT (r = − 0.355, P = 0.004) and AST (r = − 0.254, P = 0.043) and a significant positive correlation with HDL-C (r = 0.281, P = 0.025). There was also significant negative correlation between plasma level of FAM19A5 and liver stiffness (LS) (r = − 0.294, P = 0.021). Furthermore, significant negative correlations were found between FAM19A5 levels and BMI (r = − 0.285, P = 0.024) as well as FAM19A5 and visceral fat (r = − 0.317, P = 0.011). (Table 3). There was also a significant negative correlation between cIMT and FAM19A5 (r = − 0.268, P = 0.037) (Fig. 2).
Stepwise multiple linear regression analysis was performed to determine whether obesity (BMI, visceral fat), fatty liver (ALT, AST, LS) and atherosclerosis (cIMT) indices influenced FAM19A5 levels. ALT (P = 0.003) and cIMT (P = 0.024) were found to be the only significant determinants of FAM19A5 levels with the model explaining 20% of the variance in levels of FAM19A5 (log FAM19A5 = 2.887–0.679[log ALT]- 1.539 [log cIMT]) (Table 3).
Discussion
In the current study, we found lower circulating FAM19A5 concentrations in NAFLD group compared to the control group, suggesting a role of this adipokine in NAFLD risk. To our knowledge, this is the first study ever to report the association of FAM19A5 circulating level with NAFLD.
Several studies have shown association of FAM19A5 gene with neurological and/or psychiatric diseases [22,23,24,25, 28, 29]. FAM19A5 has been linked to inflammation, differentiation and cognition [22, 24, 26, 29, 30]. But few studies have addressed the role of FAM19A5 in cardiometabolic disorders. Recently, Wang et al. identified FAM19A5 as a new secretory protein which is highly expressed in adipose tissue [8]. Having analyzed the expression of FAM19A5 in multiple human tissues, they observed FAM19A4 expressed in the adipose tissue even more than the brain [8]. They compared FAM19A5 expression in the epididymal adipose tissues of non-obese and obese mice and found reduced expression of FAM19A5 in both high-fat diet-induced obese and leptin receptor- deficient (db/db) mice compared to the non-obese ones [8]. These results are in agreement with our findings which showed lower circulating levels of FAM19A5 in NAFLD. Moreover, an in vitro study showed that TNF-α-induced inflammation in adipocytes decreased expression of FAM19A5 suggesting that a pro-inflammatory condition as it observed in NAFLD might cause downregulation of FAM19A5 [31, 32]. However, Lee et al. reported higher serum levels of FAM19A5 in diabetic patients compared to non-diabetic subjects [9]. Due to the previously reported protective roles of FAM19A5 in atherosclerosis, obesity and inflammation, we assume that lower levels of FAM19A5 in our study might suggest its protective role in the NAFLD pathogenesis [8, 31, 32]. The clinical relevance of this hypothesis is indirectly supported by the other studies showed decreased levels of other protective adipokines in the NAFLD patients [4, 6, 33]. However, we cannot rule out the possible influence of the race-ethnic difference between study populations. A previous study showed significant race-ethnic differences in circulating levels of other adipokines [34].
In the present study, circulating levels of FAM19A5 was negatively correlated with BMI and the visceral adipose tissue. This finding is in good agreement with the results from Wong et al. which showed negative correlation between FAM19A5 mRNA level of the epididymal adipose tissue and body weights in mice [8]. After adjusting for BMI, logistic regression analysis revealed a borderline significant relationship between FAM19A5 and NAFLD. Moreover, after adjusting for the visceral fat, the association of FAM19A5 with NAFLD remined significant. So, although adiposity is an important confounder when considering the interaction between adipokines and NAFLD, it does not seem to attenuate the relationship between FAM19A5 and NAFLD remarkably. Our findings showed negative correlations between FAM19A5 and fatty liver indices including ALT, AST, and LS.
We have also observed a negative correlation between FAM19A5 and cIMT. In line, previous studies have indicated association of other adipokines with cIMT in NAFLD patients [17, 33]. Moreover, several basic and pre-clinical studies demonstrated the vasculoprotective effects of adiponectin in atherosclerotic models. Atherosclerosis is characterized by neointima formation. One of the major processes occurs in the neointima formation is the proliferation and migration of vascular smooth muscle cells into the intimal layer of the artery. Wang et al. consistently showed adipose derived FAM19A5 inhibited vascular smooth muscle cell proliferation [8]. To study the effect of FAM19A5 on neointima formation in the injured arteries in rats, they overexpressed FAM19A5 in balloon-injured carotid arteries and observed neointima formation was significantly repressed in the FAM19A5 overexpressed vessels [8]. In the current study, when we conducted a stepwise regression analysis to identify parameters that were related to FAM19A5 levels, ALT and cIMT were found to be the parameters were associated significantly with circulating levels of FAM19A5 after controlling for BMI and the visceral fat.
Our study has some limitations. Due to the cross-sectional design of our study, clarification of the causality between FAM19A5 and other parameters was inherently limited. The sample size was relatively small, and further studies with larger sample size are needed to confirm our results. Our study population included only men. Previous studies reported gender differences in circulating levels of adipokines [35, 36]. Although our findings cannot be generalized to the whole population, the confounding effect of sex has been eliminated.
Conclusions
Here, we demonstrated that the circulating level of FAM19A5 is associated with NAFLD. We also showed a significant and independent correlation between FAM19A5 and cIMT. Our data suggest a protective role of FAM19A5 in NAFLD and subclinical atherosclerosis in patients with NAFLD who have characteristics of high CVD risk. Longitudinal studies are also required to confirm whether lower plasma FAM19A5 levels can potentiate the NAFLD patients to atherosclerosis.
Availability of data and materials
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- NAFLD:
-
Nonalcoholic fatty liver disease
- CIMT:
-
Carotid artery intima-media thickness
- BMI:
-
Body mass index
- ALT:
-
Alanine amino transferase
- AST:
-
Aspartate amino transferase
- LS:
-
Liver stiffness
- FAM19A5:
-
Family with sequence similarity 19 (chemokine (C-C motif)-like) member A5
- FBG:
-
Fasting blood glucose
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- HDLC:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- GGT:
-
Gamma glutamyl transferase
References
Iqbal U, Perumpail BJ, Akhtar D, Kim D, Ahmed A. The Epidemiology, Risk Profiling and Diagnostic Challenges of Nonalcoholic Fatty Liver Disease. Medicines. 2019;6(1).
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. https://doi.org/10.1002/hep.28431.
Ragino YI, Stakhneva EM, Polonskaya YV, Kashtanova EV. The role of secretory activity molecules of visceral adipocytes in abdominal obesity in the development of cardiovascular disease: a review. Biomolecules. 2020;10(3).
Shabani P, Naeimi Khaledi H, Beigy M, Emamgholipour S, Parvaz E, Poustchi H, et al. Circulating level of CTRP1 in patients with nonalcoholic fatty liver disease (NAFLD): is it through insulin resistance? PLoS One. 2015;10(3):e0118650. https://doi.org/10.1371/journal.pone.0118650.
Shanaki M, Fadaei R, Moradi N, Emamgholipour S, Poustchi H. The circulating CTRP13 in type 2 diabetes and non-alcoholic fatty liver patients. PLoS One. 2016;11(12):e0168082. https://doi.org/10.1371/journal.pone.0168082.
Shanaki M, Moradi N, Emamgholipour S, Fadaei R, Poustchi H. Lower circulating irisin is associated with nonalcoholic fatty liver disease and type 2 diabetes. Diabetes Metab Syndr. 2017;11(Suppl 1):S467–S72. https://doi.org/10.1016/j.dsx.2017.03.037.
Emamgholipour S, Moradi N, Beigy M, Shabani P, Fadaei R, Poustchi H, et al. The association of circulating levels of complement-C1q TNF-related protein 5 (CTRP5) with nonalcoholic fatty liver disease and type 2 diabetes: a case-control study. Diabetol Metab Syndr. 2015;7(1):108. https://doi.org/10.1186/s13098-015-0099-z.
Wang Y, Chen D, Zhang Y, Wang P, Zheng C, Zhang S, et al. Novel Adipokine, FAM19A5, inhibits Neointima formation after injury through Sphingosine-1-phosphate receptor 2. Circulation. 2018;138(1):48–63. https://doi.org/10.1161/CIRCULATIONAHA.117.032398.
Lee YB, Hwang HJ, Kim JA, Hwang SY, Roh E, Hong SH, et al. Association of serum FAM19A5 with metabolic and vascular risk factors in human subjects with or without type 2 diabetes. Diab Vasc Dis Res. 2019;16(6):530–8. https://doi.org/10.1177/1479164119860746.
Al Rifai M, Silverman MG, Nasir K, Budoff MJ, Blankstein R, Szklo M, et al. The association of nonalcoholic fatty liver disease, obesity, and metabolic syndrome, with systemic inflammation and subclinical atherosclerosis: the multi-ethnic study of atherosclerosis (MESA). Atherosclerosis. 2015;239(2):629–33. https://doi.org/10.1016/j.atherosclerosis.2015.02.011.
Zheng J, Zhou Y, Zhang K, Qi Y, An S, Wang S, et al. Association between nonalcoholic fatty liver disease and subclinical atherosclerosis: a cross-sectional study on population over 40 years old. BMC Cardiovasc Disord. 2018;18(1):147. https://doi.org/10.1186/s12872-018-0877-2.
Adams LA, Anstee QM, Tilg H, Targher G. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut. 2017;66(6):1138–53. https://doi.org/10.1136/gutjnl-2017-313884.
Ahmadi A, Argulian E, Leipsic J, Newby DE, Narula J. From subclinical atherosclerosis to plaque progression and acute coronary events: JACC state-of-the-art review. J Am Coll Cardiol. 2019;74(12):1608–17. https://doi.org/10.1016/j.jacc.2019.08.012.
Gatto L, Prati F. Subclinical atherosclerosis: how and when to treat it? Eur Heart J Suppl. 2020;22(Suppl E):E87–e90.
Singh SS, Pilkerton CS, Shrader CD Jr, Frisbee SJ. Subclinical atherosclerosis, cardiovascular health, and disease risk: is there a case for the cardiovascular health index in the primary prevention population? BMC Public Health. 2018;18(1):429. https://doi.org/10.1186/s12889-018-5263-6.
Patil R, Sood GK. Non-alcoholic fatty liver disease and cardiovascular risk. World J Gastrointest Pathophysiol. 2017;8(2):51–8. https://doi.org/10.4291/wjgp.v8.i2.51.
Fadaei R, Meshkani R, Poustchi H, Fallah S, Moradi N, Panahi G, et al. Association of carotid intima media thickness with atherogenic index of plasma, apo B/apo A-I ratio and paraoxonase activity in patients with non-alcoholic fatty liver disease. Arch Physiol Biochem. 2019;125(1):19–24. https://doi.org/10.1080/13813455.2018.1429475.
Kozakova M, Palombo C, Eng MP, Dekker J, Flyvbjerg A, Mitrakou A, et al. Fatty liver index, gamma-glutamyltransferase, and early carotid plaques. Hepatology. 2012;55(5):1406–15. https://doi.org/10.1002/hep.25555.
Targher G, Bertolini L, Padovani R, Zenari L, Zoppini G, Falezza G. Relation of nonalcoholic hepatic steatosis to early carotid atherosclerosis in healthy men: role of visceral fat accumulation. Diabetes Care. 2004;27(10):2498–500. https://doi.org/10.2337/diacare.27.10.2498.
Volzke H, Robinson DM, Kleine V, Deutscher R, Hoffmann W, Ludemann J, et al. Hepatic steatosis is associated with an increased risk of carotid atherosclerosis. World J Gastroenterol. 2005;11(12):1848–53. https://doi.org/10.3748/wjg.v11.i12.1848.
Maenhaut N, Van de Voorde J. Regulation of vascular tone by adipocytes. BMC Med. 2011;9:25.
Han KM, Tae WS, Kim A, Kang Y, Kang W, Kang J, et al. Serum FAM19A5 levels: A novel biomarker for neuroinflammation and neurodegeneration in major depressive disorder. Brain Behav Immun. 2020;87:852–9. https://doi.org/10.1016/j.bbi.2020.03.021.
Huang S, Zheng C, Xie G, Song Z, Wang P, Bai Y, et al. FAM19A5/TAFA5, a novel neurokine, plays a crucial role in depressive-like and spatial memory-related behaviors in mice. Mol Psychiatry. 2020. https://doi.org/10.1038/s41380-020-0720-x.
Kang D, Kim HR, Kim KK, Kim DH, Jeong B, Jin S, et al. Brain-specific chemokine FAM19A5 induces hypothalamic inflammation. Biochem Biophys Res Commun. 2020;523(4):829–34. https://doi.org/10.1016/j.bbrc.2019.12.119.
Lee HL, Seok HY, Ryu HW, Cho EB, Kim BC, Kim BJ, et al. Serum FAM19A5 in neuromyelitis optica spectrum disorders: can it be a new biomarker representing clinical status? Mult Scler. 2019;1352458519885489.
Park MY, Kim HS, Lee M, Park B, Lee HY, Cho EB, et al. FAM19A5, a brain-specific chemokine, inhibits RANKL-induced osteoclast formation through formyl peptide receptor 2. Sci Rep. 2017;7(1):15575. https://doi.org/10.1038/s41598-017-15586-0.
Merat S, Poustchi H, Hemming K, Jafari E, Radmard AR, Nateghi A, et al. PolyPill for prevention of cardiovascular disease in an urban Iranian population with special focus on nonalcoholic Steatohepatitis: a pragmatic randomized controlled trial within a cohort (PolyIran - liver) - study protocol. Arch Iran Med. 2015;18(8):515–23.
Inan C, Sayin NC, Gurkan H, Atli E, Gursoy Erzincan S, Uzun I, et al. Schizencephaly accompanied by occipital encephalocele and deletion of chromosome 22q13.32: a case report. Fetal Pediatr Pathol. 2019;38(6):496–502. https://doi.org/10.1080/15513815.2019.1604921.
Shahapal A, Cho EB, Yong HJ, Jeong I, Kwak H, Lee JK, et al. FAM19A5 expression during embryogenesis and in the adult traumatic brain of FAM19A5-LacZ Knock-in mice. Front Neurosci. 2019;13:917. https://doi.org/10.3389/fnins.2019.00917.
Pan X, Karner CM, Carroll TJ. Myc cooperates with beta-catenin to drive gene expression in nephron progenitor cells. Development. 2017;144(22):4173–82. https://doi.org/10.1242/dev.153700.
Recinella L, Orlando G, Ferrante C, Chiavaroli A, Brunetti L, Leone S. Adipokines: new potential therapeutic target for obesity and metabolic, rheumatic, and cardiovascular diseases. Front Physiol. 2020;11:578966. https://doi.org/10.3389/fphys.2020.578966.
Tourniaire F, Romier-Crouzet B, Lee JH, Marcotorchino J, Gouranton E, Salles J, et al. Chemokine expression in inflamed adipose tissue is mainly mediated by NF-κB. PLoS One. 2013;8(6):e66515. https://doi.org/10.1371/journal.pone.0066515.
Ebrahimi R, Shanaki M, Mohassel Azadi S, Bahiraee A, Radmard AR, Poustchi H, et al. Low level of adiponectin predicts the development of nonalcoholic fatty liver disease: is it irrespective to visceral adiposity index, visceral adipose tissue thickness and other obesity indices? Arch Physiol Biochem. 2019:1–8. https://doi.org/10.1080/13813455.2019.1661496.
Khan UI, Wang D, Sowers MR, Mancuso P, Everson-Rose SA, Scherer PE, et al. Race-ethnic differences in adipokine levels: the study of Women's health across the nation (SWAN). Metabolism. 2012;61(9):1261–9. https://doi.org/10.1016/j.metabol.2012.02.005.
Bonakdari H, Tardif G, Abram F, Pelletier JP, Martel-Pelletier J. Serum adipokines/related inflammatory factors and ratios as predictors of infrapatellar fat pad volume in osteoarthritis: applying comprehensive machine learning approaches. Sci Rep. 2020;10(1):9993. https://doi.org/10.1038/s41598-020-66330-0.
Eglit T, Lember M, Ringmets I, Rajasalu T. Gender differences in serum high-molecular-weight adiponectin levels in metabolic syndrome. Eur J Endocrinol. 2013;168(3):385–91. https://doi.org/10.1530/EJE-12-0688.
Acknowledgments
The authors wish to thank the study participants, doctors, and co-researchers of Digestive Diseases Research Institute of Tehran University of Medical Sciences.
Funding
This work was supported by Semnan University of Medical Sciences and Digestive Diseases Research Institute of Tehran University of Medical Sciences. The funding bodies played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
ARB, HP designed, supervised the study and edited the manuscript. PS designed the study, analyzed the data and wrote the manuscript. FAY, SK and NS performed the experiments and collected the human subjects. All authors approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the medical ethics committee of Semnan University of Medical Sciences, and the written informed consent was obtained from all participants according to the guidelines of Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yari, F.A., Shabani, P., Karami, S. et al. Circulating levels of FAM19A5 are inversely associated with subclinical atherosclerosis in non-alcoholic fatty liver disease. BMC Endocr Disord 21, 153 (2021). https://doi.org/10.1186/s12902-021-00820-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-021-00820-8