Abstract
Introduction
Localized prostate cancer (PCa) is one of the most common malignancies in the United States. Despite continued refinement of robot assisted radical prostatectomy (RARP) surgical methods, post-surgical erectile dysfunction and urinary incontinence remain significant challenges due to iatrogenic injury of local nervous tissue. Thus, the development of therapeutic strategies, including the use of biologic adjuncts to protect and/or enhance recovery and function of nerves following RARP is of growing interest. Perinatal tissue allografts have been investigated as one such biologic adjunct to nerve sparing RARP. However, knowledge regarding their clinical efficacy in hastening return of potency and continence as well as the potential underpinning biological mechanisms involved remains understudied. Thus, the objective of this literature review was to summarize published basic science and clinical studies supporting and evaluating the use of perinatal allografts for nerve repair and their clinical efficacy as adjuncts to RARP, respectively.
Methods
The literature as of May 2024 was reviewed non-systematically using PubMed, EMBASE, Scopus, and Web of Science databases. The search terms utilized were “robotic prostatectomy”, “prostate cancer”, “nerve sparing”, “perinatal tissue”, “allograft”, “potency”, and “continence” alone or in combination. All articles were reviewed and judged for scientific merit by authors RP and JM, only peer-reviewed studies were considered.
Results
Eight studies of perinatal tissue allograph use in RARP were deemed worthy of inclusion in this nonsystematic review.
Conclusions
Incontinence and impotence remain significant comorbidities despite continued advancement in surgical technique. However, basic science research has demonstrated potential neurotrophic, anti-fibrotic, and anti-inflammatory properties of perinatal tissue allografts, and clinical studies have shown that patients who receive an intra-operative prostatic perinatal membrane wrap have faster return to potency and continence.
Similar content being viewed by others
Background
Clinical significance of prostate cancer
Prostate cancer (PCa) is one of the most common malignancies in the United States, with a lifetime incidence rate of one-in-nine men [1]. Additionally, 2.4% of all cancer deaths in men can be attributed to PCa-related conditions [1]. According to an estimate from the Surveillance, Epidemiology, and End Results (SEER) database, which includes patients aged 65 and older who are insured by Medicare, $22.4 billion dollars were spent on PCa healthcare in the US in 2020 [2].
Prostate cancer surgery
Robotic-assisted radical prostatectomy (RARP) first began in the 2000’s and demonstrated benefits compared to open prostatectomy, including decreased blood loss, transfusion rate, and length of stay [3]. However, despite the advances and advantages of RARP over its predecessors, long-term functional outcomes, specifically erectile function and urinary continence, have continued to be a common source of post-operative morbidity [4]. Erectile function is controlled by nerve bundles from the pelvic plexus, which run posterolateral to the prostate in a layer of fat and fascia potentially injured during prostatectomy [3]. Rates of erectile dysfunction one year post-RARP vary significantly between studies, but is estimated to be between 10 and 46%. [5] Urinary incontinence after prostatectomy is multifactorial: resecting the prostate also removes the internal urethral sphincter and iatrogenic injury damages nerves that control the external urethral sphincter [6]. Continence rates at one year post-RARP vary between 40 and 95% depending on how continence is defined: zero unwanted urine leak versus only one pad needed per day [7]. Using a patient-centered approach, studies have routinely demonstrated the negative effects of prostatectomy on quality of life [8]. Thus, there is significant motivation to improve erectile function and continence outcomes after RARP via the development of new therapeutic strategies. To develop such strategies to hasten return to sexual and urinary function following RARP, a basic understanding of the physiologic mechanisms underpinning erectile function, urinary continence and associated pathophysiology is warranted.
Physiology of erectile function and urinary incontinence
Erectile function is largely derived from proper conduction of nerve impulses from the cavernous nerves (CN). Nerve signals induce nitric oxide (NO) mediated arterial dilation and sub-tunica vein compression, resulting in tumescence [9, 10].
Urinary continence and micturition are controlled by sensory, parasympathetic, and sympathetic fibers from the hypogastric, pelvic, and pudendal nerves which travel adjacent to the prostate, urethra, and bladder [6, 11]. These nerves innervate the internal and external urethral sphincters to control urinary continence.
Mechanisms of erectile dysfunction and urinary incontinence associated with RARP
Due to the fragility of the nerves that control erections and continence, iatrogenic nerve injury is believed to be the primary contributing factor leading to erectile dysfunction following RARP [3]. Nerve injury is thought to be caused by surgical traction, thermal injury from electrocautery, inadvertent dissection or clamping of the nerves around the prostate, and ischemia due to hemostasis. Additionally, local inflammation due to the surgery itself may have detrimental implications on nerve function [12,13,14]. Ultimately, these injurious events can lead to neuropraxia and locally increased production of pro-inflammatory cytokines and reactive oxygen species [15]. With regards to erectile function, even the temporary loss of erections decreases NO production and release, which reduces blood flow and ultimately causes veno-occlusive and hypoxic changes [16, 17]. These changes are marked by apoptosis and fibrosis within the tissues of the corpus cavernosum [18, 19]. Studies have shown that resultant decreases in oxygen tension can be accompanied by biochemical changes in the penile tissue. For example, concentrations of oxygen-dependent prostaglandin E1 (PGE1) and E2 (PGE2) are reduced [10, 20]. Importantly, PGE’s are known suppressors of the pro-fibrotic growth factor transforming growth factor beta-1 (TGF-β1) [17, 21]. Consequently, TGF-β1-induced collagen synthesis and collagen content has been shown to increase concomitant with decreased cavernous smooth muscle cell content due to apoptosis [18]. Additionally, decreases in the number of nerve cells via apoptosis and their diminished staining for nitric oxide synthase has also been observed following CN injury [19]. Thus, even temporary erectile neuropraxia after RARP can result in permanent cavernosal fibrosis via the PGE and TGF-β1 pathways.
Post-prostatectomy incontinence is often due to a degree of both bladder and sphincter dysfunction [22]. However, urodynamic studies have demonstrated that sphincter deficiency appears to be the primary contributor to incontinence, as de novo bladder dysfunction (i.e. detrusor instability, decreased bladder compliance, detrusor over/under activity) following RARP is rarely the sole etiology [22, 23]. Sphincter dysfunction following RARP is believed to be due to local iatrogenic tissue injury of the sphincters and injury to the nerves that control their function. Although improved preservation of anatomic structures (including membranous urethral supporting structures, bladder neck preservation and maintenance of urethral length) has been achieved through innovations in surgical technique [22], removal of the prostate still damages the internal urethral sphincter, leaving the external urethral spinctor as the primary continence control point [6]. Additionally, the proximity of the neurovascular supply to the prostate and the complex plate-like structure of the neurovascular bundle in this location make it challenging to avoid neurogenic damage altogether [6, 24].
Taken together, iatrogenic injury to the nerves that control erectile function and continence are believed to be one of the primary contributors to de novo post prostatectomy erectile dysfunction and possibly incontinence. One major development in improving post-RARP functional outcomes is the advent of nerve sparing techniques, in which the periprostatic, interfascial nerve fibers are visually preserved during surgery [25]. The main benefit of nerve sparing RARP is improved potency and continence outcomes, although this conclusion is limited by the subjective nature of determining degree of nerve sparing [26, 27]. Not every patient is a candidate for nerve sparing surgery, as extraprostatic extension or high-risk disease increases the risk of positive cancer margins if nerve sparing is attempted [28]. Although novel nerve sparing techniques and rehabilitation protocols help patients regain sexual potency and urinary continence over time, therapeutic strategies targeting expedited biological repair and regeneration of nerves could hasten return to function following RARP [10]. One promising and recent biologic approach to expediting return to potency and continence is the utilization of commercially available perinatal tissue derived allografts. These grafts have been used to wrap the neurovascular bundle intraoperatively at the end of nerve sparing RARP [29].
Overview of perinatal tissues and their historic clinical use as allografts
The perinatal tissues include the amniotic (AM) and chorionic (CM) membranes which sequester amniotic fluid (AF) (Fig. 1). Together, these tissues physically protect the developing fetus and afford immunological segregation from the mother’s immune system [30]. The AM is the innermost membrane immediately adjacent to the AF and is composed of distinct layers including (from lumen to deep) an epithelial layer, a basement membrane, a compact layer and the intermediate (i.e. spongy) layer [31, 32]. The CM is approximately four times thicker than the AM and is comprised of a reticular layer, basement membrane and trophoblast layer which is adjacent to the maternal decidua tissue [33]. Both the AM and CM contain extracellular matrix (ECM), including proteoglycans, glycosaminoglycan, collagen types I and IV, glycoproteins, elastin, fibronectin and laminin in different quantities and ratios [34]. The umbilical cord (UC) is also considered a perinatal tissue which is comprised of two arteries and one vein that are surrounded by a hyaluronic acid and chondroitin sulfate connective tissue known as Wharton’s jelly [35]. Together, these elements are encased within a single layer of AM (Fig. 1). The UC is twice as thick as AM/CM and also contains laminin, fibronectin and type I collagen [36].
(Center) Representative schematic of the perinatal tissues (specifically amnion, chorion and umbilical cord) with respect to the developing fetus. (Left) Hierarchical structure of the amnion (blue) which includes the epithelial layer, basement membrane, a compact layer, and a fibroblast layer. An intermediate spongy layer (grey) separates the amnion and chorion. The chorion (red) consists of a reticular layer, basement membrane, and trophoblast layer. Right: (Right) The umbilical cord contains two umbilical arteries, one vein. These elements are surrounded by Wharton's jelly (WJ) which together, are encased within a layer of amnion
During gestation, the AM, CM and UC contain viable cells including amniotic epithelial cells and mesenchymal stromal cells [37, 38]. These cells synthesize and deposit pleiotropic growth factors, cytokines, and other bioactive peptides which are subsequently sequestered within the tissue ECM. Studies have demonstrated that the bioactive factors within the membranes have anti-inflammatory, anti-fibrotic, anti-adhesive and pro-regenerative effects and thus may have a therapeutic benefit in wound healing [31, 39,40,41].
The first published manuscript highlighting the clinical use of perinatal membrane allografts was for skin transplantation in 1910 by Davis at Johns Hopkins [42]. In 1940, De Rötth presented the use of amniotic allografts to replace damaged conjunctiva [43]. Perinatal tissue grafts are often processed for clinical use via dehydration and terminal sterilization. Careful cleansing and dehydration of the allografts allows for the tissues to retain their therapeutic effects while removing pathogens from the tissue [41]. These tissues have since been used in a variety of clinical applications including dermatologic, ophthalmic, orthopedic, and dental [44, 45]. Currently, perinatal tissue allografts are most often used in wound healing applications including diabetic foot ulcers, venous leg ulcers, skin burns, and other chronic wounds [44, 46]. In regard to urology, perinatal tissues are starting to be explored in therapeutic approaches for a variety of conditions, including as nerve wraps in nerve sparing RARP [47,48,49,50].
Main text
Study selection and data acquisition
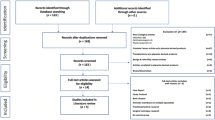
This nonsystematic literary review was performed in May 2024 using PubMed, EMBASE, Scopus, and Web of Science databases. The search terms utilized were “robotic prostatectomy”, “prostate cancer”, “nerve sparing”, “perinatal tissue”, “allograft”, “potency”, and “continence” alone or in combination. After removal of duplicates, all articles were reviewed and judged for scientific merit by authors RP and JM. Exclusion criteria were non-peer reviewed studies, abstract-only articles, non-English language articles, and studies that did not include either continence or potency outcomes. All studies included in this literature review adhered to ethical guidelines and received appropriate approvals regarding human subject participation.
Pre-clinical evidence of perinatal tissue-derived membrane allografts for nerve protection, repair and regeneration
Despite promising clinical findings, the potential mechanisms underpinning the therapeutic potential of perinatal tissue allografts have yet to be fully elucidated. Preclinical studies may provide initial clues as to the mechanisms by which these allografts may protect and help promote accelerated repair, regeneration and functional recovery of damaged nervous tissue.
To the best of the authors’ knowledge, the earliest and only known pre-clinical study evaluating the use of perinatal tissues to stimulate and support genitourinary nerve repair was reported by Burgers et al. [51] The authors transected a 5 mm segment of the cavernous nerves of sexually active male rats and subsequently anastomosed the gap with interpositional membranes or autologous nerve grafts. Membranes included AM allografts or polymeric membranes with or without nerve growth factor (NGF) [51]. Results demonstrated that rats receiving the AM graft displayed improved sexual behavior compared to both the nerve injury control rats and rats that received polymeric at 2-months post-op [51]. Moreover, the percentage of AM-treated rats that were able to achieve erection was statistically greater than the injury control and comparable to rats treated with polymeric grafts containing NGF [51]. The authors speculated that therapeutic benefit derived from the AM was due to either the release of neurotropic growth factors and/or the laminin-containing ECM that have been shown to support neuron growth [51]. Taken together, this study demonstrated that AM was able to stimulate and support regrowth of injured genitourinary nerves.
Although pre-clinical research focusing on the efficacy of perinatal tissue derived allografts to promote repair and regeneration of the genitourinary nerves is limited, studies evaluating their ability to promote repair of other peripheral nerves are increasing. These investigations point to several potential cellular mechanisms by which perinatal membrane derived allografts may support nerve repair and regeneration. For example, Lui et al. demonstrated that AM supports neuron growth and maturation in vitro [52]. Moreover, the authors demonstrated that wrapping AM around injured sciatic nerves prevented the formation of adhesions, reduced pro-inflammatory messenger RNA (mRNA) expression in local cells, and promoted a pro-regenerative / anti-inflammatory phenotype in local macrophages [52]. The authors also noted that the AM treated nerves had more dense and evenly distributed axons concomitant with increased presence of proliferating Schwann cells compared to injured controls [52]. Similarly, Mohammed et al. and Milgiliche et al. demonstrated the neuro-regenerative effects of perinatal tissue allografts using in vivo pre-clinical peripheral nerve injury models [53, 54]. Wolfe et al. demonstrated that wrapping repaired peripheral nerves with AM had fewer adhesions, significantly less perineural fibrosis, and improved nerve function at earlier time-points compared to injured controls and nerves wrapped with collagen [55]. Lemke et al. illustrated that the use of AM allografts as a nerve wrap decreased the occurrence of fibrosis and adhesions, while suppressing local tissue inflammation compared to untreated controls in a rat sciatic nerve perineural fibrosis model [56]. Furthermore, use of AM allografts decreased the occurrence of demyelination and hastened nerve recovery and regeneration [56]. Reduced fibrosis of peripheral nerves treated with perinatal membrane allografts have also been observed in other peripheral nerve transection models [57].
Taken together, these preclinical studies suggest that perinatal tissue allografts may possess physical and biological characteristics that can protect and support healing and regeneration of injured nerves and hasten return of nerve function and health. This may be due to both the neurotrophic growth factors and anti-inflammatory cytokines contained within them [58, 59]. Additionally, the allografts can serve as protective barriers to adhesions and thus may protect against tissue tethers which may impart traction injuries on the nerve bundles.
Clinical evidence of perinatal tissue allograft efficacy as an adjunct to RARP
Since 2015, eight clinical studies have been published demonstrating the efficacy of perinatal tissue allografts in radical prostatectomy treatments (Table 1) [60].
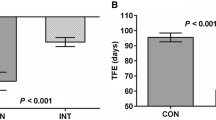
One of the first clinical series using dehydrated human amnion-chorion membrane (dHACM) as a protective wrap around the NVB during nerve sparing RARP was reported by Patel et al. [61] In this observational, retrospective, propensity score matched analysis, two patient groups (n = 58/group) were matched for age, body mass index (BMI), hypertension, diabetes, smoking history, Sexual Health Inventory for Men (SHIM) scores, PSA levels, Gleason scores, pre-operative American Urological Association symptom (AUA) scores, and D’Amico classifications. Group 1 patients received the dHACM graft wrapped around the NVB and group 2 served as controls. Post-operative potency was defined as the ability to maintain an erection with or without the use of Phosphodiesterase-5 (PDE-5) inhibitors while continence was defined as the use of zero safety pads per day. All patients completed a minimum follow-up period of 8-weeks. Results indicated that the mean time to continence was significantly shorter for group 1 (1.21 months) compared to group 2 (1.83 months; p = 0.033) [61]. Additionally, the mean time to potency was significantly shorter in group 1 (1.34 months) compared to group 2 (3.39 months; p = 0.007). [61]
Krol et al. presented a case study of a 67-year-old male who underwent a bilateral, nerve sparing RARP with NVBs allograft wrapping prior to posterior reconstruction [62]. This case study utilized dehydrated umbilical cord tissue, the only example of use of this material type in the literature. At 1 month postoperatively, the patient reported minimal stress urinary incontinence and the ability to achieve erections with 75% rigidity. At 1.5 months after surgery, the patient reported further improvements in continence and erections with 100% rigidity. The authors highlighted that patients who received tissue allografts had a faster time to recovery of continence and potency compared to the reported historical averages of 2.66 and 7.72 months, respectively. [62]
Razdan et al. performed a retrospective matched longitudinal cohort analysis of 1400 patients who underwent bilateral nerve sparing RARP to determine the impact of wrapping the CNVs with dehydrated AM allografts on early return to sexual potency [63]. Patients in the intervention (AM; n = 700) and control (no AM; n = 700) groups were matched for age, BMI, AUA score, PSA, clinical stage, baseline sexual function, Charlson comorbidity index and nerve sparing status. Study results indicated that patients receiving AM allografts demonstrated an earlier return to potency compared to controls (60.85 ± 61.2. days vs. 95.53 ± 76.2 days). Additionally, the number of patients achieving potency every month was significantly higher in the AM group compared to controls, and by the end of the 1-year follow-up, significantly higher potency rates were observed in the AM group compared to controls (93.1% vs. 87.1%) [63]. Time to potency recovery was also significantly less in the AM group.
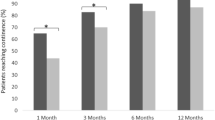
Ahmed et al. conducted a retrospective review of 200 patients who received bilateral, nerve sparing RARP [64]. The patients were split into two matched groups of statistically similar preoperative characteristics including BMI, age, comorbidities, smoking history, Gleason scores, and clinical stages. Out of these patients, 100 were treated with a cryopreserved UC allograft wrapped around the neurovascular bundles to assess acceleration of continence recovery rates. Post-operatively, all patients were assessed for continence based upon pad usage (0 or 1 safety pads per day) at 3, 6, 9, and 12 months postoperatively. Results indicated that the use of the allografts hastened return of continence at each time point compared to those who did not receive allografts at 1 month (65% vs. 44%; p = 0.018), 3 months (83% vs. 70%; p = 0.03), and at 12 months (97% vs. 87%; p = 0.009) [57]. When continence was defined as 0 pad usage, the percentage of patients exhibiting continence was statistically greater in the UC allograft group compared to controls at all time-points investigated (1 month: 55% vs. 30%; p = 0.003, 3 months: 68% vs. 52%; p = 0.021, 6 months: 84% vs. 64%; p = 0.001, 12 months (90% vs. 80%; p = 0.048). [64]
A controlled, matched propensity score analysis performed by Ogaya-Pinies et al. assessed expedited recoveries of potency by using dehydrated amnion/chorion membrane graft (dHACM) as a wrap around the neurovascular bundles after bilateral nerve sparing RARP procedures [65]. The study also examined the impact of using the dHACM on patients undergoing partial nerve sparing procedures. Study groups included 235 patients who received dHACM during their prostatectomy (group 1) and 705 patients controls (group 2). Overall, the mean time to potency was significantly shorter for group 1 (2.37 months) compared to group 2 (3.94 month; p < 0.001). The potency recovery rates with respect to time for group 1 versus group 2, respectively were as follows: 37% vs. 26.2% (p < 0.001) at 1 month, 65.1% vs. 57.8% (p < 0.001) at 3 months, 73.6% vs. 67.4% (p < 0.001) at 6 months, 77.9% vs. 72.9% (p < 0.001) at 9 months, and 80.4% vs. 78.7% (p < 0.001) at 12 months. In regard to potency outcomes by degree of nerve sparing, the investigators found that the time to potency was significantly shorter in patients receiving dHACM after full nerve sparing procedures (2.19 months) as compared to patients with full nerve sparing without dHACM (2.78 months; p = 0.029). Similarly, time to potency was significantly shorter in patients receiving dHACM after partial nerve sparing procedures (3.05 months) as compared to patients with partial nerve sparing without dHACM (3.92 months; p = 0.021). [65]
Elliot et al. performed a retrospective analysis evaluating the use of AM or UC tissue allografts (n = 162) placed intra-operatively over the bilateral NVBs versus controls that did not receive grafts (n = 181) [4]. Results demonstrated a statistically significant (p = 0.01) earlier return to continence in patients who received cryopreserved AM grafts (A1: 1.41 months) or cryopreserved UC grafts (A2: 1.45 months) versus controls (C: 1.64 months) [4]. The proportion of patients exhibiting continence for those receiving cryopreserved AM or UC grafts compared to controls were as follows: 1 month (A1: 81.2%, A2: 76.6%, C: 61.8%), 6 months (A1: 91.0%, A2: 84.3%, C: 79.7%), 9 months (A1: 94.6%, A2: 84.3%, C: 87.5%) and 12 months (A1: 98.2%, A2: 89.5%, C: 91.0%), respectively.
More recently, Noel et al. measured the medium-term functional outcomes in patients undergoing nerve sparing RALP treated with intra-operative dHACM allograft placement [29]. Five hundred twenty-nine patients were included in the study and underwent either partial bilateral nerve sparing (n = 138) or full bilateral nerve sparing (n = 391) RALP. Functionally, 82% of patients were sexually active following the procedure, defined by the ability to maintain erections for penetrative intercourse, and 96% regained continence, which was defined by zero pad usage. The median time to potency was 119 days, while the median time to continence was 42 days. When age was compared, patients ≤ 55 years old showed a median time to potency of 80 days vs. patients > 55 years old with 167 days (p = 0.005). Partial vs. full nerve sparing procedures were also compared, in which median time to potency for full nerve sparing patients was 92 days vs. 184 days in partial nerve sparing (p = 0.03) [29].
Finally, Barski et al. performed a proof of concept study exploring early functional outcomes in 14 patients undergoing open, nerve sparing radical prostatectomy that had both methylene blue and dHACM applied [66]. Methylene blue, a tinctorial dye and antioxidant [67, 68], was used to visualize the prostatic neuro-vascular plexus while amnion was placed around the nerves as well as at the dorsal portion of the vesico-urethral anastomosis. Results demonstrated that 40%, 70%, and 80% of patients recovered continence (defined as no pad) at 3 weeks, 3 months, and 12 months post-op, respectively. [66] The investigators also reported improved vesico-urethral anastomotic healing as indicated by no signs of scarring and the beginning of epithelialization in the urothelial mucosa as compared to controls evaluated with postoperative cystoscopy [66].
Taken together, the aforementioned clinical investigations indicate that the use of perinatal allografts as wraps around the NVB during RARP may quicken return to potency and continence in patients with localized PCa.
Discussion / Synthesis
Prostatectomy continues to be a mainstay of treatment for intermediate to high-risk prostate cancer and, despite the past several decades of advancements in surgical technique, there continues to be significant post-operative incontinence and erectile dysfunction morbidity [69]. Animal models and other pre-clinical studies have repeatedly elucidated how AM allografts support neurologic healing, diminish inflammation, and reduce fibrosis, although the exact mechanisms are not yet fully understood. The clinical studies reviewed in this article repeatedly demonstrate not only a statistically significant reduction in time-to-return for continence and potency, but also a clinically significant reduction time-to-return of several weeks to several months for both continence and potency.
As AM allografts continue to be used in more patients, the question emerges as to which pre-operative patient factors result in the most improved post-surgical outcomes. The studies reviewed here differ in their inclusion criteria. Several studies restricted the treated population to older patients, patients with pre-operative erectile and continence function close to normal, or patients with bilateral nerve sparing surgery, whereas others did not limit the treated population in such ways. In the context of this limitation, the data was mixed concerning which patient factors were associated with the most functional improvement. The studies generally concluded that using the allograft in bilateral nerve sparing offered the most improvement compared to unilateral nerve sparing. However, with regards to age, Ahmed et al. (UC allograft) found that patients > 60 had the most improvement with the allograft [64], however Razden et al. and Noel et al. (both dHACM allograft) found that younger patients benefitted the most from the graft [29, 63]. There was no consensus if patients with better pre-operative erectile and continence function who received the allograft had improved post-operative outcomes.
The studies included in this review differed in the type of allograft utilized. dHACM has been commercially available the longest and thus has been the most studied, but Ahmed et al. and Krol et al. used either cryopreserved or dehydrated UC allografts, respectively. [62, 64] However, new perinatal tissue allografts continue to become available, including a multi-layer, minimally processed graft that includes the intermediate layer in addition to the amnion and chorion, which has not yet been clinically studied [70].
The influence of AM allograft placement on biochemical recurrence (BCR) of PCa is a consequential question, especially in the time since Alvim et al. found faster relapse in prostate tumor cell models treated with AM allografts compared to control [71]. Overall, clinical studies of AM allografts have shown similar-to-lower rates of BCR in AM or UC treated groups compared to control [4, 29, 63, 72]. Thus, although there are in-vitro concerns that perinatal tissue allograft use could increase prostate cancer recurrence rates, this has not been substantiated by any in-vivo studies. However, as an emerging field, further study into the influence of perinatal tissue allograft use on BCR rates is warranted.
The studies presented in this review collectively have significant limitations. Most notably, several different allograft materials are represented in these studies, including dHACM, dehydrated UC, cryopreserved UC, and dehydrated amnion. Thus, although all of these materials are classified as perinatal tissue allografts, the significant heterogeneity in specific allograft type limits the generalizability of the outcomes. We theorize that as the perinatal allograft technology progresses, allograft material and preparation will begin to standardize across the industry. All the studies in this review are retrospective; some studies use propensity score matched analyses or retrospective matched longitudinal cohort analysis to improve study validity, but none of the studies resemble a randomized, controlled trial. Additionally, follow-up times are between 1 to 3.5 years, which is viable to study functional outcomes but much too short to make robust conclusions for oncologic outcomes. Furthermore, none of the literature examined surgeon nerve sparing RARP experience as a confounder of functional outcomes; we postulate that patients with experienced and adept surgeons would benefit less from allograft placement compared to patients of less-experienced nerve sparing surgeons, although this is merely a hypothesis. To date, no vigorous cost–benefit analysis of AM allografts has been conducted, although there is significant potential for cost-savings if allograft use can reduce post-prostatectomy treatment for erectile dysfunction and incontinence. Although the allografts discussed in this review were provided free-of-charge for investigational purposes, similar materials used commercially in wound healing cost $900-$2700 per graft. Since the emerging field of AM allograft placement in prostatectomy still lacks prospective, randomized controlled studies, this represents a noteworthy avenue for further study.
Conclusions
This review of current perinatal tissue allograft use in prostatectomy literature demonstrates that allograft use improves post-operative impotence and incontinence outcomes, which is further strengthened by the underlying biologic plausibility elucidated in basic science research. The emerging field has the potential to improve post-prostatectomy outcomes, but needs more robust clinical trials to truly prove its safety and efficacy.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- PCa:
-
Prostate cancer
- RARP:
-
robot assisted radical prostatectomy
- SEER:
-
Surveillance, Epidemiology, and End Results
- ED:
-
erectile dysfunction
- PSA:
-
Prostate Specific Antigen
- MRI:
-
magnetic resonance imaging
- CN:
-
cavernous nerve
- NVB:
-
prostatic neurovascular bundle
- NO:
-
nitric oxide
- PGE1 :
-
prostaglandin E1
- PGE2 :
-
prostaglandin E2
- TGF-β1:
-
growth factor transforming growth factor beta-1
- AM:
-
amniotic membrane
- CM:
-
chorionic membrane
- AF:
-
amniotic fluid
- ECM:
-
extracellular matrix
- UC:
-
umbilical cord
- dHACM:
-
dehydrated human amnion-chorion membrane
- BMI:
-
body mass index
- SHIM:
-
Sexual Health Inventory for Men
- AUA:
-
American Urological Association symptom
- PDE-5:
-
Phosphodiesterase-5
- NGF:
-
nerve growth factor
- mRNA:
-
messenger Ribonucleic Acid
- BCR:
-
biochemical recurrance
References
Siegel Mph RL, Miller KD, Sandeep N, et al. Cancer statistics, 2023. Published online. 2023. https://doi.org/10.3322/caac.21763.
Mariotto AB, Enewold L, Zhao J, Zeruto CA, Robin YK. Medical Care Costs Associated with Cancer Survivorship in the United States. Cancer Epidemiol Biomarkers Prev. 2020;29(7):1304–12. https://doi.org/10.1158/1055-9965.EPI-19-1534.
Cao L, Yang Z, Qi L, Chen M. Robot-assisted and laparoscopic vs open radical prostatectomy in clinically localized prostate cancer: perioperative, functional, and oncological outcomes: A Systematic review and meta-analysis. Med. 2019;98(22). https://doi.org/10.1097/MD.0000000000015770
Coughlin GD, Yaxley JW, Chambers SK, et al. Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: 24-month outcomes from a randomised controlled study. Lancet Oncol. 2018;19(8):1051–60. https://doi.org/10.1016/S1470-2045(18)30357-7.
Lima TFN, Bitran J, Frech FS, Ramasamy R. Prevalence of post-prostatectomy erectile dysfunction and a review of the recommended therapeutic modalities. Int J Impot Res. 2021;33(4):401–9. https://doi.org/10.1038/S41443-020-00374-8.
Hoyland K, Vasdev N, Abrof A, Bousted G. Post-radical prostatectomy incontinence: etiology and prevention. Rev Urol. 2014;16(4):181–8.
Rahnama’i MS, Marcelissen T, Geavlete B, Tutolo M, Hüsch T. Current Management of Post-radical Prostatectomy Urinary Incontinence. Front Surg. 2021;8. https://doi.org/10.3389/FSURG.2021.647656
Lardas M, Liew M, van den Bergh RC, et al. Quality of Life Outcomes after Primary Treatment for Clinically Localised Prostate Cancer: A Systematic Review. Eur Urol. 2017;72(6):869–85. https://doi.org/10.1016/J.EURURO.2017.06.035.
Dean RC, Lue TF. Physiology of penile erection and pathophysiology of erectile dysfunction. Urol Clin North Am. 2005;32(4):379–95. https://doi.org/10.1016/J.UCL.2005.08.007.
Fowler CJ, Griffiths D, De Groat WC. The neural control of micturition. Nat Rev Neurosci. 2008;9(6):453–66. https://doi.org/10.1038/NRN2401.
Jiang N, Wu C, Zhou X, Zhai G, Wu J. Cavernous Nerve Injury Resulted Erectile Dysfunction and Regeneration. J Immunol Res. 2021;2021. https://doi.org/10.1155/2021/5353785
Fregnan F, Muratori L, Simões AR, Giacobini-Robecchi MG, Raimondo S. Role of inflammatory cytokines in peripheral nerve injury. Neural Regen Res. 2012;7(29):2259–66. https://doi.org/10.3969/J.ISSN.1673-5374.2012.29.003.
Allison DJ, Green LA, Gabriel DA, Roy BD, Inglis JG, Ditor DS. Elevated concentrations of circulating cytokines and correlations with nerve conduction velocity in human peripheral nerves. J Neuroimmunol. 2014;277(1–2):134–9. https://doi.org/10.1016/J.JNEUROIM.2014.09.010.
Davies AL, Hayes KC, Shi R. Recombinant human TNFalpha induces concentration-dependent and reversible alterations in the electrophysiological properties of axons in mammalian spinal cord. J Neurotrauma. 2006;23(8):1261–73. https://doi.org/10.1089/NEU.2006.23.1261.
Ferrini MG, Davila HH, Kovanecz I, Sanchez SP, Gonzalez-Cadavid NF, Rajfer J. Vardenafil prevents fibrosis and loss of corporal smooth muscle that occurs after bilateral cavernosal nerve resection in the rat. Urology. 2006;68(2):429–35. https://doi.org/10.1016/J.UROLOGY.2006.05.011.
Hatzimouratidis K, Burnett AL, Hatzichristou D, McCullough AR, Montorsi F, Mulhall JP. Phosphodiesterase type 5 inhibitors in postprostatectomy erectile dysfunction: a critical analysis of the basic science rationale and clinical application. Eur Urol. 2009;55(2):334–47. https://doi.org/10.1016/J.EURURO.2008.10.028.
Gonzalez-Cadavid N, Rajfer J. The pleiotropic effects of inducible nitric oxide synthase (iNOS) on the physiology and pathology of penile erection. Curr Pharm Des. 2005;11(31):4041–6. https://doi.org/10.2174/138161205774913372.
Iacono F, Giannella R, Somma P, Manno G, Fusco F, Mirone V. Histological alterations in cavernous tissue after radical prostatectomy. J Urol. 2005;173(5):1673–6. https://doi.org/10.1097/01.JU.0000154356.76027.4F.
Casanova MR, Mota P, Vala H, et al. Functional recovery of injured cavernous nerves achieved through endogenous nerve growth factor-containing bioactive fibrous membrane. Acta Biomater. 2023;168:416–28. https://doi.org/10.1016/J.ACTBIO.2023.07.015.
C B, OO C, KT M, CA P. Nitric Oxide Synthase is Necessary for Normal Urogenital Development. Andrology (Los Angel). 2013;2(01). https://doi.org/10.4172/2167-0250.1000108
Li K, Zhao J, Wang M, et al. The Roles of Various Prostaglandins in Fibrosis: A Review. Biomol. 2021;11(6). https://doi.org/10.3390/BIOM11060789
Gacci M, De Nunzio C, Sakalis V, Rieken M, Cornu JN, Gravas S. Latest Evidence on Post-Prostatectomy Urinary Incontinence. J Clin Med. 2023;12(3). https://doi.org/10.3390/JCM12031190
Ficazzola MNV. The etiology of post-radical prostatectomy incontinence and correlation of symptoms with urodynamic findings. J Urol. 1998;160(4):1317–20.
Castellan P, Ferretti S, Litterio G, Marchioni M, Schips L. Management of Urinary Incontinence Following Radical Prostatectomy: Challenges and Solutions. Ther Clin Risk Manag. 2023;19:43–56. https://doi.org/10.2147/TCRM.S283305.
Noël J, Mascarenhas A, Patel E, et al. Nerve spare robot assisted laparoscopic prostatectomy with amniotic membranes: medium term outcomes. J Robot Surg Published online. 2022. https://doi.org/10.1007/s11701-022-01370-4.
Keeley R, Topoluk N, Mercuri J. Tissues reborn: fetal membrane-derived matrices and stem cells in orthopedic regenerative medicine. Crit Rev Biomed Eng. 2014;42(3–4):249–70. https://doi.org/10.1615/CRITREVBIOMEDENG.2014011591.
Mamede AC, Carvalho MJ, Abrantes AM, Laranjo M, Maia CJ, Botelho MF. Amniotic membrane: from structure and functions to clinical applications. Cell Tissue Res. 2012;349(2):447–58. https://doi.org/10.1007/S00441-012-1424-6.
Niknejad H, Peirovi H, Jorjani M, Ahmadiani A, Ghanavi J, Seifalian AM. Properties of the amniotic membrane for potential use in tissue engineering. Eur Cell Mater. 2008;15:88–99. https://doi.org/10.22203/ECM.V015A07.
Sabol TJ, Tran GS, Matuszewski J, Weston WW. Standardized reporting of amnion and amnion/chorion allograft data for wound care. Published online. 2022. https://doi.org/10.1002/hsr2.794.
Malak TM, Ockleford CD, Bell SC, Dalgleish R, Bright N, Macvicar J. Confocal immunofluorescence localization of collagen types I, III, IV, V and VI and their ultrastructural organization in term human fetal membranes. Placenta. 1993;14(4):385–406. https://doi.org/10.1016/S0143-4004(05)80460-6.
Davies JE, Walker JT, Keating A. Concise Review: Wharton’s Jelly: The Rich, but Enigmatic, Source of Mesenchymal Stromal Cells. Stem Cells Transl Med. 2017;6(7):1620–30. https://doi.org/10.1002/SCTM.16-0492.
Bullard JD, Lei J, Lim JJ, Massee M, Fallon AM, Koob TJ. Evaluation of dehydrated human umbilical cord biological properties for wound care and soft tissue healing. J Biomed Mater Res B Appl Biomater. 2019;107(4):1035–46. https://doi.org/10.1002/JBM.B.34196.
Parolini O, Alviano F, Bagnara GP, et al. Concise review: isolation and characterization of cells from human term placenta: outcome of the first international Workshop on Placenta Derived Stem Cells. Stem Cells. 2008;26(2):300–11. https://doi.org/10.1634/STEMCELLS.2007-0594.
Miki T. Amnion-derived stem cells: in quest of clinical applications. Stem Cell Res Ther. 2011;2(3). https://doi.org/10.1186/SCRT66
Kogan S, Sood A, Granick M. Amniotic membrane adjuncts and clinical applications in wound healing: a review of the literature. Wounds. 2018;30(6):168–73.
Koob TJ, Lim JJ, Massee M, Zabek N, Denozière G. Properties of dehydrated human amnion/chorion composite grafts: Implications for wound repair and soft tissue regeneration. J Biomed Mater Res B Appl Biomater. 2014;102(6):1353–62. https://doi.org/10.1002/jbm.b.33141.
Koob TJ, Rennert R, Zabek N, et al. Biological properties of dehydrated human amnion/chorion composite graft: implications for chronic wound healing. Int Wound J. 2013;10(5):493–500. https://doi.org/10.1111/IWJ.12140.
Davis JS. II. Skin grafting at the Johns Hopkins hospital. Ann Surg. 1909;50(3):542–9. https://doi.org/10.1097/00000658-190909000-00002.
De Rotth A. Plastic repair of conjunctival defects with fetal membranes. Arch Ophthalmol. 1940;23(3):522–5.
Jirsova K, Jones GLA. Amniotic membrane in ophthalmology: properties, preparation, storage and indications for grafting-a review. Cell Tissue Bank. 2017;18(2):193–204. https://doi.org/10.1007/S10561-017-9618-5.
Nejad AR, Hamidieh AA, Amirkhani MA, Sisakht MM. Update review on five top clinical applications of human amniotic membrane in regenerative medicine. Placenta. 2021;103:104–19. https://doi.org/10.1016/J.PLACENTA.2020.10.026.
Jahanafrooz Z, Bakhshandeh B, Behnam Abdollahi S, Seyedjafari E. Human amniotic membrane as a multifunctional biomaterial: recent advances and applications. J Biomater Appl. 2023;37(8):1341–54. https://doi.org/10.1177/08853282221137609.
Dinh T, Lewis C. Amnion Applications in the Foot and Ankle. Clin Podiatr Med Surg. 2019;36(4):563–76. https://doi.org/10.1016/J.CPM.2019.06.004.
Ramuta TŽ, Kreft ME. Human Amniotic Membrane and Amniotic Membrane-Derived Cells: How Far Are We from Their Use in Regenerative and Reconstructive Urology? Cell Transplant. 2018;27(1):77–92. https://doi.org/10.1177/0963689717725528.
Akerman J, Kovac JR. Amnion/chorion grafts and their applications in urology. Transl Androl Urol. 2017;6(Suppl 5):S903–5. https://doi.org/10.21037/TAU.2017.11.06.
Oottamasathien S, Hotaling JM, Craig JR, Myers JB, Brant WO. Amniotic therapeutic biomaterials in urology: current and future applications. Transl Androl Urol. 2017;6(5):943–50. https://doi.org/10.21037/TAU.2017.09.01.
Noël J, Ahmed S, Mascarenhas A, et al. Impact of human placental derivative allografts on functional and oncological outcomes after radical prostatectomy: a literature review. J Robot Surg. 2023;17(2):265–73. https://doi.org/10.1007/S11701-022-01433-6.
Patel VR, Samavedi S, Bates AS, et al. Dehydrated human amnion/chorion membrane allograft nerve wrap around the prostatic neurovascular bundle accelerates early return to continence and potency following robot-assisted radical prostatectomy: Propensity score-matched analysis. Eur Urol. 2015;67(6):977–80. https://doi.org/10.1016/j.eururo.2015.01.012.
Krol BC, Hemal AK, Peak T, Liu S, Pathak RA. Early return to continence and potency with use of dehydrated human umbilical cord graft at the time of robot-assisted radical prostatectomy: A case study and analysis of relevant literature. IJU Case Rep. 2021;4(3):151–3. https://doi.org/10.1002/IJU5.12267.
Razdan S, Bajpai RR, Razdan S, Sanchez MA. A matched and controlled longitudinal cohort study of dehydrated human amniotic membrane allograft sheet used as a wraparound nerve bundles in robotic-assisted laparoscopic radical prostatectomy: a puissant adjunct for enhanced potency outcomes. J Robot Surg. 2019;13(3):475–81. https://doi.org/10.1007/S11701-018-0873-7.
Ahmed M, Esposito M, Lovallo G. A single-center, retrospective review of robot-assisted laparoscopic prostatectomy with and without cryopreserved umbilical cord allograft in improving continence recovery. J Robot Surg. 2020;14(2):283–9. https://doi.org/10.1007/S11701-019-00972-9.
Ogaya-Pinies G, Palayapalam-Ganapathi H, Rogers T, et al. Can dehydrated human amnion/chorion membrane accelerate the return to potency after a nerve sparing robotic-assisted radical prostatectomy? Propensity score-matched analysis J Robot Surg. 2018;12(2):235–43. https://doi.org/10.1007/s11701-017-0719-8.
Elliott PA, Hsiang S, Narayanan R, et al. Cryopreserved placental tissue allograft accelerates time to continence following robot-assisted radical prostatectomy. J Robot Surg. 2021;15(6):877–83. https://doi.org/10.1007/S11701-020-01187-Z.
Barski D, Tsaur I, Boros M, Brune J, Otto T. Functional Recovery after the Application of Amniotic Tissues and Methylene Blue during Radical Prostatectomy-A Pilot Study. Biomedicines. 2023;11(8). https://doi.org/10.3390/BIOMEDICINES11082260
Seif C, Martínez Portillo FJ, Osmonov DK, et al. Methylene blue staining for nerve sparing operative procedures: An animal model. Urology. 2004;63(6):1205–8. https://doi.org/10.1016/j.urology.2003.12.020.
Stelmashook E V., Voronkov DN, Stavrovskaya A V., et al. Neuroprotective effects of methylene blue in streptozotocin-induced model of Alzheimer’s disease. Brain Res. 2023;1805. https://doi.org/10.1016/J.BRAINRES.2023.148290
Burgers JK, Nelson RJ, Quinlan DM, Walsh PC. Nerve growth factor, nerve grafts and amniotic membrane grafts restore erectile function in rats. J Urol. 1991;146(2):463–8. https://doi.org/10.1016/S0022-5347(17)37825-4.
Liu C, Liu D, Zhang X, Hui L, Zhao L. Nanofibrous polycaprolactone/amniotic membrane facilitates peripheral nerve regeneration by promoting macrophage polarization and regulating inflammatory microenvironment. Int Immunopharmacol. 2023;121. https://doi.org/10.1016/J.INTIMP.2023.110507
Mohammad J, Shenaq J, Rabinovsky E, Shenaq S. Modulation of peripheral nerve regeneration: a tissue-engineering approach. The role of amnion tube nerve conduit across a 1-centimeter nerve gap. Plast Reconstr Surg. 2000;105(2):660–6. https://doi.org/10.1097/00006534-200002000-00027.
Mligiliche N, Endo K, Okamoto K, Fujimoto E, Ide C. Extracellular matrix of human amnion manufactured into tubes as conduits for peripheral nerve regeneration. J Biomed Mater Res. 2002;63(5):591–600. https://doi.org/10.1002/JBM.10349.
Wolfe EM, Mathis SA, Ovadia SA, Panthaki ZJ. Comparison of Collagen and Human Amniotic Membrane Nerve Wraps and Conduits for Peripheral Nerve Repair in Preclinical Models: A Systematic Review of the Literature. J Reconstr Microsurg. 2023;39(4):245–53. https://doi.org/10.1055/S-0041-1732432.
Lemke A, Ferguson J, Gross K, et al. Transplantation of human amnion prevents recurring adhesions and ameliorates fibrosis in a rat model of sciatic nerve scarring. Acta Biomater. 2018;66:335–49. https://doi.org/10.1016/J.ACTBIO.2017.11.042.
Bai J, Liu C, Kong L, Tian S, Yu K, Tian D. Electrospun Polycaprolactone (PCL)-Amnion Nanofibrous Membrane Promotes Nerve Regeneration and Prevents Fibrosis in a Rat Sciatic Nerve Transection Model. Front Surg. 2022;9. https://doi.org/10.3389/FSURG.2022.842540
Bourgeois M, Loisel F, Obert L, Pluvy I, Gindraux F. Can the amniotic membrane be used to treat peripheral nerve defects? A review of literature. Hand Surg Rehabil. 2019;38(4):223–32. https://doi.org/10.1016/J.HANSUR.2019.05.006.
Moore MC, Bonvallet PP, Damaraju SM, Modi HN, Gandhi A, McFetridge PS. Biological characterization of dehydrated amniotic membrane allograft: Mechanisms of action and implications for wound care. J Biomed Mater Res B Appl Biomater. 2020;108(8):3076–83. https://doi.org/10.1002/JBM.B.34635.
Samaritan Biologics - Perinatal Allografts. https://www.samaritanbiologics.com/products/perinatal-allografts. Accessed 21 Apr 2024.
Alvim RG, Hughes C, Somma A, et al. The potential risk of tumor progression after use of dehydrated human amnion/chorion membrane allograft in a positive margin resection model. Ther Adv Urol. 2019;11:1–10. https://doi.org/10.1177/1756287219837771.
Noël J, Stirt D, Moschovas MC, et al. Oncologic outcomes with and without amniotic membranes in robotic-assisted radical prostatectomy: A propensity score matched analysis. Asian J Urol. 2024;11(1):19–25. https://doi.org/10.1016/J.AJUR.2022.05.004.
Moschovas MC, Patel V. Nerve-sparing robotic-assisted radical prostatectomy: how I do it after 15.000 cases. Int Braz J Urol. 2022;48(2):369–70. https://doi.org/10.1590/S1677-5538.IBJU.2022.99.03.
Görgen ARH, Burttet LM, Cachoeira ET, et al. Association of nerve-sparing grading in robotic radical prostatectomy and trifecta outcome. World J Urol. 2022;40:2925–30. https://doi.org/10.1007/s00345-022-04196-9.
Wang X, Wu Y, Guo J, et al. Intrafascial nerve-sparing radical prostatectomy improves patients’ postoperative continence recovery and erectile function: A pooled analysis based on available literatures. Med. 2018;97(29):11297. https://doi.org/10.1097/MD.0000000000011297.
Moris L, Gandaglia G, Vilaseca A, et al. Evaluation of Oncological Outcomes and Data Quality in Studies Assessing Nerve-sparing Versus Non-Nerve-sparing Radical Prostatectomy in Nonmetastatic Prostate Cancer: A Systematic Review. Eur Urol Focus. 2022;8(3):690–700. https://doi.org/10.1016/j.euf.2021.05.009.
Acknowledgements
Not applicable
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AGP, JM, and KR contributed to manuscript drafting. AGP, AK, JM, and RAP contributed to manuscript revision. JC, JM, and RAP contributed to conception and design. AGP, KR, and JM contributed to table and figure preparation. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
JM and JC are employed by Samaritan Biologics. The other authors declare that they have no competing interests.
Additional information
Publishers’ Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Perry, A.G., Kahn, A., Mercuri, J. et al. Preclinical and clinical evidence for using perinatal tissue allografts in nerve sparing robot assisted radical prostatectomy to hasten recovery of functional outcomes: a literature review. BMC Urol 24, 208 (2024). https://doi.org/10.1186/s12894-024-01593-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-024-01593-7