Abstract
Background
Diffuse pigmented villonodular synovitis (PVNS) is prone to recurrence after surgery, and it is difficult to achieve a long-term complete cure.
Objective
To reduce the recurrence rate of PVNS, the author pioneered the arthroscopic total synovial peel (ATSP).
Methods
From March 2014 to July 2020, a total of 19 patients (6 males and 13 females) with diffuse PVNS of the knee were treated in our department and underwent ATSP. It’s ‘peel’ rather than simple excision. This method is similar to peeling bark. Relapse rates and functional scores were determined, with follow-ups ranging from 12 to 72 months, on average 36 months.
Results
Treatment efficacy was assessed by imaging and functional scores. Imaging results indicated a recurrence rate of 10.5%. In patients without recurrence, the visual analog score (VAS) decreased from 4.76 ± 2.02 preoperatively to 1.56 ± 1.15 postoperatively. The Tegner-Lysholm knee function score (TLS) score increased from 67.76 ± 15.64 preoperatively to 90.32 ± 8.32 postoperatively. Compared with the literature, ATSP significantly reduces the postoperative recurrence rate of diffuse PVNS. The preliminarily findings suggest that this approach could greatly reduce the recurrence rate of postoperative PVNS in follow-up studies.
Conclusion
This approach may be a viable option for treating diffuse PVNS via arthroscopy and is worthy of clinical consideration.
Similar content being viewed by others
Introduction
Diffuse pigmented villonodular synovitis (PVNS) is a group of chronic synovial proliferative lesions of unknown etiology which are inflammatory and benign, often occurring in joints, tendons, and synovium [1]. PVNS usually occurs in adults between the ages of 20 and 40 years and most often involves the synovium of large joints, especially the knee [2]. At present, the main treatment method is arthroscopic total synovectomy. Postoperative recurrence rates are high with either open or arthroscopic surgery, especially for diffuse PVNS of the knee joint, and repeated attacks of PVNS can lead to damage to articular cartilage. The destruction of bone affects joint function [3,4,5]. Therefore, the complete removal of the synovium of the lesions and the reduction of recurrence are the basic principles of diffuse PVNS treatment [6, 7]. To completely remove diffuse PVNS synovial lesions, the Department of Joint and Orthopedics of Zhu Jiang Hospital of Southern Medical University innovatively adopted the method of arthroscopic total synovial peel (ATSP). The purpose of this study was to test whether ATSP can effectively reduce the recurrence of diffuse PVNS and its effects on patients’ pain scores and Tegner Lysholm knee function scores.
Materials and methods
Study design
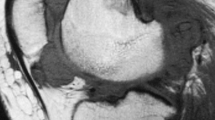
From March 2014 to July 2020, a total of 19 patients (6 males and 13 females) with diffuse PVNS of the knee were treated in our department, aged 6–78 years (average 39.8 years), and the course of the disease was 20 days−10 years. This study have been performed in accordance with the Declaration of Helsinki and been approved by the ethics committees of Zhu Jiang Hospital of Southern Medical University ethically and provided the corresponding ethical certificate (No. 2021-KY-165-03) and informed consent. All patients complained of varying degrees of knee joint swelling, pain, and dysfunction before surgery. A preoperative MRI examination was performed for the initial diagnosis of diffuse PVNS as shown in Fig. 1, then all cases were confirmed to be PVNS by postoperative pathology. The postoperative follow-up time was 1–6 years. As shown in Table 1 below.
Main equipment
The 4.0 mm, 30 ° angle arthroscopy, cold light source, camera imaging system and planing system produced by Shrek company of the United States (model 1488-010-0001). The plasma cold ablation instrument and the electric pneumatic tourniquet produced by Smith & nephew company of the United Kingdom.
Surgical methods
The patient was placed in a supine position, and the combined spinal-epidural nerve block (intratracheal general anesthesia for children and patients unable to lumbar puncture), a pneumatic tourniquet on the upper-middle and upper thighs (200mmHg for children, 350mmHg for adults, 90 min), and the normal saline with the specification of 3 L/Bag was suspended at a height of about 1.5 m from the operating table for joint cavity irrigation. The anterolateral approach of the patella is routinely used to examine the suprapatellar capsule, patellofemoral joint, medial groove, medial joint space, intercondylar fossa, lateral joint space, and lateral groove in turn to understand the distribution and proliferation of synovium, as well as ligaments, and semilunar involvement of the plate. After the exploration, an operating instrument was placed in the anteromedial approach, and part of the synovial tissue was clipped with forceps at the typical site of synovial hyperplasia for pathological examination. Subsequent HE staining was performed. Then a planer was used to operate alternately in the anteromedial and anterolateral approach, sequentially removing diseased synovial tissue in the surface of the suprapatellar pouch, medial groove, inferomedial groove and intercondylar groove, lateral groove and inferolateral groove, and medial and lateral meniscal. For diseased synovial tissue in the cruciate ligaments as well as on the medial and lateral patellar surfaces, they also need to be cleared together. The most critical surgical approach is to find the synovial space between the synovial layer and the muscle layer, based on this space, the synovial layer, the sub-synovial layer and the adipose layer were nearly completely peeled off, and the stripping depth reached to the muscle layer. The intraoperative image is shown in Fig. 2. Finally, the joint cavity was rinsed thoroughly with a large amount of normal saline, the intra-articular saline was sucked up before suturing the surgical port, and injecting 5ml of local anesthetic along with 40 mg of triamcinolone acetonide acetate into the joint cavity from the outer edge of the patella with a syringe for postoperative analgesia and avoiding joint adhesion. There was 1 built-in drainage tube for closed negative pressure drainage. Appropriate pressure dressing with cotton pads and elastic bandages was applied to the affected limb.
Histological staining
Synovial tissues were harvested and fixed with 4% paraformaldehyde for 2 h. They were subsequently dehydrated and embedded in paraffin. Paraffin sections were made to a thickness of 5 μm. Conventional HE staining was subsequently performed, and the stained sections were scanned using a multifunctional digital pathology scanner (Aperio VERSA 8). Subsequently, image information was acquired.
Post-operative management and rehabilitation exercises
After the operation, symptomatic treatments such as ice compress, analgesia, stomach protection, and appropriate dehydration were given. Isometric contractions and quadriceps straight leg raises were performed after the patient was awake. After 2 days, the drainage tube was removed depending on the amount of drainage, the dressing was changed every other day, and the wound was properly pressurized and bandaged; after the drainage tube was removed, active knee flexion and extension exercises and continuous passive training (1/day, 30 min/time) were performed, and active and passive training was required 1 week after surgery including bending the knee to ≥ 120°. None of the 19 cases showed excessive joint effusion after the operation, and the patients were instructed to avoid strenuous activities within half a year after discharge and to perform daily straight-leg raising exercises.
Efficacy evaluation criteria
The main evaluation index was the recurrence rate at the last follow-up, and the secondary evaluation indexes were the VAS and the TLS [8] at the last follow-up compared with the preoperative data.
Statistical analysis
SPSS 25.0 software package was used for data processing. The VAS and TLS were used for paired data t-test before knee arthroscopy and during the return visit. All test data were expressed as (Mean ± SD), and the test level was set as α = 0.05.
Result
The histological structure of the synovium
The synovial space between the synovial layer and the muscle layer was found, based on this space, the synovial layer, the sub-synovial layer and the adipose layer were nearly completely peeled off. The histological structure of the synovium is shown in Fig. 3.
Recurrence rates
Follow-up was obtained postoperatively in all cases, the wounds had all healed by stage I at the 1-month postoperative follow-up, and the joint mobility, joint effusion, and pain showed significant improvement postoperatively than they did preoperatively. Among the treated patients, 2 of them suffered from postoperative recurrence. The criteria for the diagnosis of postoperative recurrence is PVNS confirmed by pathological examination. The two cases suffered recurrence at 7 and 10 months after operation, respectively (both were treated by secondary surgery and showed no recurrence manifestations in subsequent follow-ups), giving a recurrence rate of 10.5%, which is much smaller than reported in the literature [9]. MRI examination of non-recurred case, as shown in Fig. 4.
Functional outcome
As indicated in Fig. 5, the VAS reduced from 4.76 ± 2.02 preoperational to 1.56 ± 1.15 at the last follow-up (19th August, 2021) (P < 0.001), and the TLS improved from 67.76 ± 15.64 to 90.32 ± 8.32 at the last follow-up (19th August, 2021) (P < 0.001). The functional outcome calculated from all 19 cases. These score values all indicated a good functional prognosis.
Discussion
There are many factors contributing to the recurrence of PVNS. The prevailing view currently holds that incomplete clearance of diseased synovial tissue is the underlying cause of PVNS recurrence [10]. At present, the reported methods are only to resect the pathological synovial tissue. There are various ways of resection, which often cannot guarantee complete resection. For the first time, we clarified how to nearly completely remove the pathological synovial tissue from the perspective of tissue anatomy.
Based on the histological characteristics of synovial tissue, the method of peel is used, resulting in not only decreased bleeding but also nearly complete decortication of lesion tissue, which considerably minimizes recurrence and is suitable for clinical promotion. PVNS, particularly diffuse PVNS, is distinguished by its proclivity for recurrence [11,12,13]. Mollon et al. [14] showed an overall incidence of 21.8% after surgical resection of PVNS. Patel et al. [15] found a high recurrence rate of 47.6% after diffuse PVNS surgery with the use of arthroscopic procedures through a retrospective analysis of 214 patients. Hans Roland Dürr et al. [16] counted a 24% recurrence rate after surgical resection of PVNS, and there was no significant difference in the recurrence rate after surgical synovectomy of PVNS with or without adjunctive radiological synovioplasty (RSO). QinWei Guo et al. [11] demonstrated a higher recurrence rate in PNVS with lesion metastasis to the extra articular site compared to common PNVS. Studies have indicated that the preoperative neutrophil to lymphocyte ratio is valuable in predicting recurrence of PVNS of the knee [17]. Ogilvie Harris et al. [18] manifested that whether complete resection of diseased synovial tissue is the key factor affecting whether PVNS recur. Our team’s innovative approach to synovial peel was designed to overcome the current problem of incomplete synovial resection. According to statistics, our postoperative recurrence rate of PVNS was lowered to 10.5%, which is significantly lower than the more than 20% currently reported.
We found that the patients’ pain symptoms and joint function scores were significantly improved after treatment by ATSP through the postoperative follow-up statistics. The postoperative recovery of joint function was greatly improved, which has a close relationship with the less traumatic nature of arthroscopic surgery, as patients frequently appear with joint function issues following open surgery [19, 20]. Second, the entire treatment course was performed without radiological or chemical synostosis. Particularly radioisotope synovectomy must be performed by experienced professionals because of its potential for significant complications [21].
We treated diffuse PVNS starting from the anatomical characteristics of the synovium, and the study had certain limitations. First, the sample size of the present study was small, which was related to the characteristics of the low incidence of PVNS. Second, individual patient follow-up was relatively short. As is known to all, the longer the follow-up, the more reliable the data obtained. Carl Ferdinand Capellen et al. [22] suggested that 18% of patients recurred within 18 months, and more than 90% of patients recurred within the first three years. This seems to illustrate that the recurrence of diffuse PVNS is mainly within three years after surgery.
Conclusion
An arthroscopic synovectomy is the main method for the treatment of PVNS. We have greatly reduced the recurrence rate of patients with diffuse lesions by total synovial peel. Moreover, the knee function recovered significantly after the operation, with less trauma and rapid recovery. Therefore, the preliminarily findings suggest that ATSP in the treatment of PVNS is worthy of clinical promotion.
Availability of data and materails
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PVNS:
-
Pigmented villonodular synovitis
- ATSP:
-
Arthroscopic total synovial peel
- VAS:
-
Visual analog score
- TLS:
-
Tegner-Lysholm score
- RSO:
-
Radiological synovioplasty
References
Stephan SR, Shallop B, Lackman R, Kim TWB, Mulcahey MK. Pigmented villonodular synovitis: a comprehensive review and proposed treatment algorithm. JBJS Rev. 2016;4(7):e3.
Tyler WK, Vidal AF, Williams RJ, Healey JH. Pigmented villonodular synovitis. J Am Acad Orthop Surg. 2006;14(6):376–85.
O’Keefe RJ, Rosier RN, Teot LA, Stewart JM, Hicks DG. Cytokine and matrix metalloproteinase expression in pigmented villonodular synovitis may mediate bone and cartilage destruction. Iowa Orthop J. 1998;18:26–34.
Shekhar A, Singh S, Patil SS, Tapasvi SR. Osteochondral lesion in diffuse pigmented Villonodular Synovitis of the knee. Knee Surg Relat Res. 2019;31(1):67–71.
Uchibori M, Nishida Y, Tabata I, Sugiura H, Nakashima H, Yamada Y, Ishiguro N. Expression of matrix metalloproteinases and tissue inhibitors of metalloproteinases in pigmented villonodular synovitis suggests their potential role for joint destruction. J Rheumatol. 2004;31(1):110–9.
De Ponti A, Sansone V, Malchere M. Result of arthroscopic treatment of pigmented villonodular synovitis of the knee. Arthroscopy. 2003;19(6):602–7.
Martin RC, Osborne DL, Edwards MJ, Wrightson W, McMasters KM. Giant cell tumor of tendon sheath, tenosynovial giant cell tumor, and pigmented villonodular synovitis: defining the presentation, surgical therapy and recurrence. Oncol Rep. 2000;7(2):413–9.
Chen WM, Wu PK, Liu CL. Simultaneous anterior and posterior synovectomies for treating diffuse pigmented villonodular synovitis. Clin Orthop Relat Res. 2012;470(6):1755–62.
Xie GP, Jiang N, Liang CX, Zeng JC, Chen ZY, Xu Q, Qi RZ, Chen YR, Yu B. Pigmented villonodular synovitis: a retrospective multicenter study of 237 cases. PLoS ONE. 2015;10(3):e0121451.
Keyhani S, Kazemi SM, Ahn JH, Verdonk R, Soleymanha M. Arthroscopic treatment of diffuse pigmented Villonodular Synovitis of the knee: complete synovectomy and septum removal-midterm results. J Knee Surg. 2019;32(5):427–33.
Guo Q, Shi W, Jiao C, Xie X, Jiang D, Hu Y. Results and recurrence of pigmented villonodular synovitis of the ankle: does diffuse PVNS with extra-articular extension tend to recur more often? Knee Surg Sports Traumatol Arthrosc. 2018;26(10):3118–23.
Fecek C, Carter KR. Pigmented Villonodular Synovitis. StatPearls.edn. Treasure Island (FL); 2022.
Cao C, Wu F, Niu X, Hu X, Cheng J, Zhang Y, Li C, Duan X, Fu X, Zhang J, et al. Cadherin-11 cooperates with inflammatory factors to promote the migration and invasion of fibroblast-like synoviocytes in pigmented villonodular synovitis. Theranostics. 2020;10(23):10573–88.
Mollon B, Lee A, Busse JW, Griffin AM, Ferguson PC, Wunder JS, Theodoropoulos J. The effect of surgical synovectomy and radiotherapy on the rate of recurrence of pigmented villonodular synovitis of the knee: an individual patient meta-analysis. Bone Joint J. 2015;97–B(4):550–7.
Patel KH, Gikas PD, Pollock RC, Carrington RW, Cannon SR, Skinner JA, Briggs TW, Aston WJS. Pigmented villonodular synovitis of the knee: a retrospective analysis of 214 cases at a UK tertiary referral centre. Knee. 2017;24(4):808–15.
Durr HR, Capellen CF, Klein A, Baur-Melnyk A, Birkenmaier C, Jansson V, Tiling R. The effects of radiosynoviorthesis in pigmented villonodular synovitis of the knee. Arch Orthop Trauma Surg. 2019;139(5):623–7.
Zhao G, Wang J, Xia J, Wei Y, Wang S, Huang G, Chen F, Chen J, Shi J, Yang Y. The predictive value of preoperative neutrophil-lymphocyte ratio (NLR) on the recurrence of the local pigmented villonodular synovitis of the knee joint. BMC Musculoskelet Disord. 2018;19(1):339.
Ogilvie-Harris DJ, McLean J, Zarnett ME. Pigmented villonodular synovitis of the knee. The results of total arthroscopic synovectomy, partial, arthroscopic synovectomy, and arthroscopic local excision. J Bone Joint Surg Am. 1992;74(1):119–23.
Nakahara H, Matsuda S, Harimaya K, Sakamoto A, Matsumoto Y, Okazaki K, Tashiro Y, Iwamoto Y. Clinical results of open synovectomy for treatment of diffuse pigmented villonodular synovitis of the knee: case series and review of literature. Knee. 2012;19(5):684–7.
Flandry FC, Hughston JC, Jacobson KE, Barrack RL, McCann SB, Kurtz DM. Surgical treatment of diffuse pigmented villonodular synovitis of the knee. Clin Orthop Relat Res. 1994;300:183–92.
Andre V, Dalibard V, Dernis E, Varin S, Cormier G. Current role for radioisotope synovectomy. Jt Bone Spine. 2018;85(3):295–9.
Capellen CF, Tiling R, Klein A, Baur-Melnyk A, Knosel T, Birkenmaier C, Roeder F, Jansson V, Durr HR. Lowering the recurrence rate in pigmented villonodular synovitis: a series of 120 resections. Rheumatology (Oxford). 2018;57(8):1448–52.
Acknowledgements
We thank the nursing staff of the Department of Joint and Orthopedics, Zhujiang Hospital for their insightful care of the patients.
Funding
This work was financially supported by the Natural Science Foundation of Guangdong Province (grant no. 2214050005549).
Author information
Authors and Affiliations
Contributions
H-QS and G-FW completed follow-up and collected data, and the writing of the first draft of the article. W-ZQ assisted in collecting and writing the article. L-JL designed the experiment, analyzed the data and perfected the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study have been performed in accordance with the Declaration of Helsinki and been approved by the ethics committees of Zhu Jiang Hospital of Southern Medical University ethically and provided the corresponding ethical certificate (NO. 2021-KY-165-03) and informed consent. Written informed consent was obtained from each participants after clarification of the study objectives and activities.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Song, HQ., Wu, GF., Qi, WZ. et al. Diffuse pigmented villonodular synovitis treated with arthroscopic total synovial peel. BMC Surg 23, 12 (2023). https://doi.org/10.1186/s12893-023-01906-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-023-01906-x