Abstract
Background
To explore and evaluate the predictive value of preoperative Neutrophil-lymphocyte ratio (NLR) on the recurrence of pigmented villonodular synovitis (PVNS) of the knee joint treated by arthroscopic surgery combining local radiotherapy.
Methods
Sixty pathological-proven PVNS cases of the knee joint in our department from April 2006 to March 2017 were included. All of them are treated by arthroscopic synovectomy combined with adjuvant radiotherapy. The pre-operative hematological indexes such as c-reactive protein (CRP), erythrocyte sedimentation rate (ESR), NLR, Platelet-lymphocyte ratio (PLR) and Lymphocyte-monocyte ratio (LMR) were collected retrospectively and their relationship with postoperative recurrence was analyzed by using univariate and multivariate analysis, the receiver operating characteristic curves (ROC curve), the Kappa correspondence test and the Mc Nemar Chi-square test.
Results
All 60 patients were followed up for a median of 52.8 months (7–138 months) and the recurrence rate is about 23.3% (14/60). There is a significant difference in NLR between the recurrent and non-recurrent group (P = 0.002). It had a certain correlation with postoperative recurrence (correlation coefficient r = 0.438, P = 0.001). The optimal thresholds in ROC curve were 2.42 (sensitivity 71.4%, specificity 78.3% respectively). which had predictive ability for recurrence after arthroscopic treatment.
Conclusion
The preoperative NLR is an easy and cost-effective predictor for relapse in PVNS of the knee joint after the arthroscopic surgery combined with local radiotherapy, which is of profound significance to guide clinical work.
Similar content being viewed by others
Background
Pigmented villonodular synovitis (PVNS) is a rare and benign disease of the synovial membrane characterized by abnormal synovium proliferation and hemosiderin deposition. According to previously reported statistics, the incidence rate is about 1.8/100000. It mostly affects the knee joint [1, 2], but can occurs in any synovial joint including the hip, ankle and elbow joint [3, 4]. The PVNS can be classified into the localized and diffuse forms (LPVNS and DPVNS) [5]. The etiology of the PVNS is still unknown yet while it was regarded as an inflammatory disorder in the past decades. Some risk factors have been recognized such as the trauma, chronic inflammation, and abnormal lipid metabolism [6]. Furthermore, PVNS would invade the adjacent bone and soft tissue leading to the bone errosion and the deformity of the involved joint [7, 8]. The high recurrence rate and metastasis risk of PVNS had also been reported [9], hence, up to now, PVNS has been considered to be a neoplastic-like disorder of the synovium, with synovitis as a secondary reaction in PVNS [10].
Many researchers has found that some hematological parameters like CRP [11], platelet volume [12], NLR [13] and PLR [14] are closely related with the outcomes of many diseases such as inflammatory disease, autoimmune disease and neoplastic disease [15]. Notably, NLR, PLR or LMR are new, simple and cost-effective predictors for prognosis. A meta-analysis conducted by Zhang J [16] found that the elevated NLR has a close relationship with the poorer overall survival of colorectal cancer (HR = 1.92 95%CI = 1.57–2.34; P < 0.00001). Kaida T et al. [17] also reported that PLR is an independent predictive factor of recurrence beyond the Milan criteria after liver resection for patients with hepatocellular carcinoma (odds ratio, 2.55; 95% confidence interval, 1.17–5.49; P = 0.018). However, there have been no reports regarding the relationship between NLR, PLR or LMR and the relapse of PVNS of knee joint, in addition, no quantitative parameters now can predict the recurrence of the PVNS of knee joint effectively.
In this study, we retrospectively reviewed the clinical characteristics, blood indexes, and recurrence of sixty cases diagnosed with LPVNS of knee joint in our department. The purpose of the present study is to explore the relationship between the NLR, PLR or LMR and the recurrence of the PVNS of knee joint. We hypothesized that some of these parameters could be used as new predictors for the recurrence of LPVNS of knee joint which were treated by arthroscopic surgery and adjuvant radiotherapy.
Methods
Patients
Huashan Hospital follow-up system (HSFS) is a database established on the inpatient and outpatient database. The HSFS comprises medical complete records of inpatient and outpatient. Sixty patients histopathological diagnosed with knee PVNS (29 men and 31 women) are included in this study at orthopedic department of Huashan Hospital from April 2006 to March 2017. The study was approved by the Ethical Committee in Huashan Hospital. Baseline data including age, sex, height, weight, body mass index, X rays, Magnetic Resonance images (MRI), and results of laboratory tests including neutrophil, lymphocyte, monocyte, platelet counts, erythrocyte sedimentation rate (ESR), C-reactive protein(CRP) were collected from HSFS in the study. Chronic synovitis, such as rheumatoid synovitis and synovial chondromatosis were excluded. All enrolled participants had no history of trauma and surgery when initially visited our department. Repeated swelling, pain and limited joint function were the main clinical manifestation and the time between symptom onset and hospital admission ranged from 2 months to 8 years.
Peroperative examinations
All patients received routine blood test and imaging examination including X rays and magnetic resonance image scan (MRI) before the surgery. In addition, the function of the involved knee joint before the surgery was assessed using Knee Society Score (KSS) and the Lyshoml Knee Score system.
Surgical procedures
All patients underwent comprehensive arthroscopic synovectomy in supine position under general anesthesia by an experienced surgeon. The pneumatic tourniquet (55-65 KPa) was used to stop the bleeding. Briefly, the standard anterolateral and anteromedial approaches were adopted and two 1 cm incisions was made on both sides of the patellar ligament in the front of the involved knee joint. Under the arthroscopic camera, the whole knee joint cavity was examined systematically according to the following order, suprapatellar bursa, patellofemoral joint, medial and lateral recess of the knee joint, tibiofemoral joint, meniscus and the anterior cruciate ligament. The abnormal synovial was removed as much as possible by using radiofrequency vaporization and shaving instruments. For PVNS lesions in the posterior joint, which was difficult to access from the anterior portals, the patients were placed prone. Posterolateral and posteromedial portals were used, and the PVNS lesions were removed as described before. Pathological examination of the abnormal synovium was performed routinely for each case. At the end of the procedure, surgeon would examine entire knee carefully again (Fig. 1). Finally, the wound was closed in layers.
Postoperative management
On the first day after surgery, Wound compression and ice compress were used as usual and patients were encouraged to start range of motion (ROM) exercise after removing the thick dressing on the next day. Furthermore, the patients were permitted to conduct full weight-bearing as long as they can tolerate the pain and the non-steroid anti-inflammatory drugs or analgesics and decongestants are provided to relieve the pain. All patients discharged with a significant improvement in range of motion of the affected knee joint (0–90 degrees). Importantly, in order to reduce the local recurrence rate, patients were all advised to the Cancer Hospital of Fudan University for adjuvant radiotherapy 4–6 weeks after the surgery (average total dose is 2000 cGy to 3000 cGy, 10–15 times).
Follow up
All 60 patients were followed through outpatient visit or telephone. The postoperative recurrence is defined as reoccurred joint swelling and pain 6 months after the treatment with typical appearance of PVNS on MRI images [18]. All patients were divided into the recurrent and non-recurrent group according to the outcome of the follow-up. The symptoms, Lysholm score and American KSS score were recorded before surgery and at final follow up evaluation or at the time of recurrence.
Data analysis
The normal distribution of the data was assessed using the Kolmogorov–Smirnov test, the normally distributed data are presented as the means ± standard deviation (X ± SD) and M (P25, P75) for non-normally distributed variables. Clinical characteristics were compared between the recurrent group and non-recurrent group using Pearson’s X2 test for categorical variables and independent t-test for continuous variables. Spearman correlation was applied to assess correlations between relpase and the preoperative NLR. Receiver operating characteristic (ROC) analysis was used for evaluation of predictive markers in the recurrence of the knee PVNS. The optimal cutoff values of several markers including NLR, PLR, LMR that the best distinguished recurrent group from the non-recurrent group was determined with the maximum value of Youden’s index, which was calculated by sensitivity + 1-specificity [19]. The overall diagnostic accuracy and predictive ability were estimated based on the area under the curve (AUC) which is reported with its standard error. A multivariable analysis was performed with significant markers from ROC curves to determine which of them are independently associated with the relapse of knee PVNS. McNemar test and Kappa consistency test were also conducted to evaluate the effectiveness of the predictors. All Statistical analysis were performed with the SPSS software for windows (version 20.0; SPSS, Chicago, IL). P < 0.05 was considered statistically significant.
Results
Sixty patients pathological diagnosed with PVNS were included (26 right knee, 34 left knee). The median age was 32 (range 14–75) years. On the MRI, the low signal intensity was presented on both T1 and T2 weighted images before the operation [18, 20]. The median duration of follow up was 52.8 (7–138) months and no complication of skin or wound infection was observed. Fourteen patients recurred and the median relapse time was 33.75 (20–51) months. Among the recurrent group, 3 patients underwent total knee arthroplasty and others received a second arthroscopy surgery.
Table 1 shows the clinical characteristics of the recurrent and non-recurrent group. The recurrent group showed higher NLR and CRP than non-recurrent group (PNLR = 0.002, PCRP = 0.04). There were no significant difference in other characteristics including PLR and LMR between the two groups (PPLR = 0.23, PLMR = 0.68).
The univariate and multivariate analysis were also performed with significant markers from ROC curves to determine which of them are independently associated with the diagnosis for relapse. The results indicates that NLR was significantly associated for prediction of relapse (odds ratio = 7.999, P = 0.017) (Table 2).
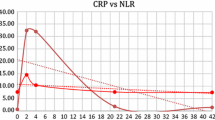
The optimal cutoff value that best distinguished recurrent from non-recurrent was determined at the maximum value, which was calculated by sensitivity + 1-specificity in the ROC curves. The ROC analysis of ESR, CRP, NLR, PLR and LMR showed the area under the curve (AUC) were 0.578 (95% CI = 0.443–0.704), 0.679 (95% CI = 0.545–0.793), 0.775 (95% CI = 0.649–0.873), 0.607 (95% CI = 0.473–0.731) and 0.537 (95% CI = 0.404–0.667) respectively (Fig. 2). Among the variables, the AUC of the NLR is the largest (AUC = 0.775, 95% CI = 0.649–0.873) and the optimal cut-off value is 2.42 for distinguishing the relapse which means when the NLR value is above 2.42 before treatment, the patient is more likely to have a relapse after the surgery. The Kappa test results (Kappa = 0.432, P = 0.001) and McNemar Chi-square test (P = 0.180) indicated that the NLR is valuable index for predicting the relapse.
The lyshoml and KSS score both improved in the two groups after the surgery though there is no significant difference before surgery and at the time of relapse in the recurrent group. Tables 3 and 4 shows that recurrent patients had poorer joint function than non-recurrent patients before the treatment did. In recurrent group, the knee functional score was higher at the time of relapse than that before operation while no significant difference was obtained. However, in non-recurrent group, most patients were satisfied with the greatly improved knee joint function and the difference in Lyshoml score and KSS score were statistically significant (P < 0.001) before surgery and at final follow up.
Discussion
This is the first study to explore the relationship between preoperative hematological parameters and the recurrence of the PVNS of the knee joint. Our results indicate that the preoperative NLR is a useful predictive biomarker for the recurrence of PVNS. In our research, the NLR is significantly higher in the recurrence group (P = 0.002), besides, the NLR shows good correlation with the relapse and has a high sensitivity and specificity to predict the postoperative relapse with a cutoff value of 2.42.
The PVNS is a locally aggressive, neoplastic-like disorder of synovial tissue that it would cause functional deterioration of the involved joint. The recurrence rate of the PVNS is as high as 10–50% for the residual diseased synovium after the simple synovectomy [21]. Isart A et al. [22] also reported a high recurrence of PVNS (61.5%, 8/13) after arthroscopic synovectomy. Moreover, it is almost impossible to resect the pathological synovium completely by open access or arthroscopic therapy [23]. So the high recurrence rate is still an intractable clinical issue despite many reports have claimed that adjuvant local radiotherapy after the synovectomy may be a salvage option [24]. What’s more, the non-specific symptoms of PVNS at its early stage often contribute to a delay in establishing a diagnosis, and the joint arthroplasty is the curative surgery in the terminal stage cases with severe bone erosion. So the early diagnosis of relapse is necessary in PVNS after the first treatment for its high recurrence rate. However, there has been no effective quantitatively marker for the relapse. The pathological examination is the gold standard and the MRI is the mostly used radiological tool for monitoring the relapse of PVNS. However, the MRI is qualitative and expensive and not available in some remote districts, additionally, the pathological examination always needs a second invasive procedure. Hence, finding an easy, non-invasive and cost-effective biomarker for relapse is a great challenge for surgeons.
The NLR can be obtained simply from neutrophil and lymphocyte counts. In addition, the NLR is cheaper relatively and it is obtainable in most medical institution for the blood routine examination is one of the routine preoperative test. Sever studies have demonstrated that the NLR、LMR and PLR are significantly associated with the outcome of many diseases. For example, Kucuk A et al. [25] reported that the NLR is obviously higher in Ankylosing spondylitis (AS) patients compared to controls. (NLR = 2.47 ± 1.33, 1.72 ± 0.47, respectively, P < 0.0001). Additionally, there is a significant difference between the severe AS disease activity and the mild AS disease activity (NLR = 2.72 ± 1.41, 2.20 ± 1.19, P = 0.001). The results of the ROC analysis (cutoff value = 1.91, sensitivity 69%, specificity 54%) also proved that NLR is a simple and inexpensive marker to indicate disease activity in patients with AS in daily clinical practice. Lin JP et al. [26] found preoperative LMR is an independent prognostic factor for GC which can improve the predictability of individual survival and recurrence of gastric cancer. Moreover, the predictive value of the NLR, LMR or PLR have been found in more and more diseases including the diabetes, hypertension, pancreatic cancer and hepatocellular carcinoma [27,28,29].
To our knowledge, there have been no report about the NLR, LMR or PLR in predicting the recurrence of the knee PVNS. In our study, 60 patients diagnosed with LPVNS were enrolled. With respect to the gender ratio, our result (1.07, 31/29) was similar to those reported in Portugal (1.15) [30]. The BMI has no significant difference between two groups All participants received an arthroscopic synovectomy for the diagnosis of the LPVNS, and Xie et al. [15] found that no significant recurrence difference was identified between PVNS patients that were treated with open versus arthroscopic surgery (p = 0.78). In addition, the knee arthroscopic surgery, a minimally invasive surgery, is beneficial for fast recovery and shorter the hospitalization time. What’s more, the local adjuvant radiotherapy was applied to decrease the local relapse as much as possible. In a multicenter retrospective study, the recurrence rate in patients with knee PVNS is 24% (42/175) [2]. In our study, the recurrence rate is about 23.3% (14/60) which is consistent with the literatures. Among all hematologic indexes, Only CRP and NLR are significantly higher in recurrent patients (PCRP = 0.04, PNLR = 0.002). Other parameters like WBC, Neutrophils count and ESR are higher in recurrent group compared to controls, but don’t reach a statistical difference (PWBC = 0.51, PESR = 0.208) which may implied that the PVNS is not a simple inflammatory disease. The results of ROC analysis and the multivariate analysis (Odds ratio = 7.99, 95% CI = 1.451–44.103, P = 0.017) indicated that the NLR may be a valuable marker for predicting relapse of knee PVNS after the treatment.
Limitations
There were also some limitations in our study. Firstly, the number of the participants is relatively small for the low incidence of the PVNS, so the larger clinical researches with longer-term follow up are needed. VSecondly, all the patients enrolled in our study received the arthroscopic synovectomy and radiotherapy. Therefore, the effect of the surgical methods on the relapse is unknown. Thirdly, the mean duration of symptoms before the treatment is not included in our study for its inaccuracy.
Conclusion
Our report suggests that the preoperative NLR is a valuable marker to predict the relapse of Knee PVNS treated by arthroscopic synovectomy combining radiotherapy. Our study indicated that these patients (preoperative NLR > 2.42) should be closely followed after the operation for the higher possibility of relapse. We hope this study could provide the orthopedic clinicians with a new method for predicting the postoperative recurrence of patients with PVNS.
Abbreviations
- AUC:
-
Area under the curve
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- HSFS:
-
Huashan Hospital follow-up system
- KSS:
-
Knee Society Score
- LMR:
-
Lymphocyte-monocyte ratio
- MRI:
-
Magnetic Resonance images
- NLR:
-
Neutrophil-lymphocyte ratio
- PLR:
-
Platelet-lymphocyte ratio
- PVNS:
-
Pigmented villonodular synovitis
- ROC:
-
Receiver operating characteristic
- ROM:
-
Range of motion
References
Myers BW, Masi AT. Pigmented villonodular synovitis and tenosynovitis: a clinical epidemiologic study of 166 cases and literature review. Medicine (Baltimore). 1980;59:223–38.
Xie GP, Jiang N, Liang CX, et al. Pigmented villonodular synovitis: a retrospective multicenter study of 237 cases. PLoS One. 2015;10:e0121451.
Wong JJ, Phal PM, Wiesenfeld D. Pigmented villonodular synovitis of the temporomandibular joint: a radiologic diagnosis and case report. J Oral Maxillofac Surg. 2012;70:126–34.
Lu H, Chen Q, Shen H. Pigmented villonodular synovitis of the elbow with rdial, median and ulnar nerve compression. Int J Clin Exp Pathol. 2015;8:14045–9.
Abdul-Karim FW, el-Naggar AK, Joyce MJ, Makley JT, Carter JR. Diffuse and localized tenosynovial giant cell tumor and pigmented villonodular synovitis: a clinicopathologic and flow cytometric DNA analysis. Hum Pathol. 1992;23:729–35.
Ottaviani S, Ayral X, Dougados M, Gossec L. Pigmented villonodular synovitis: a retrospective single-center study of 122 cases and review of the literature. Semin Arthritis Rheum. 2011;40:539–46.
Baba S, Motomura G, Fukushi J, et al. Osteonecrosis of the femoral head associated with pigmented villonodular synovitis. Rheumatol Int. 2017;37:841–5.
Descamps F, Yasik E, Hardy D, Lafontaine M, Delince P. Pigmented villonodular synovitis of the hip. A case report and review of the literature. Clin Rheumatol. 1991;10:184–90.
Yoon HJ, Cho YA, Lee JI, Hong SP, Hong SD. Malignant pigmented villonodular synovitis of the temporomandibular joint with lung metastasis: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:e30–6.
Yudoh K, Matsuno H, Nezuka T, Kimura T. Different mechanisms of synovial hyperplasia in rheumatoid arthritis and pigmented villonodular synovitis: the role of telomerase activity in synovial proliferation. Arthritis Rheum. 1999;42:669–77.
Ide S, Toiyama Y, Okugawa Y, et al. Clinical significance of C-reactive protein-to-albumin ratio with rectal Cancer patient undergoing Chemoradiotherapy followed by surgery. Anticancer Res. 2017;37:5797–804.
Wang X, Cui MM, Xu Y, et al. Decreased mean platelet volume predicts poor prognosis in invasive bladder cancer. Oncotarget. 2017;8:68115–22.
Liao LJ, Hsu WL, Wang CT, et al. Prognostic impact of pre-treatment neutrophil-to-lymphocyte ratio (NLR) in nasopharyngeal carcinoma: a retrospective study of 180 Taiwanese patients. Clin Otolaryngology. 2018;43(2):463–469.
Cetinkaya M, Buldu I, Kurt O, Inan R. Platelet-to-lymphocyte ratio: a new factor for predicting systemic inflammatory response syndrome after percutaneous Nephrolithotomy. Urol J. 2017;14:4089–93.
Yang Z, Zhang Z, Lin F, et al. Comparisons of neutrophil-, monocyte-, eosinophil-, and basophil- lymphocyte ratios among various systemic autoimmune rheumatic diseases. APMIS. 2017;125:863–71.
Zhang J, Zhang HY, Li J, Shao XY, Zhang CX. The elevated NLR, PLR and PLT may predict the prognosis of patients with colorectal cancer: a systematic review and meta-analysis. Oncotarget. 2017;8:68837–46.
Kaida T, Nitta H, Kitano Y, et al. Preoperative platelet-to-lymphocyte ratio can predict recurrence beyond the Milan criteria after hepatectomy for patients with hepatocellular carcinoma. Hepatol Res. 2017;47:991–9.
Cheng XG, You YH, Liu W, Zhao T, Qu H. MRI features of pigmented villonodular synovitis (PVNS). Clin Rheumatol. 2004;23:31–4.
Bewick V, Cheek L, Ball J. Statistics review 13: receiver operating characteristic curves. Crit Care. 2004;8:508–12.
Mandelbaum BR, Grant TT, Hartzman S, et al. The use of MRI to assist in diagnosis of pigmented villonodular synovitis of the knee joint. Clin Orthop Relat Res. 1988(231):135–139.
Murphey MD, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming DJ, Walker EA. Pigmented villonodular synovitis: radiologic-pathologic correlation. Radiographics. 2008;28:1493–518.
Isart A, Gelber PE, Besalduch M, et al. High recurrence and good functional results after arthroscopic resection of pigmented villonodular synovitis. Revista espanola de cirugia ortopedica y traumatologia. 2015;59:400–5.
Shabat S, Kollender Y, Merimsky O, et al. The use of surgery and yttrium 90 in the management of extensive and diffuse pigmented villonodular synovitis of large joints. Rheumatology (Oxford). 2002;41:1113–8.
Horoschak M, Tran PT, Bachireddy P, et al. External beam radiation therapy enhances local control in pigmented villonodular synovitis. Int J Radiat Oncol Biol Phys. 2009;75:183–7.
Kucuk A, Uslu AU, Ugan Y, et al. Neutrophil-to-lymphocyte ratio is involved in the severity of ankylosing spondylitis. Bratislavske lekarske listy. 2015;116:722–5.
Lin JP, Lin JX, Cao LL, et al. Preoperative lymphocyte-to-monocyte ratio as a strong predictor of survival and recurrence for gastric cancer after radical-intent surgery. Oncotarget. 2017;8:79234–47.
Hong YF, Chen ZH, Wei L, et al. Identification of the prognostic value of lymphocyte-to-monocyte ratio in patients with HBV-associated advanced hepatocellular carcinoma. Oncol Lett. 2017;14:2089–96.
Xue P, Hang J, Huang W, et al. Validation of lymphocyte-to-monocyte ratio as a prognostic factor in advanced pancreatic Cancer: an east Asian cohort study of 2 countries. Pancreas. 2017;46(8):1011–1017.
Guo X, Zhang S, Zhang Q, et al. Neutrophil:lymphocyte ratio is positively related to type 2 diabetes in a large-scale adult population: a Tianjin chronic low-grade systemic inflammation and health cohort study. Eur J Endocrinol. 2015;173:217–25.
Coutinho M, Laranjo A, Casanova J. Pigmented Villonodular synovitis: a diagnostic challenge. Review of 28 cases. Acta reumatologica portuguesa. 2012;37:335–41.
Availability of data and materials
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
GLZ and JW were involved in all the work of the article. JX were involved in the data collection and analysis. YBW, SQW, GYH, FYC, JC, JSS and YQY were involved in data collection. All authors have read and approved the manuscript, and ensure that this is the case.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Huashan Hospital. The participant consent was written, and was performed in accordance with the ethical standards of the Declaration of Helsinki of 1964.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhao, G., Wang, J., Xia, J. et al. The predictive value of preoperative neutrophil-lymphocyte ratio (NLR) on the recurrence of the local pigmented villonodular synovitis of the knee joint. BMC Musculoskelet Disord 19, 339 (2018). https://doi.org/10.1186/s12891-018-2258-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-018-2258-5