Abstract
Background
This study was to explore the relationship between cardiovascular health (CVH) and the risk of all-cause mortality in patients with osteoarthritis (OA).
Methods
This cohort study retrieved the data of 3642 patients with OA aged ≥ 20 years from the 2007—2018 National Health and Nutrition Examination Survey (NHANES). CVH was evaluated based on Life’s Essential 8 (LE8) includes diet, physical activity, nicotine exposure, sleep health, body mass index, blood lipids, blood glucose, and blood pressure. The outcome of all-cause mortality was assessed using the death certificate records of participants from the National Death Index. Variables that might affect all-cause mortality were used as covariates. The weighted univariate COX proportional hazards model was used to explore the association between each covariate and all-cause mortality. The weighted univariate and multivariate COX proportional hazards models were used to explore the association between different CVH levels and all-cause mortality. A restricted cubic spline (RCS) curve was plotted to show the association between different CVH levels and all-cause mortality in OA patients. Hazard ratio (HR) and 95% confidence interval (CI) were calculated.
Results
Findings show that people with moderate CVH (HR = 0.67, 95% CI = 0.45—0.98) and high CVH (HR = 0.47, 95% CI = 0.26—0.87) were associated with reduced risk of all-cause mortality in patients with OA. The HR of all-cause mortality in patients with OA decreased by 0.12 as per 10 points increase of LE8 score (HR = 0.81, 95% CI = 0.73—0.90). The RCS curve revealed that the HR of all-cause mortality decreased with the increase in LE8 score. The survival probability of patients in the high CVH group was higher than the moderate CVH group and low CVH group (p = 0.002).
Conclusion
Moderate-to-high CVH is associated with a decreased risk of all-cause mortality in patients with OA. These findings might provide a reference for the formulation of prognosis improvement strategies for the management of patients with OA.
Similar content being viewed by others
Background
Osteoarthritis (OA) is a prevalent form of arthritis, which is a chronic degenerative disease that causes disability characterized by complex disorders affecting the entire synovial joint [1]. The prevalence of symptomatic osteoarthritis (OA) is estimated to be around 240 million individuals worldwide, with approximately 10% of men and 18% of women aged 60 and above [2]. The Global Burden of Diseases, Injuries and Risk Factors Study (GBD) revealed that the age-standardized point prevalence and annual incidence rate of symptomatic, radiographically confirmed hip and knee OA were 3754.2 and 181.2 per 100,000 individuals, respectively, indicating a respective increase of 9.3% and 8.2% since 1990, globally [3]. OA has caused a huge disease burden, and patients with OA are at an increased risk of all-cause mortality [4, 5]. Previous studies have shown that various cardiovascular disease-related risk factors were closely associated with the progression and prognosis of OA [6,7,8,9,10,11,12,13].
Lifestyle factors such as diet quality, physical activity level, tobacco exposure, sleep duration, and metabolic disorders such as overweight and obesity, hypertension, diabetes, and dyslipidemia are important factors affecting cardiovascular health (CVH) [14,15,16,17,18]. Taking into account the comprehensive influence of various factors, the American Heart Association (AHA) has recently proposed a new score system, Life’s Essential 8 (LE8), which includes diet, physical activity, nicotine exposure, sleep health, body mass index, blood lipids, blood glucose, and blood pressure, as a tool to assess CVH [19]. The score of 8 components of LE8 score ranges from 0 to 100 points, and generates a new composite CVH score varying from 0 to 100 points. Different levels of LE8 score suggests different CVH [20]. Diet and exercise interventions were reported to be associated with the reduction of IL-6 levels [21]. The results from a surgical-induced murine model indicated that exposure to second-hand cigarette smoke exhibited more severe OA [22]. The risk of developing knee OA was elevated with a shorter duration of sleep at night and lower quality of sleep [23]. Several metabolic regulators were identified to play key roles in the pathogenesis of OA [24]. Dyslipidemia was also found as a risk factor for OA [25].
Studies have revealed that the LE8 score was associated with the risk of mortality in the general population and patients with inflammation-related diseases [26]. Higher LE8 scores were significantly related to a deceleration in PhenoAge, and oxidative stress biomarkers may play a mediating role in this relationship [27]. However, no study has investigated the effect of comprehensive CVH status on the long-term mortality risk of patients with OA. Thus, we aimed to explore the relationship between moderate-to-high CVH and the risk of all-cause mortality in patients with OA. We hypothesized that moderate-to-high CVH would be associated with a reduced risk of all-cause mortality in patients with OA compared to those with low CVH.
Methods
Study design and data source
Secondary data analysis was performed using data from the National Health and Nutrition Examination Survey (NHANES) between 2007 and 2018 in this cohort study. The NHANES, conducted by the Centers for Disease Control and Prevention’s National Center for Health Statistics (NCHS), has been monitoring the nation’s nutrition and health for over five decades. It gathers data that can be obtained through direct physical examinations, clinical and laboratory tests, personal interviews, and related measurement procedures. The examinations are carried out in mobile examination centers (MECs) that travel to various locations nationwide, ensuring a standardized environment for health assessments [28]. The surveys were approved by the National Center for Health Statistics Research. Details of study implementation are available for online access to NHANES Questionnaires, Datasets, and Related Documentation (cdc.gov) (https://wwwn.cdc.gov/Nchs/Hhanes).
Study participants
The data of 3642 individuals were retrieved from NHANES for this study if they met the following criteria: 1) ≥ 20 years old; 2) self-reported OA according to personal interview data on a variety of health conditions; 3) information for calculating LE8. Patients with OA without survival data were excluded. The status of OA was obtained through the following questionnaire: “Have you ever been diagnosed with arthritis by a doctor or other healthcare professional?” If the response to the initial question was “yes”, a follow-up query would be posed: “Which specific type of arthritis did you receive this diagnosis for?” Participants were categorized as having OA based on their responses to these questionnaires. All the participants were divided into high CVH (n = 239), moderate CVH (n = 1136), and low CVH (n = 301) groups.
The requirement of ethical approval for this study was waived by the Institutional Review Board of Binzhou Medical University Hospital because the data was accessed from a publicly available database of NHANES. The need for written informed consent was also waived due to the retrospective nature of the study. All methods were performed in accordance with the relevant guidelines and regulations.
All-cause mortality
The primary outcome of all-cause mortality was assessed using the death certificate records of participants obtained through linkage with the National Death Index (NDI). The all-cause mortality includes all deaths occurring during the follow-up period extending through December 2019.
Cardiovascular health
The CVH was assessed using the LE8 score [29]. The components of LE8 include diet, physical activity, nicotine exposure, sleep health, body mass index, blood lipids, blood glucose, and blood pressure. Diet quality was measured based on the Healthy Eating Index 2015 (HEI-2015) using data from 24-h dietary recalls. The assessment of physical activity was conducted based on self-reported frequency and duration of moderate exercise (resulting in mild perspiration or a slight increase in breathing or heart rate) and vigorous exercise (resulting in significant perspiration or a substantial increase in breathing or heart rate) over the preceding 30-day period. Nicotine exposure was assessed based on self-reported consumption of combustible cigarettes, use of e-cigarettes and other tobacco products within the previous 30 days, as well as self-reported secondhand smoke exposure in the participant's household. Sleep health was evaluated from the question on usual sleep duration per day. BMI was calculated as weight (kg)/height squared (m2).
Blood samples were collected at a mobile examination center and subsequently dispatched to a central laboratory for the evaluation of blood lipids, fasting glucose levels, and hemoglobin A1c concentrations. Information regarding the utilization of lipid-lowering medications, insulin therapy, or oral hypoglycemic agents was obtained through an in-depth questionnaire administered during home visits. Blood pressure measurements were taken thrice consecutively following 5 min of seated rest, with the average value derived from the second and third readings employed or the average value from the first two measurements for participants who only had two readings or solely relied on the initial measurement for those with just one reading. Details of antihypertensive drug usage were ascertained via interviews conducted during home visits.
Each metric has a new scoring algorithm ranging from 0 to 100 points according to the AHA scoring algorithm, allowing the generation of a new composite CVH score that also varies from 0 to 100 points, with a higher score meaning a better health status. LE8 score of 80 to 100 points was considered high CVH, 50 to 79 points was considered moderate CVH, and 0 to 49 points was considered low CVH according to the AHA advisory [19].
Covariates
The following variables that might affect all-cause mortality were used as covariates. Age in years used as continuous, gender dichotomized as female or male, and race categorized as Mexican American, non-Hispanic Black, non-Hispanic White, other Hispanic, or other races. The level of education was classified into less than 9th Grade, 9th-11th Grade, high school Grade/general equivalent diploma or equivalent, some college or Associate of Arts degree, or college graduate or above. Marital status and drinking alcohol were dichotomized into married or unmarried, yes or no, respectively. Moreover, the duration of OA, fracture, CVD, cancer, and drug for OA were dichotomized as yes or no, respectively. In addition, poverty to income ratio (PIR: ≤ 1.85, > 1.85, or unknown), white blood cell count (1000 cells/uL), and energy (kcal) were variables analyzed in our study.
CVD was defined based on the answer to the following question: “Have you ever been told you had (congestive) heart failure, coronary heart disease, angina/angina pectoris, heart attack, or stroke”. Patients with any one or more diseases were defined as CVD. Cancer was diagnosed according to the answer to “Have you ever been told you had cancer or malignancy?”. Drugs for OA include nonsteroidal anti-inflammatory agents, glucosamine, and sodium hyaluronate. Energy was calculated as dietary intake and dietary supplement use.
Statistical analysis
The measurement data were described as mean and standard error (S.E). The enumeration data were described as the number and percentage. The analysis of variance test for continuous variables and the Chi-square test or Fisher’s exact probability method for categorical variables was used to calculate the significance between groups. SDMVSTRA, SDMVPSU, and WTMEC2YR were applied as weighted variables.
As exhibited in Supplementary Table 1 and Supplementary Fig. 1–2, the Cox proportional hazard regression models are valid. The weighted univariate COX proportional hazards model was used to explore the association between each variable and all-cause mortality. The COX proportional hazards models (1, 2, and 3) were used to examine the association between moderate-to-high CVH and the risk of all-cause mortality. The low CVH was used as a reference group. Model 1 was the crude model, Model 2 adjusted for demographic covariates, and Model 3 adjusted for all covariates. The modifying effect of OA on the association between different CVH levels and mortality was evaluated using the weighted univariate and multivariate COX proportional hazards models. Missing values were dealt with using multiple imputations (Supplementary Table 2), and sensitivity analysis was conducted by comparing the analysis results of the data sets before and after the imputation of the missing values.
Subgroup analysis was stratified according to OA duration (< 5 and ≥ 5) and CVD (with and without CVD). A restricted cubic spline (RCS) curve was plotted to show the association between different CVH levels and all-cause mortality in OA patients. The modifying effect of OA on the association between CVH and mortality risk was further evaluated. Kaplan–Meier curve was plotted to show the survival probability of participants in low CVH, moderate CVH, and high CVH groups. Hazard ratio (HR) and 95% confidence interval (CI) were calculated. The confidence level was 0.05. SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) was used for data extraction and statistical analysis.
Results
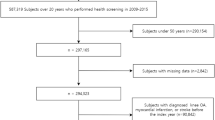
Of 3642 participants, 1676 were included in the analysis. Participants who had not completed the LE8 score (n = 1964) and those who did not have survival information (n = 2) were excluded. Out of 1676 participants, 301 had low CVH, 1136 had moderate CVH, and 239 had high CVH. Finally, 1676 subjects were involved including 1457 survivors and 219 deaths. The screening process is exhibited in Fig. 1.
Characteristics of participants with low CVH, moderate CVH, and high CVH
Of 1676 patients, 301 (17.9%) had low, 1136 (67.8%) had moderate, and 239 (14.3%) had high CVH. Most patients in the total sample, especially those who had high CVH belonged to the non-Hispanic white race (90.2%), had college graduates or above education (65.7%), and above PIR (84.7%). The majority of patients with high CVH were married (73.7%) and had CVD (93.8%). The death rate, especially those who had low CVH was high (15.2%). The percentage of participants with CVD in the low CVH, moderate CVH, and high CVH groups were statistically different (29.36% vs 17.79% vs 6.17%). The percentage of participants receiving OA drugs in the low CVH, moderate CVH, and high CVH groups were statistically different (3.63% vs 1.08% vs 0.71%) (Table 1).
Association between CVH and all-cause mortality in OA patients
In Model 1, compared with low CVH, moderate CVH (HR = 0.63, 95%CI: 0.47–0.85) and high CVH (HR = 0.37, 95%CI: 0.21–0.67) were associated with decreased risk of all-cause mortality in OA patients. In Model 2 a, we found that moderate CVH (HR = 0.62, 95%CI: 0.43–0.89) and high CVH (HR = 0.37, 95%CI: 0.21–0.65) were likely to reduce the risk of all-cause mortality in OA patients. In Model 3 a, lowered risk of all-cause mortality was identified in people with moderate CVH (HR = 0.67, 95%CI: 0.45–0.98) and high CVH (HR = 0.47, 95%CI: 0.26–0.87). The HRs of all-cause mortality in OA patients decreased by 0.12 as per 10-point increase of LE8 score (HR = 0.81, 95%CI: 0.73–0.90) according to the results in Model 3 b (Table 2). Sensitivity analysis revealed that no significant difference was found between the data before and after missing values manipulation (Supplementary Table 3). Sensitivity analysis was also conducted for avoiding overadjustment, and the results were presented in Supplementary Table 4. The sex-specific results were shown in Supplementary Table 5–6.
RCS curve revealed that there was a non-linear association between the LE8 score and the HRs of all-cause mortality (P = 0.343). The HRs of all-cause mortality were decreased with the increase of LE8 score, and participants with LE8 scores of 80 to 100 points presented a lower risk of all-cause mortality than those with LE8 score < 49 points (Fig. 2). The deflection point in the RCS analysis was 64.4, and the mortality rate of patients above and below the deflection point was significantly different (Supplementary Table 7). The LE8 score of all participants were stratified by deflection point in the RCS analysis, and the results delineated that LE8 score ≥ 64.4 was associated with a decreased risk of all-cause mortality (HR = 0.69, 95%CI: 0.51–0.93) (Supplementary Table 8). Sensitivity analysis was performed and adjusted for less confounding factors to avoid overadjustment (Supplementary Table 9). The survival probability of participants in the high CVH group was higher than the moderate CVH group, and the low CVH group (P = 0.002) (Fig. 3).
The modifying effect of OA on the association between LE8 score and all-cause mortality was further estimated. The characteristics of participants with or without OA in different CVH groups were presented in Supplementary Table 10. The percentage of participants with OA who had low CVH was higher than those who had high CVH. Covariates associated with all-cause mortality are shown in Supplementary Table 11. Detailed information on the modifying effect of OA on the association between LE8 score and all-cause mortality in each model was delineated in Supplementary Table 12.
Subgroup analysis of the association between LE8 score and all-cause mortality in OA patients
In patients with OA ≥ 5 years, moderate CVH (HR = 0.57, 95%CI: 0.37–0.88) or high CVH (HR = 0.41, 95%CI: 0.21–0.82) was associated with decreased risk of all-cause mortality in OA patients. A 10-point increase in LE8 score was associated with decreased risk of all-cause mortality in OA patients (HR = 0.79, 95%CI: 0.71–0.87). The risk of all-cause mortality in OA patients was decreased by 0.19 as per a 10-point increase of LE8 score in subjects with CVD (HR = 0.81, 95%CI: 0.68–0.97). In those without CVD, high CVH was correlated with a reduced risk of all-cause mortality (HR = 0.42, 95%CI: 0.22–0.80). The HRs of all-cause mortality in OA patients without CVD decreased as per a 10-point increase in LE8 score (Table 3).
Discussion
The current study investigated the association between CVH status and all-cause mortality in patients with OA. The results revealed that patients with high CVH was correlated with a decreased risk of all-cause mortality in patients with OA. Increased LE8 score was associated with reduced risk of all-cause mortality in OA patients. Subgroup analysis revealed that moderate and high CVH were correlated with decreased risk of all-cause mortality in patients with OA ≥ 5 years, and high CVH was associated with lowered all-cause mortality in OA patients without CVD. The findings provide a reference for the formulation of prognosis improvement strategies for the management of patients with OA.
The importance of dietary diversity as an indicator of nutritional adequacy has been consistently demonstrated in previous studies, and enhancing dietary diversity not only increases the quality of diet but also ensures sufficient intake of essential nutrients [30]. Diet quality was associated with the inflammatory potential, and further predicted the mortality [31]. The correlation between sufficient physical activity and a significant reduction in the risk of subsequent mortality are well-established [32]. Physical activity was previously reported to mitigate the symptoms of OA [33]. The impact of physical activity on the association between the composite dietary antioxidant index and all-cause mortality was modified in the OA population in the United States [34]. The excess mortality among individuals with OA might include reduced levels of physical activity due to involvement of lower limb joints and the presence of comorbid conditions [35]. Nicotine, acting as an exogenous agonist of nicotinic acetylcholine receptors (nAChR) to modulate nAChR expression, induces senescent changes by intervening in multiple pathological molecular pathways [36]. Nicotine exposure was identified to be associated with all-cause mortality, with cohort studies demonstrating that abstaining from smoking was associated with a decreased risk of all-cause mortality compared to current smoking [37]. Lei et al. identified a significant threshold effect of sleep duration on bone mineral density [38]. Evidence revealed that short (< 7 h) or long (> 8 h) habitual sleep duration was correlated with all-cause and CVD-specific mortality [39]. Increased body mass index became more strongly associated with CVD and all-cause mortality [40]. A prospective cohort study among 12.8 million adults demonstrated that total cholesterol was associated with all-cause mortality by sex and age [41]. Higher fasting blood glucose was found to worsen knee symptoms in patients with radiographic knee OA [42]. Blood pressure was associated with knee cartilage volume in patients with knee OA, and correlated with the progression of knee OA [43]. These factors are the components of LE8 score, and the results of these studies provide evidence for the findings in our study. We found that people with LE8 score ≥ 50, representing moderate or high CVH, was associated with decreased risk of all-cause mortality in OA patients. Increased LE8 score, indicating high CVH was associated with reduced risk of all-cause mortality in OA patients.
The LE8 is a scoring system that demonstrates heightened sensitivity to inter-individual differences and places greater emphasis on the social determinants of health and mental well-being [44]. The LE8 score and its components are measured on a continuous scale from 0 to 100, and each component of the score has at least 5 levels allowing each level to have a narrow range of values, which inherently enhances comprehensibility, improves the quantification of CVH at an individual level, and increases the sensitivity in measuring changes in CVH over time both at an individual and population level [45].
In this study, the relationship between LE8 score and the risk of mortality in patients with OA was explored, which provide a reference for the development of relevant strategies to improve the long-term prognosis of patients with OA. For OA patients, maintaining high CVH through the components of LE8 score, such as improving diet quality, increase physical activity level and sleep duration, decrease tobacco exposure, might be helpful for improving the prognosis of OA patients. The sample of this study was obtained from the NHANES database through multi-stage random sampling, which had a good representation of the local population. There were some limitations in this study. Firstly, the information obtained through the questionnaire might be affected by recall bias. Secondly, 2) Due to the limitation of the database, some components of LE8 score were obtained from a single measurement and did not consider the trajectory or changes over time. The association between the changes in CVH and the risk of death in OA patients still needs to be further studied.
Conclusion
The association between CVH and all-cause mortality in patients with OA was evaluated in the current study, which showed that moderate and high CVH was correlated with decreased risk of all-cause mortality in OA patients, and higher CVH was associated with reduced risk of all-cause mortality in OA patients. The findings provide a reference for the formulation of prognosis improvement strategies for the management of patients with OA.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the NHANES database, https://wwwn.cdc.gov/nchs/nhanes/.
Abbreviations
- OA:
-
Osteoarthritis
- AHA:
-
American Heart Association
- LE8:
-
Life’s Essential 8
- CVH:
-
Cardiovascular health
- NHANES:
-
National Health and Nutrition Examination Survey
- CVD:
-
Cardiovascular disease
- NCHS:
-
National Center for Health Statistics
- MECs:
-
Mobile examination centers
- GED:
-
General equivalent diploma
- PIR:
-
Poverty to income ratio
- ANOVA:
-
Analysis of Variance
- RCS:
-
Restricted cubic spline
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
References
Yao Q, Wu X, Tao C, Gong W, Chen M, Qu M, et al. Osteoarthritis: pathogenic signaling pathways and therapeutic targets. Signal Transduct Target Ther. 2023;8:56.
Conditions WHOCr. https://www.who.int/chp/topics/rheumatic/en/. Accessed 22 Jul 2020.
Safiri S, Kolahi AA, Smith E, Hill C, Bettampadi D, Mansournia MA, et al. Global, regional and national burden of osteoarthritis 1990–2017: a systematic analysis of the global burden of disease study 2017. Ann Rheum Dis. 2020;79(6):819–28.
Scheuing WJ, Reginato AM, Deeb M, Acer KS. The burden of osteoarthritis: Is it a rising problem? Best Pract Res Clin Rheumatol. 2023;37:101836.
Foster NE, Eriksson L, Deveza L, Hall M. Osteoarthritis year in review 2022: epidemiology & therapy. Osteoarthritis Cartilage. 2023;31:876–83.
Turkiewicz A, Kiadaliri AA, Englund M. Cause-specific mortality in osteoarthritis of peripheral joints. Osteoarthritis Cartilage. 2019;27:848–54.
Zemedikun DT, Lee H, Nirantharakumar K, Raza K, Chandan JS, Lord JM, et al. Comorbidity phenotypes and risk of mortality in patients with osteoarthritis in the UK: a latent class analysis. Arthritis Res Ther. 2022;24:231.
Büchele G, Günther KP, Brenner H, Puhl W, Stürmer T, Rothenbacher D, et al. Osteoarthritis-patterns, cardio-metabolic risk factors and risk of all-cause mortality: 20 years follow-up in patients after hip or knee replacement. Sci Rep. 2018;8:5253.
Yoshimura N, Muraki S, Oka H, Tanaka S, Kawaguchi H, Nakamura K, et al. Accumulation of metabolic risk factors such as overweight, hypertension, dyslipidaemia, and impaired glucose tolerance raises the risk of occurrence and progression of knee osteoarthritis: a 3-year follow-up of the ROAD study. Osteoarthritis Cartilage. 2012;20:1217–26.
Pitaraki EE. The role of Mediterranean diet and its components on the progress of osteoarthritis. J Frailty Sarcopenia Falls. 2017;2:45–52.
Lo GH, Musa SM, Driban JB, Kriska AM, McAlindon TE, Souza RB, et al. Running does not increase symptoms or structural progression in people with knee osteoarthritis: data from the osteoarthritis initiative. Clin Rheumatol. 2018;37:2497–504.
Roux CH, Coste J, Roger C, Fontas E, Rat AC, Guillemin F. Impact of smoking on femorotibial and hip osteoarthritis progression: 3-year follow-up data from the KHOALA cohort. Joint Bone Spine. 2021;88: 105077.
Parmelee PA, Tighe CA, Dautovich ND. Sleep disturbance in osteoarthritis: linkages with pain, disability, and depressive symptoms. Arthritis Care Res (Hoboken). 2015;67:358–65.
Shan Z, Li Y, Baden MY, Bhupathiraju SN, Wang DD, Sun Q, et al. Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern Med. 2020;180:1090–100.
German C, Makarem N, Fanning J, Redline S, Elfassy T, McClain A, et al. Sleep, sedentary behavior, physical activity, and cardiovascular health: MESA. Med Sci Sports Exerc. 2021;53:724–31.
Elagizi A, Kachur S, Carbone S, Lavie CJ, Blair SN. A review of obesity, physical activity, and cardiovascular disease. Curr Obes Rep. 2020;9:571–81.
Glovaci D, Fan W, Wong ND. Epidemiology of diabetes mellitus and cardiovascular disease. Curr Cardiol Rep. 2019;21:21.
Kostis JB. The importance of managing hypertension and dyslipidemia to decrease cardiovascular disease. Cardiovasc Drugs Ther. 2007;21:297–309.
Lloyd-Jones DM, Allen NB, Anderson CAM, Black T, Brewer LC, Foraker RE, et al. Life’s essential 8: updating and enhancing the American heart association’s construct of cardiovascular health: a presidential advisory from the american heart association. Circulation. 2022;146:e18–43.
Li C, Li Y, Zhao M, Zhang C, Bovet P, Xi B. Using the new “life’s essential 8” metrics to evaluate trends in cardiovascular health among US adults from 2005 to 2018: analysis of serial cross-sectional studies. JMIR Public Health Surveill. 2023;9:e45521.
Messier SP, Mihalko SL, Legault C, Miller GD, Nicklas BJ, DeVita P, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA. 2013;310(12):1263–73.
Rose BJ, Weyand JA, Liu B, Smith JF, Perez BR, Clark JC, et al. Exposure to second-hand cigarette smoke exacerbates the progression of osteoarthritis in a surgical induced murine model. Histol Histopathol. 2021;36(3):347–53.
Zhou S, Wu L, Si H, Li M, Liu Y, Shen B. Association between nighttime sleep duration and quality with knee osteoarthritis in middle-aged and older Chinese: A longitudinal cohort study. Arch Gerontol Geriatr. 2024;118: 105284.
Sampath SJP, Venkatesan V, Ghosh S, Kotikalapudi N. Obesity, metabolic syndrome, and osteoarthritis-an updated review. Curr Obes Rep. 2023;12(3):308–31.
Xiong J, Long J, Chen X, Li Y, Song H. Dyslipidemia might be associated with an increased risk of osteoarthritis. Biomed Res Int. 2020;2020:3105248.
Yi J, Wang L, Guo X, Ren X. Association of life’s essential 8 with all-cause and cardiovascular mortality among US adults: a prospective cohort study from the NHANES 2005–2014. Nutr Metab Cardiovasc Dis. 2023;33:1134–43.
Liu W, Wang J, Wang M, Hou H, Ding X, Ma L, et al. Oxidative stress factors mediate the association between life’s essential 8 and accelerated phenotypic aging: NHANES 2005–2018. J Gerontol Series A, Biological sciences and medical sciences. 2024;79(1):glad240.
Paulose-Ram R, Graber JE, Woodwell D, Ahluwalia N. The National Health and Nutrition Examination Survey (NHANES), 2021–2022: adapting data collection in a COVID-19 environment. Am J Public Health. 2021;111:2149–56.
Liu F, Liu F, Wang H. Association between Life's Essential 8 and rheumatoid arthritis. Clin Rheumatol. 2024;43:2467–77.
Shan Z, Wang F, Li Y, Baden MY, Bhupathiraju SN, Wang DD, et al. Healthy Eating Patterns and Risk of Total and Cause-Specific Mortality. JAMA Intern Med. 2023;183:142–53.
Shivappa N, Godos J, Hébert JR, Wirth MD, Piuri G, Speciani AF, et al. Dietary Inflammatory Index and Cardiovascular Risk and Mortality-A Meta-Analysis. Nutrients. 2018;10:200.
Han L, You D, Ma W, Astell-Burt T, Feng X, Duan S, et al. National trends in American Heart Association Revised Life’s Simple 7 Metrics Associated With Risk of Mortality Among US Adults. JAMA Netw Open. 2019;2: e1913131.
White DK, Jakiela J, Bye T, Aily J, Voinier D. Stepping forward: a scoping review of physical activity in osteoarthritis. J Rheumatol. 2023;50:611–6.
Zhang Y, Duan Z, Lu H, Lu G, Fu Y, Li G, et al. Physical activity modifies the association of the composite dietary antioxidant index with all-cause mortality in the US osteoarthritis population. Front Public Health. 2023;11: 1297245.
Hochberg MC. Mortality in osteoarthritis. Clin Exp Rheumatol. 2008;26:S120–4.
Majdi A, Kamari F, Vafaee MS, Sadigh-Eteghad S. Revisiting nicotine’s role in the ageing brain and cognitive impairment. Rev Neurosci. 2017;28:767–81.
Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco product use among adults - United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69:1736–42.
Lei T, Li M, Qian H, Yang J, Hu Y, Hua L. The effect of sleep on metabolism, musculoskeletal disease, and mortality in the general US population: analysis of results from the national health and nutrition examination survey. JMIR Public Health Surveill. 2023;9: e46385.
Liu TZ, Xu C, Rota M, Cai H, Zhang C, Shi MJ, et al. Sleep duration and risk of all-cause mortality: a flexible, non-linear, meta-regression of 40 prospective cohort studies. Sleep Med Rev. 2017;32:28–36.
Kjøllesdal MKR, Smith GD, Ariansen I, Kinge JM, Degerud E, Næss Ø. The association between BMI and mortality using early adulthood BMI as an instrumental variable for midlife BMI. Sci Rep. 2018;8:11499.
Yi SW, Yi JJ, Ohrr H. Total cholesterol and all-cause mortality by sex and age: a prospective cohort study among 12.8 million adults. Sci Rep. 2019;9:1596.
Chiba D, Ohyama T, Sasaki E, Daimon M, Nakaji S, Ishibashi Y. Higher fasting blood glucose worsens knee symptoms in patients with radiographic knee osteoarthritis and comorbid central sensitization: an Iwaki cohort study. Arthritis Res Ther. 2022;24:269.
Wang Y, Meng T, Ruan G, Zheng S, Zhu J, Cen H, et al. Associations of blood pressure and arterial stiffness with knee cartilage volume in patients with knee osteoarthritis. Rheumatology (Oxford). 2021;60:4748–54.
Correction to: Status of Cardiovascular Health in US Adults and Children Using the American Heart Association's New "Life's Essential 8" Metrics: Prevalence Estimates From the National Health and Nutrition Examination Survey (NHANES), 2013 Through 2018. Circulation. 2022;146:e298.
Shetty NS, Parcha V, Patel N, Yadav I, Basetty C, Li C, et al. AHA Life’s essential 8 and ideal cardiovascular health among young adults. Am J Prev Cardiol. 2023;13:100452.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
TL and CL designed the study. TL wrote the manuscript. YW, TM, QR, and HS collected, analyzed, and interpreted the data. CL critically reviewed, edited, and approved the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The requirement of ethical approval for this was waived by the Institutional Review Board of Binzhou Medical University Hospital, because the data was accessed from NHANES (a publicly available database). The need for written informed consent was waived by the Institutional Review Board of Binzhou Medical University Hospital due to retrospective nature of the study. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, T., Wang, Y., Meng, T. et al. Association between cardiovascular health and all-cause mortality risk in patients with osteoarthritis. BMC Musculoskelet Disord 25, 641 (2024). https://doi.org/10.1186/s12891-024-07729-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07729-y