Abstract
Background
Femoral neck system (FNS) is a new type of internal fixation system which has been widely used for treating femoral neck fractures (FNFs).Compared with other internal fixation methods, FNS is minimally invasive and stable, and often achieves satisfactory short-term efficacy.Early failure of FNS (EFFNS) is not uncommon, however, there are few literatures and reports on factors associated with EFFNS.This study aimed to survey the prevalence and risk factors of EFFNS.
Methods
We retrospectively analysed 62 patients with FNFs and underwent FNS fixation between 2019 and 2021. Demographic data, clinical characteristics, radiographic features and treatment process were described. Multifactor logistic regression analysis was used to analyse the different influencing factors.
Results
Out of the 62 FNFs patients, 10 patients (16.1%) developed EFFNS, including 6 cases of severe femoral neck shortening, 2 cases of screw-out, 1 case of avascular necrosis of the femoral head and 1 case of nonunion. In the failure group, all patients were younger than 65 years old, which was significantly higher than 59.6% in the healing group (P = 0.012). There were no significant differences in sex(P = 0.490), BMI (P = 0.709), injured side (P = 0.312), injury mechanism (P = 0.617), reduction method(P = 0.570),femoral neck-shaft angle(P = 0.545), Pauwels classification (P = 0.564) and Garden classification (P = 0.195). Moreover, we not found that Garden classification (P = 0.464) and age (P = 0.128) were statistically significant risk factors for EFFNS at multivariate analysis.
Conclusion
In this study, sex, BMI, injury side, injury mechanism, reduction method, Pauwels angle, femoral neck-shift angle, Pauwels classification and Garden classification were excluded as EFFNS risk factors. Moreover, our study demonstrated that age and Garden classification were not significant risk factors at multivariate analysis.
Trial registration
ChiCTR, ChiCTR2100051360. Registered on 21 September, 2021. https://www.chictr.org.cn/index.aspx.
Similar content being viewed by others
Introduction
As the population ages, femoral neck fractures (FNFs) are becoming a common injury in middle-aged and elderly people, accounting for approximately 54% of hip fractures [1, 2]. Various approaches to internal fixation such as cannulated compression screws (CCSs) [3], sliding hip screws [4], Hansson pin system [5] and dynamic hip screws (DHSs) [6] have been used for the treatment of FNFs.
However,failure of internal fixation and functional loss after surgery are not uncommon and often lead to rehospitalization or even more serious consequences [7, 8]. Different studies have reported that 7–22% of patients receive secondary operations, mostly due to complications, such as avascular necrosis of the femoral head (ANFH), nonunion, severe femoral neck shortening (SFNS), and screw-out [9, 10]. To reduce postoperative complications, researchers have been committed to innovation of internal fixation methods and devices. In recent years, researchers have developed the femoral neck system (FNS)(DePuy Synthes, USA), which consists of four parts: a barrel plate, a blade, an antirotation screw and a locking screw. The FNS is a novel internal fixation system featuring anti-rotation, anti-sliding, and anti-shearing functions for the treatment of FNFs.
Several studies have reported comparative efficacy between FNS and other internal fixation approaches, suggesting that the short-term efficacy of FNS is satisfactory [11,12,13]. In addition, the literature also reported that early failure of the FNS (EFFNS) occurred after internal fixation of FNFs.The previous literature suggested that there were many risk factors for the failure of internal fixation of FNFs, among which the Garden classification was an important one that has been widely discussed [14, 15]. However, there is a paucity of literature looking at the factors associated with EFFNS in patients with FNFs. Therefore, we assume that the Garden classification is one of the risk factors for EFFNS. In this study, we aimed to investigate the prevalence of EFFNS among patients with FNFs, verify the validity of the hypothesis and identify other risk factors for EFFNS in patients with FNFs.
Materials and methods
Study design
This study was performed at a level-I orthopedic trauma centre from October 2019 to March 2021. A series of patients with a diagnosis of femoral neck fracture were treated operatively using the FNS technique.We conducted a retrospective study of the factors associated with early failure of the femoral neck system (FNS) in these patients with femoral neck fractures.
Inclusion and exclusive criteria
All subjects considered in this study had to be admitted to our trauma unit in the selected period and had undergone operative intervention FNS. The AO/OTA (Albeitgemainshaft fur Osteosynthesisfrag/Orthopaedic Trauma Association) classification was 31-B [16]. Age was 18 years old or older, with no sex limitation. Only patients capable of walking independently or with aid before the trauma and who did not present serious impairment of consciousness were included in the study. Exclusion criteria included pathological fractures, < 6 months of follow-up, postoperative infection, pre-existing femoral head necrosis, developmental dysplasia of the hip, severe hip arthritis, multiple traumatic injuries, and any risk factors that induce ANFH or fracture nonunion, such as long-term hormone application or smoking, and alcohol abuse.
Surgical techniques, postoperative treatment, and rehabilitation programs
All surgeries were performed at our institution by senior orthopedic surgeons. The surgical procedures were based on standard protocols for FNS [17]. Firstly, we insert a 2.5 mm guide pin to maintain fracture reduction.Then, insert a 130° guide pin along the femoral neck as the central guide. Under C-arm fluoroscopy, adjust the insertion point and angle of the guide to ensure it located in the center of the femoral neck in both the anteroposterior and lateral positions. Measure the length and choose the proper implant. Expand the hole along the center guide and insert the bolt-and-plate assembly into the femoral head.Finally, position the anti-rotation screw and locking screw in appropriate location. Antibiotic intravenous prophylaxis was administered with cefazolin 30 min preoperatively and 24 h postoperatively. Patients with stable fractures (Garden type I and II) were allowed partial weight-bearing on the second day postoperatively. Meanwhile, patients with unstable fractures (Garden type III and IV) were allowed to undergo isometric contraction exercises of the quadriceps of the femoris and active and passive flexion and extension training of the ankle joint to reduce oedema of the lower extremities. Low-molecular weight heparin (0.2–0.4 ml, according to the weight of patients) was routinely injected until discharge to prevent deep vein thrombosis. All patients were required to return to the outpatient department for follow-up at 1, 3, and 6 months postoperatively. Partial weight-bearing and full weight-bearing exercises were gradually increased according to the rate of fracture healing on X-ray radiography performed at each visit.
Patient assessment
Two external and independent investigators not involved in the patients' treatment were responsible for data collection. Demographic data, medical history, surgery data and radiographic data at presentation were collected. The following demographic information was recorded: patient age, sex, and body mass index (BMI). BMI (kg/m2) was calculated by dividing weight (kg) by the square of height (m).Medical history included injury mechanism and injury side.The mechanism of injury that can easily cause femoral neck fracture was defined into four categories: fall from standing, road accident, fall from height and others. Surgical information included injury-to-surgery interval and fracture reduction methods (open reduction or closed reduction). Standard preoperative and postoperative anteroposterior and lateral radiographs of the femoral neck were used to evaluate the radiographic features of the patients [18]. The radiographs were analyzed by two independent observers who knew nothing about the outcomes [19]. All FNFs were radiographically classified by the Garden classification [20] and the Pauwels system [21]. The Pauwels angle was defined as the angle between the fracture line and the horizontal plane and measured before surgery [22]. The femoral neck-shaft angle was assessed as the angle between the longitudinal femoral shaft axis and the femoral head-neck axis and measured immediately after surgery [23].
Standard radiographic and clinical follow-up were scheduled at 1, 3, and 6 months postoperatively and continued until fracture healing or until a main complication leading to EFFNS. Complications were defined as ANFH,SFNS, nonunion, and screw-out. ANFH was defined as a cortical collapse of the femoral head, while SFNS was defined as a degree of shortening of the femoral neck greater than 10 mm. The shortening degree was calculated by analysis of the displacement of the screw normalized to the length of the barrel for FNS and described previously by Vazquez et al [13]. Nonunion was defined as the absence of radiographic and clinical signs of fracture healing within 6 months and screw-out as a cut-out of the bolt-and-plate or the antirotation screw or loosening of the locking screw. The cohort was then divided into two groups, depending on the complications leading to failure of the internal fixation or healing of the fracture: failure group and healing group.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation, and categorical variables are expressed as absolute values and percentages. All data were analysed using the Wilcoxon rank sum test (Mann–Whitney U test). Differences in continuous variables were tested using the two-tailed Student’s t-test, and differences in categorical variables were assessed using the Pearson χ2 test or Fisher’s exact test where appropriate. Multifactor logistic regression analysis was used to analyse the different influencing factors. Odds ratios and 95% confidence intervals were calculated. All statistical analyses were carried out using SPSS version 21.0 statistical software (IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp).A P value < 0.05 was regarded as statistically significant.
Results
Patients’ characteristics
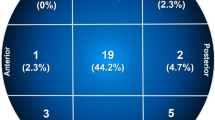
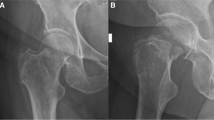
Between 2019 and 2021, 74 consecutive patients with a diagnosis of FNF underwent FNS fixation at our hospital. Twelve of them were excluded based on inclusion and exclusion criteria, leaving 62 patients with a mean age of 56 years (range 20–93 years) who met the inclusion criteria and were analyzed(two groups: failure group [n = 10] versus healing group [n = 52]) (Fig. 1). Patients were followed up for a minimum of 6 months to a maximum of 15 months. The average BMI was 22.7 (range 12.0–30.1). There were 33 right hips and 29 left hips. The sex distribution was 50:50. All patients had successful surgeries. There were 10 cases of EFFNS with 6-month follow-up, accounting for 16.1% of all patients. Ten patients showed pain or dysfunction during the rehabilitation exercise during the follow-up period and came to seek medical treatment. After their physical examination and imaging was reviewed, cases of EFFNS were identified, including 6 cases of SFNS, 1 case of ANFH, 1 case of nonunion, and 2 cases of screw-out (Fig. 2). In terms of treatment options, a total of 5 patients received THA, including 1 case of ANFH, 2 cases of screw-out and 2 cases of SFNS. The other 5 patients (4 cases of SFNS and 1 case of nonunion) chose to continue observation because the symptoms were tolerable.
Preoperative anteroposterior radiograph of a left femoral neck fracture (Garden IV) in a 57-year-old woman (A). Anteroposterior radiograph at 2-month follow-up showing excellent healing and no evidence of femoral head necrosis (B). Anteroposterior radiograph at 6-month postoperatively showing screw-out and femoral head necrosis (C)
There were no significant differences in sex (P = 0.490), BMI (P = 0.709), injury mechanism (P = 0.617), injury-to-surgery interval (P = 0.466) or injury side (P = 0.312). However, in the failure group, all patients were younger than 65 years old. The proportion was significantly higher than 59.6% of the healing group (P = 0.012) (Table 1).
Comparison of surgery and radiographic data
There were no significant differences in reduction methods (P = 0.570), Pauwels angle (P = 0.542), or femoral neck-shaft angle (P = 0.545). No significant differences were observed in terms of Garden classification (P = 0.195) or Pauwels classification (P = 0.564) (Table 2).
Multifactor logistic regression analysis
Multifactor logistic regression analysis indicated that Garden classification (P = 0.464) and age (P = 0.128) were not statistically significant risk factors for the EFFNS (Table 3).
Discussion
Surgical treatment of FNFs mainly comprises closed or open reduction and internal fixation and primary arthroplasty. The internal fixation implants are CCSs, SHSs, DHSs and Hansson pin system, while primary arthroplasty includes total hip arthroplasty (THA) and hemiarthroplasty [24]. Many factors including displacement of the femoral neck, presence of hip osteoarthritis, age, reduction quality, and stable internal fixation affect the surgeon's decision on the surgery method [17].
The ideal implant is considered as a conduct with the characteristics of strong fixation of fractures, prevention of femoral neck shortening, and avoidance of tilting and rotation of the femoral head [25]. The FNS is a newly developed femoral neck internal fixation device in recent years. It contains a bolt, an anti-rotation screw and a femoral lateral plate. This plate has 1 hole or 2 holes for the standard 5.0 mm locking screw. After assembly, the FNS forms a stable structure with an angle of 130° in the femoral neck and femoral shaft. This stable structure combines the advantages of angular stability and minimally invasive surgical techniques, and allows the bolt and anti-rotation screw to slide together in the plate barrel to dynamically compress the fractured end, similar to a DHS. However, the surgical incision for an FNS is smaller than that for a DHS, thereby reducing soft tissue damage and protecting the blood supply. Therefore, FNS is considered the next generation of internal fixation devices for the treatment of FNFs [26]. It combines many advantages, including providing sufficient angular stability, reducing blood supply damage, dynamic compression and anti-rotation.
A few advantages of the FNS are due to its biomechanical characteristics. Fan et al. indicated that the internal fixation stress of FNS was higher than that of CCS in finite element analysis, which is approximately 1.6–3.0 times that of CCS in Pauwels III fractures at 50°, 60°, and 70° [27]. Especially at 70°, the displacement of the double-hole FNS was the smallest in the various groups. A biomechanical loading test conducted by Stoffel et al. evaluated the performance of FNS in comparison with DHS and CCS [28]. The experiment increased at a rate of 0.1 N/cycle until the termination criteria were achieved. The study found that cycles until 15 mm leg shortening and 15 mm femoral neck shortening in FNS were significantly higher than those in CCS. Similarly, Schopper et al. evaluated the biomechanical performance between FNS and Hansson pin systems in models of Pauwels II FNFs [29]. They indicated that the angular stability of the FNS provided superior resistance against varus deformation and performed in a less sensitive way to variations in implant placement.
Several comparative studies have reported the clinical outcomes between FNS and various internal fixations, indicating that the short-term efficacy of FNS is satisfactory [11,12,13, 17, 26]. However, FNS related complications, such as SFNS, ANFH, nonunion or delayed healing, and screw-out, have also been reported in these literature.
A total of 6 patients developed SFNS in this study. One of the characteristics of the FNS is dynamic compression. The precollapsed insertion allows the anti-rotation screw and bolt to slide in the maximum 20 mm packaging to meet femoral neck shortening during fracture healing. Similar to a DHS, femoral neck shortening after FNS placement is also a common phenomenon. The principle of fracture site compression utilized by surgical constructs may promote healing. However, SFNS is associated with worse patient-reported outcomes and objective functional measures. Most studies defined SFNS as a shortening of 10 mm or longer in length. Both the retrospective FAITH trial [30] and the prospective SHOC trial [31] showed that SFNS after internal fixation was associated with inferior functional outcomes. Similarly, Zlowodzki et al. found differences in scores related to the degree of shortening, indicating worse functional outcomes with a greater degree of shortening [32]. Therefore, in this study, half of SFNS patients chose to receive THA, and their function was partially restored after surgery.
In this study, all EFFNSs existed in young and middle-aged patients (under 65 years old). The general treatment strategy for FNFs is widely considered to be that internal fixation is more suitable for young and middle-aged patients, while THA is more suitable for elderly patients with poor physical condition and bone quality. However, this strategy did not form a consensus. A meta-analysis by Xu et al. reviewed 2065 patients with FNFs from 17 case–control studies and found no association between age and osteonecrosis of the femoral head [33]. However, another meta-analysis by Slobogean et al. reviewed 1558 cases of FNFs from 41 studies, indicating that the high total incidence of ANFH in patients under 60 years old was 14.3%, and nonunion was 9.3% [9]. In addition, for elderly patients, the best functional results could be achieved in patients with a well-healed femoral neck without ANFH after urgent reduction and internal fixation of displaced FNFs [34]. Therefore, patient selection and surgical skill were important factors influencing clinical outcomes. We suggest that future studies emphasize the importance of surgical indications in the young and middle-aged patient populations. Furthermore, the promotion of surgical skills is key for avoiding postoperative complications and EFFNS.
Garden classification was an important parameter when considering surgery in FNF patients. There were a few studies supporting the Garden classification as one of the risk factors for ANFH after internal fixation of FNFs [14, 33, 35, 36]. In this study, displaced fractures (Garden III and IV) in the failure group accounted for 90%, while in the healing group, they accounted for only 75%. Although there was no statistical significance, EFFNS may be associated with the high proportion of displaced fractures. However, after regression analysis, we did not find support for Garden classification as a risk factor for EFFNS. The reason may be the short follow-up time (6 months) of this study, and the short-term efficacy of FNS was satisfactory.The good anti-rotation, anti-sliding and anti-shear function of FNS, as well as the reduction of blood supply injury, may reduce the occurrence of early complications of displaced FNF.And long-term clinical outcomes after FNS fixation need to be determined with longer follow-up.All cases during follow-up did not routinely performed MRI examinations but only X-rays.However, the manifestation of ANFH can only be clearly seen on X-rays of Ficat III-IV patients [19], so some ANFH patients in Ficat I-II may be overlooked during outpatient follow-up.Therefore, we recommend that regular review of MRI for early detection and treatment of ANFH.
In addition, we could not find the relationship between EFFNS and sex, BMI, injured side, injury mechanism, reduction method, Pauwels angle, femoral neck-shaft angle, or Pauwels classification.
This study had some limitations. Firstly, it was a single-centre study. Therefore, there must have been some selective bias. Secondly, the small number of enrolled patients can not provide enough information and may result in sample bias. Thirdly,this study did not investigate other possible risk factors, such as weight-bearing time, anatomical classification, posterior tilt, preoperative bone quality and bone mineral density, and length of the screws, that may have significantly affected the prognosis of the patients. Hence, future studies need to be conducted to clarify these issues.
Conclusion
In summary, our study suggests that age and Garden classification were not found significant risk factors at multivariate analysis. Moreover, we cannot determine whether age and Garden classification are independent risk factors for EFFNS in the treatment of FNFs. In this study, sex, BMI, injured side, injury mechanism, reduction method, Pauwels angle, femoral neck-shaft angle, and Pauwels classification were ruled out as correlative risk factors for EFFNS.
Availability of data and materials
The original data of this study are available from the corresponding author for reasonable request.
Abbreviations
- ANFH:
-
Avascular necrosis of the femoral head
- BMI:
-
Body mass index
- CCS:
-
Cannulated compression screws
- DHS:
-
Dynamic hip screws
- EFFNS:
-
Early failure of the femoral neck system
- FNFs:
-
Femoral neck fractures
- FNS:
-
Femoral neck system
- MRI:
-
Magnetic resonance imaging
- SFNS:
-
Severe femoral neck shortening
- THA:
-
Total hip arthroplasty
References
Florschutz A, Langford J, Haidukewych G, Koval K. Femoral neck fractures: current management. J Orthop Trauma. 2015;29(3):121–9.
Cronin PK, Freccero DM, Kain MS, Marcantonio AJ, Horwitz DS, Tornetta P. Garden 1 and 2 femoral neck fractures collapse more than expected after closed reduction and percutaneous pinning. J Orthop Trauma. 2019;33(3):116–9.
Zhang Y, Zhang W, Zhang C. A new angle and its relationship with early fixation failure of femoral neck fractures treated with three cannulated compression screws. Orthop Traumatol Surg Res. 2017;103(2):229–34.
Gupta M, Arya RK, Kumar S, Jain VK, Sinha S, Naik AK. Comparative study of multiple cancellous screws versus sliding hip screws in femoral neck fractures of young adults. Chin J Traumatol. 2016;19(4):209–12.
Kalland K, Aberg H, Berggren A, et al. Similar outcome of femoral neck fractures treated with Pinloc or Hansson Pins: 1-year data from a multicenter randomized clinical study on 439 patients. Acta Orthop. 2019;90(6):542–6.
Siavashi B, Aalirezaei A, Moosavi M, Golbakhsh M, Savadkoohi D, Zehtab M. A comparative study between multiple cannulated screws and dynamic hip screw for fixation of femoral neck fracture in adults. Int Orthop. 2015;39(10):2069–71.
Ceolin C, Bano G, Biz C, et al. Functional autonomy and 12-month mortality in older adults with proximal femoral fractures in an orthogeriatric setting: risk factors and gender differences. Aging Clin Exp Res. 2023;35(5):1063–71.
Bano G, Dianin M, Biz C, et al. Efficacy of an interdisciplinary pathway in a first level trauma center orthopaedic unit: A prospective study of a cohort of elderly patients with hip fractures. Arch Gerontol Geriatr. 2020;86: 103957.
Slobogean GP, Sprague SA, Scott T, Bhandari M. Complications following young femoral neck fractures. Injury. 2015;46(3):484–91.
Bigoni M, Turati M, Leone G, et al. Internal fixation of intracapsular femoral neck fractures in elderly patients: mortality and reoperation rate. Aging Clin Exp Res. 2020;32(6):1173–8.
Hu H, Cheng J, Feng M, Gao Z, Wu J, Lu S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J Orthop Surg Res. 2021;16(1):370.
Nibe Y, Matsumura T, Takahashi T, Kubo T, Matsumoto Y, Takeshita K. A comparison between the femoral neck system and other implants for elderly patients with femoral neck fracture: a preliminary report of a newly developed implant. J Orthop Sci. 2022;27(4):876–80.
Vazquez O, Gamulin A, Hannouche D, Belaieff W. Osteosynthesis of non-displaced femoral neck fractures in the elderly population using the femoral neck system (FNS): short-term clinical and radiological outcomes. J Orthop Surg Res. 2021;16(1):477.
Jo S, Lee SH, Lee HJ. The Correlation between the Fracture Types and the Complications after Internal Fixation of the Femoral Neck Fractures. Hip Pelvis. 2016;28(1):35–42.
Zeng X, Zhan K, Zhang L, et al. The impact of high total cholesterol and high low-density lipoprotein on avascular necrosis of the femoral head in low-energy femoral neck fractures. J Orthop Surg Res. 2017;12(1):30.
Hoffmann R, Haas NP. Femur: proximal. In: Ruedi TP, Murphy WM, editors. AO Principles of Fracture Management. New York: Thieme Medical Publishers; 2001. p. 449–52.
Tang Y, Zhang Z, Wang L, Xiong W, Fang Q, Wang G. Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: a preliminary comparative study. J Orthop Surg Res. 2021;16(1):504.
He C, Lu Y, Wang Q, et al. Comparison of the clinical efficacy of a femoral neck system versus cannulated screws in the treatment of femoral neck fracture in young adults. BMC Musculoskelet Disord. 2021;22(1):994.
Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br 1985;67(1):3–9.
Garden RS. Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br. 1961; 43-B:647–63.
Pauwels F. Atlas zur Biomechanik der gesunden und kranken Hüfte. Berlin: Springer; 1973.
Nandi S. Revisiting Pauwels’ classification of femoral neck fractures. World J Orthop. 2021;12(11):811–5.
Yang F, Zhang Z, Zhang X, Huang H, Wang J. Femoral neck-shaft angle can predict the anterior capsular thickness in patients with femoracetabular impingement syndrome. Knee Surg Sports Traumatol Arthrosc. 2023;31(7):2716–20.
Health I, Bhandari M, Einhorn TA, et al. Total Hip Arthroplasty or Hemiarthroplasty for Hip Fracture. N Engl J Med. 2019;381(23):2199–208.
Zlowodzki M, Jönsson A, Paulke R, Kregor PJ, Bhandari M. Shortening after femoral neck fracture fixation: is there a solution? Clin Orthop Relat Res. 2007;461:213–8.
Zhou XQ, Li ZQ, Xu RJ, et al. Comparison of Early Clinical Results for Femoral Neck System and Cannulated Screws in the Treatment of Unstable Femoral Neck Fractures. Orthop Surg. 2021;13(6):1802-9.
Fan Z, Huang Y, Su H, Jiang T. How to choose the suitable FNS specification in young patients with femoral neck fracture: A finite element analysis. Injury. 2021;52(8):2116–25.
Stoffel K, Zderic I, Gras F, et al. Biomechanical Evaluation of the Femoral Neck System in Unstable Pauwels III Femoral Neck Fractures: A Comparison with the Dynamic Hip Screw and Cannulated Screws. J Orthop Trauma. 2017;31(3):131–7.
Schopper C, Zderic I, Menze J, et al. Higher stability and more predictive fixation with the Femoral Neck System versus Hansson Pins in femoral neck fractures Pauwels II. J Orthop Transl. 2020;24:88–95.
Felton J, Slobogean GP, Jackson SS, et al. Femoral Neck Shortening After Hip Fracture Fixation Is Associated With Inferior Hip Function: Results From the FAITH Trial. J Orthop Trauma. 2019;33(10):487–96.
Slobogean GP, Stockton DJ, Zeng BF, Wang D, Ma B, Pollak AN. Femoral neck shortening in adult patients under the age of 55 years is associated with worse functional outcomes: Analysis of the prospective multi-center study of hip fracture outcomes in China (SHOC). Injury. 2017;48(8):1837–42.
Zlowodzki M, Brink O, Switzer J, et al. The effect of shortening and varus collapse of the femoral neck on function after fixation of intracapsular fracture of the hip: a multi-centre cohort study. J Bone Joint Surg Br. 2008;90(11):1487–94.
Xu JL, Liang ZR, Xiong BL, et al. Risk factors associated with osteonecrosis of femoral head after internal fixation of femoral neck fracture:a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20(1):632.
Iorio R, Healy W, Lemos D, Appleby D, Lucchesi C, Saleh K. Displaced femoral neck fractures in the elderly: outcomes and cost effectiveness. Clin Orthop Relat Res. 2001;383:229–42.
Wang T, Sun JY, Zha GC, Jiang T, You ZJ, Yuan DJ. Analysis of risk factors for femoral head necrosis after internal fixation in femoral neck fractures. Orthopedics. 2014;37(12):e1117–23.
Biz C, Tagliapietra J, Zonta F, Belluzzi E, Bragazzi NL, Ruggieri P. Predictors of early failure of the cannulated screw system in patients, 65 years and older, with non-displaced femoral neck fractures. Aging Clin Exp Res. 2020;32(3):505–13.
Acknowledgements
We thank the database administrator Ms. Lihong Zhao for data extraction.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
Chen L designed the study, analysed the study data, drafted the manuscript. Jiang JB, Ma H and Duan X corrected the study data and searched the relevant literature. Chen JL revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Biomedical Research Ethical Committee of West China Hospital of Sichuan University. (Date: September 10, 2021/No. 2021–1115). Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, L., Jiang, J., Ma, H. et al. Factors associated with early failure of the femoral neck system (FNS) in patients with femoral neck fractures. BMC Musculoskelet Disord 24, 912 (2023). https://doi.org/10.1186/s12891-023-06994-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06994-7