Abstract
Introduction
The recently developed femoral neck system (FNS) for treatment of femoral neck fractures (FNF), comprises theoretical biomechanical advantages compared to other implants. The aim of this study was to validate the safety and to report outcomes of patients treated with the FNS.
Method
A retrospective multicentric analysis of patients treated by FNS with a minimum of three months of follow-up. Details analysed from three medical centres were operative duration, estimated blood loss, initial hospitalisation duration, fixation quality as well as complications and reoperation rate. Patients who had revision surgery were compared to all other patients to identify risk factors for failure. In addition, a literature review was performed to analyse data on FNS clinical implementation and patient’s outcomes. The two data sets were combined and analysed.
Results
One-hundred and two patients were included in this study cohort with an average follow-up of seven months (range 3–27). Ten papers were included in the literature review, reporting data on 278 patients. Overall, 380 patients were analysed. Average age was 62.6 years, 52% of the fractures were classified as Gardens 1–2. Overall, the revision rate was 9.2% (14 patients diagnosed with cut-out of implant, 10 with AVN, 8 with non-union and 8 with hardware removal). For the 102 patients in the cohort risk factors for reoperation included patients age, surgeon seniority and inadequate placement of the implant.
Conclusion
This study shows that FNS is a safe treatment option for FNF. Intra-operative parameters and failure rates are comparable to previously reported rates for this implant and other frequently used implants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Femoral neck fractures (FNF) are common and account for over 50% of all hip fractures [1]. Standard treatment for FNF is surgical. The surgical treatment can be either internal fixation or arthroplasty, depending on bone quality, fracture severity and patient’s age [2]. Over the past decades, great effort has been put into deciphering specific biomechanical characteristics of FNF to develop an optimised fixation construct [3]. The recently developed femoral neck system (FNS), (DePuy Synthes, Raynham, MA, USA) comprises the theoretical mechanical advantages of combining compression and anti-rotation qualities during internal fixation. The effective solution the FNS design provides, involves the screw-plate construct, allowing stronger fixation, as well as a combination of blade and anti-rotation screw, that improves axial and rotational stability. Biomechanical studies have shown axial and rotational stability superiority of FNS implant over the traditional cannulated screws (CS) and the dynamic hip screw (DHS) [4, 5]. In addition, the FNS is relatively a minimally invasive procedure which theoretically reduces blood loss and infection risk.
There are only few reports discussing the clinical implementation of FNS [6,7,8,9,10,11,12,13,14,15]. Studies are retrospective in nature and include small number of patients. Surgical workflow and surgeons experience operating with this implant were not evaluated. Moreover, intraoperative parameters such as duration of surgery and blood loss have not been fully explored. In addition, medium- and long-term patient’s outcomes, with relation to re-operation, mechanical failure and avascular necrosis (AVN) rates, are inconclusive.
While the FNS has mechanical superiority over the traditional implants in cadaveric experiments, it is crucial to evaluate the safety and report outcomes of this new implant.
The aim of this study therefore was to investigate the outcome of patients with FNF managed with FNS in our institutions and in the published literature. Moreover, we wish to validate the safety of this implant, and compare the outcome of patients treated with FNS to other implants. Our hypothesis was that the FNS implant would demonstrate if not better, analogous results to similar implants used for fixation of FNFs.
More specifically, the study’s objectives were as follows:
-
1.
Analyse data obtained from three medical centres on patient treated by FNS regarding the operative duration, estimated blood loss and initial hospitalisation duration.
-
2.
Assess patients’ medium- and long-term outcomes regarding AVN, mechanical failure, re-operation rates and the associated risk factors.
-
3.
Perform literature review and analyse data reported on FNS clinical implementation and patient’s outcomes.
-
4.
Compare the data collected on FNS to other implants published outcome and peri-operative parameters.
Patients and methods
Data on FNF patients treated with FNS from three different medical centres, between 01 March 2019 and 01 August 2021, was retrospectively collected and analysed. Institutional review board approval, from all institutes participating in the study, was obtained. Inclusion criteria for the study were patients with FNF treated with FNS and a minimum of three month post-operative follow-up. Exclusion criteria were open fractures, evidence of pathological fracture, skeletally immature patients and revision procedure for a failed fixation. Data was collected from electronic records of each institution and included patients’ demographics and recorded comorbidities. Comorbidities were defined as six distinct categories: cardiac, neurological, chronic kidney disease, chronic lung disease, diabetes mellitus and active malignancy. Data on the initial hospitalisation was collected regarding time from admission to surgery and length of hospital stay. In addition, operation time, estimated operative blood loss, which was estimated by the surgeon at the end of the procedure and surgeon seniority, qualified orthopaedic surgeon versus a trainee were recorded. Quality of reduction was evaluated by radiographic measurements performed on initial postoperative radiographs. Measurement of the tip apex distance (TAD) [16] and Parker ratio [17] in the anterior posterior and lateral radiographs was obtained. The rationale to add the Parkers ratio was that this measurement evaluates the importance of the position of the blade in the neck and not only the position of the tip of the blade.
Fracture classification and the radiographic measurements were performed by two of the authors. Fractures were classified according to the Garden classification [18]. Fractures were considered stable if classified as types 1 and 2 and unstable for types 3 or 4.
Treatment outcome for all patient was evaluated by collecting data from the follow-up records on, follow-up duration, reports of mechanical failure of implant (cut-out), nonunion (defined as no sign of union six months after surgery) and re-operations. Re-operated patients were evaluated for the diagnostic reason for the reoperation, time interval from primary surgery and the secondary procedure performed. Patients in the cohort were divided into two groups: group (1) underwent re-operation and group (2) did not require additional surgical procedure. Groups were compared for patients’ factors (demographics and comorbidities), fracture classification and surgical procedure-related collected data in order to evaluate specific risk factors for re-operation.
Data was collected from centres which had different implants for treatment of FNF. At one centre, FNS was the only construct used for FNF fixation, whereas at the other two centres either FNS, DHS or CS were applied for internal FNF fixation. The decision which implant to use was taken by the senior surgeon. Generally, elderly patients (aged above 65) suffering from a displaced fracture (Gardens 3–4), were treated by arthroplasty, whereas younger patients were treated by internal fixation, regardless to the displacement rate of the fracture, in all centres.
Systematic review of the literature
The medical search engine employed in this study was PubMed; medical subject headings words used included FNS, femoral neck system and femur fractures. Articles reporting on FNS clinical outcomes were collected and analysed. Inclusion criteria were papers reporting on patients treated with FNS for FNF which were published in English. Case reports, biomechanical studies and non-English publications were excluded. When available, data obtained in the literature review was collected for the variables described above.
For the statistical analysis of this study, contingency data were analysed using two-tailed χ2 test or Fisher exact test, as appropriate. Continuous variables were compared using the Student’s t test.
In the systematic literature review section, literature mean numbers were calculated as weighted means, according to each sample size proportion out of all.
Results
One hundred twenty-five patients treated with FNS were collected from three medical centres. However, twenty-three were excluded as they did not have at least three months of post-operative follow-up. In total, 102 patients (53 male) with a mean age of 62.9 years were included in this study. Data on demographics, fracture classification, surgical time, estimated blood loss, initial hospitalisation duration and patient comorbidities is presented in Table 1. The average follow-up was seven months (range 3 to 27). Nine patients underwent revision surgery, out of which five were due to a failure of fixation and cut-out of the blade, three due to AVN and one as a result of fracture nonunion. All patients who required re-operation were treated by hip arthroplasty. The average time interval from the initial surgery to the revision surgery was 18 weeks, ranging from two to 36 weeks. Two patients were diagnosed with AVN by magnetic resonance imaging (MRI) but did not require surgical treatment as they were diagnosed with low-grade AVN stage and had minor clinical symptoms at their last follow-up examination. One patient, 93-year-old male, was diagnosed with mechanical failure of the implant (cut-out) six weeks post- operation. This patient was bedridden before the operation and suffered from major comorbidities, therefore he was treated non-operatively.
Results comparing patients who underwent revision surgery (9) to all other patients (93) are presented in Table 2. Significant differences between the two groups were patient age, surgeon seniority and fixation quality assessed by radiographic measurements of the Lateral Parker ratio. No correlation to fracture stability was found.
Literature review revealed 16 articles which provided data on FNS-treated patients, however, six were excluded (two were written in Chinese [19, 20], three were biomechanical articles [4, 5, 21] and one was a technical note [22]). From the ten eligible articles [6,7,8,9,10,11,12,13,14,15], data on 278 patients treated with FNS was collected and included in the final analysis. Table 3 summarises the number of patients, inclusion criteria, follow-up period, complications, re-operations rate and the main conclusions of the included articles. Data on demographics, fracture classification, surgical time, estimated blood loss, initial hospitalisation duration, follow-up duration and patient-reported comorbidities of the 278 patients described in the literature is presented in Table 1. In addition, cumulative analysis on the above variables for all 380 patients treated with FNS (102 patients described in this study and 278 from the literature review), is presented in Table 1. Finally, data regarding postoperative complications requiring revision surgery from the literature review and the 102 patients included in this paper is summarised and presented in Table 1.
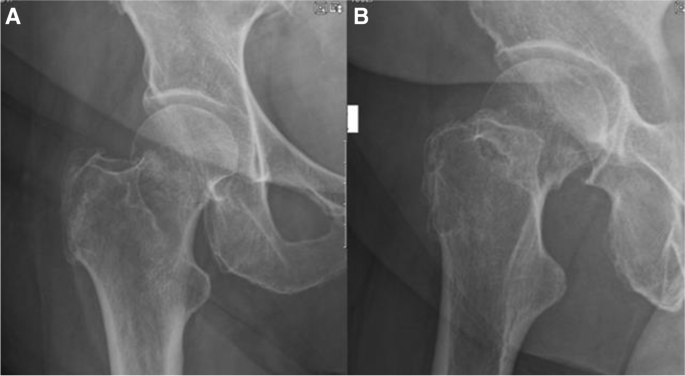
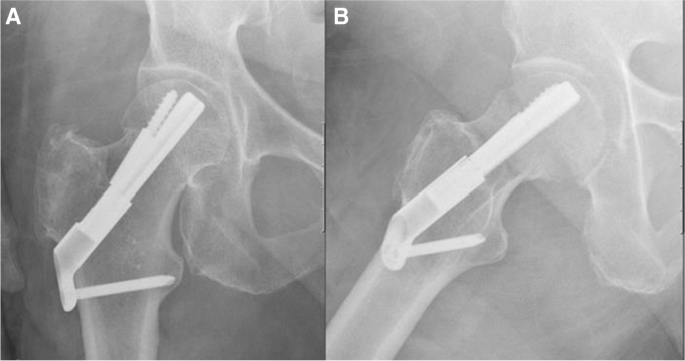
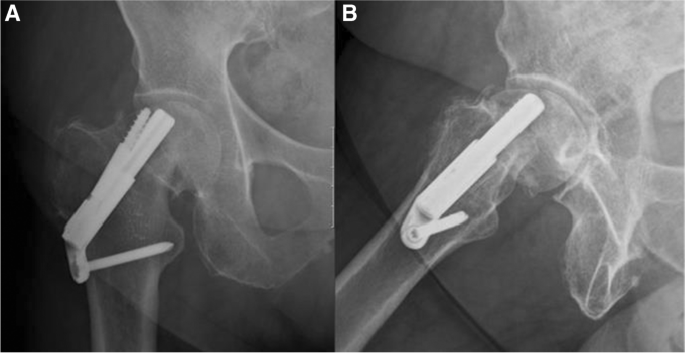
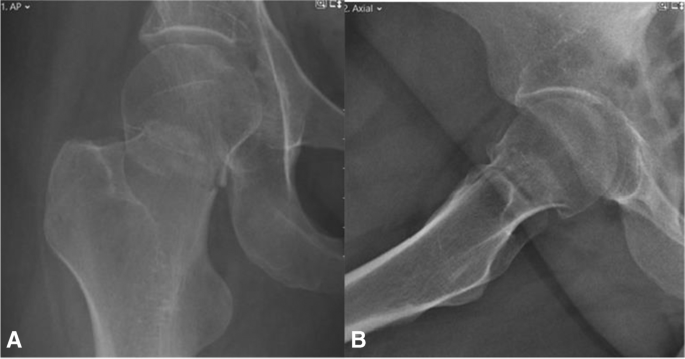
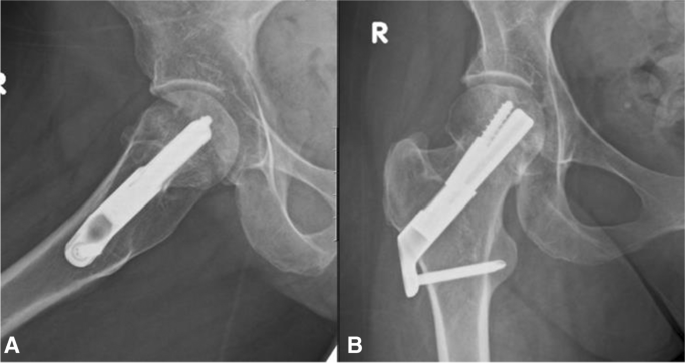
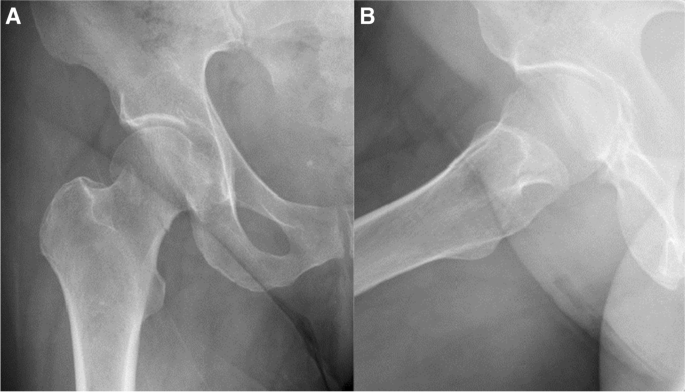
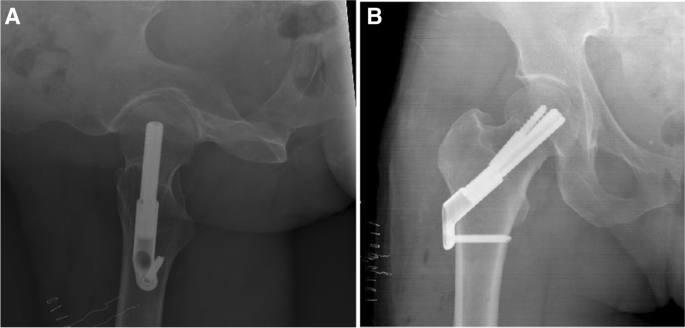
Radiographs and descriptions of three different patients from this study cohort are presented in Figs. 1, 2, 3, 4, 5, 6, 7, 8, 9.
A, B AP and lateral radiographs 6 weeks after the surgical treatment. Radiographs demonstrate failure of fixation, cut-out of the implant. After the initial surgery, the patient was discharged home with instruction to full weight bear on the operated leg and was referred for physiotherapy treatment. Patient suffered from progressive hip pain and limp, walked short distance with the aid of a Zimmer frame. She was treated with revision surgery, hemiarthroplasty of the right hip
Discussion
In this study, we present data regarding 102 patients treated with FNS, and this represents the largest number of patients reported in literature to date. Adding data from previous publications enable us to analyse 380 patients treated with FNS. This study shows that FNS is a safe treatment option for FNF. Intraoperative parameters and clinical outcome of patients treated with FNS are comparable to those observed in other frequently used implants for fixation of FNF [23, 24].
Reported reoperation rates of FNF vary; 8% for non-displaced fractures and up to 42% in displaced fractures have been reported [25,26,27]. In the FAITH study [24], a large randomised control study of FNF treated by different fixation constructs, the reoperation rate was 21%. Re-operation rate for all patients treated with FNS analysed in this study was 9.2%. In the literature review, one study showed reduced reoperation rate in the FNS group in comparison to the alternative implant [9]; in contrast, all other studies showed similar re-operation rates. The average follow-up period for this study was seven months (range 3–27). The relatively short follow-up period can be explained by the fact that the FNS was released only in 30 January 2019, and since then, it has been gradually used in our institutes. Generally, the majority of the reoperations of FNF occur in the first 12 months, in particular, re-operations related to fracture nonunion. The low number of nonunions, 1% (1/102), shown in our cohort, is an important finding and might reflect the biomechanical advantages of this implant. Longer follow-up would be ideal for exploring reoperation rates of FNFs. However, we believe that providing failure rates of a new implant, even before the desirable follow-up duration, can still provide useful information to both patients and clinicians.
Our study investigated intraoperative parameters of patients treated with FNS. The average operative time was 44 (range 21–95) minutes. This operative time is not dissimilar to other reported operative times for similar implants such as the Targon FN being 56 minutes [23]. Interestingly, three studies showed significant shorter operative time in the FNS group compared to the alternative implant [8, 9, 12]. One might have expected that a new implant would require longer operative time. The reported short operative time can be attributed to the low number of surgical steps in FNS which enhances procedural efficiency.
The average estimate blood loss for the FNS procedure was 47 (ml), an estimate, which is in the lower reported range for similar procedures. Fox et al. reported median intra-operative blood loss of 50 (ml) for CS and 200 (ml) for HA and DHS [28]. Other intra/peri-operative parameters which were reported for the FNS are reduced radiation exposure [7, 14, 15], shorter operation time [8, 9, 12, 14, 15], reduced initial hospitalisation and nonsurgical complication rate such as urinary tract infection and pneumonia [6, 7], reduced femoral neck shortening [8, 11, 14] and improved functional outcome (Harris hip score) [11, 14]. All these parameters demonstrate that the FNS is a relatively minimally invasive and operator-friendly implant.
Several predisposing factors are related to fixation failure in FNF, including female sex, increased BMI, older age, fracture type and suboptimal fracture reduction and implant positioning [24]. One of the objectives of this study was to identify risk factors for re-operation in patients treated with FNS. Our study found that patient’s age, surgeons’ seniority and precise surgical placement of implants were factors which affected the rate of re-operations. Only one other study evaluated risk factors for failure in patients treated with FNS and found patient age and presence of chronic lung disease as risk factors [10].
One of the limitations of this study is the short follow-up period. A longer follow-up period is necessary to effectively evaluate outcomes of FNF, preferably at 24 months. In addition, a larger cohort would enable assessment of the different fracture’s subgroups, displaced and non-displaced, and different patients age groups. A multi-centre randomised control study, with a long follow-up period, would be desirable to provide solid conclusions regarding the potential superiority of this implant in relation to the alternative treatment choices.
In conclusion, our hypothesis that the FNS implant would demonstrate analogous results to similar implants used for fixation of FNFs was confirmed. This study supports the view that FNS is a safe treatment option for FNF as shown in previously published literature.
Data availability
Raw data were generated from electronical records of the participating medical centres. Derived data supporting the findings of this study are available from the corresponding author [A.D] on request.
References
Physicians RCo (2017) National hip fracture database (NHFD) annual report 2017. In. RCP London.
Zelle BA, Salazar LM, Howard SL, Parikh K, Pape HC (2022) Surgical treatment options for femoral neck fractures in the elderly. Int Orthop. https://doi.org/10.1007/s00264-022-05314-3
Panteli M, Rodham P, Giannoudis PV (2015) Biomechanical rationale for implant choices in femoral neck fracture fixation in the non-elderly. Injury 46:445–452
Stoffel K, Zderic I, Gras F, Sommer C, Eberli U, Mueller D, Oswald M, Gueorguiev B (2017) Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: a comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma 31:131–137
Schopper C (2018) Biomechanical evaluation of the femoral neck fracture fixation technique with the new implant FNS in comparison to DHS Blade. Universität Ulm, DHS Screw with antirotation screw and Three Cannulated Screws. In
Cintean R, Pankratz C, Hofmann M, Gebhard F, Schutze K (2021) Early results in non-displaced femoral neck fractures using the femoral neck system. Geriatr Orthop Surg Rehabil 12:21514593211050150. https://doi.org/10.1177/21514593211050153
He C, Lu Y, Wang Q, Ren C, Li M, Yang M, Xu Y, Li Z, Zhang K, Ma T (2021) Comparison of the clinical efficacy of a femoral neck system versus cannulated screws in the treatment of femoral neck fracture in young adults. BMC Musculoskelet Disord 22:994. https://doi.org/10.1186/s12891-021-04888-0
Hu H, Cheng J, Feng M, Gao Z, Wu J, Lu S (2021) Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J Orthop Surg Res 16:370. https://doi.org/10.1186/s13018-021-02517-z
Nibe Y, Matsumura T, Takahashi T, Kubo T, Matsumoto Y, Takeshita K (2021) A comparison between the femoral neck system and other implants for elderly patients with femoral neck fracture: a preliminary report of a newly developed implant. J Orthop Sci. https://doi.org/10.1016/j.jos.2021.04.016
Stassen RC, Jeuken RM, Boonen B, Meesters B, de Loos ER, van Vugt R (2021) First clinical results of 1-year follow-up of the femoral neck system for internal fixation of femoral neck fractures. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04216-0
Tang Y, Zhang Z, Wang L, Xiong W, Fang Q, Wang G (2021) Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: a preliminary comparative study. J Orthop Surg Res 16:504. https://doi.org/10.1186/s13018-021-02659-0
Vazquez O, Gamulin A, Hannouche D, Belaieff W (2021) Osteosynthesis of non-displaced femoral neck fractures in the elderly population using the femoral neck system (FNS): short-term clinical and radiological outcomes. J Orthop Surg Res 16:477. https://doi.org/10.1186/s13018-021-02622-z
Zhou XQ, Li ZQ, Xu RJ, She YS, Zhang XX, Chen GX, Yu X (2021) Comparison of early clinical results for femoral neck system and cannulated screws in the treatment of unstable femoral neck fractures. Orthop Surg 13:1802–1809. https://doi.org/10.1111/os.13098
Zhang YZ, Lin Y, Li C, Yue XJ, Li GY, Wang B, Wang YQ, Zhu ZQ (2022) A comparative analysis of femoral neck system and three cannulated screws fixation in the treatment of femoral neck fractures: a six-month follow-up. Orthop Surg. https://doi.org/10.1111/os.13235
Niemann M, Braun KF, Ahmad SS, Stöckle U, Märdian S, Graef F (2022) Comparing perioperative outcome measures of the dynamic hip screw and the femoral neck system. Medicina (Kaunas) 58. https://doi.org/10.3390/medicina58030352
Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM (1995) The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. JBJS 77
Pervez H, Parker MJ, Vowler S (2004) Prediction of fixation failure after sliding hip screw fixation. Injury 35:994–998. https://doi.org/10.1016/j.injury.2003.10.028
Garden RS (1961) Low-angle fixation in fractures of the femoral neck. The Journal of Bone and Joint Surgery British 43:647–663
Yan C, Wang X, Xiang C, Jiang K, Li Y, Chen Q, Deng C, Chen L (2021) Comparison of effectiveness of femoral neck system and cannulate compression screw in treatment of femoral neck fracture in young and middle-aged patients. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 35:1286–1292. https://doi.org/10.7507/1002-1892.202103099
Yang J, Zhou X, Li L, Xu L, Zhu W, Xu W, Xia R, Wang X, Wang G, Hua X, Xu X, Fang S (2021) Comparison of femoral neck system and inverted triangle cannulated screws fixations in treatment of Pauwels typle III femoral neck fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 35:1111–1118. https://doi.org/10.7507/1002-1892.202102046
Fan Z, Huang Y, Su H, Jiang T (2021) How to choose the suitable FNS specification in young patients with femoral neck fracture: a finite element analysis. Injury 52:2116–2125. https://doi.org/10.1016/j.injury.2021.05.043
Cha Y, Song J-U, Yoo J-I, Park KH, Kim J-T, Park CH, Choy W-S (2021) Improved control over implant anchorage under the use of the femoral neck system for fixation of femoral neck fractures: a technical note. BMC Musculoskelet Disord 22:1–8
Parker MJ, Stedtfeld HW (2010) Internal fixation of intracapsular hip fractures with a dynamic locking plate: initial experience and results for 83 patients treated with a new implant. Injury 41:348–351. https://doi.org/10.1016/j.injury.2009.09.004
Nauth A, Creek AT, Zellar A, Lawendy A-R, Dowrick A, Gupta A, Dadi A, van Kampen A, Yee A, de Vries AC (2017) Fracture fixation in the operative management of hip fractures (FAITH): an international, multicentre, randomised controlled trial. The Lancet 389:1519–1527
Rogmark C, Carlsson A, Johnell O, Sernbo I (2002) A prospective randomised trial of internal fixation versus arthroplasty for displaced fractures of the neck of the femur. Functional outcome for 450 patients at two years. J Bone Joint Surg Br 84:183–188. https://doi.org/10.1302/0301-620x.84b2.11923
Frihagen F, Nordsletten L, Madsen JE (2007) Hemiarthroplasty or internal fixation for intracapsular displaced femoral neck fractures: randomised controlled trial. BMJ 335:1251–1254. https://doi.org/10.1136/bmj.39399.456551.25
Oñativia IJ, Slullitel PA, Diaz Dilernia F, Gonzales Viezcas JM, Vietto V, Ramkumar PN, Buttaro MA, Piuzzi NS (2018) Outcomes of nondisplaced intracapsular femoral neck fractures with internal screw fixation in elderly patients: a systematic review. Hip Int 28:18–28. https://doi.org/10.5301/hipint.5000532
B. FN, H. K (2006) Hidden blood loss after surgery for hip fracture. The Journal of Bone and Joint Surgery British volume 88-B:1053–1059. https://doi.org/10.1302/0301-620x.88b8.17534
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This research study was conducted retrospectively from data obtained for clinical purposes. We consulted extensively with the IRB of SZMC and Asaf Harofeh medical centre who determined that our study did not need ethical approval. An IRB official waiver of ethical approval was granted from the IRB of SZMC, Asaf Harofeh medical centres (013–22-SZMC, ASF-0316–20).
Consent to participate
This is a retrospective anonymised data collecting data on patients treated for a common injury; the identity of the patients cannot be revealed. The ethic committee of the participating canters exempt this study form the need to obtain consent to participate.
Consent for publication
In this study, there is an X-ray image of one of the patients from the study cohort. This image purpose is to describe and visualise the paper subject. The X ray image is anonymised, and there is no concerns that the identity of this patient would be revealed. Following this journal instructions, there is no need in this case to perform informed consent from this specific patient.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Davidson, A., Blum, S., Harats, E. et al. Neck of femur fractures treated with the femoral neck system: outcomes of one hundred and two patients and literature review. International Orthopaedics (SICOT) 46, 2105–2115 (2022). https://doi.org/10.1007/s00264-022-05414-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05414-0