Abstract
Background
Posterior shoulder dislocations are rare injuries that are often missed on initial presentation. Cases left untreated for more than three weeks are considered chronic, cannot be reduced closely (they become locked) and are usually associated with a significant reverse Hill-Sachs defect. The aim of this study was to evaluate the outcomes of chronic locked posterior shoulder dislocations treated with the McLaughlin procedure (classic or modified).
Methods
This retrospective study included 12 patients with chronic locked posterior shoulder dislocation operated on between 2000 and 2021 by two surgeons in two institutions. Patients received a thorough clinical examination and radiological assessment before and after surgery. Shoulders were repaired with the McLaughlin or modified McLaughlin procedure. Outcomes were assessed by comparing pre- and postoperative values of clinical variables.
Results
Most of the dislocations were of traumatic origin. The average delay between dislocation and surgical reduction was 13.5 ± 9.7 weeks. Postoperative clinical outcomes were favourable, with an average subjective shoulder value of 86.4 ± 11.1 and a normalized Constant –Murley score of 90 ± 8.3. None of the patients had a recurrence of shoulder dislocation, but one patient developed avascular necrosis of the humeral head and two patients developed glenohumeral osteoarthritis.
Conclusions
In this group of patients with chronic locked posterior shoulder dislocation, the clinical outcomes of McLaughlin and modified McLaughlin procedures were satisfactory, even when surgery was significantly delayed.
Similar content being viewed by others
Background
Posterior shoulder dislocation is a rare injury, accounting for just 2 to 5% of all shoulder dislocations [1,2,3]. The most common causes are convulsions (epileptic, hypoglycaemic or drug withdrawal), trauma and electric shocks [3, 4]. A significant percentage (50–79%) of posterior shoulder dislocations are missed on initial presentation [5]. Thorough clinical examination is crucial and usually shows flattening of the anterior shoulder, a prominent coracoid process, severely limited external rotation and reduced abduction [6]. True anteroposterior and axillary or scapular Y radiographic views of the affected shoulder are also required. Several diagnostic signs (light bulb, vacant glenoid, double trough, rim) have been described on anteroposterior radiographs [5, 7].
Posterior shoulder dislocations are associated in 30 to 90% of cases [8] with an osteochondral impression fracture of the anteromedial part of the humeral head called a reverse Hill-Sachs lesion (RHSL) [9]; however, the term posterior shoulder fracture-dislocation is usually only used in cases (about one third [10]) with fractures of the humeral neck or the tuberosities [11]. Alternatively, Robinson et al. [12] have suggested referring to the latter as "complex" fracture-dislocations, as opposed to "simple" fracture-dislocations involving only an impression fracture (RHSL).
Computed tomography (CT) is required to evaluate the RHSL and other associated fractures and for preoperative planning. Irreducible dislocations with an RHSL are called "locked" or "fixed" [5], and cases neglected for more than three weeks are considered "chronic" [4]. Reverse Hill-Sachs lesions continue to grow while the shoulder remains dislocated [13].
The choice of procedure and prognosis depend on the time to surgery, the size of the RHSL and the possible presence of glenohumeral osteoarthritis. Conservative treatment can be effective in promptly diagnosed cases with stable shoulders and minor bone defects (less than 25% of the articular surface) after closed reduction [6]. Locked posterior shoulder dislocations with an RHSL involving 25–40% of the articular surface can be repaired by transposition of the subscapularis muscle (McLaughlin procedure) [14, 15], lesser tuberosity transposition (Hawkins et al.’s modified McLaughlin procedure) [15,16,17], a modified McLaughlin procedure augmented with an autograft from the iliac crest [18], reconstruction of the humeral head defect using an allograft [19, 20], rotational osteotomy of the humerus [21, 22] or posterior bone block [23]. Cases in which the RHSL involves more than 40% of the articular surface are usually treated by shoulder replacement surgery, either hemiarthroplasty [24], anatomic total shoulder arthroplasty [24, 25], or reverse total shoulder arthroplasty [26].
The purpose of this study was to evaluate the outcomes of open reduction and stabilisation of chronic locked posterior shoulder dislocations using the McLaughlin or modified McLaughlin procedure.
Methods
Study design
This was a retrospective investigation of twelve patients with chronic locked posterior shoulder dislocations operated on between 2000 and 2021 by two surgeons (LNJ and EGH) in two institutions (Hôpital Privé Jean Mermoz, Lyon, France and Foișor Orthopaedic Hospital, Bucharest, Romania).
Pre- and postoperative data
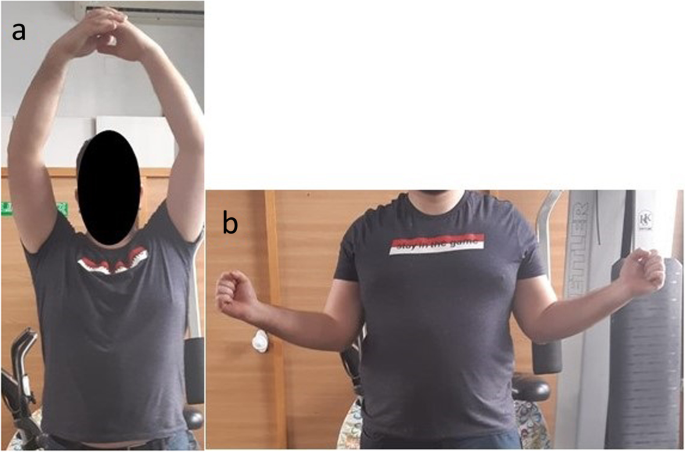
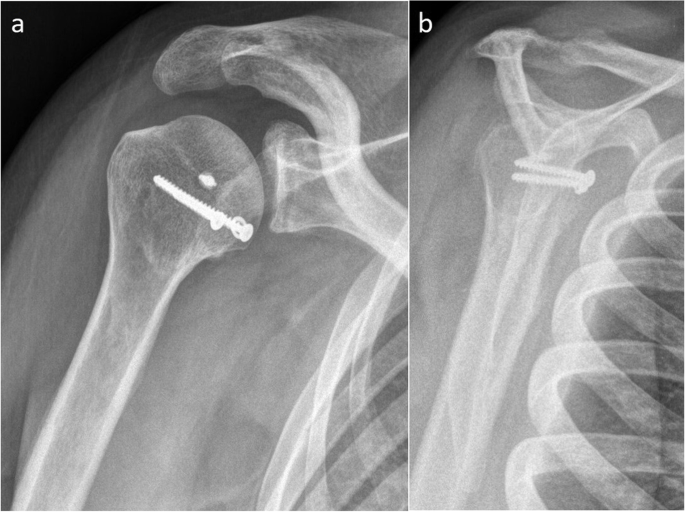
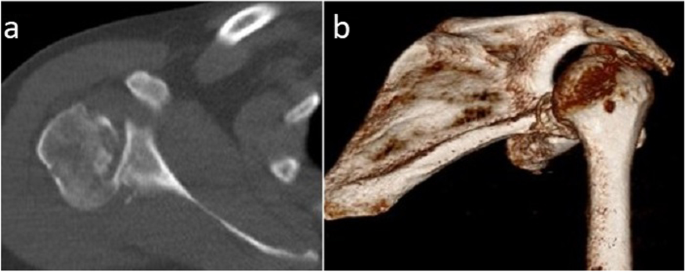
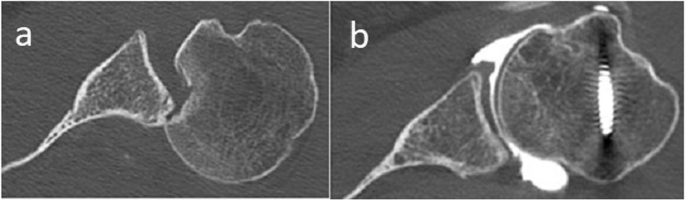
The data considered included the mechanism of injury, the active range of motion of the shoulder before and after surgery (anterior elevation, abduction, external rotation elbow at side, and internal rotation (Figs. 1 and 2)) pre- and postoperative Constant–Murley scores [27, 28], and subjective results at last follow-up (satisfaction on a 5-point Likert scale and subjective shoulder value (SSV) scores [29]). Internal rotation was evaluated using the Constant–Murley scale [27, 28] based on the highest position reached by the patient’s thumb on their back. Strength in external rotation was measured using the Medical Research Council Manual Muscle Testing scale [30]. Shoulder X-rays (anteroposterior and scapular Y images, Figs. 3 and 4) and CT scans (Figs. 5 and 6) were also evaluated. We measured the size of the defect on CT-scans in the axial plane (alpha axial angle) using the method described by Moroder et al. [31]. We estimated the percentage of the involved articular surface, in the axial plane, considering the angular defect on the humeral joint surface in relation with the entire humeral articular surface [31]. Post-operatively, all patients were followed-up radiologically (x-rays and in two cases CT-scans), however we did not evaluate the healing of the subscapularis using ultrasonography or MRI.
Locked posterior shoulder dislocation (right shoulder), postoperative physical examination. Photographs of the right arm of a patient with locked posterior shoulder dislocation treated with the modified McLaughlin procedure in (a) active anterior elevation and (b) active external rotation elbow at side
Surgery
All operations were performed using a deltopectoral approach, with the patient under general anaesthesia in the beach chair position.
In patients treated with the McLaughlin procedure (n = 2), the cranial two-thirds of the subscapularis tendon was released from its insertion on the lesser tuberosity. The tendon was marked with strong non-absorbable suture and was retracted medially. The RHSL and the glenoid were inspected after removing all fibrous tissue present. A blunt Hohmann retractor was placed between the humeral head and the glenoid. The joint was reduced using lateral distraction and gradual external rotation and the remaining humeral head cartilage and RHSL were evaluated. The base of the RHSL was rasped to obtain a bleeding surface. The subscapularis tendon was then transferred inside the RHSL, as close as possible to the medial edge, using either transosseous sutures (one case) or suture anchors (one case).
In patients treated with the modified McLaughlin procedure (n = 10), the lesser tuberosity was osteotomised laterally from the bicipital groove up to the level of the RHSL. The subscapularis tendon was tagged with strong non-absorbable suture and the lesser tuberosity was retracted medially. After inspecting the joint and RHSL and preparing the RHSL as described above, the lesser tuberosity was transferred inside the RHSL, close to its medial edge and fixed with cancellous screws and washers. An additional anchor was inserted in the RHSL in four cases (metallic in two cases, resorbable in two cases) along with sutures passed through the subscapularis tendon. No graft was used.
The stability of the joint was evaluated at the end of the procedure.
Postoperative management
Patients wore a shoulder brace maintaining the shoulder in neutral or external rotation (mainly depending on the available brace type) for 4 to 6 weeks. Hand and elbow mobilisation began from the first day after surgery. Shoulder rehabilitation was started after removal of the brace, beginning with self-rehabilitation and passive mobilisation. Active shoulder mobilization was started at about 6 weeks for patients immobilized for 4 weeks and at about 8 weeks for patients immobilized for 6 weeks.
Statistical analysis
Categorical variables were summarised as frequencies. Continuous variables were expressed as mean ± standard deviation and compared before and after surgery using paired t tests. Independent samples t tests were run to compare the postoperative results. Differences were considered statistically significant at p < 0.05. All analyses were performed using IBM SPSS Statistics, version 24.
Results
The average age at surgery was 48.2 ± 13.3 years (range, 30–67 years). Ten of the twelve patients were men. The average delay between injury and surgery was 13.5 ± 9.7 weeks (range, 3–32 weeks).
The cause of the dislocation was in one case, electrocution, in one case reflex epilepsy, in one case, unclear (apparently, the dislocation occurred when the patient rolled over in bed), and in the nine remaining cases, trauma (three motorcycle accidents, and six falls).
The initial dislocation was associated with a humeral fracture (other than the RHSL) in 8 of the 12 patients (66.7%), an isolated lesser tuberosity fracture in three cases, an oblique fracture of the proximal third of the humerus in two cases, and in one case each a spiral humeral shaft fracture, a fracture of the surgical neck and lesser tuberosity, and a multifragmentary fracture of the proximal humerus including the surgical neck, and the lesser and greater tuberosity. In all these cases of complex posterior shoulder fracture-dislocations, the associated fractures were initially treated conservatively. The posterior dislocation was missed on initial presentation in all but one case, in which, after closed reduction, the dislocation recurred. The associated fractures had healed at the time of surgery in six of eight cases because the patients presented late. In the two remaining cases, the unhealed lesser tuberosity fragment was fixed at the level of the RHSL.
The average alpha angle was 46.9° ± 7.9° (32.1°—59.5°). The RHSL represented on average 25.6% ± 5% (17.1%-36%) of the articular surface.
The McLaughlin procedure was used in two cases (16.7%) and the modified McLaughlin procedure in ten cases (83.3%).
The postoperative immobilisation period was four weeks in three patients (25%) and six weeks in nine patients (75%). The shoulder was immobilised in external rotation in six patients (50%) and in neutral rotation in six patients (50%).
One of the patients, a 44-year-old male, treated with the modified Mclaughlin procedure in 2014, had the last follow-up at 43 days postoperatively. The patient was satisfied with the result, had no pain, no early complications, and the reduction was maintained. Because of the very short follow-up, we decided to exclude this patient from our clinical results. The following analysis was performed on the remaining eleven patients.
The average delay between injury and surgery was 14.2 ± 9.9 weeks (range, 3–32 weeks).
The average postoperative follow-up, when the SSV, Constant score and shoulder range-of motion were recorded, was 37 ± 58 months (range, 6–206 months).
Pre- and postoperative clinical variables are compared in Table 1.
Six patients (54.5%) were satisfied and five patients (45.5%) were very satisfied with postoperative outcomes.
The average postoperative SSV was 86.4 ± 11.1 (range 70–100). The strength in external rotation elbow at side was grade 5 in all seven cases in which it was evaluated.
All clinical variables increased significantly between pre- and postoperative assessments (Table 1). None of the patients had a recurrence of the dislocation on the operated shoulder. There were no implant-related, infectious or neurological complications. At last follow-up (12 months), one patient had avascular necrosis of the humeral head (Cruess stage IV [32]) and two patients had glenohumeral osteoarthritis (Samilson-Prieto Allain stages 2 and 3 [33, 34], respectively).
There were no significant differences between the outcomes of patients treated with McLaughlin and modified McLaughlin procedures (independent samples t test, p > 0.05 for all the followed clinical variables). Also, the results of cases operated by LNJ or EGH were similar for all the observed clinical variables (independent samples t test, p > 0.05), with the exception of the normalized Constant score, which was better in the group of patients operated by LNJ (independent samples t test, p = 0.04).
Discussion
The clinical results obtained with the original or modified McLaughlin procedures in patients with locked posterior shoulder dislocation were favourable and comparable with those of other published studies [7, 17, 18, 35].
McLaughlin called posterior shoulder dislocation a "diagnostic trap" [36] because of the high percentage of cases missed on initial presentation. This was also the case in our study, with a significant delay between dislocation and reduction (14 weeks on average). However, even with this treatment delay in a traumatic intra-articular pathology, the clinical outcomes were still favourable, with significant improvements in all clinical variables. Also, all operated shoulders remained stable. It has to be noted that in our study the RHSL was moderate on average and this might explain our good results. A larger average RHSL would have been associated with a poorer result and, in some cases, the necessity of shoulder replacement.
These outcomes contrast with the results of the wide range of open reduction and stabilisation techniques used in chronic anterior shoulder dislocations, where a high incidence of re-subluxation and early osteoarthritis have been reported [37]. The Latarjet procedure, otherwise very successful, is considered by Walch et al. [38] to be contraindicated for locked anterior shoulder dislocations. Li et al. [39] evaluated the effectiveness of the Latarjet procedure in patients with chronic anterior dislocation and found an overall rate of postoperative redislocation or subluxation of 48%. The authors noted that in cases where the reduction was possible through a subscapularis-splitting approach, no postoperative instability was encountered [39]. However, in these chronic cases it can be very difficult to obtain reduction without a subscapularis tenotomy [37, 39].
Nevertheless, missed diagnoses of posterior shoulder dislocations – and thereby in most cases, the need for surgery – could easily be avoided by increasing orthopaedic surgeons’ and emergency doctors’ awareness of this pathology.
The proportion of cases with an associated fracture (complex posterior fracture-dislocations, 73%) was comparable to the value reported in a literature review of locked posterior shoulder dislocations (75.8%) [4]. The incidence of glenohumeral osteoarthritis was higher than reported in the same review (18.2% vs. 6.7% [4]). However, one of the two patients had pre-existing osteoarthritis (Samilson-Prieto Allain stage 1 before surgery, which progressed to stage 2 at 19 months’ follow-up) and the other developed osteoarthritis (Samilson-Prieto Allain stage 3) a very long time (more than 17 years) after surgery. The latter patient was very satisfied with the result of surgery at last follow-up, and had 110° of active anterior elevation, 25° of active external rotation, elbow at the side, and could reach L3 with his thumb on internal rotation. His normalised Constant score was 98.5%. The other patient with shoulder osteoarthritis (Samilson-Prieto 2) was satisfied with the result of surgery, had 160° of active anterior elevation, 40° of active external rotation, elbow at side, could reach L5 with his thumb, and had a normalised Constant score of 81.1%. None of the patients required shoulder arthroplasty.
There was one case of avascular necrosis (9%), in keeping with the reported incidence in the literature (3.5%) [4] given the number of patients in the study. This case (Cruess stage IV) developed soon after surgery, after a long delay between dislocation and surgical reduction (23 weeks). The patient had a good clinical outcome (no pain and acceptable function) and did not require shoulder arthroplasty.
There were no postoperative subluxations or re-dislocations. The patient with epilepsy had posterior dislocation of the contralateral shoulder caused by another seizure, but the operated shoulder remained stable.
The modified McLaughlin procedure addresses the problem of poor healing of the transferred subscapularis at the level of the RHSL in the classic McLaughlin procedure. The transfer of the lesser tuberosity together with the subscapularis should lead to faster and more predictable bone-to-bone healing.
Hawkins et al. [15] achieved equally good results with McLaughlin and modified McLaughlin procedures. These authors also reported the results of five revisions of failed McLaughlin procedures performed by other surgeons and ascribed these failures either to the RHSL being too large for this technique or to the cartilage being too severely damaged at the time of the initial surgery.
The most commonly described treatments for chronic locked posterior shoulder dislocation are the McLaughlin procedure (classic or modified) and segmental reconstruction of the humeral head with a bone graft. Both are valid alternatives and have been shown to have consistently good long term outcomes and low complication rates [19, 20, 37, 40].
In our study, the classic McLaughlin procedure was used in only two cases, with a RHSL of 17.1% and 17.9%, respectively. The reduction delay was in one case 3 weeks. However, in the other case the reduction delay was 25 weeks. The clinical results in both cases were good, with a normalized Constant score of 85% and 95%, respectively. The clinical result was better in the case of the patient with a much longer reduction delay.
Proximal humerus derotational osteotomy [21, 22, 41] can also lead to good outcomes in patients without severe articular cartilage damage. However, because of the technical complexity of the procedure and the risk of humeral head necrosis and osteoarthritis progression, some surgeons only consider derotational osteotomy as a salvage procedure when there are no other treatment options [7].
Posterior bone block has also been used to treat chronic locked posterior dislocations, with satisfactory mid-term clinical results but a high rate of postoperative osteoarthritis [23].
Results could still potentially be improved by using less invasive techniques. Arthroscopic McLaughlin procedures have recently been described [42, 43]. A recent comparison [44] of the outcomes of open modified McLaughlin and arthroscopic McLaughlin procedures found that while there were no significant differences in terms of clinical results or subscapularis strength recovery, the arthroscopic McLaughlin procedure was associated with a better sense of stability and well-being.
The limitations of this study include its retrospective nature, small number of patients (which reflects the rarity of this pathology), the fact that it was conducted in only two centers and, in some cases, relatively short follow-up. As a result, this study suffers from inadequate case representation and case selective bias. However, this is a very rare pathology so most of the series in the literature have the same weaknesses.
Conclusions
This group of patients with chronic locked posterior shoulder dislocation treated using the McLaughlin or the modified McLaughlin procedure had good clinical outcomes, even when surgical reduction was significantly delayed.
Availability of data and materials
The datasets used and/or analysed in this study are available from the corresponding author on reasonable request.
Abbreviations
- RHSL:
-
Reverse Hill–Sachs Lesion
References
Kowalsky MS, Levine WN. Traumatic posterior glenohumeral dislocation: classification, pathoanatomy, diagnosis, and treatment. Orthop Clin North Am. 2008;39(4):519–33.
Krøner K, Lind T, Jensen J. The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg. 1989;108(5):288–90.
Robinson CM, Aderinto J. Posterior shoulder dislocations and fracture-dislocations. J Bone Joint Surg Am. 2005;87(3):639–50.
Basal O, Dincer R, Turk B. Locked posterior dislocation of the shoulder : A systematic review. EFORT Open Rev. 2018;3(1):15–23.
Kelly MJ, Holton AE, Cassar-Gheiti AJ, Hanna SA, Quinlan JF, Molony DC. The aetiology of posterior glenohumeral dislocations and occurrence of associated injuries: a systematic review. Bone Joint J. 2019;101B(1):15–21.
Guehring M, Lambert S, Stoeckle U, Ziegler P. Posterior shoulder dislocation with associated reverse Hill-Sachs lesion: Treatment options and functional outcome after a 5-year follow up. BMC Musculoskelet Disord. 2017;18(1):1–7.
Babhulkar A, Unnithan V, Patil P. A treatment algorithm for locked posterior dislocation of shoulder. J Arthrosc Joint Surg. 2018;5(2):90–8.
Moroder P, Tauber M, Scheibel M, Habermeyer P, Imhoff AB, Liem D, et al. Defect characteristics of reverse hill-sachs lesions. Am J Sports Med. 2016;44(3):708–14.
Abdel-Hameed SK, Abdel-Aal MA. New technique in reconstructing humeral head defect in locked posterior dislocation of the shoulder: a case series of nine patients. Eur Orthop Traumatol. 2015;6(3):157–62.
Rouleau DM, Hebert-Davies J. Incidence of associated injury in posterior shoulder dislocation: Systematic review of the literature. J Orthop Trauma. 2012;26(4):246–51.
Kokkalis ZT, Iliopoulos ID, Antoniou G, Antoniadou T, Mavrogenis AF, Panagiotopoulos E. Posterior shoulder fracture–dislocation: an update with treatment algorithm. Eur J Orthop Surg Traumatol. 2017;27(3):285–94.
Robinson CM, Akhtar A, Mitchell M, Beavis C. Complex posterior fracture-dislocation of the shoulder: Epidemiology, injury patterns, and results of operative treatment. J Bone Joint Surg Am. 2007;89(7):1454–66.
Cohen M, Fonseca R, Amaral MVG, Monteiro MT, Filho GRM. Treatment of chronic locked posterior dislocation of the shoulder with the modified McLaughlin procedure. J Shoulder Elbow Surg. 2022;31(1):100–6.
McLaughlin HL. Locked posterior subluxation of the shoulder: diagnosis and treatment. Surg Clin North Am. 1963;43(6):1621–2.
Hawkins MD, Neer CS, Pianta RM, Mendoza FX. Locked Posterior Dislocation of the Shoulder. J Bone Joint Surg Am. 1987;69(1):9–18.
Castagna A, Delle Rose G, Borroni M, Markopoulos N, Conti M, Maradei L, et al. Modified MacLaughlin procedure in the treatment of neglected posterior dislocation of the shoulder. Chir Organi Mov. 2009;93(Suppl 1):1–5.
Shams A, El-Sayed M, Gamal O, ElSawy M, Azzam W. Modified technique for reconstructing reverse Hill-Sachs lesion in locked chronic posterior shoulder dislocation. Eur J Orthop Surg Traumatol. 2016;26(8):843–9.
Khira YM, Salama AM. Treatment of locked posterior shoulder dislocation with bone defect. Orthopedics. 2017;40(3):e501–5.
Gerber C, Catanzaro S, Jundt-Ecker M, Farshad M. Long-term outcome of segmental reconstruction of the humeral head for the treatment of locked posterior dislocation of the shoulder. J Shoulder Elbow Surg. 2014;23(11):1682–90.
Martinez AA, Navarro E, Iglesias D, Domingo J, Calvo A, Carbonel I. Long-term follow-up of allograft reconstruction of segmental defects of the humeral head associated with posterior dislocation of the shoulder. Injury. 2013;44(4):488–91.
Keppler P, Holz U, Thielemann FW, Meinig R. Locked posterior dislocation of the shoulder: Treatment using rotational osteotomy of the humerus. J Orthop Trauma. 1994;8(4):286–92.
Ziran B, Nourbakhsh A. Proximal humerus derotational osteotomy for internal rotation instability after locked posterior shoulder dislocation: Early experience in four patients. Patient Saf Surg. 2015;9(1):1–5.
Aksekili MAE, Mahmut U, Çetin I, Yüksel K, Beçici V, Bozkurt M. Posterior bone block of chronic locked posterior shoulder dislocations with glenoid augmentation : a retrospective evaluation of ten shoulders. Int Orthop. 2015;40(4):813–20.
Wooten C, Klika B, Schleck CD, Harmsen WS, Sperling JW, Cofield RH. Anatomic shoulder arthroplasty as treatment for locked posterior dislocation of the shoulder. J Bone Joint Surg Am. 2014;96(3):1–6.
Cheng SL, Mackay FCMB, Richards RR, Toronto FC. Treatment of locked posterior dislocation of the shoulder by total shoulder arthroplasty. J Shoulder Elbow Surg. 1997;6:11–7.
Raiss P, Edwards TB, Bruckner T, Loew M, Zeifang F, Walch G. Reverse arthroplasty for patients with chronic locked dislocation of the shoulder (type 2 fracture sequela). J Shoulder Elbow Surg. 2017;26(2):279–87.
Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–4.
Constant CR, Gerber C, Emery RJH, Søjbjerg JO, Gohlke F, Boileau P. A review of the Constant score: Modifications and guidelines for its use. J Shoulder Elbow Surg. 2008;17(2):355–61.
Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8(6):599–605.
Dyck PJ, Boes CJ, Mulder D, Millikan C, Windebank AJ, Dyck PJ, et al. History of standard scoring notation and summation of neuromuscular signs A current survey and recommendation. J Peripher Nerv Syst. 2005;10(2):158–73.
Moroder P, Tauber M, Hoffelner T, Auffarth A, Korn G, Bogner R, et al. Reliability of a New Standardized Measurement Technique for Reverse Hill-Sachs Lesions in Posterior Shoulder Dislocations. Arthroscopy. 2013;29(3):478–84.
Cruess R. The current status of avascular necrosis of the femoral head. Clin Orthop Relat Res. 1978;131:309–11.
Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65(4):456–60.
Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am. 1998;80(6):841–52.
Kokkalis ZT, Mavrogenis AF, Ballas EG, Papagelopoulos PJ, Zoubos AB. Bilateral neglected posterior fracture-dislocation of the shoulders. Orthop. 2012;35(10):e1537–41.
McLaughlin HL. Posterior dislocation of the shoulder. J Bone Joint Surg Am. 1952;24(A3):584–90.
Sahu D, Rathod V, Phadnis A, Shyam A. Results and complications of head preserving techniques in chronic neglected shoulder dislocation: a systematic review. J Shoulder Elbow Surg. 2021;30(3):685–94.
Domos P, Lunini E, Walch G. Contraindications and complications of the Latarjet procedure. Shoulder Elbow. 2018;10(1):15–24.
Li Y, Jiang C. The effectiveness of the latarjet procedure in patients with chronic locked anterior shoulder dislocation: a retrospective study. J Bone Joint Surg Am. 2016;98(10):813–23.
Diklic ID, Ganic ZD, Blagojevic ZD, Nho SJ, Romeo AA. Treatment of locked chronic posterior dislocation of the shoulder by reconstruction of the defect in the humeral head with an allograft. J Bone Joint Surg Br. 2010;92(1):71–6.
Porteous MJ. Humeral Rotation Osteotomy for Chronic Posterior Dislocation of the Shoulder. J Bone Joint Surg Br. 1990;72(3):468–9.
Besnard M, Audebert S, Godenèche A. Arthroscopic McLaughlin Procedure for Treatment of Posterior Instability of the Shoulder With an Engaging Reverse Hill-Sachs Lesion. Arthrosc Tech. 2019;8(12):e1491–4.
Bernholt DL, Lacheta L, Goldenberg BT, Millett PJ. Arthroscopic Knotless Modified McLaughlin Procedure for Reverse Hill-Sachs Lesions. Arthrosc Tech. 2020;9(1):e65-70.
Ippolito G, Zitiello M, De Marinis G, D’Angelo F, Surace MF, Ronga M, et al. Posterior shoulder dislocation with engaging reverse hill-sachs lesion: a retrospective study of ten patients treated with arthroscopy or open reduction and stabilisation. J Clin Med. 2021;10(7):1410.
Acknowledgements
Not applicable
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Emil George Haritinian: study design, data collection and analysis and article writing.Ioan Cristian Stoica: study design, supervision. Roman Popescu: data collection and analysis. Gavril Lucian Gheorghievici: data collection and analysis. Laurent Nové-Josserand: study design, supervision, data analysis and article writing. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by Ramsay Santé Ethical Committee (COS-RGDS-2022–04-001-NOVEJOSSERAND-L /12/04/2022) and Foișor Orthopaedic Hospital Ethical Committee (3421/04.04.2022).
All methods were performed in accordance with the relevant guidelines and regulations.
All patients included in this study provided informed consent for their participation.
Consent for publication
This article contains no identifying images or details. However, it includes clinical images of one patient. Written informed consent for the clinical details and clinical images was obtained from the patient. A copy of the consent form is available for review by the Editor of this journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Haritinian, E.G., Stoica, I.C., Popescu, R. et al. Treatment and outcomes of chronic locked posterior shoulder dislocations: a retrospective case series. BMC Musculoskelet Disord 24, 82 (2023). https://doi.org/10.1186/s12891-023-06200-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06200-8