Abstract
Background
Many surgical options have been described to manage post-tubercular kyphosis, but the standard approach for treating severe post-tubercular angular kyphosis in children has not been established yet. The present study was performed to evaluate the safety and efficacy of deformed complex vertebral osteotomy (DCVO) for the treatment of severe thoracic post-tubercular angular kyphosis (> 70°) in children.
Methods
Deformed complex vertebrae indicated that multiple deformed and fused vertebrae were usually involved with two or more vertebral bodies and the partial or total fusion of many segments' facet joints and intervertebral discs. Thus, DCVO indicated that a wider posterior wedge-shaped and three-column osteotomy was performed within deformed complex vertebrae to correct a more extensive range of angles. From 2010 to 2017, 15 children who suffered from severe thoracic post-tubercular angular kyphosis underwent DCVO. Deformed complex vertebrae involved two vertebral bodies in 9 patients and three vertebral bodies in 6 patients. The Visual Analogue Scale (VAS) and Oswestry Disability Index (ODI) were assessed preoperatively and at the final follow up. This was a retrospective study analysing the outcome after grade 4/5 spinal osteotomies in deformed complex vertebrae.
Results
The mean duration of surgery was 239 ± 37.81 min. The average period of follow-up was 31.6 ± 6.98 months. The preoperative mean kyphosis of deformed complex vertebrae was 83.39° ± 9.04°; the mean thoracic kyphosis (TK) and lumbar lordosis (LL) were 81.09° ± 8.51° and 80.51° ± 7.64°, respectively; the mean sagittal vertical axis (SVA) was 3.83 cm ± 1.43 cm. The postoperative mean kyphosis of deformed complex vertebrae was reduced to 19.98° ± 2.47° (P < 0.001) with a mean kyphosis correction of 63.41°; at the final follow up, it was 18.4° ± 2.29° (P < 0.001) without obvious loss of correction. The postoperative mean TK, LL, and SVA were reduced to 24.05° ± 3.84°, 46.9° ± 3.53°, and 0.6 cm ± 0.34 cm, respectively (P < 0.001 for all); and there was no obvious loss of sagittal alignment and balance at the final follow up (p = 0.982, p = 0.604, p = 0.754). Complicated with neural dysfunction preoperatively, 5 Frankel's grade D cases showed complete neurological recovery at final follow up. VAS score reduced from 3.6 ± 1.18 to 0.87 ± 0.64 (P < 0.001); and ODI score reduced from 22.21 ± 6.93 to 5.02 ± 2.6 (P < 0.001) at the final follow up.
Conclusions
DCVO was an individualized osteotomy for treating severe thoracic post-tubercular angular kyphosis in children and could be safe and effective in reducing the incidence of complications and significantly improving kyphosis correction.
Similar content being viewed by others
Background
Spinal tuberculosis accounts for half the cases of osteo-articular tuberculosis. Vertebral inoculation occurs via the haematogenous route, and the process then spreads to the intervertebral disk and, in some cases, to the adjacent vertebra. Para-spinal abscesses may develop by direct spread from the vertebral lesion. The thoracic spine is predominantly involved [1]. The patients with spinal tuberculosis that were treated conservatively presented with kyphosis with an average of 15°, and eventually, 3–5% of them ended up with a kyphotic angle of more than 60° [2,3,4,5]. Furthermore, even if spinal tuberculosis heals during the period of growth and development of children, an imbalance in the spinal growth of the anterior and posterior columns could still aggravate kyphosis [6, 7]. Severe post-tubercular angular kyphosis generally affects children's self-confidence and appearance and could even lead to severe neurological impairment and cardiopulmonary dysfunction. Many surgical options have been described to manage post-tubercular angular kyphosis, but the standard approach has not yet been established.
Until now, surgical osteotomy has been the leading choice for correcting the deformity and realigning the spine. Posterior column osteotomy (PCO) is not indicated as a first-line treatment for post-tubercular angular kyphosis because of the difficulty in decompressing the spine canal anteriorly and the relatively small correction angle [8,9,10]. Conversely, pedicle subtraction osteotomy (PSO) is a wedge-shaped resection in one vertebra which includes the partial vertebral body and posterior column elements and can only acquire correction of 30°-40° [9,10,11]. Vertebral column resection (VCR) requires removing one or several whole vertebrae, concurrently including adjacent discs and a portion of the ribs in the thoracic region, which could significantly correct severe kyphoscoliosis. However, VCR has several disadvantages, such as neurological complications, blood loss, operation time, nonunion or pseudoarthrosis, and a significant increase in the incidence of postoperative complications [12,13,14,15]. Therefore, the present study was performed to evaluate the safety and efficacy of modified posterior wedge osteotomy within deformed complex vertebrae to treat severe thoracic post-tubercular angular kyphosis (> 70°) in children. This was a retrospective study analysing the outcome after grade 4/5 spinal osteotomies.
Materials and methods
Patient data
In this study, we retrospectively evaluate the clinical efficacy of 15 children (8 boys and 7 girls; age, 5–11 years; average age, 7.8 ± 2.0 years) that suffered from severe thoracic post-tubercular angular kyphosis and were treated in our department between 2010 to 2017. In all children, X-ray, CT, and MRI examinations revealed: deformed complex vertebrae involved with two vertebral bodies in 9 patients and three vertebral bodies in 6 patients; the lesions healed completely in all 15 cases without further destruction of the vertebral bodies or abscesses.
All cases presented with apparent kyphotic deformity and persistent back pain, and some of them incurred incomplete paralysis. C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) in all cases were normal. The Frankel scoring system was used to assess neurological function. Frankel's grade D was in 5 patients, and Grade E in 10 patients. The Ethics Committee of Xiangya Hospital of Central South University approved the study. All methods were performed by following the relevant guidelines and regulations. Written informed consent was acquired from each patient (or their parents and legal guardians) to authorize treatment, imaging studies, and photographic documentation. The patients (or their parents or legal guardians) permitted their photographs and anonymised clustering data for publication.
The inclusion criteria were based on the following criteria: (1) severe thoracic angular kyphosis more than 70°; (2) the tuberculosis lesions completely healed; (3) CRP (range, 0—8 mg/L) and ESR (range, 0—21 mm/h) were normal; (4) deformed complex vertebrae involved two or more vertebral bodies; (5) children of elementary school age; (6) patients treated at our hospital with a minimum 2-year follow-up.
Exclusion criteria were based on: (1) no severe or progressive kyphosis; (2) deformed vertebra involved with only one vertebral body; (3) spine deformities caused by congenital malformations or trauma; (4) incomplete clinical and radiological documentation at follow-up.
Operative procedure
During the operation, somatosensory evoked potential (SEP) and motor evoked potential (MEP) were thoroughly utilized to monitor the spinal cord functions. After exposure of posterior spinal components through a midline incision, pedicle screws were placed in one or two segments above and below deformed complex vertebrae. The ribs in affected segments were resected enough to reveal the lateral aspect of deformed complex vertebral bodies. The laminae and facet joints were removed to expose the spinal canal and nerve root canal. The nerve roots were identified and preserved. Isolation and decompression of the nerve roots were acquired to reduce the tension of the spinal cord and dura. If intraoperative exposure and osteotomy suffer from difficulties, corresponding nerve roots should be ligated appropriately. The temporary rod adhered to screws alternately. Deformed complex vertebral osteotomy (DCVO) was performed at the apex of kyphotic deformity. Pre-bent rods were used to gently and progressively replace the temporary rod. Compression was applied to the screws and rods to achieve bone-to-bone closure. Laminectomy was performed on the adjacent regions of the normal vertebrae when the dura was folded. The shorter spinal cord could be further decompressed by increasing the inner diameter of the spinal canal. For fusion, allogeneic or autogenous bone grafts could be used.
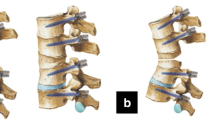
Deformed complex vertebrae indicated that multiple deformed and fused vertebrae were usually involved with two or more vertebral bodies and the partial or total fusion of many segments' facet joints and intervertebral discs [16]. The DCVO involves performing a larger posterior wedge-shaped and three-column osteotomy within deformed complex vertebrae using an ultrasonic scalpel, osteotomes, and high-speed drilling to correct a wider range of angles. The upper and lower endplates of deformed complex vertebrae that adjoined normal vertebrae were preserved. Special attention was taken not to break the anterior longitudinal ligament, which served as a hinge when closing the gap. Bone-to-bone closure and fusion were achieved without the interbody fusion cages, resulting in a better fusion efficiency (Fig. 1).
Diagram of the DCVO. A a wider posterior wedge-shaped and three-column osteotomy was performed within multiple deformed complex vertebrae. B The upper and lower endplates were preserved. Anterior longitudinal ligament was also preserved as a hinge for closure of the gap. C bone-to-bone closure was achieved in the anterior and middle columns without interbody fusion cages, resulting in better fusion efficiency. The part surrounded by a blue dotted line was prepared to avoid root entrapment through decompression and expanding the inner diameter of the intervertebral foramen
Visual Analogue Scale (VAS) and Oswestry Disability Index (ODI)
According to self-assessment, the pain was measured preoperatively and at the final follow up by VAS without an analgesic. Furthermore, the daily activities were also assessed preoperatively and at the final follow up by ODI to analyse clinical function.
Radiographical and statistical analysis
At the preoperative, postoperative, and final follow-up stages, radiographs' parameters, including kyphosis of deformed complex vertebrae, TK, LL, SVA, were measured. The data were shown as means ± SD and analysed using SPSS 22.0. Paired t-test was used to compare the parameters preoperatively, postoperatively, and at the final follow up. P < 0.05 indicates statistically significant difference.
Results
Surgical results
The mean duration of surgery was 239 ± 37.81 min (range, 170—310 min) and the mean blood loss was 641.33 ± 185.12 ml (range, 410—1010 ml). A thorough neurological examination was carried out in all of the cases after the operation and at the final follow up. During operation, no severe complications such as extensive vessel injury, spinal cord injury, or nerve injury occurred. Moreover, there were no cerebrospinal fluid leakage, death, or severe infection cases, and none showed new irreversible neural injury. The average period of follow-up was 31.6 ± 6.98 months (range, 24—48 months). No complications related to instrumentation failure occurred. Two cases experienced MEP changes that were reduced by more than 50% of baseline amplitude. However, the intraoperative wake-up test was successful in all of them. Complicated with neural dysfunction preoperatively, 5 Frankel's grade D cases showed complete neurological recovery at final follow up.
Kyphosis correction
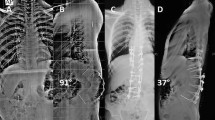
The preoperative mean kyphosis of deformed complex vertebrae was 83.39° ± 9.04° (range, 70.8°-102.6°); the mean thoracic kyphosis (TK) and lumbar lordosis (LL) were 81.09° ± 8.51° (range, 66.1°-97.4°) and 80.51° ± 7.64° (range, 68.5°-93.8°), respectively; the mean sagittal vertical axis (SVA) was 3.83 cm ± 1.43 cm (range, 1.7 cm-6.8 cm). The postoperative mean kyphosis of deformed complex vertebrae was reduced to 19.98° ± 2.47° (range, 15.7°-23.6°) with a mean kyphosis correction of 63.41°, which showed a statistically significant difference between the preoperative and postoperative data (P < 0.001). At the final follow up, the mean kyphosis of deformed complex vertebrae was 18.4° ± 2.29° (range, 13.8°—21.2°) without apparent loss of correction as compared with the postoperative data. The postoperative mean TK, LL, and SVA were reduced to 24.05° ± 3.84° (range, 17.1°-29.8°), 46.9° ± 3.53° (range, 41.3°-54.1°), and 0.6 cm ± 0.34 cm (range, 0.1 cm-1.2 cm), respectively. All the indexes also showed significant improvement compared with the preoperative data (P < 0.001 for all); there was no statistically significant difference between postoperative and final follow-up data (P > 0.05 for all). (Fig. 2) (Table 1).
A 5-year-old girl with severe thoracic post-tubercular angular kyphosis. a-d Preoperative X-ray, CT, and MRI showed post-tubercular deformed complex vertebrae involved with T9-11. The angular kyphosis of deformed complex vertebrae was 81.2°, TK was 91.3°, LL was 85.7°, SVA was 4.3 cm, and the spinal cord was compressed obviously. e–g After DCVO, postoperative X-ray and CT showed that the kyphosis of deformed complex vertebrae was reduced to 20.3° with kyphosis correction of 60.9°, TK was 27.5°, LL was 47.9°, and SVA was 0.9 cm. h Postoperative radiographs at 30 months after surgery showed that the kyphosis of deformed complex vertebrae was further reduced to 18.4°, TK was 29.8°, LL was 55.3°, and SVA was 1.4 cm
VAS and ODI
VAS and ODI were assessed preoperatively and at the final follow up. At the final follow up, VAS score reduced from 3.6 ± 1.18 (range, 2–6) to 0.87 ± 0.64 (range, 0–2); and ODI score reduced from 22.21 ± 6.93 (range, 11.1–33.3) to 5.02 ± 2.6 (range, 2.2–11.1); they both revealed significant statistical differences between final follow-up and preoperative scores (P < 0.001).
Discussion
In this study, severe thoracic post-tubercular angular kyphosis was involved with two or more fused vertebrae, and the preoperative mean kyphosis of deformed complex vertebrae was 83.39°. Given these characteristics of this group of patients account, it was difficult to choose an appropriate resection area and find a proper osteotomy technique that could be safe and effective. Therefore, DCVO was performed at the apex of kyphotic deformity. A wider posterior wedge-shaped, three-column and grade 4/5 spinal osteotomy was performed within deformed complex vertebrae. The upper and lower endplates of the deformed complex vertebrae were preserved to prevent growth imbalance of the anterior and posterior columns in children during their growth phase by keeping the growth potentials of the anterior column and to reduce surgical trauma and intraoperative blood loss. The anterior longitudinal ligament served as a hinge for the bone-to-bone closure of the gap. In this group of cases, the nerve roots were not ligated and slightly affected the visibility of the operative field and the freedom of osteotomy. However, there was no direct damage to the nerve roots, and this helped preserve nervous system functional integrity.
After DCVO, the postoperative mean kyphosis was reduced to 19.98° with a kyphosis correction of 63.41°. The correction rate was considerably better than that of PSO and VCR reported by some authors [9, 10, 12, 14, 17, 18]. Patients' body figure, sagittal alignment and balance (TK, LL, and SVA), pain (VAS), daily activities (ODI), and neurological function (Frankel's grade) all showed good improvement. However, the operation time, blood loss, difficulty of operation, incidence of complications, and neurological events were significantly lower than those of VCR reported in previous studies [12, 14, 17, 19, 20].
Although conservative treatment is effective with the use of antituberculosis medication, however, it is well known that progressive collapse of anterior spinal elements may still occur under gravity and compression. Moreover, due to eccentric loads and spinal growth imbalance of anterior and posterior columns in children, the wedge shape of the vertebral body and kyphotic deformity could be aggravated. Neurological deterioration, cardiopulmonary dysfunction, and severe persistent back pain are all possible side effects of post-tubercular kyphosis [2, 21, 22]. As a result, children with severe thoracic post-tubercular angular kyphosis frequently require surgery.
The primary goal of surgery is to treat spinal deformity and prevent further deformity, as well as to restore and reconstruct the physiological sagittal alignment and decompress the nerve to improve its function. To date, numerous techniques have been developed to treat kyphosis secondary to spinal tuberculosis, mainly including Smith-Petersen Osteotomy (SPO), PSO, and VCR [10, 14, 21, 23]. However, none of those mentioned above techniques was considered a golden criterion for attaining minor trauma and significant correction.
SPO could only achieve approximately 10.7° per segment of kyphosis correction. However, after opening the anterior column, it was determined that there was a risk of permanent neurological impairment and aortic rupture [10, 24]. In recent years, three-column osteotomy has been the primary technique for the treatment of severe angular kyphosis. Hu et al. [9] compared SPO and PSO in the treatment of rigid thoracolumbar kyphotic deformity, finding that PSO's kyphosis correction ranged from 31.7° to 48° with an average of 36.7°, while SPO's was 8.74° less. Furthermore, the incidence of biomechanical complications, including instrument breakage, anterior cortex fracture, pedicle screw loosening, pedicle fraction, vertebral body translation, and nonunion, in PSO was lower than in SPO [10, 25]. In addition, a retrospective study of patients with rigid post-tuberculous kyphosis and no neurological deficit preoperatively, whose mean kyphotic angle was 58.8°, revealed the mean kyphosis correction of only 44.2° after PSO [18].
However, there are several disadvantages of PSO for the treatment of severe thoracic angular kyphosis (> 70°) [13, 18, 26]: (1) The PSO technique only achieves limited deformity correction and cannot achieve the goal of treating severe angular kyphosis of more than 70°. (2) Severe post-tubercular angular kyphosis commonly involves two or more deformed fused vertebrae. Thus, defined PSO in one vertebra may not accord with the requirements of appropriate resection area wedge osteotomy at the apex of kyphosis. However, multiple deformed and fused vertebrae were treated as a single unit, according to DCVO, and a wider posterior wedge-shaped and three-column osteotomy was performed within multiple deformed and fused vertebrae to correct a more extensive range of angles.
The most effective therapeutic technique is VCR, and 3-column circumferential vertebral osteotomy created a segmental defect with apparent instability, necessitating temporary instrumentation. Following that, the two divided parts were brought together for rectification and realignment, which necessitated titanium mesh or block bone grafts. Suk et al. [17] reported seventy patients with severe spinal deformity were treated by posterior VCR, and the deformity correction was 45.2° in the sagittal plane and 61.9% in the coronal plane. The mean blood loss was 2980 ml in the postinfectious kyphosis group, and 24 patients suffered severe complications.
However, in a study of 147 patients with severe spinal deformity who underwent VCR, Lenke et al. [14] discovered that these complex reconstructions were associated with a 59% complication rate, with 39 cases (27%) suffering an intraoperative neurological event, such as a failed wake-up test or a change in spinal cord monitoring. Hua et al. [20] treated severe post-tubercular kyphosis with VCR: 2 of 13 cases had spinal cord injuries, including one complete paraplegia and one incomplete paraplegia, and a total neurological complication rate of about 15.4%; the mean operative time and blood loss were 388 min and 2554 ml. Other complications, including fixation failure due to nonunion or pseudoarthrosis, hematomas, hemopneumothorax, and infections, also occurred frequently [12, 14, 17, 19]. Therefore, VCR was an exhausting and technically demanding procedure with possible risks of significant complications. This point of view was commonly recognized as a consensus by most surgeons.
Therefore, when compared to PSO and VCR, the following characteristics and benefits of DCVO can be summarized [8,9,10,11,12,13,14,15,16,17,18,19,20, 26]: (1) Deformed complex vertebrae usually involve two or more vertebral bodies and the partial or total fusion of many segments' facet joints and intervertebral discs. Multiple deformed and fused vertebrae were treated as a single unit, which simplified complicated problems and aided in developing a more specific osteotomy within the unit and precise positioning during surgery. (2) A wider posterior wedge-shaped and three-column osteotomy was performed within deformed complex vertebrae to correct a larger range of angles. The upper and lower endplates and the part of cancellous bone that adjoined normal vertebrae were preserved without involving normal discs. Thus, beneficial for reducing surgical trauma and intraoperative blood loss. (3) Anterior longitudinal ligament was also kept as a hinge for closure of the gap. The spine structure was relatively stable, and closure resistance was lower, which reduces the risk of displacement. (4) Bone-to-bone closure was achieved in the anterior and middle columns without interbody fusion cages, resulting in better fusion efficiency. (5) After DCVO, this group of patients had a kyphosis correction of 63.41°, which was more significant than the PSO correction rate. (6) It was effective to treat kyphosis and prevent growth imbalance of the anterior and posterior columns in children during their growth phase by keeping the growth potentials of the anterior column without destroying the upper and lower endplates. (7) DCVO combined the benefits of both PSO (hinge for bone-to-bone closure) and VCR (maximal correction of a wide range of angles). While also avoiding the drawbacks of both PSO (in one vertebra with restricted and lower correction rate) and VCR (greater incidence of complications, blood loss, and difficulty of operation; longer operation time and neurological sequelae).
Some limitations need to be taken into account. The included cases had a small sample size, and the long-term follow-up outcome should be investigated further. Future prospective comparative studies may provide further insight into the advantages and potential fallacies of these procedures.
Conclusions
In conclusion, DCVO was an individualized osteotomy for treating severe thoracic post-tubercular angular kyphosis in children. It could be safe and effective in reducing the incidence of complications and significantly improving kyphosis correction.
Availability of data and materials
The datasets analyzed during the current study are not publicly available because a further study about severe angular kyphosis is in progress in our institution, but are available from the corresponding author on reasonable request.
Abbreviations
- DCVO:
-
Deformed complex vertebral osteotomy
- SVA:
-
Sagittal vertical axis
- VAS:
-
Visual Analogue Scale
- ODI:
-
Oswestry Disability Index
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- TK:
-
Thoracic kyphosis
- LL:
-
Lumbar lordosis
- MEP:
-
Motor evoked potential
- SEP:
-
Somatosensory evoked potential
- PCO:
-
Posterior column osteotomy
- SPO:
-
Smith-Petersen Osteotomy
- PSO:
-
Pedicle subtraction osteotomy
- VCR:
-
Vertebral column resection
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
References
Ferrer MF, Torres LG, Ramírez OA, Zarzuelo MR, González NDP, Tuberculosis of the spine. A systematic review of case series. Int Orthop. 2012;36(2):221–31.
Rajasekaran S. Kyphotic deformity in spinal tuberculosis and its management. Int Orthop. 2012;36(2):359–65.
Wang YX, Zhang HQ, Tang MX, Guo CF, Deng A, Wu JH, Liu JY, Deng Z, Chen J. One-stage posterior focus debridement, interbody grafts, and posterior instrumentation and fusion in the surgical treatment of thoracolumbar spinal tuberculosis with kyphosis in children: a preliminary report. Childs Nerv Syst. 2016;32(8):1495–502.
Deng A, Zhang HQ, Tang MX, Liu SH, Gao QL, Wang YX, Guo CF, Wang XY. One-stage combined posterior and anterior approaches for active tuberculosis of the subaxial cervical spine complicated with kyphosis in children: a preliminary study. Int J Clin Exp Med. 2016;9(2):3953–9.
Zhang HQ, Li JS, Guo CF, Liu SH, Tang MX, Wang YX, Deng A, Le Gao Q, Lin MZ. Two-stage surgical management using posterior instrumentation, anterior debridement and allografting for tuberculosis of the lower lumbar spine in children of elementary school age: minimum 3-year follow-up of 14 patients. Arch Orthop Trauma Surg. 2012;132(9):1273–9.
Rajasekaran S, Prasad Shetty A, Dheenadhayalan J, Shashidhar Reddy J, Naresh-Babu J, Kishen T. Morphological changes during growth in healed childhood spinal tuberculosis: a 15-year prospective study of 61 children treated with ambulatory chemotherapy. J Pediatr Orthop. 2006;26(6):716–24.
Moon MS, Kim SS, Lee BJ, Moon JL. Spinal tuberculosis in children: retrospective analysis of 124 patients. Indian J Orthop. 2012;46(2):150–8.
Rathod TN, Shah KA. Vertebral column resection for post tuberculosis severe kyphotic deformity: results of 5 year follow-up. J Orthop. 2019;19:122–7.
Hu XM, Thapa AJ, Cai ZP, Wang P, Huang L, Tang Y, Ye JC, Cheng K, Shen HY. Comparison of smith-petersen osteotomy, pedicular subtraction osteotomy, and poly-segmental wedge osteotomy in treating rigid thoracolumbar kyphotic deformity in ankylosing spondylitis a systematic review and meta-analysis. BMC Surg. 2016;16:4.
Cho KJ, Bridwell KH, Lenke LG, Berra A, Baldus C. Comparison of Smith-Petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine. 2005;30(18):2030–7.
Park JS, Kim J, Joo IH, Sim KD, Park YS. Analysis of risk factors for sagittal translation after pedicle subtraction osteotomy in patients with ankylosing spondylitis. Spine J. 2018;18(8):1356–62.
Yang C, Zheng Z, Liu H, Wang J, Kim YJ, Cho S. Posterior vertebral column resection in spinal deformity: a systematic review. Eur Spine J. 2016;25(8):2368–75.
Schwab F, Blondel B, Chay E, Demakakos J, Lenke L, Tropiano P, Ames C, Smith JS, Shaffrey CI, Glassman S, Farcy JP, Lafage V. The comprehensive anatomical spinal osteotomy classification. Neurosurgery. 2014;74(1):112–20.
Lenke LG, Newton PO, Sucato DJ, Shufflebarger HL, Emans JB, Sponseller PD, Shah SA, Sides BA, Blanke KM. Complications after 147 consecutive vertebral column resections for severe pediatric spinal deformity: a multicenter analysis. Spine. 2013;38(2):119–32.
Riley MS, Lenke LG, Chapman TM Jr, Sides BA, Blanke KM, Kelly MP. Clinical and radiographic outcomes after posterior vertebral column resection for severe spinal deformity with five-year follow-up. J Bone Joint Surg Am. 2018;100(5):396–405.
Zhang HQ, Xiao LG, Guo CF, Wang YX, Wu JH, Liu JY. Deformed complex vertebral osteotomy technique for management of severe congenital spinal angular kyphotic deformity. Orthop Surg. 2021;13(3):1016–25.
Suk SI, Kim JH, Kim WJ, Lee SM, Chung ER, Nah KH. Posterior vertebral column resection for severe spinal deformities. Spine. 2002;27(21):2374–82.
Kalra KP, Dhar SB, Shetty G, Dhariwal Q. Pedicle subtraction osteotomy for rigid post-tuberculous kyphosis. J Bone Joint Surg Br. 2006;88(7):925–7.
Zhang HQ, Li JS, Liu SH, Guo CF, Tang MX, Gao QL, Lin MZ, Yin XH, Wang YX, Deng A. The use of posterior vertebral column resection in the management of severe posttuberculous kyphosis: a retrospective study and literature review. Arch Orthop Trauma Surg. 2013;133(9):1211–8.
Hua W, Wu X, Zhang Y, Gao Y, Li S, Wang K, Liu X, Yang S, Yang C. Incidence and risk factors of neurological complications during posterior vertebral column resection to correct severe post-tubercular kyphosis with late-onset neurological deficits: case series and review of the literature. J Orthop Surg Res. 2018;13:269.
Bezer M, Kucukdurmaz F, Guven O. Transpedicular decancellation osteotomy in the treatment of posttuberculous kyphosis. J Spinal Disord Tech. 2007;20(3):209–15.
Pappou IP1, Papadopoulos EC, Swanson AN, Mermer MJ, Fantini GA, Urban MK, Russell L, Cammisa FP Jr, Girardi FP. Pott disease in the thoracolumbar spine with marked kyphosis and progressive paraplegia necessitating posterior vertebral column resection and anterior reconstruction with a cage. Spine. 2006;31(4):E123-127.
Issack PS, Boachie-Adjei O. Surgical correction of kyphotic deformity in spinal tuberculosis. Int Orthop. 2012;36(2):353–7.
Liu H, Yang C, Zheng Z, Ding W, Wang J, Wang H, Li S. Comparison of Smith-Petersen osteotomy and pedicle subtraction osteotomy for the correction of thoracolumbar kyphotic deformity in ankylosing spondylitis: a systematic review and meta-analysis. Spine. 2015;40(8):570–9.
Hong-Qi Z, Yong C, Jia H, Chaofeng G, Xiongke H. Modified pedicle subtraction osteotomies (mPSO) for thoracolumbar post-tubercular kyphosis in pediatric patients: retrospective clinical cases and review of the literature. Childs Nerv Syst. 2015;31(8):1347–54.
Yang BP, Ondra SL, Chen LA, Jung HS, Koski TR, Salehi SA. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine. 2006;5(1):9–17.
Acknowledgements
Not applicable.
Funding
The study was supported by the Natural Science Foundation of Hunan Province, China (NO. 2020JJ4873). The funding bodies had no role in the design of the study or in collection, analysis, interpretation or presentation of data.
Author information
Authors and Affiliations
Contributions
HQZ was involved in critical revision of the manuscript, statistical expertise and performing most of the analyses presented in the paper. AD was involved in study design, data analysis and interpretation, writing the manuscript and critical revision of the manuscript. CFG was involved in data collection, preliminary data analysis and interpretation, critical revision of the manuscript and statistical expertise. QLG was involved in study conception and design, data analysis and interpretation, writing the manuscript, critical revision of the manuscript, supervision and administrative support. EA was involved in study conception and design, data collection, development of data collection instruments and critical revision of the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee in Xiangya Hospital of Central South University approved the study. All methods were performed in accordance with the relevant guidelines and regulations. Written informed consent was acquired from each of the patients (or their parents and legal guardians) to authorize treatment, imageology findings, and photographic documentation. The patients (or their parents and legal guardians) consented to the publication of their pictures as well as their anonymous and clustered data.
Consent for publication
Written informed consent was acquired from each of the patients (or their parents and legal guardians) to authorize treatment, imageology findings, and photographic documentation. The patients (or their parents and legal guardians) consented to the publication of their pictures as well as their anonymous and clustered data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, HQ., Deng, A., Guo, CF. et al. Retrospective analysis of deformed complex vertebral osteotomy in children with severe thoracic post-tubercular angular kyphosis. BMC Musculoskelet Disord 23, 805 (2022). https://doi.org/10.1186/s12891-022-05756-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05756-1