Abstract
Background
Approximately 20% of people experience chronic postsurgical pain after total knee replacement. The STAR randomised controlled trial (ISCRTN92545361) evaluated the clinical- and cost-effectiveness of a new multifaceted and personalised care pathway, compared with usual care, for people with pain at three months after total knee replacement. We report trial participants’ experiences of postoperative pain and the acceptability of the STAR care pathway, which consisted of an assessment clinic at three months, and up to six follow-up telephone calls over 12 months.
Methods
Semi-structured interviews were conducted with 27 people (10 men, 17 women) between February 2018 and January 2020. Participants were sampled purposively from the care pathway intervention group and interviewed after completion of the final postoperative trial questionnaire at approximately 15 months after knee replacement. Interviews were audio-recorded, transcribed, anonymised and analysed using inductive thematic analysis.
Findings
Many participants were unprepared for the severity and impact of postoperative pain, which they described as extreme and constant and that tested their physical and mental endurance. Participants identified ‘low points’ during their recovery, triggered by stiffening, pain or swelling that caused feelings of anxiety, depression, and pain catastrophising. Participants described the STAR assessment clinic as something that seemed “perfectly normal” suggesting it was seamlessly integrated into NHS care. Even in the context of some ongoing pain, the STAR care pathway had provided a source of support and an opportunity to discuss concerns about their ongoing recovery.
Conclusions
People who have knee replacement may be unprepared for the severity and impact of postoperative pain, and the hard work of recovery afterwards. This highlights the challenges of preparing patients for total knee replacement and suggests that clinical attention is needed if exercise and mobilising is painful beyond the three month postoperative period. The STAR care pathway is acceptable to people with pain after total knee replacement.
Similar content being viewed by others
Introduction
Total knee replacement is a common elective surgical procedure most often performed to improve mobility and relieve pain associated with osteoarthritis. Over 100,000 primary knee replacements are usually performed in the United Kingdom’s National Health Service (NHS) annually [1,2,3]. Although knee replacement reduces pain severity for many people, about 20% of those having this operation experience chronic pain afterwards [4, 5]. Chronic postsurgical pain is defined as pain developing or increasing in intensity at three months or longer after surgery [6]. People with chronic postsurgical pain after knee replacement are often dissatisfied with their outcome [3, 7], and struggle physically and mentally with their ongoing pain [8]. Some people describe that that they feel abandoned by healthcare services/professionals [9], or that the advice they receive is unhelpful if told that their pain is a normal part of recovery or that radiography shows no technical or mechanical reason for pain [10]. People who do not seek healthcare for chronic postsurgical knee pain may not do so because a complex mix of physical, social and psychological factors leads them to believe that nothing more can be done for their pain [10].
Current service provision for chronic pain after knee replacement is varied and inconsistent [11]. Complexities and variation in assessment and management of people with chronic postsurgical pain, coupled with a lack of explicit access points to services, means that clinicians often struggle to help [12]. There is an acknowledged need for a comprehensive multidisciplinary approach to manage chronic pain after knee replacement [13].
Based on this pressing need for individualised, targeted care, an applied research programme funded by the National Institute for Health Research (RP-PG-0613–20,001) developed a new care pathway that was evaluated in a pragmatic randomised controlled trial: the Support and Treatment After joint Replacement (STAR) trial [14].
The STAR trial, conducted in eight UK NHS hospitals, evaluated the clinical and cost-effectiveness of the new care pathway [15]. The pathway consisted of early postoperative screening to identify people with ongoing pain and an assessment clinic at three months postoperatively with a trained Extended Scope Practitioner (an allied healthcare professional with specialist orthopaedic training), with up to six follow-up telephone calls over 12 months as required. The 1-h assessment was held 3–4 months after the surgery and involved: clinical history taking, a review of patient reported outcomes including pain, depression, and neuropathic pain. A knee examination involved evaluating the sites and nature of knee tenderness, wound healing, signs of infection, range of motion, and signs of and symptoms of Complex Regional Pain Syndrome as per the Budapest Criteria [16]. Knee radiographs were taken to check implant fixation, alignment, evidence of fracture of concerns with sizing. Blood tests were taken for markers of infection. Further details of the pathway are provided in the previously published trial protocol [15]. The pathway enabled appropriate onwards referral to existing services which included any of the following: a surgeon, if pain was thought to attributable to surgical factors or infection; physiotherapy for exercise and mobility advice and support; a GP for further assessment of depression or anxiety; and/or pain specialists for neuropathic pain or Complex Regional Pain Syndrome (via GPs). Referrals aimed to ensure that underlying reasons for chronic pain were identified early, to prevent pain persistence and ensure that treatment is targeted at likely reasons for pain. The development and refinement of the new pathway and its potential for implementation is described elsewhere [4, 11, 12, 14].
The trial evaluated whether supplementing usual care with the new STAR care pathway improved pain outcomes for people with troublesome pain three months after total knee replacement when compared with usual care alone. The co-primary outcomes for the trial were pain severity and pain interference, assessed using the Brief Pain Inventory [17] at 12 months after randomisation, which was approximately 15 months after surgery. A total of 363 patients with troublesome pain at three months after surgery (defined as a score of ≤ 14 on the Oxford Knee Score Pain subscale [18]) were randomised; 242 to receive usual care and the STAR care pathway and 121 to receive usual care alone. Those who received the STAR care pathway had better pain outcomes than people who received usual care alone, and the care pathway was cost-effective [19].
Qualitative methods embedded within clinical trials can provide insight into how people view interventions, which can add another layer of insight to trial findings [20, 21]. In this article we describe findings from a qualitative study embedded in the STAR trial. The study aimed to explore trial participants’ experiences of the first 15 months after total knee replacement surgery and the STAR care pathway.
Methods
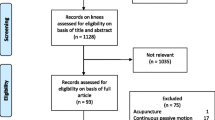
One-to-one, semi-structured interviews were conducted between February 2018 and January 2020 with trial participants allocated to receive the STAR care pathway. A sample of 27 participants (10 men, 17 women) selected from the intervention group were interviewed after they had completed the final postoperative trial questionnaire, at 15 months after their surgery. A purposive sample of 30 participants was planned as an approximation expected to achieve data saturation, so that no new data were identified by the time that data collection was complete. This is in keeping with standards of qualitative research [22]. The sample was chosen purposively to include patients with a range of outcomes (pain severity and interference) to ensure a diversity of experience within the sample. The study received ethical approval from the South West – Central Bristol Research Ethics Committee in July 2016 (REC reference 16/SW/0154) and Health Research Authority approval in August 2016.
Recruitment
Participants were sampled purposively to include people selected from six study sites, all NHS hospitals, across the North, Central and South of England and Wales, and to reflect diversity in outcomes for pain and interference over time, assessed through the Brief Pain Inventory. After return of the 15-month postoperative trial questionnaire, selected trial participants in the intervention group were then sent a letter of invitation and information about the qualitative study, after which they were contacted by telephone to discuss the study and arrange an interview.
Data collection
All interviews were conducted face-to-face in participants’ homes between February 2018 and January 2020. Interviews were conducted by the lead author AJM (male, PhD) with a background in health sociology and extensive qualitative research experience. Interviews lasted between 24 and 76 min (mean: 45 min). All participants provided written informed consent before interview, including consent to audio-recording and publication of anonymised quotations. The topic guide was developed in collaboration with patient representatives (See Additional file 1) and covered experience of the postsurgical period, pain after surgery, experience of the STAR care pathway, and what participants judged had worked or not worked to improve their pain. The interviewer was able to follow up and ask further questions of participants if new or unexpected findings emerged. Interviews took place after participants had completed their final follow-up for the trial to reduce any risk that reflecting on their experiences might affect completion of their 15-month postoperative trial questionnaire.
Analysis
Audio-recordings of the interviews were transcribed, anonymised and uploaded to NVivo 12 data management software [23]. Inductive thematic analysis was undertaken [24]. Transcripts were initially coded inductively on a line-by-line basis by AJM. Coding was descriptive in nature. As similarities and relationships between the codes were established, themes were developed. As coding became more conceptual, moving towards higher levels of abstraction, the themes were refined. For example, some participants described how in the postoperative phase they progressed until their knee began to stiffen or a different kind of pain began to develop, and they began to struggle physically and psychologically. As more participants began to describe similar experiences, this developed into the theme referred to as ‘Low points’. To ensure rigour in the coding process, four transcripts were independently coded and codes were agreed and applied. Double coding was by two other team members with different disciplinary perspectives: RGH (Professor of Health and Anthropology) and WB (Trial Manager).
Results
Participant characteristics
Twenty-seven participants were interviewed, from six of the eight trial sites. Two sites opened to recruitment in the latter part of the trial and their participants had not yet completed 15-month postoperative trial questionnaires by the time of the qualitative study. Out of 30 people invited, three did not take part: one decided that other health problems were their priority, and two did not respond to telephone calls. The final sample included 10 men and 17 women, aged 55 to 84 years (mean: 71 years) (Table 1). Change in pain scores varied across the sample (Table 2).
Main findings
Two thematic domains were developed: The first domain, entitled “The postsurgical journey” includes the severity of postoperative pain; endurance and the hard work of progress; and low points. The second domain describes the “Experiences of the STAR care pathway”, including the acceptability and the perceived benefits of the STAR care pathway. Illustrative quotations relating to our interpretation of experiences can be found in Table 3. All names are fictional to preserve anonymity.
The postsurgical journey
Severity of postoperative pain
The majority of participants spoke about the intensity of postoperative pain, describing it as extreme and constant. A common feature of participants’ accounts was the unremitting and constant nature of pain in the first few weeks postoperatively, up to three months and beyond. Without a reference point such as previous surgery, it is understandable that patients might underestimate the likely degree of pain, but even those who had previous knee replacement surgery struggled to remember how painful it was. Helen kept a diary during her recovery and reflected that she would have forgotten how intense the pain was if she had not documented it. A number of participants believed themselves to have high pain thresholds but were surprised by the intensity and duration of the pain, Josie describing herself as “beaten” by the pain. Participants suggested they would have liked to have had more information before the surgery about pain intensity afterwards.
Endurance and the hard work of progress
When describing their postoperative recovery, participants often spoke about the physical and mental effort required to endure their pain. Caroline described how her experience of recovery had tested her endurance, and that she would recommend surgery only for those “willing to put in the work”. Mandy and Chloe cautioned that unless one could endure and push through the pain, the final outcome could be worse.
Some participants endured pain for long periods, which led to problems sleeping. Deborah described enduring intense postoperative pain for six months, which had affected her sleep as she had to apply ice packs several times throughout the night and keep herself moving to distract herself from the pain. Clive described frustration at his lack of progress, before reasoning and accepting that it was “a part of the process”. Enduring pain for prolonged periods was described as an essential element of recovery.
Caroline described a division of labour which was related to taking back ownership of ‘the knee’. She saw the knee as belonging to the surgeon, initially—“it’s sort of like his knee. He’s put the part in”—but then having worked through her prescribed exercises, she started to do her own exercises. She described feeling a need to take control of her own recovery, and in doing so taking back ownership of her knee, which seemed to be physically and psychologically important to her progression, and part of the ‘work’ of a positive recovery.
Low Points
Many participants described how during the first three months after surgery, and sometimes beyond, they had experienced negative emotions, or a “low point”, typically periods of low mood, feeling depressed and anxious, or worried about their progress. They described a number of reasons for low mood, including: pain; sudden onset of stiffness or swelling; and the realisation that they were not progressing as well as they had hoped, which led to confusion and uncertainty about ongoing symptoms.
The sudden onset of knee stiffening during her third week, led Caroline to feel that she was “going backwards” rather than recovering. This worried her and she felt uncertain about why this apparent regression was happening, despite her adherence to prescribed exercises. Helen also described feeling “weak, hopeless and depressed” at her lack of progress, and by the tenth postoperative week had wondered if something was “really wrong” with her knee. However, by the twelfth week she had begun to make progress in her recovery.
Nora described how she initially felt full of optimism, making good progress in the first five weeks, before then experiencing sudden swelling, which derailed her progression. Chloe also experienced low points related to the onset of stiffening and how this made her exercises difficult and more painful. She described the need to push past this barrier to progress.
Experiences of the STAR care pathway
Acceptability of the STAR assessment clinic and follow-up calls
Impressions of the STAR postoperative assessment clinic varied. Some participants remembered the clinic’s comprehensive and “thorough” approach, characterised by the amount of questions they were asked and radiographs taken. Participants also appreciated the opportunity to ask questions and to talk about their concerns at length with a specialist clinician. Mandy suggested this gave her a sense of being “well looked after”. Some participants spoke of being made to feel welcome, and having a sense of being “fussed over”. Despite the clinic assessment taking an hour or so, Caroline reflected on how efficiently it was run and that it was “not overly intrusive time-wise.”
Other participants saw the STAR assessment clinic as “perfectly normal” while some struggled to remember the clinic as it did not stand out as different to them, from other care they had received. Others were not sure whether they had benefitted specifically from the clinic review, partly because they were unsure which elements of the clinic were novel and how these differed from usual care. For example, Nora wondered if she would have received a referral to the pain clinic regardless of whether she had attended the STAR clinic, and so was unsure whether the clinic had helped. Nora was referred to pain management services after assessment by the STAR clinic. She also received six follow-up telephone calls from the STAR Extended Scope Practitioner, to review her progress and give further advice on pacing activity. It seems likely that because most participants had no previous experience of knee replacement, they saw the STAR clinic as seamlessly integrated into the care that they would usually expect to receive from the NHS. This contributed to the acceptability of the STAR clinic and subsequent follow-up.
Perceived benefits of the STAR assessment clinic and follow-up
We explored which elements of the STAR care pathway worked best for participants. Participants described how the assessment clinic referred them to other treatments/services, but also benefited from psychological support through the efforts of healthcare professionals taking time to focus on their pain and recovery, and to provide care during this assessment.
Elizabeth described feeling encouraged in her efforts to recover because she felt “looked after” by the STAR clinic team and she expressed motivation to reciprocate the efforts of the team by “getting herself right”. Similarly, Anne and Grace described how talking with the STAR Extended Scope Practitioner and the follow-up calls put their minds at rest about their pain, with Grace suggesting that had she not spoken to the ESP she would have gone to hospital otherwise. Others also reported being actively listened to and were reassured by being “checked up on” by clinic staff.
Some participants described how even though subsequent treatments had not resolved their pain, they felt reassured because of the information they had received about the possible cause of their pain. It appears this sense of certainty made their pain more acceptable. For example, Deborah was referred to her orthopaedic surgeon for suspected malalignment who discovered that the prosthesis had indeed worked loose. She described feeling “fortunate” to know the reason for her pain, rather than “going mad” with uncertainty. Similarly, Andy was referred to his surgeon for suspected malalignment. To Andy, knowing the reason for his ongoing pain and that he was not to blame, was a benefit of the STAR clinic. Chloe also derived confidence from the STAR clinic, as it helped her to understand that the pain was not her fault, and that she should continue with her exercises. Although designed to assess and attend to individuals’ needs and to tailor support to reasons for pain, the STAR pathway had not explicitly set out to provide psychological support. This finding was unexpected yet a common experience.
Discussion
We explored the experience of postoperative recovery and of a new care pathway for chronic pain after knee replacement. Previous research shows that patients often struggle with pain in the postoperative period, and that support for ongoing pain following surgery is lacking [9, 10]. Although some participants described ongoing pain, they nonetheless found the STAR care pathway acceptable and provided them with reassurance and confidence in their ongoing recovery. Participants’ descriptions of the STAR clinic as something they would expect to receive, and “perfectly normal” suggests the clinic was seamlessly integrated into NHS care and normalised, at least from the perspective of people with pain. This holds promise for the future implementation potential of the STAR care pathway. Healthcare professionals’ perspectives on the implementation of the STAR care pathway will be reported separately.
Participants valued the opportunity to discuss concerns with a health professional and derived reassurance and encouragement from the clinic and follow-up telephone calls. Self-blame has been acknowledged as a prominent rationalisation for ongoing pain amongst people who have received a total knee replacement [8, 9], and we found that some patients, having received an explanation for their pain during the STAR clinic, felt reassured that it was not their fault. The timeliness of this support and education is important as other recent studies show that support within the three month post-surgery period, could improve patients’ chances of better long-term outcomes [25, 26].
A key finding of the study is that many patients were unprepared for the severity and impact of acute postoperative pain, and this seemed to characterise the recovery of those with suspected chronic postsurgical pain. This aligns with evidence that severe acute postoperative pain is a predictor of chronic postsurgical pain [27,28,29] and whilst many patients recover as expected, a sub-group who experience severe postoperative pain may be most likely to develop chronic postsurgical pain.
While some patients suggested they would have liked more information preoperatively about how much pain they might experience, even those who had previous knee replacement surgery had forgotten the intensity of acute postoperative pain. The phenomenon of diminishing pain recall has been reported in other types of surgery and in experiences of childbirth [30,31,32]. Our findings further highlight the challenges of preparing people for the intensity and duration of pain they may experience after total knee replacement. In the NHS, patients often receive information during a preoperative clinic about what to expect before and after surgery. Future research might focus on understanding and improving information delivery at preoperative clinics.
Another key finding was our identification of a period between the acute postoperative and three-month time points, during which participants experienced a low point, characterised by depression and anxiety associated with a plateauing of progress, and onset of stiffness, swelling or pain. Standard six-week follow-up appointments often focus on radiological evidence, and if there is no mechanical explanation for ongoing pain, patients can feel uncertain about their progress and fearful about the future [10]. Rehabilitative support during this early postoperative period can be variable [33] and continuity of support is often absent. Participants in our study described pushing through this low point, and different aspects of the experience of postoperative pain related to the idea of recovery as ‘hard work’, requiring both physical effort and the ability to endure and tolerate pain. This might suggest that preventive interventions for pain are required beyond the early postoperative period if exercise and mobilising is painful. The concept of physical and emotional ‘hard work’ has previously been identified in studies of self-management of painful osteoarthritis [34]. We find that the concept is also relevant to the postoperative experience and that the STAR assessment clinic was an opportunity to provide reassurance and encouragement to people who experience these low points and who may have concerns about their progress. May and colleagues suggest that patients have an increasingly important role in managing their illness and recovery “the new proactive work of patient-hood” [35]; the STAR care pathway may enable patients to play a greater part in the management of their recovery. Participants’ account of their postoperative experience and the STAR care pathway suggests that rather than being thought of as a one-off event done to the patient, total knee replacement may be more usefully seen as a treatment that lasts beyond the surgical procedure, requiring multiple specialist input and patient self-management, until patients return as near as possible to their desired state of health. Our findings show the STAR care pathway can ensure the provision of multiple specialist input and provide people with confidence to manage their own recovery.
Strengths and limitations
This study fulfils the criteria specified in the Standards for Reporting Qualitative Research (SRQR), a 21-item checklist for qualitative research [36]. A qualitative approach enabled us to explore the complexity of people’s varied experiences of the STAR care pathway. Our inductive approach allowed us to address the study aims and to identify areas of relevance to study participants. The sample included 27 participants from six hospitals. Participants had diverse outcomes for pain intensity and interference over time, and all had pain after their knee replacement. The sample size provided sufficient data to achieve data saturation, the point at which the collection of further data was unnecessary [22]. The demographics of the trial sample in terms of ethnicity (100% white), mean age (71 years) and gender (63% female) broadly reflects the national population of individuals undergoing total knee replacement at the time of the study (95% white, mean age 69 years, 57% female) [37]. However, a weakness of the study is that the participants were all white, and understanding the experience and acceptability of the STAR care pathway from the perspective of people of other ethnicities would strengthen its validity. Interviewing participants more than 15 months post-surgery may introduce some recall bias. However, patients attended the STAR assessment clinic at 3 months post-surgery with up to 6 follow-up calls over 12 months, which will have reinforced their experiences over time. We are confident that we have identified the aspects most salient to experiences of the STAR intervention and that participants found it acceptable.
In conclusion, we found that after surgery people say that they were unprepared for the severity and impact of postoperative pain after knee replacement. This further highlights the challenges of preparing people for total knee replacement surgery and future research efforts should focus on the best ways of achieving this. We also identified a period between the acute postoperative and three-month time point during which many patients were pushed to the limits of their physical and mental endurance, suggesting that interventions for pain could be recommended beyond the acute postoperative period if pain continues to interfere with exercise and recovery. The STAR care pathway is an acceptable source of care and support for people with chronic postsurgical pain and can provide reassurance and confidence in their ongoing recovery while ensuring they that they receive the most appropriate management for their pain.
Availability of data and materials
Anonymised data may be shared via the University of Bristol Research Data Repository (https://data.bris.ac.uk/data/). Access to the data will be restricted to ensure that data is only made available to bona fide researchers for ethically approved research projects, on the understanding that confidentiality will be maintained and after a Data Access Agreement has been signed by an institutional signatory.
Abbreviations
- ESP:
-
Extended Scope Practitioner
- NHS:
-
National Health Service
- STAR:
-
Support and Treatment After knee Replacement
References
Types of Primary Knee Replacements Undertaken [https://reports.njrcentre.org.uk/knees-all-procedures-activity]
Public Health Scotland. Scottish Arthroplasty Project Annual Report 2020. https://www.arthro.scot.nhs.uk/Reports/Main.html.
Nilsdotter AK, Toksvig-Larsen S, Roos EM. Knee arthroplasty: are patients’ expectations fulfilled? A prospective study of pain and function in 102 patients with 5-year follow-up. Acta Orthop. 2009;80(1):55–61.
Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2(1):e00043.
Lenguerrand E, Wylde V, Gooberman-Hill R, Sayers A, Brunton L, Beswick AD, Dieppe P, Blom AW. Trajectories of pain and function after primary hip and knee arthroplasty: The ADAPT cohort study. PLoS ONE. 2016;11(2):e0149306.
Schug SA, Lavand’homme P, Barke A, Korwisi B, Rief W, Treede R-D. The IASP Taskforce for the Classification of Chronic Pain: The IASP classification of chronic pain for ICD-11: chronic postsurgical or posttraumatic pain. Pain. 2019;160(1):45–52.
Scott CEH, Howie CR, MacDonald D, Biant LC. Predicting dissatisfaction following total knee replacement. J Bone Joint Surg Br. 2010;92-B(9):1253–8.
Woolhead GM, Donovan JL, Dieppe PA. Outcomes of total knee replacement: a qualitative study. Rheumatol (Oxford). 2005;44(8):1032–7.
Jeffery AE, Wylde V, Blom AW, Horwood JP. “It’s there and I’m stuck with it”: patients’ experiences of chronic pain following total knee replacement surgery. Arthritis Care Res (Hoboken). 2011;63(2):286–92.
Moore AJ, Gooberman-Hill R. Why don’t patients seek help for chronic post-surgical pain after knee replacement? A qualitative investigation Health Expect. 2020;23(5):1202–12.
Wylde VMF, Dixon S, Gooberman-Hill R. Service provision for patients with chronic postsurgical pain after total knee replacement: An evaluation of current practice. J Pain Manage. 2014;7:147–54.
MacKichan F, Wylde V, Gooberman-Hill R. Pathways Through Care for Long-Term Pain After Knee Replacement: A Qualitative Study With Healthcare Professionals. Musculoskeletal Care. 2015;13(3):127–38.
Phillips JRA, Howells N, Toms AD. Pain after knee replacement. Knee. 2020;27(5):1667–70.
Wylde V, Howells N, Bertram W, Moore AJ, Bruce J, McCabe C, Blom AW, Dennis J, Burston A, Gooberman-Hill R. Development of a complex intervention for people with chronic pain after knee replacement: the STAR care pathway. Trials. 2018;19(1):61.
Wylde V, Bertram W, Beswick AD, Blom AW, Bruce J, Burston A, Dennis J, Garfield K, Howells N, Lane A, et al. Clinical- and cost-effectiveness of the STAR care pathway compared to usual care for patients with chronic pain after total knee replacement: study protocol for a UK randomised controlled trial. Trials. 2018;19(1):132.
Harden NR, Bruehl S, Perez RSGM, Birklein F, Marinus J, Maihofner C, Lubenow T, Buvanendran A, Mackey S, Graciosa J, et al. Validation of proposed diagnostic criteria (the “Budapest Criteria”) for Complex Regional Pain Syndrome. Pain. 2010;150(2):268–74.
Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain. 2004;5(2):133–7.
Pinedo-Villanueva R, Khalid S, Wylde V, Gooberman-Hill R, Soni A, Judge A. Identifying individuals with chronic pain after knee replacement: a population-cohort, cluster-analysis of Oxford knee scores in 128,145 patients from the English National Health Service. BMC Musculoskelet Disord. 2018;19(1):354.
Wylde VBW, Sanderson S, Noble S, Howells N, Peters T, Beswick A, Blom A, Moore A, Bruce J, Walsh A, Eccleston C, Harris S, Garfield K, White S, Toms A, Gooberman-Hill R. The STAR care pathway for patients with pain at three months after total knee replacement: a multicentre, pragmatic randomised controlled trial. Lancet Rheumatol. 2022;4(3):e188–97.
Cathain A, Thomas KJ, Drabble SJ, Rudolph A, Hewison J. What can qualitative research do for randomised controlled trials? A systematic mapping review. BMJ Open. 2013;3(6):e002889.
Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, Moore L, O’Cathain A, Tinati T, Wight D, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ : Br Med J. 2015;350:h1258.
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, Burroughs H, Jinks C. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907.
QSR International Pty Ltd. NVivo (Version 12). 2018. https://www.qsrinternational.com/nvivo-qualitative-data-analysissoftware/home.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Gandhi R, Mahomed NN, Cram P, Perruccio AV. Understanding the Relationship Between 3-Month and 2-Year Pain and Function Scores After Total Knee Arthroplasty for Osteoarthritis. J Arthroplasty. 2018;33(5):1368–72.
Yang HY, Losina E, Lange JK, Katz JN, Collins JE. Longitudinal Trajectories of Pain and Function Improvement Following Total Knee Replacement. ACR Open Rheumatology. 2019;1(5):308–17.
Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017;10:2287–98.
Lavand’homme PM, Grosu I, France MN, Thienpont E. Pain trajectories identify patients at risk of persistent pain after knee arthroplasty: an observational study. Clin Orthop Relat Res. 2014;472(5):1409–15.
Thomazeau J, Rouquette A, Martinez V, Rabuel C, Prince N, Laplanche JL, Nizard R, Bergmann JF, Perrot S, Lloret-Linares C. Predictive Factors of Chronic Post-Surgical Pain at 6 Months Following Knee Replacement: Influence of Postoperative Pain Trajectory and Genetics. Pain Physician. 2016;19(5):E729-741.
Daoust R, Sirois M-J, Lee JS, Perry JJ, Griffith LE, Worster A, Lang E, Paquet J, Chauny J-M, Émond M. Painful Memories: Reliability of Pain Intensity Recall at 3 Months in Senior Patients. Pain Res Manage. 2017;2017:5983721.
Tasmuth T, Estlanderb A-M, Kalso E. Effect of present pain and mood on the memory of past postoperative pain in women treated surgically for breast cancer. Pain. 1996;68(2):343–7.
Waldenström U, Schytt E. A longitudinal study of women’s memory of labour pain—from 2 months to 5 years after the birth. BJOG. 2009;116(4):577–83.
Smith TO, Dainty JR, Clark EM, Whitehouse MR, Price AJ, MacGregor AJ. Demographic and geographical variability in physiotherapy provision following hip and knee replacement. An analysis from the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. Physiotherapy. 2020;106:1–11.
Ong BN, Jinks C, Morden A. The hard work of self-management: Living with chronic knee pain. Int J Qual Stud Health Well-being. 2011;6(3). https://doi.org/10.3402/qhw.v6i3.7035.
May CR, Eton DT, Boehmer K, Gallacher K, Hunt K, MacDonald S, Mair FS, May CM, Montori VM, Richardson A, et al. Rethinking the patient: using Burden of Treatment Theory to understand the changing dynamics of illness. BMC Health Serv Res. 2014;14:281–281.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for Reporting Qualitative Research: A Synthesis of Recommendations. Acad Med. 2014;89(9):1245–51.
Smith MC, Ben-Shlomo Y, Dieppe P, Beswick AD, Adebajo AO, Wilkinson JM, Blom AW. Rates of hip and knee joint replacement amongst different ethnic groups in England: an analysis of National Joint Registry data. Osteoarthritis Cartilage. 2017;25(4):448–54.
Acknowledgements
The authors would like to acknowledge the following people for their help and input into the STAR research programme: Andrew D Beswick, Tim J Peters, Emily Sanderson, Sian Noble, Ashley W. Blom, David A Walsh, Shaun Harris, Kirsty Garfield, Simon White, Andrew Toms, Andrew Judge, Athene Lane, Fiona MacKichan, Nicolas Ambler, Susan Bridgewater, Leigh Morrison, Gemma Munkenbeck, Candida McCabe, Rowenna Stroud, Kate Button, Nigel Arden, Andrew Price, Rafael Pinedo-Villaneuva, Anushka Soni, Stewart Long, Joanne Adams, and the PEP-R group.
Funding
This study is funded by the National Institute for Health Research (NIHR) [Programme Grant for Applied Research (Grant Reference Number RP-PG-0613–20001)]. The research team acknowledge the support of the NIHR, through the Clinical Research Network. This work was also supported by the NIHR Biomedical Research Centre at University Hospitals Bristol and Weston NHS Foundation Trust and the University of Bristol. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
The Bristol Trials Centre (formed through a merger of the Bristol Randomised Trials Collaboration with another UK Clinical Research Collaboration registered Clinical Trials Unit (CTU)) receives National Institute for Health Research CTU Support Funding to underpin the development and conduct of NIHR-funded trials.
JB is supported from NIHR Research Capability Funding via University Hospitals Coventry and Warwickshire NHS Trust.
The funder had no role in the conduct of the trial, the writing of the manuscript or the decision to submit it for publication. The team was not paid to write this article by a pharmaceutical company or other agency. All authors had full access to the full data in the study and accept responsibility to submit for publication.
Author information
Authors and Affiliations
Contributions
RGH was Chief Investigator. RGH, VW, CE and JB were applicants on the grant application to the NIHR. NH was a collaborator. AM and all named above were involved in the design of the qualitative study. AM led data collection, analysis and interpretation, and RGH, VW, JB, NH, CE and WB contributed to interpretation of the findings. AM drafted the manuscript and all authors revised it for important intellectual content and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
In line with the UK Policy Framework for Health and Social Care Research, and the Declaration of Helsinki, the study received ethical approval from the Southwest – Central Bristol Research Ethics Committee in July 2016 (REC reference 16/SW/0154) and Health Research Authority approval in August 2016. All participants received patient information and gave their informed consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
AM and VW are Associate Editors for BMC Musculoskeletal Disorders. JB, NH, WB, CE and RGH have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
STAR Topic Guide: Participant experience of STAR.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Moore, A., Wylde, V., Bruce, J. et al. Experiences of recovery and a new care pathway for people with pain after total knee replacement: qualitative research embedded in the STAR trial. BMC Musculoskelet Disord 23, 451 (2022). https://doi.org/10.1186/s12891-022-05423-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05423-5