Abstract
Background
Persistent postsurgical pain is a major source of dissatisfaction after knee arthroplasty. Postoperative pain trajectories allow a dynamic view of pain resolution after surgery and might help to identify patients at risk for persistent pain.
Questions/purposes
In this prospective observational study, we examined the relationship between postoperative pain trajectories and persistent pain, specifically neuropathic pain, at 3 months after knee arthroplasty.
Methods
Over a 1-year period, all patients undergoing elective unilateral knee arthroplasty for osteoarthritis by one surgeon were invited to participate in the study, provided they had not had prior knee surgery and their American Society of Anesthesiologists grade was 3 or lower; 128 patients fulfilled these criteria. Patients filled in a diary questioning postoperative pain at rest and during mobilization and maximal pain from Day 1 until Day 8 after surgery. At 3 months, the patients were questioned concerning the presence of persistent pain and its nature and intensity using the Douleur Neuropathique 4 [Neuropathic Pain 4] and Brief Pain Inventory questionnaires. At 3 months, 112 of the 128 patients (87%) were successfully contacted.
Results
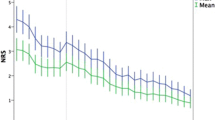
At 3 months, 47 of the 112 (42%) patients were totally pain free and 65 (58%) reported persistent pain at the surgical site. Among the latter, 12 patients (11%) presented with a neuropathic component and more severe persistent pain. Pain trajectories highlighted higher acute pain scores for maximal pain (from Day 1 until Day 8) and for pain at mobilization (from Day 3 until Day 8) in patients with neuropathic persistent pain (p < 0.05 at all time points compared with the no persistent pain group).
Conclusions
Postoperative pain trajectories constructed from patient’s pain diary suggest that a subgroup of patients who will present with higher pain at 3 months after knee arthroplasty might be identified early in the postoperative period and might benefit from preventative treatment.
Level of Evidence
Level III, diagnostic study. See Instructions for Authors for a complete description of levels of evidence.


Similar content being viewed by others
References
Beswick A, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2:e000435.
Bonnet A, Lavand’homme P, France MN, Reding R, De Kock M. [Postoperative pain trajectories to identify risk of chronic postsurgical pain in living donors for liver transplantation] [in French]. Ann Fr Anesth Reanim. 2012;31:945–949.
Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, Bruxelle J, Cunin G, Fermanian J, Ginies P, Grun-Overdyking A, Jafari-Schluep H, Lantéri-Minet M, Laurent B, Mick G, Serrie A, Valade D, Vicaut E. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain. 2005;114:29–36.
Buvanendran A, Kroin J, Della Valle C, Kari M, Moric M, Tuman K. Perioperative oral pregabalin reduces chronic pain after total knee arthroplasty: a prospective, randomized, controlled trial. Anesth Analg. 2010;110:199–207.
Chapman C, Donaldson G, Davis J, Bradshaw D. Improving individual measurement of postoperative pain: the pain trajectory. J Pain. 2011;12:257–262.
Cleeland C, Ryan K. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129–138.
Erdemoglu AK, Koc R. Brief Pain Inventory score identifying and discriminating neuropathic and nociceptive pain. Acta Neurol Scand. 2013 April 18 [Epub ahead of print].
Haroutiunian S, Nikolajsen L, Finnerup N, Jensen T. The neuropathic component in persistent postsurgical pain: a systematic literature review. Pain. 2013;154:95–102.
Hayes C, Browne S, Lantry G, Burstal R. Neuropathic pain in the acute pain service: a prospective study. Acute Pain. 2002;4:45–48.
Johansen A, Romundstad L, Nielsen C, Schirmer H, Stubhaug A. Persistent postsurgical pain in a general population: prevalence and predictors in the Tromso study. Pain. 2012;153:1390–1396.
Kehlet H, Jensen T, Woolf C. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367:1618–1625.
Lavand’homme P. The progression from acute to chronic pain. Curr Opin Anaesthesiol. 2011;24:545–550.
Liu S, Buvanendran A, Rathmell J, Sawhney M, Bae J, Moric M, Perros S, Pope A, Poultsides L, Della Valle C, Shin N, McCartney C, Ma Y, Shah M, Wood M, Manion S, Sculco TP. A cross-sectional survey on prevalence and risk factors for persistent postsurgical pain 1 year after total hip and knee replacement. Reg Anesth Pain Med. 2012;37:415–422.
Macrae WA, Davies HT. Chronic postsurgical pain. In: Crombie IK, Linton S, Croft P, Von Korff M, LeResche L, eds. Epidemiology of Pain. Seattle, WA: IASP Press; 1999:125–142.
Martinez V, Ben Ammar S, Judet T, Bouhassira D, Chauvin M, Fletcher D. Risk factors predictive of chronic postsurgical neuropathic pain: the value of the iliac crest bone harvest model. Pain. 2012;153:1478–1483.
Morze C, Johnson N, Williams G, Moroney M, Lamberton T, McAuliffe M. Knee pain during the first three months after unilateral total knee arthroplasty: a multi-centre prospective cohort study. J Arthroplasty. 2013;28:1565–1570.
Puolakka P, Rorarius M, Roviola M, Puolakka T, Nordhausen K, Lindgren L. Persistent pain following knee arthroplasty. Eur J Anaesthesiol. 2010;27:455–460.
Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983.
Sullivan M, Lynch M, Clark A. Dimensions of catastrophic thinking associated with pain experience and disability in patients with neuropathic pain conditions. Pain. 2005;113:310–315.
Thienpont E. Faster quadriceps recovery with the far medial subvastus approach in minimally invasive total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2013;21:2370–2374.
Torrance N, Smith B, Bennett M, Lee A. The epidemiology of chronic pain of predominantly neuropathic origin: results from a general population survey. J Pain. 2006;7:281–289.
Wylde V, Hewlett S, Learmonth I, Dieppe P. Persistent pain after joint replacement: prevalence, sensory qualities, and postoperative determinants. Pain. 2011;152:566–572.
Wylde V, Rooker J, Halliday L, Blom A. Acute postoperative pain at rest after hip and knee arthroplasty: severity, sensory qualities and impact on sleep. Orthop Traumatol Surg Res. 2011;97:139–144.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Lavand’homme, P.M., Grosu, I., France, MN. et al. Pain Trajectories Identify Patients at Risk of Persistent Pain After Knee Arthroplasty: An Observational Study. Clin Orthop Relat Res 472, 1409–1415 (2014). https://doi.org/10.1007/s11999-013-3389-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-3389-5