Abstract
Background
Serum lactate dehydrogenase (LDH) is a nonspecific inflammatory biomarker and has been reported to be associated with pneumonia prognosis. This study aimed to evaluate the relationship between LDH levels and ventilator-associated pneumonia (VAP) risk in intensive care unit (ICU) patients.
Methods
This retrospective cohort study used data from the Multiparameter Intelligent Monitoring in Intensive Care database from 2001 to 2019. ICU patients aged ≥ 18 years and receiving mechanical ventilation were included. LDH levels were analyzed as continuous and categorical variables (< 210, 210–279, 279–390, > 390 IU/L), respectively. Restricted cubic spline (RCS) curves and quartiles were used to categorize LDH levels. Logistic regression and linear regression were utilized to assess the relationship of LDH levels with VAP risk and duration of mechanical ventilation, respectively.
Results
A total of 9,164 patients were enrolled, of which 646 (7.05%) patients developed VAP. High levels of LDH increased the risk of VAP [odds ratio (OR) = 1.15, 95% confidence interval (CI): 1.06–1.24] and LDH levels were positively correlated with the duration of mechanical ventilation [β = 4.49, 95%CI: (3.42, 5.56)]. Moreover, patients with LDH levels of 279–390 IU/L (OR = 1.38, 95%CI: 1.08–1.76) and > 390 IU/L (OR = 1.50, 95%CI: 1.18–1.90) had a higher risk of VAP than patients with LDH levels < 210 IU/L. Patients with LDH levels of 279–390 IU/L [β = 3.84, 95%CI: (0.86, 6.82)] and > 390 IU/L [β = 11.22, 95%CI: (8.21, 14.22)] (vs. <210 IU/L) had a longer duration of mechanical ventilation.
Conclusion
Elevated serum LDH levels were related to a higher risk of VAP and longer duration of mechanical ventilation and may be useful for monitoring VAP risk.
Similar content being viewed by others
Introduction
Ventilator-associated pneumonia (VAP) is an infection of the lung parenchyma in patients exposed to invasive mechanical ventilation for at least 48 h [1]. VAP is one of the most common acquired pneumonias in intensive care unit (ICU) patients, affecting 5-40% of patients receiving invasive mechanical ventilation [1,2,3]. VAP is associated with increased length of hospitalization, mortality, infections caused by multidrug-resistant pathogens, and a heavy economic burden [4,5,6]. A meta-analysis based on randomized controlled studies showed that the overall attributable mortality rate for VAP was 13%, with higher mortality rates in surgical patients and those with a moderate severity score on admission [7]. Identifying risk factors associated with AVP is important for disease prevention and management.
The endotracheal tube is one of the major risk factors for VAP because it may serve as a reservoir for potentially infectious microorganisms, while at the same time it can bypass host defenses and act as a bridge between the oropharyngeal environment and the sterile bronchoalveolar space [8]. Other risk factors associated with the development of VAP include duration of mechanical ventilation, chronic lung disease, acute respiratory distress, sepsis, red blood cell transfusions, neurologic disorders, and prior antibiotic use [9]. Recently, several studies have reported a relationship between lactate dehydrogenase (LDH) levels and other pneumonia [10,11,12]. LDH levels can be used as a biomarker to predict refractory Mycoplasma pneumoniae pneumonia in early hospitalization [10]. Elevated LDH levels were related to an increased risk of acquired pneumonia [11]. Serum LDH is a metabolic and prognostic biomarker as well as a nonspecific biomarker of inflammation, and high LDH levels are usually associated with poor prognosis [13]. However, the relationship between LDH levels and VAP risk remains unclear. Herein, this study aimed to explore the relationship between LDH levels and VAP risk in ICU patients to provide more evidence for the monitoring of VAP risk.
Methods
Study design and population
Data for this retrospective cohort study were obtained from the Multiparameter Intelligent Monitoring in Intensive Care III and IV (MIMIC-III/IV) database from 2001 to 2019 (https://mimic.mit.edu/docs/iii/). MIMIC-III is a large, publicly available database that collects hospitalization data for more than 40,000 patients admitted to the ICU at Beth Israel Deaconess Medical Center between 2001 and 2012. MIMIC-IV is an updated MIMIC-III and collects hospitalization data for ICU patients between 2008 and 2019. The MIMIC database collects patient demographics, interventions, medical history, clinical measures, clinical laboratory tests, and medical data. Patients were included according to the following criteria: (1) patients who received mechanical ventilation; (2) patients aged ≥ 18 years; and (3) patients who were admitted to the ICU for more than 48 h. Patients with missing LDH levels on the first admission were excluded. MIMIC-III database was approved by the Institutional Review Boards of Beth Israel Deaconess Medical Center and the Massachusetts Institute of Technology, and informed consent was obtained from each patient. In this study, local institutional review board approval and informed consent were not required because MIMIC research data were publicly available and all patient data were de-identified.
Outcomes
The outcome of this study was the occurrence of VAP. Patients with VAP in the MIMIC database were identified based on the International Classification of Diseases 9th edition and 10th edition codes (ICD-9: 4957 and 99,731; ICD-10: J95851). The length of follow-up was from the time the patient was admitted to the ICU to the time the patient was discharged from the hospital or had a VAP. For patients with multiple ICU admissions recorded, only data from the patient’s first ICU admission were analyzed.
Data collection
Patient data were collected including age, gender (male, female), insurance (Medicare, others), weight, heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), respiratory rate, temperature, saturation of peripheral oxygen (SPO2), white blood cell (WBC), international normalized ratio (INR), prothrombin time, vasopressors, antibiotics, sepsis, Sequential Organ Failure Assessment (SOFA) score, Simplified Acute Physiology Score (SAPS) II, Glasgow Coma Score (GCS), Charlson comorbidity index (CCI), myocardial infarction, congestive heart failure, liver disease, malignant cancer, pneumonia, chronic obstructive pulmonary disease (COPD), acute kidney injury (AKI), acute respiratory distress syndrome (ARDS), type of mechanical ventilation (invasive, non-invasive), duration of mechanical ventilation, and LDH levels at admission.
Statistical analysis
Continuous data were presented as median and quartiles [M (Q1, Q3)], and the Mann-Whitney U test was applied to compare differences between groups. Categorical data were presented as numbers and percentages [n (%)], and the Chi-square test or Fisher’s exact test was applied to compare differences between groups.
Confounders associated with VAP risk were screened using the univariable logistic regression model (Supplementary Table S1), and variables with P < 0.05 were included in the multivariable regression models for adjustment (model 2). In addition, a Directed Acyclic Graph (DAG) was applied to elucidate the associations of confounders with LDH and VAP. Potential confounders presented in the DAG were also adjusted for in the multivariate regression models (model 3). The effects of confounders on VAP and duration of mechanical ventilation were presented in Supplementary Tables S2 and S3. The univariable and multivariable logistic regression models were utilized to explore the relationship between LDH levels and VAP risk, and results were presented as odds ratio (OR) and 95% confidence interval (CI). LDH levels were analyzed as continuous and categorical variables, respectively. Restricted cubic spline (RCS) curves were utilized to explore the relationship between LDH levels and VAP risk. LDH levels were categorized into four groups [< Q1 (< 210 IU/L), Q1-cutoff value (210–279 IU/L), cutoff value-Q3 (279–390 IU/L), > Q3 (> 390 IU/L)] based on the quartiles of LDH and the cutoff values of the RCS curves. The association between LDH levels and the risk of VAP was stratified according to type of mechanical ventilation (invasive, non-invasive), duration of mechanical ventilation (≤ 27.2 h, > 27.2 h), sepsis (no, yes), and antibiotics (no, yes). Moreover, the linear regression models were utilized to analyze the relationship between LDH levels and duration of mechanical ventilation, and results were expressed as beta values (β) and 95%CI. Statistical analyses were conducted using R 4.2.0 software (Institute for Statistics and Mathematics, Vienna, Austria). A P-value < 0.05 was considered statistically significant.
Results
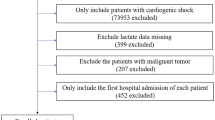
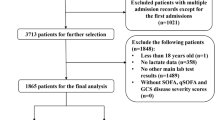
Characteristics of patients
A total of 10,248 patients who received mechanical ventilation were recorded in the MIMIC database between 2001 and 2019. After screening, 1,084 patients were excluded and 9,164 patients were included in the analysis (Fig. 1). The characteristics of these 9,164 patients were listed in Table 1. The median age of patients was 65.0 (53.7, 77.0) years and 5,189 (56.6%) patients were male. The median duration of mechanical ventilation was 27.2 (12.0, 56.0) hours and 4,495 (49.1%) patients received invasive mechanical ventilation. There were 4,389 (47.9%) patients who received vasopressors and 6,948 (75.8%) patients received antibiotics. The median LDH levels were 279.0 (210.0, 390.0) IU/L. There were 646 (7.0%) patients who developed VAP and 8,518 (93.0%) patients who did not.
Relationship between LDH levels and VAP risk and duration of mechanical ventilation
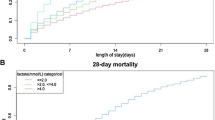
The RCS curves showed that the risk of VAP increased with the increase of LDH levels (Fig. 2). The incidence of VAP and duration of mechanical ventilation in the four LDH level groups was presented in Supplementary Figure S1. The incidence of VAP and duration of mechanical ventilation increased in stages in the group with higher LDH levels.
The relationship between LDH levels and VAP risk was showed in Table 2. The results demonstrated that high levels of LDH increased the risk of VAP (OR = 1.24, 95%CI: 1.16–1.34) when LDH was used as a continuous variable. After adjusting for age, gender, insurance, sepsis, DBP, SOFA, SAPS II, GCS, CCI, type of mechanical ventilation, duration of mechanical ventilation, vasopressors, antibiotics, liver disease, malignant cancer, AKI, and ARDS (model 2), high levels of LDH increased the risk of VAP (OR = 1.12, 95%CI: 1.03–1.21). After adjustment for confounders in DAG (model 3: age, gender, sepsis, SOFA, SAPS II, GCS, CCI, liver disease, malignant cancer, AKI, and ARDS) (Fig. 3), high levels of LDH were still associated with a higher risk of VAP (OR = 1.15, 95%CI: 1.06–1.24). When LDH was used as a categorical variable, patients with LDH levels of 279–390 IU/L (OR = 1.51, 95%CI: 1.19–1.92) and > 390 IU/L (OR = 1.86, 95%CI: 1.48–2.35) had a higher risk of VAP than patients with LDH levels < 210 IU/L in univariable analysis, but not in patients with LDH levels of 210–279 IU/L (P = 0.267). Moreover, patients with LDH levels of 279–390 IU/L (OR = 1.38, 95%CI: 1.08–1.76) and > 390 IU/L (OR = 1.50, 95%CI: 1.18–1.90) still had a higher risk of VAP than patients with LDH levels < 210 IU/L after adjustment for confounders (model 3).
A Directed Acyclic Graph (DAG) for elucidating the associations of confounders with lactate dehydrogenase (LDH) levels and ventilator-associated pneumonia (VAP). Variables associated with both LDH and VAP (potential confounders) were adjusted for in multivariable analyses, whereas mediators were not adjusted. SOFA, Sequential Organ Failure Assessment score; SAPSII, Simplified Acute Physiology Score II; GCS, Glasgow Coma Score; CCI, Charlson comorbidity index, ARDS, acute respiratory distress syndrome
The results of the stratified analysis between LDH levels and VAP risk were shown in Fig. 4. In patients with different types of mechanical ventilation, only non-invasive mechanical ventilation patients with LDH levels > 390 IU/L (vs. <210 IU/L) (P < 0.05) had a higher risk of VAP. Among patients with a duration of mechanical ventilation < 27.2 h, the risk of VAP was higher in patients with LDH levels > 390 IU/L (vs. <210 IU/L) (P < 0.05). Patients with sepsis who had LDH levels > 390 IU/L (vs. <210 IU/L) (P < 0.05) were at increased risk for VAP. Moreover, patients who did not receive antibiotics had an increased risk of VAP at LDH levels of 279–390 IU/L and > 390 IU/L (P < 0.05) (vs. <210 IU/L) increased the risk of VAP.
Stratified analysis of the association between lactate dehydrogenase (LDH) levels and ventilator-associated pneumonia (VAP) risk. OR, odds ratio; CI, confidence interval. All analyses were multivariable logistic regression analysis adjusted for age, gender, insurance, sepsis, DBP, SOFA, SAPS II, GCS, CCI, type of mechanical ventilation, duration of mechanical ventilation, vasopressors, and antibiotics
The relationships between LDH levels and the duration of mechanical ventilation were presented in Table 3. LDH levels were positively correlated with the duration of mechanical ventilation in univariable [β = 6.60, 95%CI: (5.52, 7.67)] and multivariable [β = 4.49, 95%CI: (3.42, 5.56)] analyses when LDH was used as a continuous variable. When LDH was used as a categorical variable, patients with LDH levels of 279–390 IU/L [β = 3.84, 95%CI: (0.86, 6.82)] and > 390 IU/L [β = 11.22, 95%CI: (8.21, 14.22)] (vs. <210 IU/L) had a longer duration of mechanical ventilation in multivariable analysis.
Discussion
This study examined the association between LDH levels and the risk of VAP in patients receiving mechanical ventilation. High LDH levels increased the risk of VAP in patients with mechanical ventilation. Moreover, high LDH levels were associated with a longer duration of mechanical ventilation.
VAP is one of the most common acquired infections in ICU patients [1]. Mechanical ventilation damages the tracheal epithelium, resulting in increased infection by environmental microorganisms and migration of environmental microorganisms in the respiratory tract [14]. Microaspiration and biofilm formation are the two most important mechanisms by which VAP occurs [8]. Microaspiration occurs when microorganisms in secretions that accumulate above the endotracheal tube cuff migrate distally [15]. Secretions and attached microorganisms form a network, or biofilm, that migrates along the endotracheal tube cuff aggregates and inside the lumen of the endotracheal tube, thereby facilitating transfer to the sterile bronchial tree [16]. Oropharyngeal contents may be introduced into the airway during endotracheal intubation, and some studies have shown that bacteria have been observed to colonize endotracheal tubes after several hours of mechanical ventilation [17]. LDH is a widespread enzyme and a nonspecific biomarker of inflammation, and LDH levels may be elevated during inflammatory processes [10]. Several studies have reported the associations of high LDH levels with acquired pneumonia, mycoplasma pneumoniae pneumonia, and complicated pneumonia [10,11,12]. High LDH levels increase the risk of death in patients with acquired pneumonia [11]. Serum LDH is a significant factor in predicting mycoplasma pneumoniae pneumonia, and the area under the curve of the LDH prediction effect reaches 0.718 [10]. Elevated LDH levels are significantly associated with prolonged hospitalization in patients with complicated pneumonia [12]. Our results demonstrated that elevated LDH levels increased the risk of VAP in patients with mechanical ventilation, which was consistent with previous findings in the association between LDH and mycoplasma pneumoniae pneumonia [10]. In addition, our results showed that high LDH levels were related to a longer duration of mechanical ventilation. Duration of mechanical ventilation is a risk factor for the development of VAP [18]. However, the relationship between serum LDH levels and duration of mechanical ventilation has rarely been reported in previous studies. In conclusion, elevated LDH levels in patients undergoing mechanical ventilation may suggest a high risk of VAP, which may prompt clinicians to intervene promptly to reduce the burden of VAP.
The effect of LDH levels on VAP risk may be related to the function of LDH. Elevated LDH levels reflect tissue or cellular damage and are considered a common sign of tissue or cellular injury, suggestive of viral infection or lung injury [19, 20]. Severe infections may result in cytokine-mediated tissue damage and LDH release [21]. Park et al. showed that pulmonary LDH released during infection is an important target for streptococcus pneumoniae binding via pneumococcal surface protein A and pneumococcal surface protein C, and that pneumococci benefit in vivo by utilizing LDH-A-derived lactic acid [22]. Moreover, serum LDH is a prognostic biomarker for metabolism and immunomonitoring, and elevated serum LDH is associated with immunocompromise [23, 24]. LDH promotes lactate synthesis, which enhances immunosuppressive cells such as macrophages, and suppresses cytolytic cells such as NK cells and cytotoxic T lymphocytes [23]. Low LDH activity provides anti-inflammatory effects by down-regulating various inflammatory mediators (e.g., cytokines, NO) as well as lactate fluctuations that modulate macrophage inflammatory responses [25]. Elevated LDH may lead to hyperactivation of lung tissue inflammation and reduced immune response, all of which are associated with a poor prognosis in patients with severe infections [26, 27]. These roles of LDH may explain the association between elevated LDH levels and increased risk of VAP. However, additional mechanisms of the effect of serum LDH levels on VAP may need to be explored in more studies.
We analyzed the relationship between LDH levels and the risk of VAP in ICU patients, which may provide additional evidence for the recognition of VAP risk factors. Nevertheless, several limitations should be considered. First, the data in the MIMIC database are from a single center, and future studies need multicenter prospective data. Second, we only analyzed the relationship between LDH levels at initial ICU admission and the risk of VAP, whereas the effect of changes in LDH levels after admission to ICU on the risk of VAP is still unclear. Third, the effect of LDH levels on the risk of different types of VAPs is unclear due to database limitations. Fourth, we can only obtain whether patients have VAP after admission to the ICU, but cannot obtain the specific time of VAP occurrence due to the limitations of the MIMIC database.
Conclusions
This study assessed the relationship between LDH levels and the risk of VAP in ICU patients based on a large sample MIMIC database. Elevated serum LDH levels were associated with a higher risk of VAP and a longer duration of mechanical ventilation. Serum LDH levels may be useful as a biomarker for VAP risk monitoring. Future studies may need to investigate the effect of changes in LDH levels on VAP risk based on prospective data.
Data availability
The datasets used and/or analyzed during the current study are available from the MIMIC-III and -IV database, https://mimic.mit.edu/docs/iii/, https://mimic.physionet.org/iv/.
Abbreviations
- VAP:
-
Ventilator-associated pneumonia
- ICU:
-
Intensive care unit
- LDH:
-
Lactate dehydrogenase
- MIMIC:
-
The Multiparameter Intelligent Monitoring in Intensive Care
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- SPO2 :
-
Saturation of peripheral oxygen
- WBC:
-
White blood cell
- INR:
-
International normalized ratio
- SOFA:
-
Sequential Organ Failure Assessment
- SAPS II:
-
Simplified Acute Physiology Score II
- GCS:
-
Glasgow Coma Score
- CCI:
-
Charlson comorbidity index
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- RCS:
-
Restricted cubic spline
References
Papazian L, Klompas M, Luyt CE. Ventilator-associated pneumonia in adults: a narrative review. Intensive Care Med. 2020;46(5):888–906.
Reignier J, Mercier E, Le Gouge A, Boulain T, Desachy A, Bellec F, Clavel M, Frat JP, Plantefeve G, Quenot JP, et al. Effect of not monitoring residual gastric volume on risk of ventilator-associated pneumonia in adults receiving mechanical ventilation and early enteral feeding: a randomized controlled trial. JAMA. 2013;309(3):249–56.
Seguin P, Laviolle B, Dahyot-Fizelier C, Dumont R, Veber B, Gergaud S, Asehnoune K, Mimoz O, Donnio PY, Bellissant E, et al. Effect of oropharyngeal povidone-iodine preventive oral care on ventilator-associated pneumonia in severely brain-injured or cerebral hemorrhage patients: a multicenter, randomized controlled trial. Crit Care Med. 2014;42(1):1–8.
Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R. Guidelines for preventing health-care–associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recommendations and reports: Morbidity and mortality weekly report Recommendations and reports 2004, 53(Rr-3):1–36.
Shorr AF, Zilberberg MD, Kollef M. Cost-effectiveness analysis of a silver-coated endotracheal tube to reduce the incidence of ventilator-associated pneumonia. Infect Control Hosp Epidemiol. 2009;30(8):759–63.
Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, Keohane C, Denham CR, Bates DW. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173(22):2039–46.
Melsen WG, Rovers MM, Groenwold RH, Bergmans DC, Camus C, Bauer TT, Hanisch EW, Klarin B, Koeman M, Krueger WA, et al. Attributable mortality of ventilator-associated pneumonia: a meta-analysis of individual patient data from randomised prevention studies. Lancet Infect Dis. 2013;13(8):665–71.
Fernandez JF, Levine SM, Restrepo MI. Technologic advances in endotracheal tubes for prevention of ventilator-associated pneumonia. Chest. 2012;142(1):231–8.
Guidelines for the management. Of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416.
Lu A, Wang C, Zhang X, Wang L, Qian L. Lactate Dehydrogenase as a Biomarker for Prediction of Refractory Mycoplasma pneumoniae Pneumonia in Children. Respir Care. 2015;60(10):1469–75.
Tao RJ, Luo XL, Xu W, Mao B, Dai RX, Li CW, Yu L, Gu F, Liang S, Lu HW, et al. Viral infection in community acquired pneumonia patients with fever: a prospective observational study. J Thorac Disease. 2018;10(7):4387–95.
Breuer O, Picard E, Benabu N, Erlichman I, Reiter J, Tsabari R, Shoseyov D, Kerem E, Cohen-Cymberknoh M. Predictors of prolonged hospitalizations in Pediatric Complicated Pneumonia. Chest. 2018;153(1):172–80.
Claps G, Faouzi S, Quidville V, Chehade F, Shen S, Vagner S, Robert C. The multiple roles of LDH in cancer. Nat Reviews Clin Oncol. 2022;19(12):749–62.
Mangram AJ, Sohn J, Zhou N, Hollingworth AK, Ali-Osman FR, Sucher JF, Moyer M, Dzandu JK. Trauma-associated pneumonia: time to redefine ventilator-associated pneumonia in trauma patients. Am J Surg. 2015;210(6):1056–61. discussion 1061 – 1052.
Dezfulian C, Shojania K, Collard HR, Kim HM, Matthay MA, Saint S. Subglottic secretion drainage for preventing ventilator-associated pneumonia: a meta-analysis. Am J Med. 2005;118(1):11–8.
Koerner RJ. Contribution of endotracheal tubes to the pathogenesis of ventilator-associated pneumonia. J Hosp Infect. 1997;35(2):83–9.
Adair CG, Gorman SP, Feron BM, Byers LM, Jones DS, Goldsmith CE, Moore JE, Kerr JR, Curran MD, Hogg G, et al. Implications of endotracheal tube biofilm for ventilator-associated pneumonia. Intensive Care Med. 1999;25(10):1072–6.
Awasthi S, Tahazzul M, Ambast A, Govil YC, Jain A. Longer duration of mechanical ventilation was found to be associated with ventilator-associated pneumonia in children aged 1 month to 12 years in India. J Clin Epidemiol. 2013;66(1):62–6.
Bartziokas K, Kostikas K. Lactate dehydrogenase, COVID-19 and mortality. Med Clin. 2021;156(1):37.
Alsolamy S. Middle East respiratory syndrome: knowledge to date. Crit Care Med. 2015;43(6):1283–90.
Martinez-Outschoorn UE, Prisco M, Ertel A, Tsirigos A, Lin Z, Pavlides S, Wang C, Flomenberg N, Knudsen ES, Howell A, et al. Ketones and lactate increase cancer cell stemness, driving recurrence, metastasis and poor clinical outcome in breast cancer: achieving personalized medicine via Metabolo-Genomics. Cell Cycle (Georgetown Tex). 2011;10(8):1271–86.
Park SS, Gonzalez-Juarbe N, Martínez E, Hale JY, Lin YH, Huffines JT, Kruckow KL, Briles DE, Orihuela CJ. Streptococcus pneumoniae Binds to Host Lactate Dehydrogenase via PspA and PspC To Enhance Virulence. mBio 2021, 12(3).
Peng M, Yin N, Chhangawala S, Xu K, Leslie CS, Li MO. Aerobic glycolysis promotes T helper 1 cell differentiation through an epigenetic mechanism. Sci (New York NY). 2016;354(6311):481–4.
Gupta GS. The Lactate and the Lactate dehydrogenase in inflammatory diseases and Major Risk factors in COVID-19 patients. Inflammation. 2022;45(6):2091–123.
Song YJ, Kim A, Kim GT, Yu HY, Lee ES, Park MJ, Kim YJ, Shim SM, Park TS. Inhibition of lactate dehydrogenase a suppresses inflammatory response in RAW 264.7 macrophages. Mol Med Rep. 2019;19(1):629–37.
Drent M, Cobben NA, Henderson RF, Wouters EF, van Dieijen-Visser M. Usefulness of lactate dehydrogenase and its isoenzymes as indicators of lung damage or inflammation. Eur Respir J. 1996;9(8):1736–42.
Van Wilpe S, Koornstra R, Den Brok M, De Groot JW, Blank C, De Vries J, Gerritsen W, Mehra N. Lactate dehydrogenase: a marker of diminished antitumor immunity. Oncoimmunology. 2020;9(1):1731942.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (No. 81571916 and 81201478), Key Research and Development Program of Zhejiang Province (No. 2024C03186), Major Project of National-Zhejiang Provincial Administration of Traditional Chinese Medicine (No. GZY-ZJ-KJ-24030), General items of Hangzhou Health Science and Technology program (No. B20220306), and Hangzhou government supports science and technology in the development of bio-pharmaceutical and health industries (No. 2021WJCY390).
Author information
Authors and Affiliations
Contributions
XQ and YX designed the study and XQ wrote the manuscript. XQ, YS, and YJ collected, analyzed, and interpreted the data. YX critically reviewed, edited, and approved the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
MIMIC-III database was approved by the Institutional Review Boards of Beth Israel Deaconess Medical Center and the Massachusetts Institute of Technology, and informed consent was obtained from each patient. In this study, local institutional review board approval and informed consent were not required because MIMIC research data were publicly available and all patient data were de-identified.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qian, X., Sheng, Y., Jiang, Y. et al. Association between lactate dehydrogenase and ventilator-associated pneumonia risk: an analysis of the MIMIC database 2001–2019. BMC Pulm Med 24, 273 (2024). https://doi.org/10.1186/s12890-024-03084-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03084-9