Abstract
Background
Although postoperative pulmonary infection (POI) commonly occurs in patients with esophageal cancer after curative surgery, a patient-specific predictive model is still lacking. The main aim of this study is to construct and validate a nomogram for estimating the risk of POI by investigating how perioperative features contribute to POI.
Methods
This cohort study enrolled 637 patients with esophageal cancer. Perioperative information on participants was collected to develop and validate a nomogram for predicting postoperative pulmonary infection in esophageal cancer. Predictive accuracy, discriminatory capability, and clinical usefulness were evaluated by calibration curves, concordance index (C-index), and decision curve analysis (DCA).
Results
Multivariable logistic regression analysis indicated that length of stay, albumin, intraoperative bleeding, and perioperative blood transfusion were independent predictors of POI. The nomogram for assessing individual risk of POI indicated good predictive accuracy in the primary cohort (C-index, 0.802) and validation cohort (C-index, 0.763). Good consistency between predicted risk and observed actual risk was presented as the calibration curve. The nomogram for estimating POI of esophageal cancer had superior net benefit with a wide range of threshold probabilities (4–81%).
Conclusions
The present study provided a nomogram developed with perioperative features to assess the individual probability of infection may conducive to strengthen awareness of infection control and provide appropriate resources to manage patients at high risk following esophagectomy.
Similar content being viewed by others
Introduction
Esophageal cancer (EC) was diagnosed with 572,034 new cases and results in 508,585 deaths around the world in 2018 [1]. The past few decades have seen a rapid increase in the incidence of esophageal cancer [2]. Although multimodal therapy is composed of surgical treatment, radiotherapy, and chemotherapy, prognosis outcomes remain poor for EC, with only 15–25% of patients surviving beyond 5 years [3]. For patients with esophageal cancer, esophagectomy remains the primary option for esophageal cancer patients because of removing the tumors of the esophagus and improving symptoms. Despite the incidence and mortality of esophageal cancer decline resulting from medical advances and perioperative management, postoperative pulmonary complications, especially postoperative pulmonary infection (POI), which is a principal problem associated with patient’s prognosis and outcomes [4]. Several studies reported that POI occurred in almost 16–40% of EC patients and has been identified to be a factor for perioperative death and long-term survival [5,6,7]. It needs to, therefore, distinct and identify those patients at the greatest risk of POI, and promote early intervention to reduce its incidence or improve postoperative prognosis outcomes. A study observed that the increasing POI rate was connected with several risk factors such as age, smoking, preoperative comorbidity, lower hemoglobin, higher creatinine, postoperative dysphagia [8,9,10]. However, the risk factors of POI following esophageal cancer resection are inconclusive, showing the differences in institutions and healthcare delivery facilities.
Construct a mathematical model to predict POI may be a solution to the issue. A nomogram is a graphical depiction that presents a regression model in a friendly manner and simplifies risk assessment, offering healthcare practitioners a user-friendly interface to map the probability of an event to individual patients and enhancing clinical decision-making of both medical personnel and patients [11, 12]. Such a device would strengthen the validity and objectivity of risk assessment. Therefore, this study seeks to develop and validate a nomogram for predicting POI with perioperative information.
Methods
Study population
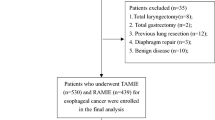
This retrospective cohort study involved adult patients with a newly diagnosed EC from January 1, 2018, to December 31, 2019 at the Shandong Provincial Hospital. Study samples and treatment data were retrieved from the database of respective surgical departments. Patients will be included in this study if they meet the following requirements: (1) aged 18 years or older (2) pathological section diagnosed as malignant esophageal cancer (3) underwent curative esophagectomy. On the other hand, if EC patients who died within 24 hours after surgery or lack complete case records were excluded. The data used in this study was approved by the Institutional Review Board of Shandong University, and was exempt from the requirement for individual patient consent because contained no personal identifiers. The study complied with the principles of Declaration of Helsinki.
Study outcomes and data collection
The primary endpoint POI, definition referred to Centers for Disease Control and Prevention and National Healthcare Safety Network surveillance definition [13]. Pathological staging was performed according to the American Joint Committee on Cancer (AJCC) Staging Handbook (7th edition) [14].The following data were collected: gender, age, length of stay, body mass index, smoking, drinking, hypertension, diabetes mellitus, coronary heart disease, chronic obstructive pulmonary disease, pulmonary tuberculosis, tumor type, primary tumor site, AJCC pathological stage, AJCC clinical stage, chemoradiotherapy, lymph node metastasis, forced vital capacity, forced vital capacity percentage predicted, forced expiratory volume in one second, forced expiratory volume in one second percentage predicted, albumin, hemoglobin, pattern of anastomosis, surgery time, intraoperative bleeding, perioperative blood transfusion, American Society of Anesthesiologists score, postoperative pulmonary infection.
Statistical analysis
Continuous variables were reported as mean with standard deviation (SD) and categorical variables as frequency with percentage. The Least absolute shrinkage and selection operator (LASSO) regression model was performed to tackle the collinearity of candidate variables to select the optimal predictive variables [15]. Multivariable logistic regression analysis was generated using selected predictors from LASSO analysis. The features were presented as odds ratio (OR) and 95% confidence interval (CI). A two-tailed P value < 0.05 was considered statistical significance. Model discrimination was assessed by concordance index (C-index) and calibration was evaluated by calibration curve. Decision curve analysis (DCA) was adopted to determine the clinical usefulness and net benefit of the nomogram [16]. Externally validation was generated to confirm the stability of the nomogram in the validation cohort using 1000 bootstrap resamples and calculating a relatively corrected C-index. Statistical analyses were carried out using SPSS, version 25.0 and R Studio, version 4.0.2.
Results
Population characteristics
Table 1 shows the clinical characteristics of the study population. A total of 637 EC patients were enrolled in this study, separated by training cohort (from January 1, 2018, to July 31, 2019) and validation cohort (from August 1, 2019, to December 31, 2019). Of 446 patients (mean [SD] age, 59.77 [8.3] years; 349 men [78.3%]) in training cohort, 95 patients (21.3%) were diagnosed POI, while 191 patients (mean [SD] age, 58.47[8.7] years; 170 men [89.0%]) composed of validation cohort, 36 patients (18.8%) experienced POI.
Selected predictors
Of 28 features, 4 potential predictors were finally selected on the basis of LASSO regression analysis (Fig. 1). The optimal predictors incorporated length of stay, albumin, intraoperative bleeding, perioperative blood transfusion. Multivariable logistic regression analysis based on four predictors screened from LASSO regression analysis was carried out to create the final model (Table 2).
Perioperative variable selection using a LASSO logistic regression model. (a) Dotted vertical lines were depicted at the optimal values by using the minimum criteria (lambda.min) and 1 SE of the minimum criteria (lambda.1se). (b) LASSO coefficient profile of 28 variables. The coefficient profile is plotted according to the logarithmic sequence. Five-fold cross-validation via minimum criteria was used to determine the optimal predictors of model resulted in four features with nonzero coefficients
Construction and validation of the nomogram
The nomogram for predicting POI in esophageal cancer patients who underwent curative operation was shown in Fig. 2. Model discrimination, as quantified by the C-index, was 0.802 (95% CI 0.752–0.852), indicating the predictive model can better distinguish POI patients from non-POI patients (Fig. 3a). The calibration plot (Fig. 3b) demonstrates good consistency between the predicted risk of POI and the observed actual risk. The clinical value of the nomograms was assessed by decision curve analysis on the basis of the net benefit and threshold probabilities. As for POI of esophageal cancer, the graph (Fig. 3c) suggested the nomogram had superior net benefit with a wide range of threshold probabilities (4–81%). To confirm the stability of the model, we externally validate the nomogram generated in the training cohort. The validation cohort comprised 191 esophagectomy patients from August 1, 2019, to December 31, 2019. The predictive nomogram for assessed individual risk of POI, when applied to the validation cohort with a C-index of 0.763 (95% CI 0.669–0.857).
Discussion
In this study, the incidence of POI was 20.6%, which is comparable to previous findings [17, 18]. The multivariable regression analysis of this retrospective study showed that length of stay, albumin, intraoperative bleeding, and perioperative blood transfusion were independent factors of POI. Identification of destructive and protective factors as well as perioperative management with care delivery can facilitate the control of POI, which furthers clinical prognosis and overall survival [17, 19].
The current study found that length of stay (LOS) accounts for the increasing incidence of POI. This result is in accordance with earlier observation, which showed that extra length of stay attributable to the possibility of developing infection [20]. Prior researchers examined the relationship between LOS and healthcare-associated infection, they found that 1,039 samples of 51,691 patients experienced respiratory infection. A possible explanation for these results is likely to be related to patients with prolonged LOS may undergo bacterial colonization [21].
Our study found that albumin was clinically relevant to the occurrence of respiratory infection. Consistent with the current result, previous study has demonstrated that the rate of respiratory infection occurred in patients with hypoalbuminemia after radical esophagectomy obviously increased [22]. This result may be explained by the fact that hypoalbuminemia contributes to the decrease of plasma osmotic pressure, which induces pulmonary interstitial edema. In addition, reduced gas dispersion and abnormal ventilation to blood flow ratio make pulmonary infections appeal to occur in patients with esophageal cancer. On the other hand, hypoalbuminemia patients were exposed to pulmonary infection by impairing the immunity of patients, which was frequently observed in patients who underwent resection. Moreover, previous researches have noted that hypoalbuminemia played a great role in the prediction value for the mortality and morbidity rates in esophageal cancer population [23].
The multivariate regression analysis revealed that respiratory infection after esophagectomy could be attributed to intraoperative bleeding. With respect to respiratory infection after curative esophagus surgery, several researchers observed that higher blood loss was identified as an independent risk factor for pulmonary infection [19, 24]. Furthermore, for patients with respiratory infection after esophagectomy, greater blood loss was an important indicator of mortality. Increased intraoperative blood loss has been shown to be associated with an increasing incidence of pulmonary complications and hospital death after esophagectomy [25].
In this study, perioperative blood transfusion was found to responsible for POI. There are similarities between the attitudes expressed by researchers in prior studies, they all agreed on the correlation between blood transfusion and increasing susceptibility to pulmonary infection [26, 27]. Perioperative blood transfusion may work collaboratively with operational stress to induce immunosuppression, which was considered as potential mechanisms of increasing in pulmonary infection following esophagectomy [28].
This retrospective study suggested that a nomogram developed with perioperative data to generate personalized evaluates of postoperative pulmonary infection following esophagectomy may distinguish target patients at high risk of pulmonary infection. For example, if a patient was hospitalized for 60 days, had transfused blood, had an albumin level of 25, and had intraoperative bleeding of 800 ml, his total score is approximately 72.5 points corresponded to approximately 93% risk of POI.
This study is subject to certain limitations. In this retrospective study, the type of specific-infected bacteria could not be certain. Moreover, the additional disadvantage of this study was the limited sample of participants. Additionally, the study is limited by the lack of information on sufficient variables. Some potential variables are not accessible in the database, such as patient-related factors (economic status, social support, education level, health knowledge) and perioperative factors (anesthesia method, Intubation method, medication status, other complications).
Conclusions
This research identified that length of stay, albumin, intraoperative bleeding, and perioperative blood transfusion emerged as reliable predictors of POI. The findings indicated that the patient-specific nomogram with external validation may have important implications for paying much attention to EC patients with postoperative infection and help decrease the occurrence of postoperative infection cases. Further studies, which take other clinically-relevant variables into account, will perfect the nomogram.
Availability of data and materials
The datasets are available from the corresponding author on reasonable request.
Abbreviations
- EC:
-
Esophageal cancer
- POI:
-
Postoperative pulmonary infection
- LASSO:
-
Least absolute shrinkage and selection operator
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- C-index:
-
Concordance index
- DCA:
-
Decision curve analysis
- ROC:
-
Receiver operating characteristics
- AUC:
-
Area under the curve
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Hur C, Miller M, Kong CY, Dowling EC, Nattinger KJ, Dunn M, et al. Trends in esophageal adenocarcinoma incidence and mortality. Cancer. 2013;119(6):1149–58.
Pennathur A, Gibson MK, Jobe BA, Luketich JD. Oesophageal carcinoma. Lancet. 2013;381(9864):400–12.
Chevallay M, Jung M, Chon SH, Takeda FR, Akiyama J, Mönig S. Esophageal cancer surgery: review of complications and their management. Ann N Y Acad Sci. 2020;1482(1):146–62.
Weijs TJ, Seesing MF, van Rossum PS, Koëter M, van der Sluis PC, Luyer MD, et al. Internal and external validation of a multivariable model to define hospital-acquired pneumonia after esophagectomy. J Gastrointest Surg. 2016;20(4):680–7.
van der Sluis PC, Verhage RJ, van der Horst S, van der Wal WM, Ruurda JP, van Hillegersberg R. A new clinical scoring system to define pneumonia following esophagectomy for cancer. Dig Surg. 2014;31(2):108–16.
Ohi M, Toiyama Y, Omura Y, Ichikawa T, Yasuda H, Okugawa Y, et al. Risk factors and measures of pulmonary complications after thoracoscopic esophagectomy for esophageal cancer. Surg Today. 2019;49(2):176–86.
Soutome S, Hasegawa T, Yamguchi T, Aoki K, Kanamura N, Mukai T, et al. Prevention of postoperative pneumonia by perioperative oral care in patients with esophageal cancer undergoing surgery: a multicenter retrospective study of 775 patients. Support Care Cancer. 2020;28(9):4155–62.
Dhungel B, Diggs BS, Hunter JG, Sheppard BC, Vetto JT, Dolan JP. Patient and peri-operative predictors of morbidity and mortality after esophagectomy: American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP), 2005–2008. J Gastrointest Surg. 2010;14(10):1492–501.
Zingg U, Smithers BM, Gotley DC, Smith G, Aly A, Clough A, et al. Factors associated with postoperative pulmonary morbidity after esophagectomy for cancer. Ann Surg Oncol. 2011;18(5):1460–8.
Grimes DA. The nomogram epidemic: resurgence of a medical relic. Ann Intern Med. 2008;149(4):273–5.
Levy DA, Li H, Sterba KR, Hughes-Halbert C, Warren GW, Nussenbaum B, et al. Development and validation of nomograms for predicting delayed postoperative radiotherapy initiation in head and neck squamous cell carcinoma. JAMA Otolaryngol Head Neck Surg. 2020;146(5):455–64.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36(5):309–32.
Rice TW, Blackstone EH, Rusch VW. 7th edition of the AJCC Cancer Staging Manual: esophagus and esophagogastric junction. Ann Surg Oncol. 2010;17(7):1721–4.
Liu J, Huang J, Ma S, Wang K. Incorporating group correlations in genome-wide association studies using smoothed group Lasso. Biostatistics. 2013;14(2):205–19.
Hijazi Z, Oldgren J, Lindbäck J, Alexander JH, Connolly SJ, Eikelboom JW, et al. The novel biomarker-based ABC (age, biomarkers, clinical history)-bleeding risk score for patients with atrial fibrillation: a derivation and validation study. Lancet. 2016;387(10035):2302–11.
Nakamura M, Iwahashi M, Nakamori M, Ishida K, Naka T, Iida T, et al. An analysis of the factors contributing to a reduction in the incidence of pulmonary complications following an esophagectomy for esophageal cancer. Langenbecks Arch Surg. 2008;393(2):127–33.
Saunders JH, Yanni F, Dorrington MS, Bowman CR, Vohra RS, Parsons SL. Impact of postoperative complications on disease recurrence and long-term survival following oesophagogastric cancer resection. Br J Surg. 2020;107(1):103–12.
Yoshida N, Watanabe M, Baba Y, Iwagami S, Ishimoto T, Iwatsuki M. Risk factors for pulmonary complications after esophagectomy for esophageal cancer. Surg Today. 2014;44(3):526–32.
Zhou Q, Fan L, Lai X, Tan L, Zhang X. Estimating extra length of stay and risk factors of mortality attributable to healthcare-associated infection at a Chinese university hospital: a multi-state model. BMC Infect Dis. 2019;19(1):975.
Darling JD, McCallum JC, Soden PA, Korepta L, Guzman RJ, Wyers MC, et al. Results for primary bypass versus primary angioplasty/stent for lower extremity chronic limb-threatening ischemia. J Vasc Surg. 2017;66(2):466–75.
Haridas M, Malangoni MA. Predictive factors for surgical site infection in general surgery. Surgery. 2008;144(4):496–501.
Kokudo T, Uldry E, Demartines N, Halkic N. Risk factors for incisional and organ space surgical site infections after liver resection are different. World J Surg. 2015;39(5):1185–92.
Fang W, Kato H, Tachimori Y, Igaki H, Sato H, Daiko H. Analysis of pulmonary complications after three-field lymph node dissection for esophageal cancer. Ann Thorac Surg. 2003;76(3):903–8.
Law S, Wong KH, Kwok KF, Chu KM, Wong J. Predictive factors for postoperative pulmonary complications and mortality after esophagectomy for cancer. Ann Surg. 2004;240(5):791–800.
Miki Y, Makuuchi R, Tokunaga M, Tanizawa Y, Bando E, Kawamura T, et al. Risk factors for postoperative pneumonia after gastrectomy for gastric cancer. Surg Today. 2016;46(5):552–6.
Takeuchi D, Koide N, Suzuki A, Ishizone S, Shimizu F, Tsuchiya T, et al. Postoperative complications in elderly patients with gastric cancer. J Surg Res. 2015;198(2):317–26.
Xiao H, Zhou H, Liu K, Liao X, Yan S, Yin B, et al. Development and validation of a prognostic nomogram for predicting post-operative pulmonary infection in gastric cancer patients following radical gastrectomy. Sci Rep. 2019;9(1):14587.
Acknowledgements
Not applicable.
Funding
This study was funded by the Natural Science Foundation of Shandong Province (Grant numbers ZR2015HM066).
Author information
Authors and Affiliations
Contributions
GW and SL conceived and designed the study. SL, JS, and QS collected and analyzed the data. SL wrote and revised the paper. All authors participated in the drafting and revision of the paper and agreed to the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research was approved by the Institutional Review Board of Shandong University, which was exempt from the requirement for individual patient consent because contained no personal identifiers.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, S., Su, J., Sui, Q. et al. A nomogram for predicting postoperative pulmonary infection in esophageal cancer patients. BMC Pulm Med 21, 283 (2021). https://doi.org/10.1186/s12890-021-01656-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-021-01656-7