Abstract
Background
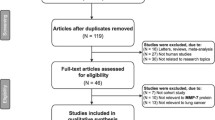
Matrix metalloproteinase 2 (MMP2) has been found to be related to malignant tumors; the aim of this study was to investigate the correlation between MMP2 expression in lung cancer tissues and clinical parameters of lung cancer.
Methods
The expression of MMP2 in lung cancer tissues and in adjacent non-malignant tissues was tested by immunohistochemistry. The correlation between the expression of MMP2 and clinical parameters of lung cancer was analyzed by Kaplan-Meier curve and multiple regression analysis.
Results
The expression of MMP2 was higher in lung cancer tissues than that in adjacent non-malignant tissues (p = 0.002). Increased MMP2 was associated with low differentiation (p = 0.022), tumor size (p = 0.032), lymph node metastasis (p < 0.001), advanced stage (p = 0.002). The post-surgical survival time in patients with high MMP2 expression was shorter than that in patients with low MMP2 expression (p = 0.001). High expression of MMP2 (p = 0.006) and advanced stage (p = 0.003) were independent prognostic indicators for survival of lung cancer patients.
Conclusions
Increased MMP2 correlates with malignant biological behavior of lung cancer and it could be a potential biomarker for diagnosis and prognosis of the disease.
Similar content being viewed by others

Introduction
Lung cancer is divided into non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) in clinical practice [1]. Most lung cancers are NSCLC, which is significantly different from SCLC in pathology, pathogenesis and prognosis [2]. It has been confirmed that many molecular signals are involved in the occurrence and development of lung cancer, which are often related to the abnormal expressions of some proteins. The research on proteomics and genomics has brought a new perspective for the prevention and treatment of lung cancer [3]. Extracellular matrix (ECM) is a complex network structure composed of macromolecular substances secreted by cells into the extracellular matrix. ECM supports and connects tissue structure, and it participates in regulating tissue generation, cell metabolism and signal transduction [4]. Matrix metalloproteinases (MMPs) are enzymes that rely on metal ions such as zinc and calcium to perform their biological functions. It can degrade various protein components in ECM, destroy the histological barrier of tumor cell invasion, and play a key role in tumor invasion and metastasis [5,6,7].
Matrix metalloproteinase 2 (MMP2) is one of the members of MMPs. The gene sequence encoding MMP2 contains 13 exons and 12 introns [8]. The protein size of MMP2 gene translation is about 72 kDa. MMP2 is a zinc-dependent enzyme that can cut extracellular matrix components [9]. It is suggested that MMP-2 is related to the degradation of ECM and plays a role in tumor cell growth, differentiation, invasion, metastasis, regulation of tumor angiogenesis and immune surveillance [10]. Up-regulation of MMP2 has been found in many tumors, and its increase promotes the proliferation, motility and metastasis of malignant tumor cells [11,12,13,14,15]. However, down-regulating the expression of MMP2 can reduce tumor cell proliferation, clonal growth and metastasis, and promote tumor cell apoptosis [16,17,18]. This study detected the expression of MMP2 in lung cancer tissues and analyzed the correlation between its expression level and the clinical characteristics of lung cancer.
Material and methods
Patients
From January 2010 to December 2012, 65 patients were diagnosed with lung cancer and underwent lung cancer resection at the Jining NO.1 People’s Hospital, Jining, China. The lung cancer tissues and the matching adjacent non-malignant tissues (from the edge of the tumor block at least 3 cm) from these patients were collected for a retrospective study. The clinicopathological data of patients are listed in Table 1. All patients were approached based on approved ethical guidelines, and those who agreed to participate in this study were required to sign consent forms. The study was approved by Research Ethics Committee of Jining NO.1 People’s Hospital, Jining, China.
Tissue microarray (TMA) construction
A tissue array instrument was employed to construct the tissue microarray (TMA) (Beecher Instruments, Manual Tissue Arrayer, USA). The representative tumor area on donor wax blocks was screened and the tissue core of 2 mm was perforated from the labeled donor tissue. The tissue core collected was placed into the small hole of the recipient wax mass. Repeatedly, the tissue cores were all placed according to the order of design. After dehydrating and fixing, the TMA block was cut into slices as a thickness of 4.5 μm. Then, the tissue slices were attached to poly-lysine-treated slides and were stored at − 4 °C.
Immunohistochemistry (IHC)
The expression of MMP2 was determined using SABC IHC techniques (SA1094, Bostere Biotech Company, Wuhan, China) according to the introduction of kit. A rabbit anti-human MMP2 monoclonal antibody (BA3716; 1:50 dilution; Bostere Biotech Company, Wuhan, China) was used as the first antibody. The slices of positive staining provided by the antibody kit were served as the positive control. The phosphate buffer saline (PBS) in stead of the first antibody was used as the negative control. Staining intensity and staining area were two semi-quantitative indicators of MMP2 staining. Immunostaining was blindly assessed according to previously published scoring methods [19]. The staining intensity includes the following levels: 0, no staining; 1, mild staining; 2, moderate staining; 3, intense staining. The score for the staining area is as follows: 0, no staining in any fields; 1, < 30% of staining area, 2, between 30 and 60% staining area; 3, > 60% staining area. A combined staining score (intensity + area) of ≤2 was defined as low expression, between 3 and 4 as moderate, and between 5 and 6 was considered as high expression [19].
Statistical analysis
The relationship between the expression of MMP2 in tissues and clinicopathological parameters was analyzed by the Chi-square test, McNemar test and Fisher’s exact test. The definition of patient’s survival is from the date of the operation to the date of death (the death of any cause) or the last known date of the patient’s life (loss of visit). The survival curve was drawn according to kaplan-meier method. The logarithmic rank test was used to determine whether the expression of MMP2 affect the survival of patients. A Cox-proportional risk regression model with multivariate analysis was employed to test the mixed effect of variables with the most closely correlated with the expression levels of MMP2. All tests were two-sided. A statistical significance was that the P value was less than 0.05. The statistical analysis was performed by the SPSS 19.0 software [20].
Results
Expression of MMP2 in lung cancer tissues was higher than that in adjacent normal tissues
In IHC analysis, MMP2 was mainly expressed in cytoplasm and membrane of lung cancer cells and normal cells (Fig. 1a-f). Statistical analysis showed that high expression rate of MMP2 reached 37% (24/65) in lung cancer tissues, whereas only accounted for 20% (13/65) in the adjacent non-malignant tissues, which suggested that the expression of MMP2 in lung cancer tissues was higher than that in adjacent normal tissues (p = 0.002) (Table 2, Fig. 2a).
IHC analysis of MMP2 in lung cancer and normal tissues (IHC × 400). a Low expression of MMP2 in normal tissues. b Low expression of MMP2 in well differentiated LAC. c High expression of MMP2 in poorly differentiated LAC. d High expression of MMP2 in SCLC. e Low expression of MMP2 in well differentiated LSCC. f High expression of MMP2 in poorly differentiated LSCC. MMP2, matrix metalloproteinase 2; SCLC, small cell lung cancer. LAC, lung adenocarcinoma. LSCC, lung squamous cell carcinoma
Correlation between the clinico-pathological features and MMP2 expression in lung cancer tissues. a MMP2 was highly expressed in lung cancer tissues, whereas it was lowly expressed in matched adjacent non-malignant tissues (p < 0.05). b Expression of MMP2 did not relate to the histological type of lung cancer patients (p > 0.05). c Upregulation of MMP2 was observed in poorly differentiated lung cancer tissues compared with well-differentiated tissues (p < 0.05). d Expression of MMP2 in lung cancer tissues at T3–4 stage was significantly higher than that in T1–2 stage (p < 0.05). e MMP2 expression in lung cancer tissues with N0-N1 of lymphnode metastasis was lower than that in those with N2-N3 of lymph node metastasis (p < 0.05). f Increase of MMP2 was displayed in tissues with lung cancer at stages III-IV compared with those at stages I-II (p < 0.05). MMP2, matrix metalloproteinase 2; SCLC, small cell lung cancer. LAC, lung adenocarcinoma. LSCC, lung squamous cell carcinoma. N, node stage (TNM classification)
Highly expressed MMP2 was associated with differentiation, tumor size, lymph node metastasis and clinical stage of lung cancer
Expression of MMP2 was not related to the sex, age, smoking status and histology of lung cancer (p > 0.05) (Table 2, Fig. 2b). However, poorly differentiated lung cancer showed a highly expressed MMP2 (10/19, 52.6%) compared with well differentiated lung cancer (2/14, 14.3%) (p = 0.022) (Table 2, Fig. 2c). Expression of MMP2 in lung cancer at T3–4 stage (12/19, 63.2%) was higher than that in lung cancer at T1–2 stage (8/37, 21.6%) (p = 0.032) (Table 2, Fig. 2d). Expression of MMP2 in lung cancer with N2-N3 (18/33, 54.5%) of lymph node metastasis was up-regulated compared with that in lung cancer with N0-N1 (2/23, 8.7%) (p < 0.001) (Table 2, Fig. 2e). Increased MMP2 was displayed in lung cancer tissues at stages IIIA-IV (13/20, 65%) compared with those of stages IA-IIB (7/36, 19.4%) (p = 0.002) (Table 2, Fig. 2f).
Increased MMP2 in lung cancer tissues was related to shorter survival of lung cancer patients
According to the different expression intensity of MMP2 in patients, it is divided into three cohorts: patients with low expression, patients with moderate expression and patients with high expression. As shown in Table 3, the average survival time for patients with low expression of MMP2 was 45.35 ± 10.85 months (95% Cl: 39.1 to 51.6), for patients with moderate expression was 33.52 ± 7.83 months (95% CI: 30.4 to 36.6) and for patients with high expression was 26.46 ± 8.92 months (95% CI: 22.7 to 30.2). The Kaplan-Meier curves suggested that post-surgical survival time in patients with high MMP2 expression was shorter than that in patients with low MMP2 expression (p = 0.001) (Fig. 3e and f).
Relationship between MMP2 expression in lung cancer tissues and the survival time of lung cancer patients. a The average survival time for patients with low expression of MMP2 was 45.35 ± 10.85 months and for patients with high expression 26.46 ± 8.92 months. b The Kaplan-Meier curves suggested that post-surgical survival time in patients with high MMP2 expression was shorter than that in patients with low MMP2 expression. MMP2, matrix metalloproteinase 2
High expression of MMP2 and advanced stage were independent prognostic indicators for survival of lung cancer patients
A total of 9 variables, gender (X1), age (X2), smoking (X3), histology (X4), differentiation (X5), lymphatic invasion (X6), T stage (X7), TNM (X8), MMP2 (X9)), were included in the multiple regression analysis. The results of analysis showed that high expression of MMP2 (p = 0.006) and advanced stage (p = 0.003) were introduced into regression equation, which means they could be independent prognostic indicators for survival of patients (p < 0.05). The final risk function was H (t) = [h0 (t)] e (2.01X8 + 1.49X9) (Table 4).
Discussion
Compared with normal cells and tissues, the expression of some proteins is often upregulated in lung cancer cells and tissues. Moreover, these up-regulated proteins often have a certain inherent relationship with the malignant biological behavior of lung cancer. So, identification of the abnormal proteins in lung cancer may be of great value in the developing of lung cancer novel diagnostic and therapeutic methods [3]. There is substantial evidence that MMP2 plays a major role in tumor cell-mediated degradation of extracellular matrix and its expression is closely related to the invasion, metastasis and prognosis of human malignant tumors [8, 10, 11, 15]. By testing the expression level of MMP2 in lung cancer tissues, we analyzed the correlation between the MMP2 and the biological behavior of lung cancer. We found that the MMP2 was highly expressed in lung cancer tissues but not in adjacent normal tissues, suggesting that high expression of MMP2 might potentially related to lung cancer occurrence and development. Our findings are consistent with previous reports that MMP2 is highly expressed in lung cancer tissues and lowly expressed in normal tissues [21, 22].
It is well known that the degree of differentiation of lung cancer cells is an independent factor affecting the prognosis of lung cancer patients, which is mainly based on that poorly differentiated lung cancer cells have a high degree of malignancy, and will soon be transferred and relapsed. In our study, we found that MMP2 was highly expressed in poorly differentiated lung cancer tissues, indicating that MMP2 may be associated with the malignant degree of lung cancer. We also found that increased MMP2 in lung cancer tissues correlated with lymph node metastasis and advanced TNM stage. In addition, we noticed that with the increase of tumor volume, the expression of MMP2 showed an increasing trend. These results showed a clear clue that determining the expression of MMP2 could be a valuable strategy for predicting metastatic potential and prognosis of lung cancer. This inference can also be testified by previous research conclusions that MMP2 is associated with the molecular classification of some malignant tumors and has a close relationship with invasiveness, proliferation, lymphatic metastasis, and poor prognosis [8, 11, 12, 15], and our findings are similar to this. This is a positive view that TNM stage correlates with prognosis of cancer patients, which is mainly based on lymph node metastasis, tumor size, and distant metastasis. Our study showed that increased MMP2 significantly correlated with the malignant features of lung cancer such as tumor size, invasion and metastasis of lymph nodes, low differentiation and advanced stage. The findings suggested that MMP2 could be used as a diagnostic and prognostic indicator of lung cancer. Existing literature shows MMP2 not only degrades the basement membrane and matrix to break through the matrix barrier, thus promoting tumor invasion and metastasis, but also accelerates tumor growth and proliferation through neovascularization [9]. Activated transcription factor 1 (ATF1) plays an important role in the migration and invasion of lung cancer cells. A study proposed that the silencing of ATF1 can induce the down-regulation of MMP2 expression, thereby inhibiting the migration and invasion of lung cancer cells [23]. Recent publications and clinical trials have emphasized the potential value of measuring circulating or tissue MMP-2 levels as a tool for tumor diagnosis or prognosis prediction, or as a primary therapeutic target. However, the application of these conclusions to patients is still uncertain, but it is undoubtedly worthy of further efforts [9].
Through the COX regression analysis, we found that lung cancer patients with high-expression of MMP2 had a shorter survival time compared with those with low-expression. In addition, we also found that advanced TNM stage was to be a strong risk factor for shorter survival time of lung cancer patients, with a hazard ratio value of 2.01. In our study, these two factors were implicated into the regression equation and the regression equation was as H(t) = [h0(t)] e (2.01X8 + 1.49X9), which suggested that determining the expression of MMP2 in lung cancer tissues is helpful for predicting the prognosis of lung cancer patients. Our conclusion is similar to previous studies that the high expression of MMP2 in NSCLC was associated with tumor type and clinical stage and has a predictive value for low survival rates, short overall survival (OS) and disease free survival (DFS) [21, 24, 25]. Increased MMP2 correlates with histo-differentiation, lymphatic metastasis, progression, and prognosis of lung cancer, suggesting that it could reflect the situation of progression and migration of lung cancer to a certain extent and that it could be a useful diagnostic, prognostic, and predictive biomarker of lung cancer. A previous study suggests that the expression of MMP2 in lung squamous cell carcinoma is higher than that in lung adenocarcinoma, and its high expression is closely related to lymph node metastasis and TNM staging, and affects the prognosis of patients [21]. However, another study suggests that MMP2 protein has nothing to do with the histology of NSCLC, but its level correlates with poorly differentiated tissue and distant metastasis [22]. These results indicate that the expression of MMP2 in lung cancer is still controversial.
However, There are opinions that MMP2 suppression decreases the expression of hypoxia inducible factor-HIF-1α (HIF-1α) and disrupts phosphoinosmde-3-kinase (PI3K) dependent vascular endothelial growth factor (VEGF) expression, and A549 xenograft tissue sections from mice that treated with MMP-2 small interfering RNA shows reduced expressions of VEGF, providing new insights into the mechanisms underlying MMP2-mediated VEGF expression in lung tumor angiogenesis [26]. Another new study suggests that silibinin inhibits the proliferation, migration, and invasion of triple-negative breast cancer cells by down-regulating the signal of MMP2 [27]. Based on the above results, we can think that MMP2 is associated with the occurrence and development of NSCLC, but the relationship between the two is still certainly unclear. In the future, more multi-center, large-scale studies are still needed to solve this problem. More importantly, the intrinsic mechanism of MMP2 affecting the development of NSCLC remains unclear, A lot of work still needs to be done in this area in the future. There are still some shortcomings in this study. Firstly, most patients of the surgical resection belong to patients with clinical stage IIIB and before, which may lead to a selective bias of the specimen. Secondly, the number of patients included is relatively small. Thirdly, this study did not concern the specific mechanisms by which MMP2 affects the growth, proliferation and metastasis of lung cancer cells. Hence, further experiments involving the mutual regulation-mechanism of MMP2 in lung cancer cells should be done.
Conclusions
First, the expression of MMP2 was increased in lung cancer tissues and increased MMP2 correlated with poorly differentiated cancer, tumor size, lymphatic metastasis and advanced TNM stage. In addition, increase of MMP2 in lung cancer tissues was correlated with shorter survival of patients. Moreover, highly expressed MMP2 is an independent risk factor for poor prognosis of lung cancer patients, suggesting that MMP2 could be a useful diagnostic, prognostic, and predictive biomarker of lung cancer.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABC:
-
Avidin-biotin-peroxidasecomplex
- ATF1:
-
Activated transcription factor 1
- DFS:
-
Disease free survival
- ECM:
-
Extracellular matrix
- EGFR:
-
Epidermal growth factor receptor
- HIF-1α:
-
Hypoxia inducible factor-1α
- IHC:
-
Immunohistochemistry
- MMP2:
-
Matrix metalloproteinase 2
- MMPs:
-
Matrix metalloproteinases
- NSCLC:
-
Non-small cell lung cancer
- OS:
-
Overall survival
- PBS:
-
Phosphate buffer saline
- PI3K:
-
Phosphoinosmde-3-kinase
- SCLC:
-
Small cell lung cancer
- TMA:
-
Tissue microarray
- TMB:
-
Tetramethylbenzidine
- VEGF:
-
Vascular endothelial growth factor
References
Lemjabbar-Alaoui H, Hassan OU, Yang YW, Buchanan P. Lung cancer: biology and treatment options. Biochim Biophys Acta. 2015;1856(2):189–210.
Shtivelman E, Hensing T, Simon GR, Dennis PA, Otterson GA, Bueno R, Salgia R. Molecular pathways and therapeutic targets in lung cancer. Oncotarget. 2014;5(6):1392–433.
Rong B, Nan Y, Liu H, Gao W. Increased stathmin correlates with advanced stage and poor survival of non-small cell lung cancer. Cancer Biomarkers. 2017;19(1):35–43.
Pickup MW, Mouw JK, Weaver VM. The extracellular matrix modulates the hallmarks of cancer. EMBO Rep. 2014;15(12):1243–53.
Gonzalez-Avila G, Sommer B, Mendoza-Posada DA, Ramos C, Garcia-Hernandez AA, Falfan-Valencia R. Matrix metalloproteinases participation in the metastatic process and their diagnostic and therapeutic applications in cancer. Crit Rev Oncol Hematol. 2019;137:57–83.
Yadav L, Puri N, Rastogi V, Satpute P, Ahmad R, Kaur G. Matrix metalloproteinases and cancer - roles in threat and therapy. Asian Pac J Cancer Prev. 2014;15(3):1085–91.
Hadler-Olsen E, Winberg JO, Uhlin-Hansen L. Matrix metalloproteinases in cancer: their value as diagnostic and prognostic markers and therapeutic targets. Tumour Biol. 2013;34(4):2041–51.
Liu RR, Li MD, Li T, Tan Y, Zhang M, Chen JC. Matrix metalloproteinase 2 (MMP2) protein expression and laryngeal cancer prognosis: a meta analysis. Int J Clin Exp Med. 2015;8(2):2261–6.
Henriet P, Emonard H. Matrix metalloproteinase-2: not (just) a “hero” of the past. Biochimie. 2019;166:223–32.
Wang B, Ding YM, Fan P, Xu JH, Wang WX. Expression and significance of MMP2 and HIF-1alpha in hepatocellular carcinoma. Oncol Lett. 2014;8(2):539–46.
Ren F, Tang R, Zhang X, Madushi WM, Luo D, Dang Y, Li Z, Wei K, Chen G. Overexpression of MMP family members functions as prognostic biomarker for breast Cancer patients: a systematic review and Meta-analysis. PLoS One. 2015;10(8):e0135544.
Liu C. Pathological and prognostic significance of matrix metalloproteinase-2 expression in ovarian cancer: a meta-analysis. Clin Exp Med. 2016;16(3):375–82.
Chen Y, Wang X, Chen G, Dong C, Zhang D. The impact of matrix metalloproteinase 2 on prognosis and clinicopathology of breast cancer patients: a systematic meta-analysis. PLoS One. 2015;10(3):e0121404.
Wang HL, Zhou PY, Zhang Y, Liu P. Relationships between abnormal MMP2 expression and prognosis in gastric cancer: a meta-analysis of cohort studies. Cancer Biother Radiopharm. 2014;29(4):166–72.
Wen X, Liu H, Yu K, Liu Y. Matrix metalloproteinase 2 expression and survival of patients with osteosarcoma: a meta-analysis. Tumour Biol. 2014;35(1):845–8.
Lou C, Zhu Z, Zhao Y, Zhu R, Zhao H. Arctigenin, a lignan from Arctium lappa L., inhibits metastasis of human breast cancer cells through the downregulation of MMP-2/−9 and heparanase in MDA-MB-231 cells. Oncol Rep. 2017;37(1):179–84.
Li C, Deng L, Shen H, Meng Q, Qian A, Sang H, Xia J, Li X. O-6-methylguanine-DNA methyltransferase inhibits gastric carcinoma cell migration and invasion by Downregulation of matrix metalloproteinase 2. Anti Cancer Agents Med Chem. 2016;16(9):1125–32.
Poudel B, Ki HH, Luyen BT, Lee YM, Kim YH, Kim DK. Triticumoside induces apoptosis via caspase-dependent mitochondrial pathway and inhibits migration through downregulation of MMP2/9 in human lung cancer cells. Acta Biochim Biophys Sin Shanghai. 2016;48(2):153–60.
Biaoxue R, Xiling J, Shuanying Y, Wei Z, Xiguang C, Jinsui W, Min Z. Upregulation of Hsp90-beta and annexin A1 correlates with poor survival and lymphatic metastasis in lung cancer patients. J Exp Clin Cancer Res. 2012;31:70.
Biaoxue R, Shuanying Y, Wei L, Zongjuan M, Xiguang C, Qiuhong Z. Co-overexpression of Hsp90-beta and annexin A1 with a significantly positive correlation contributes to the diagnosis of lung cancer. Expert Rev Mol Diagn. 2014;14(8):1067–79.
Zhang L, Li N, Yan HC, Jiang H, Fang XJ. Expression of novel CD44st and MMP2 in NSCLC tissues and their clinical significance. Oncol Res Treat. 2017;40(4):192–6.
Jiang LY, Bi R, Ding FB, Wang MS, Mei J, He Y. Prognostic significance of overexpressed matrix metalloproteinase-2, mouse-double minute: 2 homolog and epidermal growth factor receptor in non-small cell lung cancer. J BUON. 2016;21(2):341–8.
Cui J, Yin Z, Liu G, Chen X, Gao X, Lu H, Li W, Lin D. Activating transcription factor 1 promoted migration and invasion in lung cancer cells through regulating EGFR and MMP-2. Mol Carcinog. 2019;58(10):1919–24.
Cao C, Xu N, Zheng X, Zhang W, Lai T, Deng Z, Huang X. Elevated expression of MMP-2 and TIMP-2 cooperatively correlates with risk of lung cancer. Oncotarget. 2017;8(46):80560–7.
Chen GL, Wang SC, Shen TC, Tsai CW, Chang WS, Li HT, Wu CN, Chao CY, Hsia TC, Bau DT. The association of matrix metalloproteinas-2 promoter polymorphisms with lung cancer susceptibility in Taiwan. Chin J Phys. 2019;62(5):210–6.
Chetty C, Lakka SS, Bhoopathi P, Rao JS. MMP-2 alters VEGF expression via alphaVbeta3 integrin-mediated PI3K/AKT signaling in A549 lung cancer cells. Int J Cancer. 2010;127(5):1081–95.
Byun HJ, Darvin P, Kang DY, Sp N, Joung YH, Park JH, Kim SJ, Yang YM. Silibinin downregulates MMP2 expression via Jak2/STAT3 pathway and inhibits the migration and invasive potential in MDA-MB-231 cells. Oncol Rep. 2017;37(6):3270–8.
Acknowledgements
We appreciate the great help of Mr. Zhenqi and Miss Yanyizi as interviewers.
Funding
This work was supported by the Science Foundation of Jining NO.1 People’s Hospital and Affiliated Jining NO.1 People’s Hospital of Jining Medical University, Jining Medical University, China. The funding body did not play a role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
QF J conceived of the study and participated in its design and coordination. LP H, BW S and QD Z collected specimens, organized data, carried out the immunoassays and drafted the manuscript. LP H and W Y participated in the design of the study and performed the statistical analysis. All authors have read and approved the manuscript and ensure that this is the case.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Clinical Research Ethics Committee of Jining NO.1 People’s Hospital, Jining, China. All patients were approached based on approved ethical guidelines, and those who agreed to participate in this study were required to sign consent forms.
Consent for publication
Not applicable.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Han, L., Sheng, B., Zeng, Q. et al. Correlation between MMP2 expression in lung cancer tissues and clinical parameters: a retrospective clinical analysis. BMC Pulm Med 20, 283 (2020). https://doi.org/10.1186/s12890-020-01317-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-020-01317-1