Abstract
Background
Single nucleotide polymorphisms (SNPs) in the genes encoding the vitamin D receptor (VDR) and the vitamin D binding protein (DBP) have been reported to modify the influence of vitamin D deficiency on susceptibility to active tuberculosis (TB) in the UK, but this phenomenon has not been investigated in settings with a high TB burden. SNPs in CYP2R1, which encodes a vitamin D 25-hydroxylase enzyme, are known to influence vitamin D status, but their potential role in determining susceptibility to TB has not previously been investigated in any setting.
Method
We conducted a case–control study in 260 pulmonary TB patients and 112 controls recruited in Lahore, Pakistan. Analyses were conducted to test for main effects of vitamin D status and SNPs in VDR (rs731236, rs2228570 and rs1544410), DBP (rs7041 and rs4588) and CYP2R1 (rs2060793, rs10500804 and rs10766197) on susceptibility to TB, and to investigate whether these SNPs modify the association between vitamin D status and disease susceptibility.
Results
Profound vitamin D deficiency (serum 25-hydroxyvitamin D concentration ≤ 20 nmol/L) was common among TB patients (118/260, 45 %), and was independently associated with susceptibility to TB (adjusted odds ratio 1.87, 95 % CI 1.15 to 3.04, P = 0.01). However, none of the SNPs investigated associated with susceptibility to TB, either in main effects analysis, or in interaction with vitamin D status.
Conclusion
Profound vitamin D deficiency was common among TB patients in this high-burden setting, and was independently associated with disease susceptibility. However, no statistically significant associations between SNPs in the vitamin D pathway and disease susceptibility was demonstrated.
Similar content being viewed by others
Background
Tuberculosis (TB) is a leading global cause of morbidity and mortality, responsible for an estimated 1.5 million deaths in 2014 [1]. The identification of factors which increase disease susceptibility has potential to inform control strategies. Case control studies have previously reported independent associations between vitamin D deficiency and susceptibility to active TB [2]. However, interpretation of such studies is limited by their cross-sectional nature, as they cannot determine whether vitamin D deficiency is a cause or a consequence of active TB. The case for vitamin D deficiency playing a causal role in enhancing disease susceptibility is supported by findings of genetic studies reporting that polymorphisms in the vitamin D receptor (VDR) and the vitamin D binding protein (DBP) genes modify the influence of vitamin D status on susceptibility to active disease in the UK [3, 4]. Only one study is present who have investigated such gene-environment interactions; analogous investigations in high TB burden countries are therefore needed [5]. Moreover, no study has previously investigated whether polymorphisms in the gene encoding the vitamin D hydroxylase enzyme, CYP2R1, are associated with susceptibility to TB, either as a main effect, or as a modifier of the effects of vitamin D status. This gene is a plausible candidate for effect modification, as 25-hydroxylation of ‘parent’ vitamin D3 (cholecaciferol, synthesized in the skin on exposure to ultra-violet B radiation) to form the major circulating vitamin D metabolite 25-hydroxyvitamin D (25[OH]D) is a key determinant of circulating 25(OH)D concentrations [6].
We therefore conducted a case–control study to determine the influence of vitamin D status and single nucleotide polymorphisms (SNPs) in VDR, DBP and CYP2R1 on susceptibility to active TB in Pakistan, a high-burden setting where TB incidence in 2014 was estimated at 270 cases per 100,000 population per year [1]. Having demonstrated an independent association between vitamin D deficiency and susceptibility to active TB in the study population, we proceeded to investigate whether this was modified by SNPs in the vitamin D pathway.
Methods
Study design
We conducted a case control study. Cases were patients aged 14–60 years with newly-diagnosed smear-positive pulmonary TB, recruited from the Gulab Devi Chest hospital, Lahore. Patients with any of the following conditions documented in the hospital record were excluded: diabetes mellitus, ischemic heart disease, chronic renal failure, jaundice or seropositivity for hepatitis B surface antigen, Hepatitis C Virus or Human Immunodeficiency Virus. Controls were healthy relatives of TB patients or hospital staff working at the same hospital with no history of previous tuberculosis but exposed to TB cases. Participants who fulfilled eligibility criteria were asked to complete a questionnaire detailing their age, gender and monthly income. Informed consent was taken from all participants before sample collection. The study was approved from the ethical committee of the University of Punjab (Ref No: SBS 873–12) and also from Gulab Devi Chest Hospital, Lahore.
Five mL of blood were drawn from a median cubital vein; 2 mL were transferred into vials containing EDTA and frozen at −20 °C for subsequent DNA extraction, and 3 mL were added to serum vials and sent to the laboratory within two hours of collection, where serum was isolated from clotted blood by centrifugation and stored at −20 °C for subsequent determination of 25(OH)D concentration.
Serum 25 (OH)D assay
Serum 25(OH)D concentration was determined by ELISA (Immunodiagnostic Systems, Boldon,UK). Calibrators and controls provided with kits were run in duplicate. For the purpose of this study, a patient with 25(OH) vitamin D level equal or less than 20 nmol/L was considered to be vitamin D deficient. Inter-assay CV for serum 25(OH)D assay for our samples was 12.5 %.
Genotyping
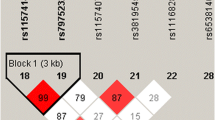
Genomic DNA was extracted from whole blood and quantified using a nanodrop spectrophotometer as previously described [7]. TaqMan allelic probe assays (Applied Biosystems, Foster City, CA, USA) were used to genotype polymorphisms in genes encoding the vitamin D receptor VDR [(rs731236 Taq I), (rs2228570 Bsm I); (rs1544410 Fok I)]; the vitamin D 25-hydroxylase CYP2R1 [(rs2060793, rs10500804, rs10766197)] and the vitamin D binding protein DBP [(rs7041) and (rs4588)]. All primers were commercially prepared. Details of primers used in this study has been provided in Additional file 1. The PCR reaction mixture contained 7.5 μL of TaqMan Genotyping master mixture, 0.75 μL of TaqMan SNP (probes), 1 μL of genomic DNA (1–10 ng), and 5.75 μL nuclease free water. Thermal conditions were as follows: initial denaturation at 95 °C for 10 min, 40 cycles were run at 95 °C for 15 seconds (denaturing) followed by 60 °C for 1 min (annealing/extension). PCR plates were read by 7900HT seq detection system ABI prism.
Sample size and statistical analysis
Sample size was calculated using OpenEpi sample calculator [8] assuming an expected frequency of 57 % vitamin D deficiency in cases and 33 % in controls [9]. Statistical analyses were done with SPSS version 20. Chi square tests were used for univariate analyses exploring potential determinants of vitamin D status and susceptibility to active TB, and binary logistic regression analysis was used for corresponding multivariate analyses. Sub-group analyses were performed to determine whether genetic variation in the vitamin D pathway modified effects of vitamin D status on susceptibility to active TB by repeating primary efficacy analyses with the inclusion of a term for an interaction between vitamin D status and genotype. Odds ratios are presented with 95 % confidence intervals and P-values.
Results
Participant characteristics
A total of 260 cases with smear-positive pulmonary TB and 112 controls were recruited to the study between August 2012 and September 2013. The mean age of cases and controls was 31.6 years (s.d. 10.5 years, range 14–55 years) vs. 30.6 years (s.d. 9.3, range 15–56 years) respectively. Fifty-four percent of cases and 48 % of controls were female. Forty-five percent of cases and 30 % of controls had profound vitamin D deficiency (serum 25[OH]D ≤20 nmol/L), and mean serum 25(OH)D concentration was lower in cases vs. controls (27.3 vs. 43.3 nmol/L respectively, 95 % CI for difference 11.5–22.8, P < 0.0001; Fig. 1).
Determinants of vitamin D status in cases and controls
Table 1 presents determinants of vitamin D status in cases and controls. Vitamin D deficiency was independently associated with female vs. male gender (aOR 2.31, 95 % CI 1.33 to 4.01, P = 0.003; aOR 3.67, 95 % CI 1.38 to 9.70, P = 0.01) and sampling in October-March vs. April-September (aOR 1.89, 95 % CI 1.14 to 3.16, P = 0.01; aOR 2.55, 95 % CI 1.03 to 6.31, P = 0.04) in both case and control populations, respectively (Table 1).
Association between phenotypic features and susceptibility to active tuberculosis
Table 2 presents results of univariate and multivariate analyses testing for associations between participants’ phenotypic features and susceptibility to active TB. Active TB was independently associated with lower monthly income (aOR 1.68, 95 % CI 1.06 to 2.66, P = 0.02) and presence of profound vitamin D deficiency (aOR 1.87, 95 % CI 1.15 to 3.04, P = 0.01). The following phenotypic features were not found to associate with susceptibility to active TB: age, sex, marital status or season of recruitment.
Association between vitamin D pathway genotype and susceptibility to active tuberculosis
Table 3 presents results of analyses testing for associations between genetic variation in VDR, CYP2R1 and DBP and susceptibility to active TB, adjusting for monthly income and vitamin D status. No statistically significant association was observed between susceptibility to active TB and any polymorphism investigated.
Association between vitamin D deficiency and host genotype, stratified by vitamin D status
We next proceeded to investigate whether genetic variation in VDR, DBP or CYP2R1 modified the association between vitamin D deficiency and susceptibility reported above. Results of the pertinent sub-group and interaction analyses are presented in Table 4: these revealed no evidence to support the hypothesis that polymorphisms in the vitamin D pathway modify the effect of vitamin D deficiency on risk of active TB.
Discussion
We report that vitamin D deficiency is very common among TB patients in Pakistan, and that it associates independently with susceptibility to active TB. Risk of deficiency was independently associated with sampling in January - March and with female gender in cases and controls alike. However, we found no evidence to suggest that polymorphisms in CYP2R1, VDR or DBP influenced susceptibility to TB in this population, either as main effects, or in interaction with vitamin D deficiency.
Our finding of an independent association between vitamin D deficiency and susceptibility to active TB is in keeping with previous reports from Pakistan [9] and elsewhere [10]. A prospective study in Pakistan has previously reported that vitamin D deficiency precedes onset of active disease [11], and laboratory studies have reported that vitamin D metabolites induce antimycobacterial activity in vitro [12]: taken together, such reports suggest that vitamin D deficiency plays a causal role in increasing susceptibility to active TB. However, cross-sectional studies such as our own cannot distinguish causality from reverse causality, and the possibility remains that active TB may be a cause, as well as a consequence, of vitamin D deficiency.
By contrast, our study did not replicate previous reports of associations between polymorphisms in VDR and DBP and susceptibility to active TB [4, 13], either as main effects or in interaction with serum 25(OH)D concentration. Neither did we find any such associations for variants in CYP2R1. “A recent study in pulmonary TB in a cohort of HIV-infected and HIV exposed uninfected children in South Africa also showed no association between polymorphisms in VDR, DBP and CYP2R1 and a diagnosis of TB [5]. It should be noted, however, that our study was formally powered to detect associations between vitamin D deficiency and susceptibility to active tuberculosis, rather than genetic associations: the strength of previously reported associations is modest, and we may have lacked power to detect weaker associations. Another limitation of this study is that we collected information on a limited set of confounders. Despite adjustment for these, we cannot exclude the possibility that residual confounding may have contributed to the association seen.
Women participants in this study had lower vitamin D status that was in keeping with our previous reports that female gender is a risk factor for vitamin D deficiency; women may experiencing less sun exposure than men, and may also have lower dietary vitamin D intake [14, 15].
Conclusion
In conclusion, our study reports an independent association between vitamin D deficiency and susceptibility to active tuberculosis in Pakistani adults. However, polymorphisms in VDR, DBP and CYP2R1 were not found to associate with susceptibility to disease in this setting.
Availability of data and materials
Primers used in this study are provided as supplementary information accompanying this paper.
References
WHO: Global tuberculosis report In. Geneva, Switzerland: World Health Organization; 2015.
Martineau AR. Old wine in new bottles: vitamin D in the treatment and prevention of tuberculosis. Proc Nutr Soc. 2012;71(01):84–9.
Wilkinson RJ, Llewelyn M, Toossi Z, Patel P, Pasvol G, Lalvani A, Wright D, Latif M, Davidson RN. Influence of vitamin D deficiency and vitamin D receptor polymorphisms on tuberculosis among Gujarati Asians in west London: a case–control study. Lancet. 2000;355(9204):618–21.
Martineau AR, Leandro ACC, Anderson ST, Newton SM, Wilkinson KA, Nicol MP, Pienaar SM, Skolimowska KH, Rocha MA, Rolla VC. Association between Gc genotype and susceptibility to TB is dependent on vitamin D status. Eur Respir J. 2010;35(5):1106–12.
Gupta A, Montepiedra G, Gupte A, Zeldow B, Jubulis J, Detrick B, Violari A, Madhi S, Bobat R, Cotton M. Low Vitamin-D Levels Combined with PKP3-SIGIRR-TMEM16J Host Variants Is Associated with Tuberculosis and Death in HIV-Infected and-Exposed Infants. PLoS One. 2016;11(2), e0148649.
Wang TJ, Zhang F, Richards JB, Kestenbaum B, Van Meurs JB, Berry D, Kiel DP, Streeten EA, Ohlsson C, Koller DL. Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet. 2010;376(9736):180–8.
Martineau AR, Maclaughlin BD, Hooper RL, Barnes NC, Jolliffe DA, Greiller CL, Kilpin K, McLaughlin D, Fletcher G, Mein CA. Double-blind randomised placebo-controlled trial of bolus-dose vitamin D3 supplementation in adults with asthma (ViDiAs). Thorax. 2015;70(5):451–7.
Sullivan KM, Dean A, Soe MM. OpenEpi: a web-based epidemiologic and statistical calculator for public health. Public Health Rep. 2009;124(3):471.
Iftikhar R, Kamran SM, Qadir A, Haider E, Bin UH. Vitamin D deficiency in patients with tuberculosis. J Coll Physicians Surg Pak. 2013;23(10):780–3.
Nnoaham KE, Clarke A. Low serum vitamin D levels and tuberculosis: a systematic review and meta-analysis. Int J Epidemiol. 2008;37(1):113–9.
Talat N, Perry S, Parsonnet J, Dawood G, Hussain R. Vitamin D deficiency and tuberculosis progression. Emerg Infect Dis. 2010;16(5):853.
Martineau AR, Wilkinson KA, Newton SM, Floto RA, Norman AW, Skolimowska K, Davidson RN, Sørensen OE, Kampmann B, Griffiths CJ. IFN-γ-and TNF-independent vitamin D-inducible human suppression of mycobacteria: the role of cathelicidin LL-37. J Immunol. 2007;178(11):7190–8.
Huang L, Liu C, Liao G, Yang X, Tang X, Chen J. Vitamin D receptor gene foki polymorphism contributes to increasing the risk of tuberculosis: an update meta-analysis. Medicine. 2015;94(51):e2256.
Junaid K, Rehman A, Saeed T, Jolliffe DA, Wood K, Martineau AR. Genotype-independent association between profound vitamin D deficiency and delayed sputum smear conversion in pulmonary tuberculosis. BMC Infect Dis. 2015;15(1):1.
Junaid K, Rehman A, Jolliffe DA, Wood K, Martineau AR. High prevalence of vitamin D deficiency among women of child-bearing age in Lahore Pakistan, associating with lack of sun exposure and illiteracy. BMC Womens Health. 2015;15(1):1.
Acknowledgements
This study was supported by Higher Education Commission of Pakistan grant number BM7-139.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’contributions
KJ designed the study, carried out experimental work and drafted this manuscript; AR helped in study design and drafting this manuscript; DAJ helped in drafting of this manuscript and experimental work, KW carried out genotyping, ARM contributed to study design, statistical analysis and critical review of drafts of the manuscript. All authors read and approved the final manuscript.
Additional file
Additional file 1:
TaqMan allelic assay primers and probes used in real time PCR. (DOCX 12 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Junaid, K., Rehman, A., Jolliffe, D.A. et al. Vitamin D deficiency associates with susceptibility to tuberculosis in Pakistan, but polymorphisms in VDR, DBP and CYP2R1 do not. BMC Pulm Med 16, 73 (2016). https://doi.org/10.1186/s12890-016-0240-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-016-0240-2