Abstract
Background
Inflammatory bowel disease (IBD) consists of two main types: Crohn’s disease (CD) and ulcerative colitis (UC). The epidemiology of IBD patients has not been comprehensively studied in EMRO countries; therefore, we conducted this meta-analysis to study the epidemiology of this disease in these countries.
Methods
We searched four international databases, namely Scopus, Web of Knowledge (ISI), Medline/PubMed, and ProQuest, from inception up to the end of May 2023. The Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guideline was used to carry out this systematic review and meta-analysis investigation. Using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist, the quality of the selected papers was assessed.
Results
Based on the results of this study, the incidence of UC in EMRO countries was 2.65 per 100,000 (95% CI: 1.39–3.90), and the incidence of CD was 1.16 per 100,000 (95% CI: 0.73–1.59). The most commonly involved intestinal segment in CD was the terminal ileum (44.7%, 95% CI: 34.7–55.2), followed by the ileum (29.8%, 95% CI: 22.2–38.6), and colon (18.7%, 95% CI: 10.8–30.4). However, in UC patients, extensive colitis was the most common finding (32.3%, 95% CI: 26.4–38.8), followed by proctosigmoiditis (27.9%, 95% CI: 21.1–35.8), left-sided colitis (27.4%, 95% CI: 22.7–32.7), and proctitis (22.6%, 95% CI: 17.5–28.5).
Conclusion
As a result, we were able to establish the traits of IBD patients in EMRO nations. UC patients had a higher incidence than CD patients. The most common regions of involvement in CD and UC patients, respectively, were the colon and pancolitis. Compared to UC patients, CD patients had a higher history of appendectomy.
Similar content being viewed by others
Introduction
Inflammatory bowel disease (IBD) has two main subtypes contains ulcerative colitis (UC) and Crohn’s disease (CD). This disease is becoming a global concern with increasing prevalence and incidence worldwide [1]. Like other Gastrointestinal diseases, IBD has imposed considerable burden globally along with significant population suffering from this condition [2, 3].
Almost 6.8 million cases of IBD were recognized in 2017 globally with the prevalence rate and death rate of 84.3 and 0.51 respectively [4]. It is estimated 2.5 million people in US and 1 million people in Europe suffering from IBD [2]. According to Global Burden of Disease (GBD) statements, North America and Caribbean were the countries with the highest and lowest prevalence of IBD respectively [4]. A study in the UK revealed that the prevalence of IBD has raised 33.8% between 2006 and 2016 [5]. A time-trend analysis has shown that 75% of CD surveys and 60% of UC studies demonstrated a statistically significant growing incidence [6]. In addition, in a study conducted by Caviglia et al., the incidence of IBD was increased from 200 per 100,000 in 2006 to 321.2 per 100,000 in 2021 presenting an increased rate of 46 percent [7].
IBD may occur as a result of the uncontrolled immune system response, which can originate from genetic or environmental determinants [8]. Environmental factors and hereditary susceptibility are the most important cause of the IBD and its course. These two factors arouse the immune system to act overactive and impaired [9, 10]. Smoking, low physical activity, hygiene status, surgeries, and antibiotic consumption are some environmental factors associated with IBD [11]. Based on the epidemiological models, environmental factors can affect individuals based on a person’s genetic characteristics, including age, gender, personality, and physical state, causing IBD susceptibility [10, 12].
Eastern Mediterranean Regional Office (EMRO) includes 22 countries which is one of the World Health Organization regional classifications [13]. The epidemiology of IBD was studies in the EMRO countries separately but a comprehensive study to assess IBD epidemiology was lacking hence we performed a comprehensive meta-analysis study to investigated epidemiological status of IBD in this region.
Materials and methods
Setting
The goal of the present research project is to determine the epidemiology of IBD in the EMRO nations by a systematic review and meta-analysis. The Systematic Review and Meta-analysis (PRISMA) protocol was used for executing the study [14].
Search strategy
We searched four international databases, namely Scopus, Web of Knowledge (ISI), Medline/PubMed, and ProQuest, from inception up to the end of May 2023. The search strategy and keywords are presented in Table 1.
Inclusion and exclusion criteria
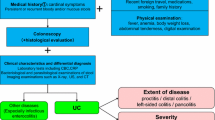
Case–control, cross-sectional, and cohort studies assessing IBD, CD, or UC individuals in the EMRO countries' population with the following criteria were eligible to be included in our study: IBD diagnosis confirmed by clinical characteristics of the individuals and endoscopy or colonoscopy confirmation. At least one of the following outcomes reported: The smoking rate in patients, family history, sites of involvement, risk factors of patients, incidence rate. Studies in English. Available full text. Studies which didn’t fulfill the inclusion criteria were excluded. Two researchers independently selected the studies, and any disagreements were resolved by the third researcher.
Quality assessment
Using The Joanna Briggs Institute (JBI) Critical Appraisal Checklist, two independent researchers conducted the quality assessment of included cross-sectional, case–control, and cohort articles. Any disagreements were finalized by face-to-face consultation and the contribution of a third researcher. The JBI checklist scores of included studies are shown in Table 2.
Data extraction
Included papers were carefully studied by two researchers. The following outcomes were extracted: Name of the first author, year of publication, region of study, duration of study, sample size of study, mean age of participants. The features of included studies are shown in Table 2.
Statistical analysis
Version 2 of the statistical software for comprehensive meta-analysis (CMA) was employed for this investigation. When three trials were available for a particular outcome, the data were pooled. To ascertain the amount of result heterogeneity, Cochran's test (where the significance level was deemed less than 0.1) and I2 statistics (where the significant level was deemed greater than 50%) were obtained. When heterogeneity was significant, the random-effects model was utilized; otherwise, the fixed-effects model was used.
Results
A total of 1671 studies were found in the initial search. After omitting the duplications, 1485 studies underwent screening. Two researchers independently screened the title, abstract, and, when necessary, the full text of the articles. A total of 1416 articles were deleted, and 69 papers underwent full-text revision. Finally, 34 studies that met our inclusion criteria were selected for our study (Fig. 1).
Description of studies
The basic characteristics of the included studies are presented in Table 2 [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48]. Based on the geographical location of the 34 included studies, 14 studies were conducted in Iran, 9 in Saudi Arabia, 3 in Kuwait, 1 in Qatar, 1 in Bahrain, 1 in the UAE, 1 in Lebanon, 1 in Oman, 1 in Pakistan, 1 in Tunisia, and 1 in Egypt. The summary characteristics of the studies are shown in Table 2.
Incidence of IBD patients
According to the results of the meta-analysis, the incidence of UC in EMRO countries was 2.6 per 100,000 (95% CI: 1.3–3.9), and the incidence of CD was 1.16 per 100,000 (95% CI: 0.7–1.5) (Fig. 2A and B).
A Incidence of UC in EMRO countries, B Incidence of UC in EMRO countries, C Prevalence of Ulcerative Colitis among men, D Prevalence of Crohn Disease among men, E Mean Age at diagnosis for Ulcerative Colitis, F Mean Age at diagnosis for Crohn Disease, G Terminal ileum involvement in CD, H Ileal involvement in CD, I Colon involvement in CD
Prevalence of IBD among men and women
Based on our meta-analysis, 46% of Ulcerative Colitis diagnoses in EMRO are from men. However, this number is 55% for Crohn Disease (Fig. 2C and D).
Age at diagnosis
The mean age at diagnosis for Ulcerative Colitis is 32.7 (95% CI: 30.3 to 35.1). In addition, the mean age at diagnosis is 30.9 (95% CI: 27.1 to 34.7) for Crohn Disease (Fig. 2E and F).
Sites of involvement
The distribution of patients with Crohn's disease (CD) and ulcerative colitis (UC) based on the area of intestinal involvement is depicted in Fig. 2G to I and Fig. 3A to D. In CD patients, the terminal ileum was the most frequently affected intestinal segment (44.7%, 95% CI: 34.7–55.2), followed by the ileum (29.8%, 95% CI: 22.2–38.6), and the colon (18.7%, 95% CI: 10.8–30.4). Regarding UC patients, extensive colitis was the most prevalent finding (32.3%, 95% CI: 26.4–38.8), followed by proctosigmoiditis (27.9%, 95% CI: 21.1–35.8), left-sided colitis (27.4%, 95% CI: 22.7–32.7), and proctitis (22.6%, 95% CI: 17.5–28.5).
A Extensive colitis involvement in UC, B Proctosigmoiditis involvement in UC, C Left sided colitis involvement in UC patients, D Proctitis involvement in UC, E Prevalence of smoking in CD patients, F Prevalence of smoking in UC patients, G Prevalence of positive family history in UC patients, H Prevalence of positive family history in CD patients, I (Upper figure): History of appendectomy in CD patients, J (Lower figure): History of appendectomy in UC patients
Smoking
The prevalence of smoking in CD patients (12.2%, 95% CI: 8.2–17.7) was higher than in UC patients (11.0%, 95% CI: 7.8–15.4) (Fig. 3E and F).
Family history
The prevalence of a positive family history in UC and CD was 11.7% (95% CI: 9.2–14.7) and 11.3% (95% CI: 8.6–14.6), respectively (Fig. 3G and H).
History of appendectomy
The history of appendectomy was higher in CD patients (15.5%, 95% CI: 12.9–18.5) compared to UC (4.8%, 95% CI: 2.9–8) (Fig. 3I and J).
Result of heterogeneity assessment
As we used random effect model for our main analyses, we presented the detailed information about possible heterogeneity for each outcome in the Table 3. We also evaluated the distribution of true effect using prediction interval (See supplementary material).
Discussion
In this study we surveyed the epidemiology of IBD in the EMRO countries. We assessed the incidence of IBD, sites of involvement in GI tract and risk factors.
According to the findings of our study, the incidence rates for UC and CD in the EMRO region were 2.65 and 1.16, respectively. Different nations have distinct rates of incidence and prevalence for IBD and its subtypes. The highest frequency of IBD was found in Europe and North America, according to a comprehensive review and meta-analysis by Ng et al. The incidence of IBD in North America and Europe appeared to be steady or declining based on the findings of this study [1]. The annual incidence rate of CD was reported to be 0.5 per 100,000 in Japan and 20.2 per 100,000 in Canada. In Japan, there were 5.8 UC patients per 100,000 people, compared to 319 UC patients per 100,000 people in Canada [49, 50]. The incidence and prevalence of UC were reported to be 0.3 and 7.6 per 100,000 people in South Korea, respectively [51]. In the United States, prior research places the incidence of UC and CD, respectively, at 10.1 to 12 and 6.3 to 7.9 per 100,000 people [52]. By comparing the findings of our study with those of other studies, we have come to the conclusion that the incidence of UC and CD is higher in the EMRO region than in eastern nations like Japan and South Korea, and lower than in eastern nations. We believe this variation is caused by varying genetic vulnerability, environmental circumstances, and lifestyle choices.
With regard to the findings of our study, CD patients had slightly higher incident rate of smoking (12.2%) than UC patients (11%). In a cohort study conducted by Lunney et al., CD patients had a greater prevalence of smoking than UC patients [53]. Smoking is a difficult component in IBD. Even though it increases the risk of CD, patients with UC benefited from it [54,55,56]. Smoking’s impact on IBD patients was shown to follow a dosage response pattern [45]. Smoking’s effects on IBD patients can be influenced by genetic and ethnic factors [57, 58].
Positive family history is one of the major risk factors for IBD patients [59]. A person’s genetic and environmental susceptibilities that they inherited from their parents are reflected in their positive family history in IBD patients [60]. First degree relatives and monozygotic twins have a higher incidence of IBD, which supports the hereditary component to IBD [61]. In this study, we demonstrated that UC (11.7%) and CD (11.3%) have slightly higher positive family history rates. Family members of UC patients were much more numerous than CD patients in a meta-analysis research by Childres et al. [62]. Asian, African American, Hispanic, and White populations all had higher rates of positive family history, ranging from 26 to 33%, 9% to 18%, 9% to 16%, and 5.9%, respectively [63,64,65,66,67].
Based to the results obtained in our study, CD patients were more likely to undergo an appendectomy (15.5%) than UC patients (4.8%). Appendectomy's impact on the course of IBD is debatable. According to research by Andersson et al., appendectomy for inflammatory diseases such appendicitis reduces the incidence of UC [68]. Higher risk of CD and UC after appendectomy was found in a different cohort research by Chung et al. [69]. Five years after surgery, an appendectomy significantly reduced the risk of UC in another trial [70].
CD can affect any part of the gastrointestinal tract in a discontinuous manner, whereas UC is limited to the rectum and colon [71]. In this study, we observed that the most common pattern of GI tract involvement in UC patients is extensive colitis (32.3%), followed by proctosigmoiditis (27.9%). For CD patients, the most frequent pattern of involvement was coloileal, followed by the ileum. Previous studies have reported that proctitis and proctosigmoiditis occur in 46% of UC patients, while left-sided colitis and extensive colitis affect 17% and 37% of UC individuals, respectively [72].
Limitation
Our research had some limitations. First, some of the EMRO region's nations lacked the appropriate literature for our analysis. Second, we do not have adequate data to conduct subgroup analyses based on gender, age, and marital status. Third, we do not have enough information about how many years each patient with IBD has had the disease.
Conclusions
In conclusion, our study identified the characteristics of patients with inflammatory bowel disease (IBD) in EMRO countries. We observed a higher incidence of ulcerative colitis (UC) compared to Crohn's disease (CD) patients. Coloileal involvement was the most common site of disease in CD patients, whereas extensive colitis was the predominant pattern in UC patients. Additionally, a history of appendectomy was more frequent among CD patients than UC patients.
Availability of data and materials
No datasets were generated or analysed during the current study.
References
Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390(10114):2769–78.
Kaplan GG. The global burden of IBD: from 2015 to 2025. Nat Rev Gastroenterol Hepatol. 2015;12(12):720–7.
Keivanlou MH, Amini-Salehi E, Joukar F, Letafatkar N, Habibi A, Norouzi N, et al. Family history of cancer as a potential risk factor for colorectal cancer in EMRO countries: a systematic review and meta-analysis. Sci Rep. 2023;13(1):17457.
GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5(1):17-30. https://doi.org/10.1016/S2468-1253(19)30333-4. Epub 2019 Oct 21.
Freeman K, Ryan R, Parsons N, Taylor-Phillips S, Willis BH, Clarke A. The incidence and prevalence of inflammatory bowel disease in UK primary care: a retrospective cohort study of the IQVIA medical research database. BMC Gastroenterol. 2021;21(1):139.
Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142(1):46-54.e42; quiz e30.
Caviglia GP, Garrone A, Bertolino C, Vanni R, Bretto E, Poshnjari A, et al. Epidemiology of Inflammatory Bowel Diseases: A Population Study in a Healthcare District of North-West Italy. J Clin Med. 2023;12(2):641.
Sairenji T, Collins KL, Evans DV. An Update on Inflammatory Bowel Disease. Prim Care. 2017;44(4):673–92.
Loddo I, Romano C. Inflammatory bowel disease: genetics, epigenetics, and pathogenesis. Front Immunol. 2015;6:551.
Kaser A, Zeissig S, Blumberg RS. Genes and environment: how will our concepts on the pathophysiology of IBD develop in the future? Dig Dis. 2010;28(3):395–405.
Piovani D, Danese S, Peyrin-Biroulet L, Nikolopoulos GK, Lytras T, Bonovas S. Environmental risk factors for inflammatory bowel diseases: an umbrella review of meta-analyses. Gastroenterology. 2019;157(3):647-59.e4.
Levine JS, Burakoff R. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2011;7(4):235–41.
Keivanlou MH, Amini-Salehi E, Hassanipour S, Mahapatro A, Raghuma N, Joukar F, et al. Association between smoking and colorectal cancer in Eastern Mediterranean Regional Office (EMRO): A systematic review and meta-analysis. Saudi J Gastroenterol. 2023;29(4):204–11.
Matthew JP, Joanne EM, Patrick MB, Isabelle B, Tammy CH, Cynthia DM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Al Awar B, Almurbati B. P1188 inflammatory bowel disease in children in United Arab Emirates. J Pediatr Gastroenterol Nutr. 2004;39:S508.
El Mouzan MI, Al Mofarreh MA, Assiri AM, Hamid YH, Al Jebreen AM, Azzam NA. Presenting features of childhood-onset inflammatory bowel disease in the central region of Saudi Arabia. Saudi Med J. 2012;33(4):423–8.
Zobeiri M, Bashiri H, Askari L, Keshavars AA, Tavvafzadeh R, Fatahi K, Najafi F. Epidemiologic characteristics of patients with inflammatory bowel disease in Kermanshah, Iran. Middle East J Dig Dis. 2017;9(3):164–9.
Yazdanbod A, Farzaneh E, Pourfarzi F, Azami A, Mostafazadeh B, Adiban V, Rasouli MR. Epidemiologic profile and clinical characteristics of ulcerative colitis in northwest of Iran: a 10-year review. Trop Gastroenterol. 2011;31(4):308–11.
Siddique I, Alazmi W, Al-Ali J, Longenecker JC, Al-Fadli A, Hasan F, Memon A. Demography and clinical course of ulcerative colitis in Arabs - a study based on the Montreal classification. Scand J Gastroenterol. 2014;49(12):1432–40.
Abdulla M, Al Saeed M, Fardan RH, Alalwan HF, Ali Almosawi ZS, Almahroos AF, Al QJ. Inflammatory bowel disease in Bahrain: single-center experience. Clin Exp Gastroenterol. 2017;10:133–45.
Al-Qabandi WA, Buhamrah EK, Hamadi KA, Al-Osaimi SA, Al-Ruwayeh AA, Madda J. Inflammatory bowel disease in children, an evolving problem in Kuwait. Saudi J Gastroenterol. 2011;17(5):323–7.
Al-Mofarreh MA, Al-Mofleh IA. Emerging inflammatory bowel disease in saudi outpatients: a report of 693 cases. Saudi J Gastroenterol. 2013;19(1):16–22.
Radhakrishnan S, Zubaidi G, Daniel M, Sachdev GK, Mohan AN. Ulcerative colitis in Oman. A prospective study of the incidence and disease pattern from 1987 to 1994. Digestion. 1997;58(3):266–70.
Masoodi M, Agah S, FaghihiKashani A, Eghbali H. Estimation of ulcerative colitis incidence in hormozgan province. Southern Iran Govaresh. 2012;16(4):265–9.
Habibi F, Mahdavi SB, Khaniabadi BM, Habibi ME, Gharavinia A, Baghaei A, Emami MH. Sleep quality and associated factors in Iranian inflammatory bowel disease patients. J Res Med Sci. 2019;24:59.
Abdul-Baki H, ElHajj I, El-Zahabi LM, Azar C, Aoun E, Zantout H, et al. Clinical epidemiology of inflammatory bowel disease in Lebanon. Inflamm Bowel Dis. 2007;13(4):475–80.
Al-Shamali MA, Kalaoui M, Patty I, Hasan F, Khajah A, Al-Nakib B. Ulcerative colitis in Kuwait: a review of 90 cases. Digestion. 2003;67(4):218–24.
Khan HA, Mahrous AS, Fachartz, Khawaja FI. Ulcerative colitis amongst the Saudis: six-year experience from Al-Madinah region. Saudi J Gastroenterol. 1996;2(2):69–73.
Mirmiran P, Moslehi N, Morshedzadeh N, Shivappa N, Hébert JR, Farsi F, Daryani NE. Does the inflammatory potential of diet affect disease activity in patients with inflammatory bowel disease? Nutr J. 2019;18(1):65.
Butt MT, Bener A, Al-Kaabi S, Yakoub R. Clinical characteristics of Crohn s disease in Qatar. Saudi Med J. 2005;26(11):1796–9.
Sayar R, Shokri Shirvani J, Hajian-Tilaki K, Vosough Z, Ranaei M. The negative association between inflammatory bowel disease and Helicobacter pylori seropositivity. Caspian J Intern Med. 2019;10(2):217–22.
Vahedi H, Merat S, Momtahen S, Olfati G, Kazzazi AS, Tabrizian T, et al. Epidemiologic characteristics of 500 patients with inflammatory bowel disease in Iran studied from 2004 through 2007. Arch Iran Med. 2009;12(5):454–60.
Hosseini SV, Safarpour AR, Taghavi SA. Developing a novel risk-scoring system for predicting relapse in patients with ulcerative colitis: A prospective cohort study. Pakistan J Med Sci. 2015;31(6):1511–6.
Aljebreen AM, Alharbi OR, Azzam NA, Almalki AS, Alswat KA, Almadi MA. Clinical epidemiology and phenotypic characteristics of Crohn’s disease in the central region of Saudi Arabia. Saudi J Gastroenterol. 2014;20(3):162–9.
Ghanadi K, Valizadeh J, Hasanvand A. Epidemiological and clinical aspects of ulcerative colitis in west of Iran: a cross sectional study. Springerplus. 2016;5(1):1588.
Fadda MA, Peedikayil MC, Kagevi I, Kahtani KA, Ben AA, Al HI, et al. Inflammatory bowel disease in Saudi Arabia: a hospital-based clinical study of 312 patients. Ann Saudi Med. 2012;32(3):276–82.
Tavakkoli H, Haghdani S, Adilipour H, Daghaghzadeh H, Minakari M, Adibi P, et al. Serologic celiac disease in patients with inflammatory bowel disease. J Res Med Sci. 2012;17(2):154–8.
Shirazi KM, Somi MH, Bafandeh Y, Saremi F, Mylanchy N, Rezaeifar P, et al. Epidemiological and clinical characteristics of inflammatory bowel disease in patients from northwestern Iran. Middle East J Dig Dis. 2013;5(2):86–92.
El Mouzan MI, Abdullah AM, Al Habbal MT. Epidemiology of juvenile-onset inflammatory bowel disease in central Saudi Arabia. J Trop Pediatr. 2006;52(1):69–71.
Mansour-Ghanaei F, Haghkerdar M, Joukar F, Aminian K, Yousefi Mashhour M, Shafaghi A, et al. Epidemiologic features of inflammatory bowel disease in Guilan Province, North of Iran, during 2002–2012. Middle East J Dig Dis. 2015;7(2):69–74.
Qureshi M, Abbas Z. Clinical presentation of ulcerative colitis in Pakistani adults. Euroasian J Hepato-Gastroenterol. 2015;5(2):127.
Ouakaa-Kchaou A, Gargouri D, Bibani N, Elloumi H, Kochlef A, Kharrat J. Epidemiological evolution of epidemiology of the inflammatory bowel diseases in a hospital of Tunis. Tunis Med. 2013;91(1):70–3.
Ghorbaninezhad SS, Ghobadi GJ, Lansour-ghanaei F. Evaluating the relationship between environmental elements and geographical distribution of inflammatory bowel disease (IBD) in Gilan province. Revista Latinoamericana de Hipertensión. 2020;15(1):6–12.
Balaii H, Asadzadeh Aghdaei H, Farnood A, Habibi M, Mafi AA, Firouzi F, et al. Time trend analysis and demographic features of inflammatory bowel disease in Tehran. Gastroenterol Hepatol Bed Bench. 2015;8(4):253–61.
Al-Ghamdi AS, Al-Mofleh IA, Al-Rashed RS, Al-Amri SM, Aljebreen AM, Isnani AC, El-Badawi R. Epidemiology and outcome of Crohn’s disease in a teaching hospital in Riyadh. World J Gastroenterol. 2004;10(9):1341–4.
Esmat S, El Nady M, Elfekki M, Elsherif Y, Naga M. Epidemiological and clinical characteristics of inflammatory bowel diseases in Cairo. Egypt World J Gastroenterol. 2014;20(3):814–21.
Alharbi OR, Azzam NA, Almalki AS, Almadi MA, Alswat KA, Sadaf N, Aljebreen AM. Clinical epidemiology of ulcerative colitis in Arabs based on the Montréal classification. World J Gastroenterol. 2014;20(46):17525–31.
Balaii H, Olfatifar M, Olianasab Narab S, Arab Hosseini A, Seyed Salehi A, Shahrokh S. Estimation the direct cost of inflammatory bowel disease in Iranian patients; the one- year follow-up. Gastroenterol Hepatol Bed Bench. 2019;12(Suppl1):S87-s93.
Morita N, Toki S, Hirohashi T, Minoda T, Ogawa K, Kono S, et al. Incidence and prevalence of inflammatory bowel disease in Japan: nationwide epidemiological survey during the year 1991. J Gastroenterol. 1995;30(Suppl 8):1–4.
Bernstein CN, Wajda A, Svenson LW, MacKenzie A, Koehoorn M, Jackson M, et al. The epidemiology of inflammatory bowel disease in Canada: a population-based study. Am J Gastroenterol. 2006;101(7):1559–68.
Yang SK, Yun S, Kim JH, Park JY, Kim HY, Kim YH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986–2005: a KASID study. Inflamm Bowel Dis. 2008;14(4):542–9.
Hou JK, Kramer JR, Richardson P, Mei M, El-Serag HB. The incidence and prevalence of inflammatory bowel disease among U.S. veterans: a national cohort study. Inflamm Bowel Dis. 2013;19(5):1059–64.
Lunney PC, Kariyawasam VC, Wang RR, Middleton KL, Huang T, Selinger CP, et al. Smoking prevalence and its influence on disease course and surgery in Crohn’s disease and ulcerative colitis. Aliment Pharmacol Ther. 2015;42(1):61–70.
Calkins BM. A meta-analysis of the role of smoking in inflammatory bowel disease. Dig Dis Sci. 1989;34(12):1841–54.
Boyko EJ, Perera DR, Koepsell TD, Keane EM, Inui TS. Effects of cigarette smoking on the clinical course of ulcerative colitis. Scand J Gastroenterol. 1988;23(9):1147–52.
Mahid SS, Minor KS, Soto RE, Hornung CA, Galandiuk S. Smoking and inflammatory bowel disease: a meta-analysis. Mayo Clin Proc. 2006;81(11):1462–71.
Yadav P, Ellinghaus D, Rémy G, Freitag-Wolf S, Cesaro A, Degenhardt F, et al. Genetic Factors Interact With Tobacco Smoke to Modify Risk for Inflammatory Bowel Disease in Humans and Mice. Gastroenterology. 2017;153(2):550–65.
Ananthakrishnan AN, Nguyen DD, Sauk J, Yajnik V, Xavier RJ. Genetic polymorphisms in metabolizing enzymes modifying the association between smoking and inflammatory bowel diseases. Inflamm Bowel Dis. 2014;20(5):783–9.
Santos MPC, Gomes C, Torres J. Familial and ethnic risk in inflammatory bowel disease. Ann Gastroenterol. 2018;31(1):14–23.
Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn’s disease. Lancet. 2017;389(10080):1741–55.
Brant SR. Update on the heritability of inflammatory bowel disease: the importance of twin studies. Inflamm Bowel Dis. 2011;17(1):1–5.
Childers RE, Eluri S, Vazquez C, Weise RM, Bayless TM, Hutfless S. Family history of inflammatory bowel disease among patients with ulcerative colitis: a systematic review and meta-analysis. J Crohns Colitis. 2014;8(11):1480–97.
Afzali A, Cross RK. Racial and ethnic minorities with inflammatory bowel disease in the United States: a systematic review of disease characteristics and differences. Inflamm Bowel Dis. 2016;22(8):2023–40.
Damas OM, Jahann DA, Reznik R, McCauley JL, Tamariz L, Deshpande AR, et al. Phenotypic manifestations of inflammatory bowel disease differ between Hispanics and non-Hispanic whites: results of a large cohort study. Am J Gastroenterol. 2013;108(2):231–9.
Sewell JL, Inadomi JM, Yee HF Jr. Race and inflammatory bowel disease in an urban healthcare system. Dig Dis Sci. 2010;55(12):3479–87.
Nguyen GC, Torres EA, Regueiro M, Bromfield G, Bitton A, Stempak J, et al. Inflammatory bowel disease characteristics among African Americans, Hispanics, and non-Hispanic Whites: characterization of a large North American cohort. Am J Gastroenterol. 2006;101(5):1012–23.
Basu D, Lopez I, Kulkarni A, Sellin JH. Impact of race and ethnicity on inflammatory bowel disease. Am J Gastroenterol. 2005;100(10):2254–61.
Andersson RE, Olaison G, Tysk C, Ekbom A. Appendectomy and protection against ulcerative colitis. N Engl J Med. 2001;344(11):808–14.
Chung WS, Chung S, Hsu CY, Lin CL. Risk of Inflammatory Bowel Disease Following Appendectomy in Adulthood. Front Med (Lausanne). 2021;8: 661752.
Fantodji C, Jantchou P, Parent ME, Rousseau MC. Appendectomy and risk for inflammatory bowel disease: effect of age and time post appendectomy - a cohort study. BMJ Open Gastroenterol. 2022;9(1):e000925.
Panaccione R. Mechanisms of inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2013;9(8):529–32.
Farmer RG, Easley KA, Rankin GB. Clinical patterns, natural history, and progression of ulcerative colitis. A long-term follow-up of 1116 patients. Dig Dis Sci. 1993;38(6):1137–46.
Acknowledgements
None.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Z.MS, RM and Z.F contributed to the conception and design of the study. H.V, R.M and Z.MS drafted the manuscript, H.V and Z.F analyzed and examined the data. Z.MS and HV participated in the literature search, quality assessment, and writing work. Z.MS, RM and Z.F participated in literature screening and data extraction. All the authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sanat, Z.M., Vahedi, H., Malekzadeh, R. et al. Epidemiologic profile of inflammatory bowel disease in Eastern Mediterranean Region (EMRO) countries: a systematic review and meta-analysis. BMC Public Health 24, 1395 (2024). https://doi.org/10.1186/s12889-024-18816-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18816-z