Abstract
Background
There is a strong association between cardiovascular disease (CVD) and periodontitis. This study utilized the Life Essentials 8 (LE8) score, a composite measure of cardiovascular health (CVH), to elucidate the relationship between CVH and periodontitis.
Methods
Data from 8,649 nationally representative participants in the National Health and Nutrition Examination Survey (NHANES) were analyzed. The independent variable in our study was the CVH score (a higher CVH score indicates better cardiovascular health), and the dependent variable was the presence or absence of periodontitis. The association between CVH and periodontitis was investigated using weighted multivariable logistic regression models and restricted cubic spline (RCS). We controlled for potential confounders such as age, sex, race, education, and socioeconomic status to minimize bias.
Results
There was a negative association between the total CVH score and the odds of periodontitis. After adjusting for all covariates, a 10-point increase in total CVH score was associated with a 10% lower in the odds of periodontitis [0.90 (0.87, 0.93)]. Participants with a higher CVH had 40% lower odds of periodontitis compared with those with a lower CVH. Socioeconomic status (education and income) modified this association (P for interaction < 0.05).
Conclusion
Our study suggests that better cardiovascular health, as indicated by higher CVH scores, is associated with a reduced likelihood of periodontitis among US adults. The relationship between CVH and periodontitis appears to be influenced by socioeconomic status, emphasizing the need for targeted interventions in populations with lower socioeconomic status.
Similar content being viewed by others
Introduction
Cardiovascular health (CVH), a critical aspect of global health, is increasingly recognized for its interconnectedness with various aspects of systemic health, including oral health [1]. The American Heart Association (AHA) introduced the Cardiovascular Health (CVH) concept in 2010, initially measured by the Life’s Simple 7 (LS7) score. This score encompassed seven crucial health behaviors and factors [1]. In 2022, the AHA updated this to the Life’s Essential 8 (LE8), incorporating sleep health and refining its assessment algorithm in response to evolving research and a broadened understanding of CVH [2,3,4]. The LE8 score, now a more encompassing and precise tool, allows for a detailed evaluation of CVH and its influence on health outcomes.
Emerging evidence indicates a bidirectional relationship between periodontal disease and cardiovascular health [5,6,7]. Periodontitis, a prevalent inflammatory condition affecting the supporting structures of teeth, has been shown to have potential implications for cardiovascular health [8]. Recent studies have increasingly highlighted the significant influence of cardiovascular health on periodontal disease. Periodontitis, a chronic inflammatory condition affecting the supporting structures of teeth, is not only a consequence of local factors but is also impacted by systemic health conditions, particularly cardiovascular diseases (CVD). There is a growing body of evidence suggesting that cardiovascular diseases exacerbate periodontal conditions [9]. For instance, systemic inflammation, a common factor in CVD, has been shown to play a major role in the progression of periodontal disease, suggesting a close interplay between the two factors [10]. This connection is further supported by studies demonstrating that conditions such as atherosclerosis, often associated with poor CVH, are significantly linked with the severity of periodontitis [11]. Furthermore, the inflammatory burden imposed by periodontal disease may also contribute to the worsening of cardiovascular conditions, underscoring the bidirectional nature of this relationship [12].
Recognizing this intricate relationship, our study aims to elucidate the association between comprehensive cardiovascular health, as quantified by the LE8 metrics, and periodontal outcomes. By leveraging NHANES data, this study seeks to contribute to the understanding of how cardiovascular wellbeing, encompassing a broader range of health metrics, correlates with periodontitis.
Methods
Study population and design
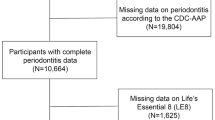
The National Health and Nutrition Examination Survey (NHANES), facilitated by the National Center for Health Statistics (NCHS), functions as a comprehensive, cross-sectional study aimed at assessing the health and nutritional status of the U.S. civilian population [13, 14]. Initiated in 1999, NHANES employs a diverse methodology that includes physical examinations and interviews to collect data on demographics, socioeconomic factors, and health indicators [15]. Comprehensive descriptions of the study’s design and methods are available on the NHANES website. The present research analyzes data from multiple NHANES cycles spanning 2009–2014. Strict exclusion criteria were applied, omitting 19,069 individuals lacking complete periodontal screening data and 2,750 individuals with insufficient information to compute Cardiovascular Health (CVH) metrics or who were pregnant during the baseline examination (Fig. 1). This resulted in a final analytical sample of 8,649 participants. The participant selection process adhered to ethical standards, and the survey protocol received approval from the NCHS Research Ethics Review Board. All participants provided written informed consent, and this research complies with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Cardiovascular health evaluation
Cardiovascular Health (CVH) is assessed using the LE8 score, a higher CVH score indicates better cardiovascular health, which amalgamates eight crucial elements: diet, physical activity, use of tobacco or nicotine, sleep habits, Body Mass Index (BMI), non-HDL cholesterol, blood glucose levels, and blood pressure metrics. The diet component is evaluated using the Dietary Approaches to Stop Hypertension (DASH) diet score. Information regarding physical activity (quantified as minutes of moderate to vigorous weekly exercise), tobacco or nicotine usage (including active smoking and exposure to secondhand smoke), sleep habits (quantified as total hours of sleep), and medication usage were obtained from standardized questionnaires. Parameters such as weight, height, blood glucose levels, and blood pressure were gathered at specialized mobile centers following standardized protocols. BMI is calculated by dividing an individual’s weight in kilograms by the square of their height in meters. The average blood pressure was determined from all readings taken during the initial evaluation. Serum cholesterol levels were ascertained using enzymatic techniques, and non-HDL cholesterol was determined by subtracting HDL cholesterol from the total cholesterol value. Glycated hemoglobin levels were assessed using high-performance liquid chromatography. Detailed descriptions and scoring methodologies for each CVH component are available in Table S1 and the cited studies [2, 3, 16]. Each CVH metric is scored on a scale from 0 to 100. The overall CVH score is computed as the average for the eight individual factors. According to the American Heart Association guidelines, CVH scores of 80–100, 50–79, and 0–49 correspond to high, moderate, and low CVH levels, respectively [17].
Definition of periodontitis
In the NHANES data, periodontal examinations were conducted on both males and females aged 30 years and above. The “Oral Health - Periodontal Screening” initiative evaluates periodontal health by measuring six regions of up to 28 teeth. The program utilizes two clinical metrics: Clinical Attachment Loss (CAL) and Probing Depth (PD). A classification system for periodontitis, based on case definitions from the CDC and the American Academy of Periodontology (AAP), has been established. Severe periodontitis is identified by at least two interproximal areas with a CAL of ≥ 6 mm and at least one interproximal area with a PD of ≥ 5 mm, not on the same tooth. Moderate periodontitis is defined by two or more interproximal sites with a probing pocket depth of ≥ 5 mm or a clinical attachment level of ≥ 4 mm, not on the same tooth [18]. Cases of moderate to severe periodontitis are classified as patients with periodontitis, while all other cases are categorized as the reference group [19].
Covariables
Data about demographics, including age, gender, ethnic background, and educational attainment, was gathered using standardized surveys. The classifications for ethnicity encompassed White, Black, Mexican American, other Hispanic, and another category that included other races such as Asian and multiracial individuals. Educational attainment was segmented into three categories: those without a high school diploma, graduates, and individuals with some college education or higher. The ratio of family income to the poverty threshold was determined by dividing the total family income by the official poverty line and subsequently categorized into low (< 1.3), intermediate (≥ 1.3 and < 3.0), and high (≥ 3.0) groups [15]. The selection of these covariates complements the CVH score components, which already include information on diet quality, physical activity duration, smoking status, sleep duration, body mass index, blood lipids, blood glucose, and blood pressure. This approach ensures a comprehensive adjustment for potential confounders in our analysis, aligning with methodologies applied in similar high-quality studies [2, 20, 21]. Our covariate selection process and model adjustments are grounded in the CVH’s encompassing nature, as these demographic and socioeconomic factors provide additional insights beyond the CVH components.
Statistical analysis
To enhance representativeness at the national level, NHANES sampling weights were applied, compensating for demographic overrepresentation and complex survey design [22,23,24]. CVH was categorized as low (< 50), intermediate (50–79), and high (≥ 80) based on the LE8 score. Categorical variables were expressed as percentages (weighted counts), and continuous variables were denoted as mean ± standard deviation (SD). Multiple imputation techniques were employed to address missing covariate data. Logistic regression models were used to investigate the relationships between the overall CVH score, its 8 subscores, and periodontitis. Three regression models were employed: Model 1, which was unadjusted for covariates (but adjusted for the other 7 subscores when assessing CVH subscores); Model 2, which built upon Model 1 by incorporating age, sex, and ethnicity; and Model 3, which extended Model 2 by adding education level and family income-to-poverty ratio. The association between CVH and periodontitis was also analyzed across various subgroups, includes sex (male/female), race (Non-Hispanic White/ Non-Hispanic Black/ Mexican American/ Other Hispanic/ Others), education level (Less than high school/ High school/ More than high school), and PIR categories (< 1.3/1.3–3.5/>3.5). To explore potential non-linear relationships between CVH and periodontitis, a restricted cubic spline (RCS) was utilized. All statistical analyses were performed using R software version 4.3.0. All tests were two-sided, with a P value < 0.05 indicating statistical significance.
Results
Baseline characteristics
In the present analysis, a total of 8,649, approximating 50.1 million U.S. adults were included. The mean (SD) for the LE8 score was 65.75 (12.46), and the odds of periodontitis was 49.8 (24.9). Figure 2 depicts the distribution of the CVH total score and 8 subscores among participants with or without periodontitis. The participant distribution, as determined by their CVH status (LE8 score), was as follows: 15.9% (equating to 8.0 million individuals) exhibited low CVH (LE8 < 50), 62.6% (approximating 31.3 million individuals) had moderate CVH (50 ≤ LE8 < 80), and 21.5% (corresponding to 10.8 million individuals) were classified with high CVH (LE8 ≥ 80). Initial evaluations revealed that those participants categorized with high CVH were generally younger and, more frequently, women and White. They were also more likely to possess a higher level of educational achievement and PIR. Additionally, these individuals exhibited a lower odd of periodontitis, as detailed in Table 1.
Association of the CVH and periodontitis
Table 2 demonstrates the association of the total CVH score and the eight CVH subscores with periodontitis. In all models, there was a negative correlation between the total CVH score and the odds of periodontitis. After adjusting for all covariates, a 10-point higher CVH score was associated with a 9% lower odds of periodontitis prevalence [0.90 (0.87, 0.93)]. The odds of periodontitis lower by 25% in participants with moderate CVH scores [0.75 (0.60, 0.95)] and by 40% in those with high CVH scores [0.60 (0.41, 0.89)], compared with participants with low CVH scores. In addition, in the fully adjusted model, all six CVH subscores maintained negative associations with periodontitis, except for the Physical activity score and Blood lipid score, which had non-significant positive associations with the odds of periodontitis. Figure 3 further demonstrates the negative correlation association between the total CVH score and the odds of periodontitis (P for overall < 0.001; P for non-linear = 0.659).
Dose–response relationships between the life’s essential 8 total score and periodontitis. Beta (solid lines) and 95% confidence levels (shaded areas) were adjusted for age, gender, race, education level, and ratio of family income to povert. Note: a higher CVH score indicates better cardiovascular health
Subgroup analyses
To investigate whether the association between CVH and periodontitis differed across populations, subgroup analyses based on sex, race, and socioeconomic status (education and PIR) were further investigated (Table 3). In all subgroups, the negative association between total CVH and periodontitis prevalence was maintained (P < 0.05). Nevertheless, the results showed significant differences in the association between CVH and periodontitis among different socioeconomic status groups (P for interaction < 0.05). A 10-point increase in total CVH score was associated with a 22% lower in the odds of periodontitis among participants with less than high school education [0.78 (0.69, 0.87)], which was significantly higher than among those with high school education [0.90 (0.86, 0.95)] and those with more than high school education [0.88 (0.80, 0.96)]. The same was true for household income, where a 10-point increase in total CVH score was associated with 28% lower odds in periodontitis among participants with lower PIR [0.72 (0.64, 0.80)], significantly higher than among participants with moderate [0.85 (0.79, 0.91)] and higher PIR [0.92 (0.86, 0.98)].
Discussion
In this nationally representative study, we found a significant negative correlation between cardiovascular health, as quantified by the LE8 score, and the odds of periodontitis. More importantly, our results suggest that differences in socioeconomic status modify the association between CVH and periodontitis, with individuals of lower socioeconomic status benefiting more from higher CVH scores. These findings emphasize the potential impact of cardiovascular health on the odds of periodontitis and highlight the importance of CVH scores quantified by LE8 in monitoring and reducing the odds of periodontitis.
To the best of our knowledge, this is the first study to investigate the relationship between exposure to CVH scores and periodontitis. Previous relevant studies have focused on the association between specific cardiovascular diseases and periodontitis [25]. In a recent meta-analysis study, in which 30 prospective cohort studies were included, the results showed a significantly higher cardiovascular risk of 20% in patients with periodontitis compared to participants without periodontitis (RR = 1.20,95% CI 1.14–1.26) [26]. A large case-control study from Sweden showed a significant 28% increase in the incidence of myocardial infarction in participants with periodontitis after detailed adjustment for all confounding factors [27]. However, it is not enough to understand the association between CVD and periodontitis; the pathogenesis of periodontitis is also strongly associated with a variety of cardiovascular risk factors, and the CVH score measured by LE8 in this study encompassed the common risk factors shared by periodontitis and cardiovascular risk. For example, smoking increases the risk of periodontitis and atherosclerosis and has a strong negative impact on the response to periodontal therapy [28]. In addition, periodontitis is associated with variables in plasma lipid levels, and abnormalities in blood lipids will accelerate disease progression in many types of CVD [29]. In addition, obesity (BMI Score) and physical activity have been shown to play an essential role in periodontitis and cardiovascular health [30]. The above evidence suggests that the CVH score, as measured by LE8, has the potential value to become a monitor of cardiovascular fitness level and prevalence and severity of periodontitis, and our results demonstrate the negative association of CVH with periodontitis from these perspectives.
Subgroup analyses of this study also elaborated on an important result: socioeconomic status modified the association between CVH and periodontitis, with participants with lower education and lower levels of household income elevating their CVH levels, resulting in a higher reduction in the odds of periodontitis than the rest of the group, so that participants with lower socioeconomic status should place more emphasis on improving or maintaining the different perspectives as measured by LE8 Cardiovascular health. There are several lines of evidence that low socioeconomic status increases the risk of cardiovascular and metabolic diseases [31,32,33]. Furthermore, the odds of periodontitis and disease severity have been reported to be negatively associated with socioeconomic status.
The mechanisms behind the negative correlation between cardiovascular health and the odds of periodontitis are extensive and complex. There are currently three main narratives explaining these mechanisms: (1) direct attachment of periodontal flora to endothelial cells through direct mechanisms and subsequent colonization of atherosclerotic plaques leading to plaque destabilization and atherosclerotic thrombotic events [5, 34]; (2) overlap of inflammatory pathways with higher systemic levels of inflammatory mediators [32, 35]; (3) shared clinical, environmental, and genetic risk factors [36,37,38].
Our study possesses several notable strengths. Foremost among them is the use of nationally representative data, which facilitates a comprehensive exploration of the association between cardiovascular health and the odds of periodontitis in the adult population of the United States [39]. This research is novel in examining the relationship between cardiovascular health scores, LE8, and periodontitis, offering new insights into the utility of CVH scores in the prevention and diagnosis of periodontitis. Nevertheless, certain limitations warrant acknowledgment. Firstly, the cross-sectional nature of the study design precludes the definitive establishment of causality [40, 41]. The reliance on self-reported data for certain indicators could potentially introduce bias. Furthermore, although we accounted for a broad spectrum of prevalent covariates to enhance the robustness of our findings, the constraints of the database meant that we could not completely eliminate the influence of all confounding factors on the results. An additional limitation of our study is the potential for selection bias. Individuals who refused participation in NHANES might differ fundamentally from those who participated, possibly influencing the generalizability of our findings. Moreover, the exclusion of older adults due to death before participation could bias our results, particularly in understanding the association of CVH and periodontitis in older populations. These factors underscore the need for cautious interpretation of our findings and suggest avenues for future research.
Conclusion
In conclusion, our study reveals a negative association between CVH, as measured by LE8, and the odds of periodontitis. In this association, individuals of lower socioeconomic status would benefit more from maintaining higher levels of CVH to reduce the probability of periodontitis.
Data availability
The survey data are publicly available on the internet for data users and researchers throughout the world (www.cdc.gov/nchs/nhanes/).
Abbreviations
- CVD:
-
Cardiovascular disease
- CAL:
-
Clinical Attachment Loss
- PD:
-
Probing Depth
- AAP:
-
American Academy of Periodontology
- LE8:
-
Life’s Essential 8
- CVH:
-
Cardiovascular health
- AHA:
-
American Heart Association
- LS7:
-
Life’s Simple 7
- NHANES:
-
National Health and Nutrition Examination Survey
- NCHS:
-
National Center for Health Statistics
- BMI:
-
Body mass index
- DASH:
-
Dietary Approaches to Stop Hypertension
- SD:
-
Standard deviation
- RCS:
-
Restricted cubic spline
References
Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586–613.
Sun J, Li Y, Zhao M, Yu X, Zhang C, Magnussen CG, Xi B. Association of the American Heart Association’s new Life’s essential 8 with all-cause and cardiovascular disease-specific mortality: prospective cohort study. BMC Med. 2023;21(1):116.
Ma H, Wang X, Xue Q, Li X, Liang Z, Heianza Y, Franco OH, Qi L. Cardiovascular Health and Life Expectancy among adults in the United States. Circulation. 2023;147(15):1137–46.
Wang X, Ma H, Li X, Heianza Y, Manson JE, Franco OH, Qi L. Association of Cardiovascular Health with Life Expectancy Free of Cardiovascular Disease, Diabetes, Cancer, and Dementia in UK adults. JAMA Intern Med. 2023;183(4):340–9.
Shetty B, Fazal I, Khan SF, Nambiar M, Prasad DKI, Raj R. Association between cardiovascular diseases and periodontal disease: more than what meets the eye. Drug Target Insights. 2023;17:31–8.
Sumayin Ngamdu K, Mallawaarachchi I, Dunipace EA, Chuang LH, Jafri SH, Shah NR, Jeong YN, Morrison AR, Bhatt DL. Association between Periodontal Disease and Cardiovascular Disease (from the NHANES). Am J Cardiol. 2022;178:163–8.
Nesse W, Dijkstra PU, Abbas F, Spijkervet FK, Stijger A, Tromp JA, van Dijk JL, Vissink A. Increased prevalence of cardiovascular and autoimmune diseases in periodontitis patients: a cross-sectional study. J Periodontol. 2010;81(11):1622–8.
Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, Listl S, Celeste RK, Guarnizo-Herreño CC, Kearns C, et al. Oral diseases: a global public health challenge. Lancet. 2019;394(10194):249–60.
Liccardo D, Cannavo A, Spagnuolo G, Ferrara N, Cittadini A, Rengo C, Rengo G. Periodontal Disease: a risk factor for diabetes and Cardiovascular Disease. Int J Mol Sci 2019, 20(6).
Sanz M, Marco Del Castillo A, Jepsen S, Gonzalez-Juanatey JR, D’Aiuto F, Bouchard P, Chapple I, Dietrich T, Gotsman I, Graziani F, et al. Periodontitis and cardiovascular diseases: Consensus report. J Clin Periodontol. 2020;47(3):268–88.
Tonetti MS, Van Dyke TE. Periodontitis and atherosclerotic cardiovascular disease: consensus report of the Joint EFP/AAP Workshop on Periodontitis and systemic diseases. J Periodontol. 2013;84(4 Suppl):24–9.
Febbraio M, Roy CB, Levin L. Is there a causal link between Periodontitis and Cardiovascular Disease? A concise review of recent findings. Int Dent J. 2022;72(1):37–51.
Zhang Y, Liu M, Xie R. Associations between cadmium exposure and whole-body aging: mediation analysis in the NHANES. BMC Public Health. 2023;23(1):1675.
Zhang Y, Wu H, Li C, Liu C, Liu M, Liu X, Yin Q, Li X, Xie R. Associations between weight-adjusted waist index and bone mineral density: results of a nationwide survey. BMC Endocr Disord. 2023;23(1):162.
Xie R, Liu Y, Wang J, Zhang C, Xiao M, Liu M, Zhang Y. Race and gender differences in the associations between Cadmium exposure and bone Mineral Density in US adults. Biol Trace Elem Res. 2023;201(9):4254–61.
Zhang J, Chen G, Habudele Z, Wang X, Cai M, Li H, Gao Y, Lip GYH, Lin H. Relation of Life’s Essential 8 to the Genetic Predisposition for Cardiovascular Outcomes and All-cause Mortality: Results from a National Prospective Cohort. Eur J Prev Cardiol 2023.
Lloyd-Jones DM, Allen NB, Anderson CAM, Black T, Brewer LC, Foraker RE, Grandner MA, Lavretsky H, Perak AM, Sharma G, et al. Life’s essential 8: updating and enhancing the American Heart Association’s construct of Cardiovascular Health: a Presidential Advisory from the American Heart Association. Circulation. 2022;146(5):e18–e43.
Zheng X, Li X, Zhen J, Xue D, Hu J, Cao Q, Xu A, Cheung BMY, Wu J, Li C. Periodontitis is associated with stroke. J Transl Med. 2023;21(1):697.
Vu GT, Shakib S, King C, Gurupur V, Little BB. Association between uncontrolled diabetes and periodontal disease in US adults: NHANES 2009–2014. Sci Rep. 2023;13(1):16694.
Xie R, Liu L, Liu C, Xie S, Huang X, Zhang Y. Associations of ethylene oxide exposure and Life’s Essential 8. Environ Sci Pollut Res Int 2023.
Mahemuti N, Zou J, Liu C, Xiao Z, Liang F, Yang X. Urinary albumin-to-creatinine ratio in normal range, Cardiovascular Health, and all-cause mortality. JAMA Netw Open. 2023;6(12):e2348333.
Xie R, Ning Z, Xiao M, Li L, Liu M, Zhang Y. Dietary inflammatory potential and biological aging among US adults: a population-based study. Aging Clin Exp Res. 2023;35(6):1273–81.
Xie R, Zhang Y. Associations between dietary flavonoid intake with hepatic steatosis and fibrosis quantified by VCTE: evidence from NHANES and FNDDS. Nutr Metab Cardiovasc Dis. 2023;33(6):1179–89.
Xie R, Zhang Y. Association between 19 dietary fatty acids intake and rheumatoid arthritis: results of a nationwide survey. Prostaglandins Leukot Essent Fat Acids. 2023;188:102530.
Tang K, Wu Y, Zheng Q, Chen X. Bibliometric research on analysis of links between periodontitis and cardiovascular diseases. Front Cardiovasc Med. 2023;10:1255722.
Larvin H, Kang J, Aggarwal VR, Pavitt S, Wu J. Risk of incident cardiovascular disease in people with periodontal disease: a systematic review and meta-analysis. Clin Exp Dent Res. 2021;7(1):109–22.
Rydén L, Buhlin K, Ekstrand E, de Faire U, Gustafsson A, Holmer J, Kjellström B, Lindahl B, Norhammar A, Nygren Å, et al. Periodontitis increases the risk of a first myocardial infarction: a Report from the PAROKRANK Study. Circulation. 2016;133(6):576–83.
Aarabi G, Eberhard J, Reissmann DR, Heydecke G, Seedorf U. Interaction between periodontal disease and atherosclerotic vascular disease–fact or fiction? Atherosclerosis. 2015;241(2):555–60.
Nepomuceno R, Pigossi SC, Finoti LS, Orrico SRP, Cirelli JA, Barros SP, Offenbacher S, Scarel-Caminaga RM. Serum lipid levels in patients with periodontal disease: a meta-analysis and meta-regression. J Clin Periodontol. 2017;44(12):1192–207.
Ferreira RO, Corrêa MG, Magno MB, Almeida A, Fagundes NCF, Rosing CK, Maia LC, Lima RR. Physical activity reduces the prevalence of Periodontal Disease: systematic review and Meta-analysis. Front Physiol. 2019;10:234.
Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, Quyyumi AA, Taylor HA, Gulati M, Harold JG, et al. Socioeconomic Status and Cardiovascular outcomes: challenges and interventions. Circulation. 2018;137(20):2166–78.
Borrell LN, Crawford ND. Socioeconomic position indicators and periodontitis: examining the evidence. Periodontol 2000. 2012;58(1):69–83.
Tang M, Liu M, Zhang Y, Xie R. Association of family income to poverty ratio and vibration-controlled transient elastography quantified degree of hepatic steatosis in U.S. adolescents. Front Endocrinol (Lausanne). 2023;14:1160625.
Ford PJ, Gemmell E, Chan A, Carter CL, Walker PJ, Bird PS, West MJ, Cullinan MP, Seymour GJ. Inflammation, heat shock proteins and periodontal pathogens in atherosclerosis: an immunohistologic study. Oral Microbiol Immunol. 2006;21(4):206–11.
Holmstrup P, Damgaard C, Olsen I, Klinge B, Flyvbjerg A, Nielsen CH, Hansen PR. Comorbidity of periodontal disease: two sides of the same coin? An introduction for the clinician. J Oral Microbiol. 2017;9(1):1332710.
Aarabi G, Zeller T, Seedorf H, Reissmann DR, Heydecke G, Schaefer AS, Seedorf U. Genetic susceptibility contributing to Periodontal and Cardiovascular Disease. J Dent Res. 2017;96(6):610–7.
Xie R, Liu X, Wu H, Liu M, Zhang Y. Associations between systemic immune-inflammation index and abdominal aortic calcification: results of a nationwide survey. Nutr Metab Cardiovasc Dis. 2023;33(7):1437–43.
Munz M, Richter GM, Loos BG, Jepsen S, Divaris K, Offenbacher S, Teumer A, Holtfreter B, Kocher T, Bruckmann C, et al. Genome-wide association meta-analysis of coronary artery disease and periodontitis reveals a novel shared risk locus. Sci Rep. 2018;8(1):13678.
Xie R, Xiao M, Li L, Ma N, Liu M, Huang X, Liu Q, Zhang Y. Association between SII and hepatic steatosis and liver fibrosis: a population-based study. Front Immunol. 2022;13:925690.
Xie R, Huang X, Liu Q, Liu M. Positive association between high-density lipoprotein cholesterol and bone mineral density in U.S. adults: the NHANES 2011–2018. J Orthop Surg Res. 2022;17(1):92.
Xie R, Liu M. Relationship between non-alcoholic fatty liver disease and degree of hepatic steatosis and bone Mineral Density. Front Endocrinol (Lausanne). 2022;13:857110.
Acknowledgements
We would like to thank all participants in this study.
Funding
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Author information
Authors and Affiliations
Contributions
HQ and SZ designed the research. HQ collected, analyzed the data, and drafted the manuscript. SZ revised the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The portions of this study involving human participants, human materials, or human data were conducted in accordance with the Declaration of Helsinki and were approved by the NCHS Ethics Review Board. The patients/participants provided their written informed consent to participate in this study.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing financial interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qu, H., Zhang, S. Association of cardiovascular health and periodontitis: a population-based study. BMC Public Health 24, 438 (2024). https://doi.org/10.1186/s12889-024-18001-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18001-2