Abstract
Background
To assess the adherence to option B + antiretroviral therapy (ART) and associated factors in pregnant and breastfeeding women in Sub-Saharan Africa (SSA).
Methods
We conducted a comprehensive search from 01st January 2012 to 03rd October 2022, across four databases: PubMed, Scopus, Proquest Central, and Index Medicus Africain, to identify studies focused on pregnant and/or breastfeeding women living with HIV and receiving option B+ ART in SSA. Studies reporting adherence data were included in the meta-analysis. Were excluded studies published before 01st January 2012, grey literature, systematic reviews, and meta-analysis studies. Articles selection and data extraction were performed independently by two reviewers. We evaluated pooled adherence and pooled association between various factors and adherence using a random-effects model.
Results
Overall, 42 studies involving 15,158 participants across 15 countries contributed to the meta-analysis. The overall pooled adherence was 72.3% (95% CI: 68.2–76.1%). Having high education level (pooled odds ratio (OR): 2.25; 95% CI: 1.57–3.21), living in urban area (pooled OR: 1.75; 95% CI: 1.10–2.81), disclosing status to a family/partner (pooled OR: 1.74; 95% CI: 1.27–2.40), having a support system (pooled OR: 3.19; 95% CI: 1.89–5.36), receiving counseling (pooled OR: 3.97; 95% CI: 2.96–5.34), initiating ART at early clinical HIV stage (pooled OR: 2.22; 95% CI: 1.08–4.56), and having good knowledge on PMTCT/HIV (pooled OR: 2.71; 95% CI: 1.40–5.25) were factors significantly associated with adherence to option B + ART.
Conclusions
Despite the implementation of option B+ ART, the level of adherence among pregnant and breastfeeding women in SSA falls short of meeting the critical thresholds for viral load suppression as outlined in the 95-95-95 objectives set for 2025. These objectives are integral for achieving HIV elimination, and in turn, preventing HIV mother-to-child transmission. To bridge this gap, urgent tailored interventions based on individual and structural factors are essential to enhance adherence within these subgroups of women. This targeted approach is crucial in striving towards the HIV elimination target in SSA.
Similar content being viewed by others
Background
Approximately, 1.3 million HIV-positive women worldwide become pregnant each year [1]. Of these, around 91% reside in Sub-Saharan Africa (SSA) with highest HIV burden in women [2, 3]. Globally, remarkable progress has been seen over the years in reducing new HIV infection among children under five years, from 320,000 in 2010 to 160,000 in 2021 [4]. However, further reduction is needed based on the global commitments to eliminate HIV by 2030, with a focus on mother to-child transmission (MTCT) [5]. According to the World Health Organization (WHO), HIV vertical transmission elimination in a country is defined based on the reduction of MTCT rate below 2% and 5% in non-breastfeeding and breastfeeding populations respectively, and the reduction of new paediatric HIV infections due to MTCT to less than 50 cases per 100,000 live births [6].
The observed decline in new infection in children under five years of age could be largely attributed to the different antiretroviral therapy (ART) strategies recommended by the WHO as part of the prevention of mother-to-child transmission (PMTCT) program. The most recent strategy includes the option B + strategy, initially conceived and implemented in Malawi in 2011, and rapidly adopted since 2013 by many SSA countries [7,8,9]. Option B + recommends lifelong ART for pregnant or breastfeeding women as soon as they test positive, regardless of gestational age, WHO clinical stage, and CD4 cell count [10, 11], and appears to be an effective PMTCT strategy as it has a significant impact on treatment uptake and improves outcomes for mothers and exposed infants [12]. In SSA, the ART coverage in pregnant women increased from 17% in 2010 to 87% in 2020, with HIV vertical transmission decreasing by 56% over the same period [13]. However, despite the success since the implementation of the option B + strategy, adherence to the regimen remains the main challenge that many countries still face, compromising the effectiveness of the strategy. The periods of pregnancy and breastfeeding represent a window of time associated with an increase in poor adherence, which leads to increased risks such as viral suppression failure, HIV progression, and the development of drug resistance, with these consequences heightening the risk of MTCT [14, 15].
Many studies in SSA have focused on the magnitude of adherence to option B + ART and the factors associated with this adherence. The results of these studies revealed disparities in the prevalence of ART adherence across different countries. Age [16,17,18], educational level [14, 19], experience of side effects [20, 21], knowledge of PMTCT or HIV [20], support from partner [16, 20, 21], disclosure to a family member or partner [11, 14, 22,23,24], receiving counseling [25], no fear of stigma [21], and employment status [26] were the factors reported to be associated with ART adherence.
In 2019, the UNICEF report revealed a vertical HIV transmission rate of 12.2% in SSA, despite reasonably good ART coverage in PMTCT programs [27]. Achieving optimal adherence to ART is essential to suppress the virus and prevent vertical transmission [28]. In the context of the global movement involving the use of option B + triple ART prophylaxis during pregnancy and breastfeeding for the prevention of HIV vertical transmission [29], a critical research question emerges: What is the extent of adherence to option B + ART prophylaxis among pregnant and breastfeeding women in Sub-Saharan Africa (SSA), and what factors contribute to or hinder optimal adherence in this specific population? Regarding the lack of comprehensive and synthetized evidence on this problematic, our systematic review and meta-analysis study, aimed at filling this knowledge gap and provide evidence-based perspectives, essential for designing targeted interventions to improve ART adherence. This research could serve as a compass to help advance the overall goal of curbing vertical HIV transmission and improving the well-being of women living with HIV in SSA.
Methods
This systematic review and meta-analysis was conducted using the Preferred Reporting Item for Systematic Review and Meta-analysis (PRISMA) guidelines [30]. To avoid duplication, we registered the protocol in PROSPERO with the registration number CRD42022346122 on 24 July 2022.
Information sources and search strategy
Four (04) electronic databases: PubMed, Scopus, Proquest Central, and Index Medicus Africain (IMA), were used in the study. The queries were developed using five (05) main keywords: a) adherence, b) prevention of mother-to-child transmission, c) antiretroviral therapy or option B, d) pregnant or breastfeeding women, and e) countries of sub-Saharan Africa (see the full search strategy and the results of the search for each database in the supplementary material). Two authors (LCF and DS) conducted searches of these databases. Terms were searched separately and together using Boolean operator “OR” or “AND”. Articles were filtered using the publication date (articles published from 01st January 2012 to 03rd October 2022). The date of 01st January 2012 was chosen because option B + strategy was first implemented in the late 2011 in SSA (Malawi) [31]. The reference manager software, Endnote X9.3.3 (bld 13966), was used to export different articles obtained from the searches and remove duplicates.
Eligibility criteria
All types of studies (observational, clinical trial) were included in the analysis if they met all the following criteria: i) the study included pregnant and/or breastfeeding women living with HIV in one or more SSA countries; ii) participants were administered option B + ART; and iii) the adherence rate to the treatment was clearly quantified. All studies that considered women in general and that did not give information on the sub-group of pregnant and/or breastfeeding women were excluded from the meta-analysis. Articles published before 01st January 2012 were excluded to avoid studies in the pre-option B + era. Moreover, grey literature (thesis, dissertations, conference papers, books, and reports) as well as systematic reviews and meta-analyses were not considered in this meta-analysis.
Study selection
All abstracts and full-text articles were independently reviewed by two authors (LCF and DS) according to the eligibility criteria using rayyan web-tool for systematic reviews [32]. Discrepancies were resolved by reaching an agreement by consensus.
Data extraction
LCF and DS independently extracted and compared data through an extraction form developed using kobo toolbox software [33]. For each paper, details were extracted on publication details (first author’s name, publication year), study characteristics (data collection years, country where the study was performed, design of the study, sample size), participant characteristics (age, type of women included in the study: pregnant women only, breastfeeding women only, or both), adherence measure characteristics (method of measure, threshold used for defining adherence, number of adherent participants, time frame used to measure adherence), and factors associated with adherence (a total of 10 relevant factors were considered in this study: age, educational level, occupation, area of residence, marital status, support of anyone or involvement from a partner, disclosure status, receiving counseling, stage of HIV/AIDS, and knowledge on PMTCT/HIV).
Study outcomes
The primary outcome of this study was the level of adherence to option B + ART. Adherence was estimated in each study by dividing the number of individuals with good adherence by the total number of individuals included in the study. The overall pooled adherence was determined based on the definition and adherence thresholds adopted in each study. A minimum threshold of 80% was considered. When a study used more than one threshold, only values related to a threshold of 80% were considered. When more than one measurement method was used in a study, only data concerning the most objective method were considered for analysis (for example: Dried blood spots > pill count > pharmacy refill > self-reported adherence).
The second outcome, which was related to the identification of factors associated with adherence, was determined using the odds ratio (OR) derived from binary outcomes. The overall pooled OR was then calculated. Studies that did not provide the necessary data for OR calculation were excluded from the combined analysis (calculation of pooled OR).
Quality assessment of the studies
The quality of the studies included in the meta-analysis was assessed using the Newcastle–Ottawa Scale (NOS) quality assessment form for observational studies recommended by the Agency for Healthcare Research and Quality (AHRQ) [34]. This scale uses a star system to assess the quality of a study in three domains: the selection of study participants (maximum 5 stars), comparability (maximum 1 star), and ascertainment of outcomes (maximum 3 stars). This form had the following criteria: representativeness, sample size justification, non-response, ascertainment of exposure, control for confounding, ascertainment of outcome, and statistical tests. The total score ranges from 0 to 9 stars. The quality of studies were indicated based on the number of stars (9 stars: very good; 7–8 stars: good; 5–6 stars: satisfactory; 0–4 stars: unsatisfactory) [34].
Statistical methods and analysis
The extracted data were analysed using R version 4.2.0. Pooled adherence to option B + ART was estimated using DerSimonian and Laird’s method with a random-effects model [35]. Heterogeneity between studies was assessed using Cochran’s Q test, and its magnitude was evaluated using Higgins I 2 statistics [36]. Publication bias was evaluated using funnel plots and Egger’s test [37].
To investigate potential sources of heterogeneity, we performed subgroup analyses and stratified our data according to the women’s status categories considered in the study (pregnancy, breastfeeding, pregnancy and breastfeeding), the year of publication (before 2018, after 2018), the SSA region (eastern, southern, western, central), the adherence recall time frame (last 7 days, last 15–30 days, last 90 days), study design (cross-sectional, cohort, randomised control trial [RCT]), and the instrument of measure used (self-report, pill count/pharmacy refill, combined measure, and others). A combined measure was defined as more than two (02) measures used simultaneously in a study. Concerning the subgroup analysis based on the instrument measure, one study [38] did not report the information associated with the instrument used and was not considered for this particular analysis. The stratification of the years of publication (before 2018 and after 2018) was based on the purpose to compare recent publications (articles published in the last five years) to less recent publications (articles published before the last five years).
Further, the potential source of heterogeneity was investigated using a random-effects meta-regression analysis to assess the associations between adherence from every studies and the study characteristics: women’s status, year of publication, instrument of measure, time frame, region, and the quality of the study.
Results
Study selection
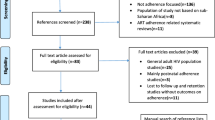
After searching different electronic databases, we found 1611 records, of which 206 were deemed relevant for full-text eligibility assessment. Finally, 42 studies were included in the quantitative analysis (Fig. 1) [11, 14, 16,17,18,19,20,21,22,23,24,25,26, 38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66].
Study characteristics
A total of 15,595 participants with available outcome data from the 43 studies were included in the qualitative analysis. These studies were conducted between 2013 and 2020 and published between 2014 and 2022. Most of the studies (17 out of 43) were conducted in Eastern African countries, followed by Austral African countries (14 out of 43), and West African countries (08 out of 43). One study was conducted in two countries (South Africa and Uganda) [67] and the other in three countries (Mozambique, South Africa, and Mali) [46]. The sample size varied between 42 [18] and 1592 [22] and more than 50% (22 out of 43) of the studies involved only pregnant women.
Out of the 43 eligible studies, 42 (97.7%) clearly reported instrument of adherence measures. Composite measure (combination of at least two different measures to produce one measure) was used in 7 studies [19, 22, 25, 26, 42, 47, 62]. Thirty-four studies [11, 14, 16,17,18, 20, 21, 23, 24, 40, 41, 43,44,45,46, 48,49,50,51,52,53,54,55,56,57,58,59,60,61, 63,64,65,66,67] used only one measure, while one study used three separate measures [Dried Blood Spot (DBS); self-report questionnaire and self-report using Visual Adherence Scale (VAS)] [39]. For this study, only DBS values were considered in the analysis because the DBS measure is more objective and precise than SR measures [39]. Globally, more than half (32 out of 43 studies) of the included studies used self-reporting (SR) as a measure of adherence, either alone (26 studies) or in combination (06 studies). The instruments used to measure self-reported adherence were as follows: simple questionnaire in most of the studies (19 studies), Visual Adherence Scale in two studies [24, 44], Center for Adherence Support Evaluation (CASE) in two studies [40, 65] and Adult AIDS Clinical Trial Group (AACTG) in three studies [52, 57, 58]. The composite measures used to measure adherence were: pharmacy refill and self-report in one study [22], pill count and self-report in four studies [25, 26, 47, 62], and a combination of self-reported questionnaire, pharmacy refill, and Visual Adherence Scale in one study [42].
Different thresholds were used to define adherence across the studies, ranging from 80–100%. Two studies used the CASE scale defined adherence based on the score threshold (> 10 [40]and > 11 [65]) instead of the percentage threshold. Moreover, a study reported adherence based on biological measurements (DBS) and did not use a threshold.
Adherence recall timeframes ranged from as recent as “the last day” [17] to as far as “the last 90 days” [22, 48, 49]. Six studies lacked clear descriptions of the timeframe used [21, 46, 47, 50, 51, 65]. The study designs were: cross-sectional (29 studies), cohort (9 studies), and controlled clinical trial (5 studies).
Eleven studies did not identify the factors associated with option B + ART adherence [24, 39, 42, 46, 48, 49, 54,55,56, 59, 67]. Table 1 presents the characteristics of the studies included in the systematic review and meta-analysis in further detail.
Quality assessment of studies
The quality assessment was limited to studies included in the quantitative analysis. Of these studies (42 in total), over half (28 studies) demonstrated satisfactory to very good quality (Table 2). When considering the selection bias domain, 13 studies showed a high risk of bias regarding sample representativeness, 24 studies in terms of sample size justification, 29 studies in terms of non-response, and 15 studies in terms of adherence measure tool ascertainment. Under the comparability domain, 7 studies exhibited high risk of bias regarding control of confounding factors. In the outcome domain, none of the studies demonstrated high risk of bias regarding outcome ascertainment, while 10 studies showed high risk of bias in reporting statistical test.
Overall adherence to option B + ART
Overall, 42 studies (involving 15,158 participants across 15 countries) were included in the quantitative analysis. Proportions of adherence to option B + ART and 95% CIs from individual studies with the pooled estimate are presented in the Fig. 2. These proportions ranged from 19% in western Uganda [18] to 89.2% in Southern Ethiopia [20]. The overall pooled adherence estimate was 72.3% (95% CI: 68.2–76.1%; I 2 = 96.5%; p < 0.01) (Fig. 2). The funnel plot revealed an asymmetric repartition of the studies (Fig. 3), although the Egger’s test did not yield statistical significance (z = 0.87; p = 0.38).
Subgroup analysis of adherence to option B + ART
Table 3 outlines the detailed results of the subgroup analysis. Stratified by women’s status, the overall pooled adherence prevalence was 71.9% (95% CI: 66.8–76.4%) for pregnant women and 61.1% (95% CI: 49.0–72.0%) for breastfeeding women. When considering the 16 studies that did not distinctly report adherence in these groups, the pooled prevalence of adherence was 75.8% (95% CI: 67.2–82.7%) in pregnant and breastfeeding women in SSA. Examining publication years, there was no discernible difference in prevalence of adherence to option B + ART between studies published after 2018 (73.6%; 95% CI: 69.5–77.3%) and those published before 2018 (67.6%; 95% CI: 55.0–78.0%).
Adherence levels significantly varied based on measurement instruments, with notably higher rates (75.5%; 95% CI: 64.9–83.7%) observed when using at least two measurement tools. In contrast, the lowest adherence (45.1%; 95% CI: 35.3–55.2%) was noted when relying on pill count or pharmacy refill measures.
Adherence to option B + ART significantly differed between regions, with the highest pooled prevalence (74.8%; 95% CI: 67.7–80.9%) reported in eastern Africa. Across study designs, the pooled prevalence of adherence was significantly higher in cross-sectional studies (76.2%; 95% CI: 71.7–80.1%), compared to cohort studies (63.0%; 95% CI: 54.4–70.9%), and randomised control trials (62.8%; 95% CI: 47.2–76.1%) studies. Moreover, based on the assessment timeframe, there was no significant difference in the adherence within the last 7 days (75.4%; 68.5–81.2%) and that within the last 90 days (66.5%; 95% CI: 61.1–71.6%).
The multiple meta-regression including all the seven variables indicated that all these variables collectively accounted for 25% of the variation between studies (R 2 = 25.56%; p = 0.003).
Factors associated with adherence to option B + ART
Association between adherence and sociodemographic factors
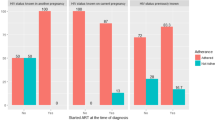
Figures 4 and 5 present the details of the association between each sociodemographic factor and adherence to option B + ART.
-
Age
Seventeen studies were included in the estimation of the pooled association between adherence to option B + ART and women's age. From these studies, only three showed significant associations, with one demonstrating a negative association [47]. Overall, the random-effects pooled association indicated that women’s age was not statistically associated with adherence (pooled OR: 1.02; 95% CI: 0.81–1.29; p = 0.84; I 2 = 60%).
-
Occupation
Twenty studies were used to determine the pooled association between adherence to option B + ART and women’s occupation. The assessment revealed that women’s occupation was not statistically associated with adherence to option B + ART (pooled OR: 0.90; 95% CI: 0.73–1.11; p = 0.33; I 2 = 53%).
-
Educational level
The random-effects pooled association between adherence to option B + ART and educational status was assessed using fourteen studies. The OR ranged from 0.74 (95% CI: 0.37–1.48) to 8.96 (95% CI: 1.00–80.33). An increased likelihood of adherence was observed among women having at least grade 1 educational level. In fact, those having at least this level of education were significantly more susceptible to adhere compared to those with no educational level background (pooled OR: 2.25; 95% CI: 1.57–3.21; p < 0.001; I 2 = 63%).
-
Area of residence
The pooled association between adherence to option B + ART and the area of residence was determined using thirteen studies. The random-effects model yielded a pooled OR of 1.76 (95% CI: 1.10–2.81; p = 0.019; I 2 = 89%), indicating a higher likelihood of adherence among pregnant or breastfeeding women residing in urban areas compared to those in rural settings.
-
Marital status
The pooled association between marital status and adherence to option B + ART was assessed using twenty-two studies, revealing no significant difference in adherence between women in couples (relationships or marriages) and those who were not (pooled OR: 1.23; 95% CI: 0.99–1.53; p=0.07; I 2 = 57%).
Association between adherence to option B + ART and social and clinical factors
Figures 6 and 7 present details of the association between social/clinical factors and adherence to option B + ART.
-
Disclosure status
Fifteen studies were included in the random-effects pooled estimation of the association between adherence to option B + ART and disclosure status. The results revealed that pregnant or breastfeeding women who disclosed their HIV status to a family member or their partner were more likely to adhere to option B + ART compared to those who did not disclose their status (pooled OR: 1.74; 95% CI: 1.27–2.40; p < 0.001; I 2 = 82 %).
-
Support of anyone or involvement from a partner
The random-effects pooled estimation of the association between adherence to option B + ART and support of anyone or involvement from a partner, including 15 studies revealed a pooled OR of 3.19 (95% CI: 1.89–5.36; p < 0.001; I 2 = 86%). This suggests that pregnant, and breastfeeding women receiving support from any person or involvement from a partner are more likely to adhere to option B + ART compared to those lacking such support or involvement.
-
Receiving counseling
The pooled association between adherence to option B + ART and receiving counseling was estimated using ten studies. The results showed low heterogeneity among the studies (I 2 = 17 %; p = 0.29). The random-effects pooled OR was 3.97 (95% CI: 2.96–5.34; p < 0.001), indicating that women who received counseling were more likely to adhere compared to those who did not.
-
Clinical stage
Eight studies were included in the estimation of the random-effects pooled association between option B + ART adherence and HIV clinical stage, revealing a pooled OR of 2.22 (95% CI: 1.08–4.56; p = 0.03; I 2 = 87%). This suggests that women who initiated treatment at clinical stage 1 were more likely to adhere compared to those initiating treatment at clinical stage 2 or beyond.
-
Knowledge on PMTCT/HIV
The random-effects pooled association between option B + ART adherence and knowledge on PMTCT/HIV, involving ten studies revealed a pooled OR of 2.71 (95% CI: 1.40–5.25; p = 0.003; I 2 = 81%), indicating that women with good knowledge on PMTCT/HIV were more likely to adhere to option B + ART compared to those with poor knowledge.
Discussion
To the best of our knowledge, this is the first study to summarise the available data on adherence to option B + ART in pregnant and breastfeeding women in SSA. The option B + strategy was first implemented in Malawi in 2011, and since then, significant reduction in MTCT has been observed [68]. However, despite the considerable progress observed, adherence to lifelong ART remains a challenge in SSA. In our meta-analysis, the pooled prevalence of adherence to option B + ART among pregnant and breastfeeding women in SSA was estimated to be 72.3% (95% CI: 68.2–76.1%). Tsegaye et al. conducted a meta-analysis in Eastern African countries and reported similar results (71.9%), although their study focused on women in general [69]. Subgroup analyses based on various factors such as women’s status, year of publication, and time frame recall did not show significant differences in option B + ART adherence. However, regional analysis revealed higher adherence in Eastern Africa, potentially influenced by specific interventions designed to improve adherence in that region. Among these interventions, the mother-mentors program stands out. This program involves training HIV-infected mothers who are employed in a healthcare facility to provide one-on-one support to HIV-infected pregnant/postpartum women, encourage enrolment, adherence, and retention in HIV care; leading to easy identification of women missing clinic visits; and educating them on PMTCT and health-related topics [70, 71]. A study conducted in Uganda between 2011 and 2014 revealed that HIV-positive mothers and their HIV-exposed infants enrolled in the mothers2mothers Ugandan Mentor Mother program had higher retention in HIV care at every step of the PMTCT, including adherence to ART [72]. Stratifying by women’s status, our study revealed that pregnant women were more adherent than breastfeeding women. These findings are similar to those of a meta-analysis conducted by Nachega et al. in low-, middle-, and high-income countries, revealing an adherence of 75.7% and 53.0% in pregnant and breastfeeding women, respectively. This difference in the two periods could be due to the fear of women to transmit HIV to their babies through pregnancy. Moreover, women may suffer from postpartum depression (PPD) after pregnancy, negatively affecting adherence to ART [73].
Our meta-analysis has revealed that around one-quarter of pregnant and breastfeeding women in SSA did not have the optimal adherence level needed for successful viral load suppression and, consequently, may be at a higher risk of transmitting HIV to their infants. Thus, evaluating the comprehensive effectiveness of interventions tailored for the prenatal and postpartum periods becomes imperative. Pellowski et al. in their systematic review and meta-analysis published in 2019 revealed limited efficacy of the behavioural ART interventions targeting pregnant and breastfeeding women despite the common motivation associated with childbirth and motherhood [74]. Urgent actions aimed at innovating and reinforcing established interventions could significantly bolster ART adherence in this critical population, especially during the postpartum period marked by insufficient adherence. Our analysis revealed substantial heterogeneity among studies (96.5%). This aligns with similar findings from studies by Nachega et al. in 2012 (97.7%) [29], Tsegaye et al. in 2020 (99%) [69], and de Mattos Costa et al. in 2018 (98%) [75]. This high heterogeneity could be attributed to considerable variations in adherence measurement methods, thresholds, instruments, and definitions employed across the studies.
Several factors associated with adherence to option B + ART in pregnant and breastfeeding women were identified in our meta-analysis. Considering the sociodemographic characteristics, both educational level and area of residence emerged as significantly positively associated with adherence to option B + ART. Pregnant and/or breastfeeding women with higher educational levels were more likely to adhere to option B + ART than those with lower educational levels. Similar results were reported by other studies [14, 16, 23, 60, 76]. However, contrasting trends were reported in some studies [50, 63], despite the lack of statistical significance in these associations. Moreover, pregnant and breastfeeding women living in urban areas exhibited higher adherence compared to those living in rural settings. This result may be due to challenging socioeconomic conditions in rural areas, constraining access to transportation to healthcare facilities [77].
Our meta-analysis revealed that disclosure of HIV status to partner and/or family members were associated with adherence to option B + ART. Pregnant and lactating women disclosing their status to a partner or family member were 1.74 times more likely to adhere to ART than those who do not disclose their status. This positive association has also been reported in other studies. This could be due to the support received after disclosing their status, which encourages continued adherence in the fight against HIV. Additionally, our study highlighted that pregnant and breastfeeding women receiving support or involvement from partners or anyone were three times more likely to adhere to ART than those lacking such support. Similar associations have been reported in previous meta-analyses [69, 75]. However, for this support to be effective, it needs to be consistent and complemented by additional interventions such as structural support or education [70].
Counselling received by pregnant and breastfeeding women emerged as a key predictor of good adherence in our study. This finding aligns with results from a meta-analysis by Wubneh et al. in 2022, indicating that pregnant and breastfeeding women who received counseling during the antenatal period were five times more likely to adhere to ART compared to those who did not receive counseling [78].
Rapid ART initiation is strongly recommended by the WHO, due to its strong association with adherence in adults and adolescents [79]. Clinical stage at ART initiation significantly influences adherence among individuals living with HIV, especially pregnant and breastfeeding women. Our meta-analysis demonstrated that pregnant and breastfeeding women initiating option B + ART at WHO clinical stage I were approximately two times more likely to be adherent compared to those initiating option B + ART at clinical stage II or higher. A study in Northern Ethiopia similarly found that HIV patients starting treatment at stage I were two times (AOR: 2.194; 95% CI: 1.116–4.314) more likely to adhere to prescribed ART compared to those starting at WHO stage IV [80]. This disparity could be linked to an increased medication burden due to additional treatments for possible opportunistic infections that may occur.
A good knowledge on PMTCT or HIV was associated with good adherence in our study. Pregnant and breastfeeding women who had good knowledge on PMTCT and/or HIV were twice as likely to adhere compared to those with limited knowledge. It should be noted that knowledge on PMTCT and/or HIV has been proven to be a predictor of retention in care and, consequently, adherence to ART [81, 82]. The awareness of the benefits of the treatment for them and for their exposed children may increase their willingness to maintain their infants’ safety; pushing to follow their treatment.
Moreover, the results of our moderator analysis revealed that individual-level behaviour plays a substantial role in improving adherence in the pregnancy and postpartum periods. However, a meta-analysis on adherence interventions for women with HIV suggested that in addition to individual-level behaviour, interventions should incorporate structural factors like peer counselor care and additional clinic support staff trained in HIV care to ensure comprehensive follow-up, both at clinics and home [74].
Evidence has shed light on gender-based disparities in the adherence to ART [74, 83]. Women, globally, have been shown to encounter several barriers that impede their adherence to ART, encompassing emotional distress, stigma, negative effects of poor social relationships, and mental health barriers, such as depression, which robustly predicts non-adherence to ART [74, 84]. Furthermore, distinct life events like pregnancy and postpartum periods introduce unique challenges and concerns, making pregnant and/or breastfeeding women more vulnerable to the impact of various barriers on their medication adherence. Our meta-analysis has identified specific barriers within this sub-population, including low educational level, residing in rural areas, non-disclosure of HIV status, lack of social support, inadequate counseling, later initiation of ART, and limited knowledge about HIV and PMTCT. The recognition of these obstacles is vital in designing targeted interventions that address the unique needs of pregnant and breastfeeding women, in order to enhance ART adherence and promote better health outcomes in the Sub-Saharan African context.
Strengths and limitation of the study
This meta-analysis is the first to determine the pooled proportion of adherence to pregnancy and breastfeeding in the option B + era in SSA. We used various databases to search published studies, and the rigorous methodology of selection facilitated the collection of a large number of articles. Moreover, we strictly followed the PRISMA guidelines for reporting systematic reviews and meta-analyses using a critical appraisal of study quality. Furthermore, no evidence of publication bias was observed, and sensitivity analysis did not reveal a significant change in the prevalence of adherence.
Despite these strengths, our study had some limitations. As we conducted a meta-analysis of observational studies, this study is prone to several biases, including selection and confounding bias in each individual study. Moreover, we observed significant between-study variability (high heterogeneity), indicating significant variations in adherence across studies, probably due to the methodological differences between the studies, including difference in the population, thresholds used, time frames, and measurement methods. To address heterogeneity, we used random-effects models for analysis. Subgroup and meta-regression analyses were used to analyse heterogeneity but did not entirely reveal the source of high heterogeneity. Another limitation is information bias as the main measurement method used in the studies was self-reporting which may have overestimated adherence level and consequently the pooled prevalence of adherence reported in our meta-analysis. Furthermore, we did not include unpublished studies, and therefore, may have missed relevant articles. Lastly, we failed to estimate the prevalence of adherence at different points in the postpartum period since it has been demonstrated that the adherence declines with time.
Conclusions
In conclusion, our study revealed that three out of ten pregnant and breastfeeding women failed to achieve adequate levels of adherence to option B + ART in SSA. Notably, postpartum period exhibited the lowest adherence rates. To enhance adherence during these pivotal stages, interventions targeting individual factors including educational level, area of residence, disclosure status, WHO clinical stage at ART initiation, support of anyone or involvement from a partner, receiving counseling, and knowledge on PMTCT/HIV are crucial. Additionally, integrating these interventions with structural components, like the presence of peer counselors, is vital for an effective approach.
Availability of data and materials
All data used in the analysis are freely and publicly available from the cited papers with full citation listed in the reference section.
Abbreviations
- AACTG:
-
Adult AIDS Clinical Trial Groups
- AHRQ:
-
Agency for Healthcare Research and Quality
- ART:
-
Antiretroviral Therapy
- CASE:
-
Center for Adherence Support Evaluation
- DBS:
-
Dry Blood Spot
- MMAS:
-
Modified Morisky Medication Adherence Scale
- MPR:
-
Medication Possession Ratio
- MTCT:
-
Mother-To-Child Transmission
- NOS:
-
Newcastle Ottawa Scale
- OR:
-
Odds Ratio
- PMTCT:
-
Prevention of Mother-To-Child Transmission
- SSA:
-
Sub-Saharan Africa
- SR:
-
Self-Report
- VAS:
-
Visual Analogue Scale
- WHO:
-
World Health Organization
References
World Health Organization. Mother-to-child transmission of HIV. https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/hiv/prevention/mother-to-child-transmission-of-hiv. Accessed 22 Nov 2022.
UNAIDS. 2015 progress report on the global plan: toward the elimination of new infections among children and keeping their mothers alive. 2015. Available on: https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/hiv/prevention/mother-to-child-transmission-of-hiv. Accessed 22 Nov 2022.
UNAIDS. Women and girls carry the heaviest HIV burden in sub-Saharan Africa. Available on: https://www.unaids.org/en/resources/presscentre/featurestories/2022/march/20220307_women-girls-carry-heaviest-hiv-burden-sub-saharan-africa. Accessed 22 Nov 2022.
UNICEF. Elimination of mother-to-child transmission: Progress in reducing new HIV infections among children has stagnated in recent years. 2023. Available on: https://data.unicef.org/topic/hivaids/emtct/. Accessed 9 Mar 2023.
WHO/UNAIDS/UNICEF. The Global Alliance to end AIDS in children. Available on: https://www.unaids.org/sites/default/files/media_asset/global-alliance-end-AIDS-in-children_en.pdf. Accessed 9 Mar 2023.
World Health Organization (WHO). Validation of eliminating of mother-to-child transmission of HIV, syphilis and hepatitis B. 2023. Available on: https://www.who.int/initiatives/triple-elimination-initiative-of-mother-to-child-transmission-of-hiv-syphilis-and-hepatitis-b/validation. Accessed 14 Feb 2023.
Muyunda B, Musonda P, Mee P, Todd J, Michelo C. Effectiveness of Lifelong ART (Option B+) in the Prevention of Mother-to-Child Transmission of HIV Programme in Zambia: Observations Based on Routinely Collected Health Data. Front Public Health. 2020;7.
DiCarlo AL, Gachuhi AB, Mthethwa-Hleta S, Shongwe S, Hlophe T, Peters ZJ, et al. Healthcare worker experiences with Option B+ for prevention of mother-to-child HIV transmission in eSwatini: findings from a two-year follow-up study. BMC Health Serv Res. 2019;19:210.
Dlamini N, Ntuli B, Madiba S. Perceptions and Experiences of Participating in PMTCT Option B Plus: An Explorative Study on HIV-positive Pregnant Women in Eswatini. Open Public Health J. 2021;14.
The Embryo Project Encyclopedia. World Health Organization Guidelines (Option A, B, and B+) for Antiretroviral Drugs to Treat Pregnant Women and Prevent HIV Infection in Infants. 2021. Available on: https://embryo.asu.edu/pages/world-health-organization-guidelines-option-b-and-b-antiretroviral-drugs-treat-pregnant-women. Accessed 22 Nov 2022.
Ebuy H, Yebyo H, Alemayehu M. Level of adherence and predictors of adherence to the Option B+ PMTCT programme in Tigray, northern Ethiopia. Int J Infect Dis. 2015;33:123–9.
Hassan F, Renju J, Songo J, Chimukuche RS, Kalua T, McLean E, et al. Implementation and experiences of integrated prevention of mother-to-child transmission services in Tanzania, Malawi and South Africa: A mixed methods study. Glob Public Health. 2021;16:201–15.
UNICEF. 2021 Sub-Saharan Africa HIV Snapshot: Children and Adolescents. 2021. Available on: https://www.childrenandaids.org/sites/default/files/2022-01/2021%20Sub-Saharan%20Africa%20HIV%20Snapshot%20Children%20and%20Adolescents_0.pdf. Accessed 15 Feb 2023.
Dada AO, Abubakar A, Bashorun A, Nguku P, Oladimeji A. Predictors of adherence to option B+ approach for the prevention of mother to child transmission of human immunodeficiency virus in Abuja, 2017. Pan Afr Med J. 2021;38:54.
Vrazo AC, Sullivan D, Phelps BR. Eliminating Mother-to-Child Transmission of HIV by 2030: 5 Strategies to Ensure Continued Progress. Glob Health Sci Pract. 2018;6:249–56.
Abdisa S, Tenaw Z. Level of adherence to option B plus PMTCT and associated factors among HIV positive pregnant and lactating women in public health facilities of Hawassa city. Southern Ethiopia PLoS One. 2021;16:e0255808.
Adeniyi OV, Ajayi AI. Level and determinants of postpartum adherence to antiretroviral therapy in the Eastern Cape. South Africa PLoS One. 2020;15:e0229592.
Decker S, Rempis E, Schnack A, Braun V, Rubaihayo J, Busingye P, et al. Prevention of mother-to-child transmission of HIV: Postpartum adherence to Option B+ until 18 months in Western Uganda. PLoS ONE. 2017;12:e0179448.
Aduloju OP, Aduloju T, Ade-Ojo IP, Akintayo AA. Medication adherence in HIV-positive pregnant women on antiretroviral therapy attending antenatal clinics in Ado metropolis, south-west Nigeria : a multicentre study. South Afri J Obstet Gynaecol. 2020;26:65–70.
Agboeze J, Ogah OE, Robinson O, Matthew NI, Chukwuemeka U, Ikeola A. Determinants of Adherence to Antiretroviral Therapy among HIV-Positive Women Accessing Prevention of Mother to Child Transmission Services in Ebonyi State, Nigeria. Ann Med Health Sci Res. 2018.
Wondimu F, Yetwale F, Admassu E, Binu W, Bulto GA, Lake G, et al. Adherence to Option B+ Care for the Prevention of Mother-to-Child Transmission Among Pregnant Women in Ethiopia. HIV. 2020;12:769–78.
Adeniyi OV, Ajayi AI, Ter Goon D, Owolabi EO, Eboh A, Lambert J. Factors affecting adherence to antiretroviral therapy among pregnant women in the Eastern Cape South Africa. BMC Infect Dis. 2018;18:175.
Asefa EY, Dirirsa DE. Level of Good Adherence on Option B+ PMTCT and Associated Factors Among HIV Positive Pregnant and Lactating Mothers in Public Health Facilities of Ilu Abba Bor and Buno Bedele Zones, Oromia Regional State, Southwestern Ethiopia, 2018. HIV. 2020;12:789–98.
Mukose AD, Bastiaens H, Makumbi F, Buregyeya E, Naigino R, Musinguzi J, et al. What influences uptake and early adherence to Option B+ (lifelong antiretroviral therapy among HIV positive pregnant and breastfeeding women) in Central Uganda? A mixed methods study. PLOS ONE. 2021;16:e0251181.
Fedlu A, Alie B, Siraj Mohammed A, Adem F, Hassen A. Adherence to Antiretroviral Treatment for Prevention of Mother-to-Child Transmission of HIV in Eastern Ethiopia: A Cross-Sectional Study. HIV AIDS (Auckl). 2020;12:725–33.
Kadima N, Baldeh T, Thin K, Thabane L, Mbuagbaw L. Evaluation of non-adherence to anti-retroviral therapy, the associated factors and infant outcomes among HIV-positive pregnant women: a prospective cohort study in Lesotho. Pan Afr Med J. 2018;30:239.
UNICEF. Children, HIV and AIDS. Regional snapshot: Sub-Saharan Africa. Available on: https://www.childrenandaids.org/sites/default/files/2020-08/SSA%20Regional%20snapshot-%20v5-%206%20Nov%20%281%29.pdf. Accessed 6 Aug 2023.
Robbins RN, Spector AY, Mellins CA, Remien RH. Optimizing ART Adherence: Update for HIV Treatment and Prevention. Curr HIV/AIDS Rep. 2014;11:423–33.
Nachega JB, Uthman OA, Anderson J, Peltzer K, Wampold S, Cotton MF, et al. Adherence to antiretroviral therapy during and after pregnancy in low-income, middle-income, and high-income countries: a systematic review and meta-analysis. AIDS. 2012;26:2039–52.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9 W64.
World Health Organization. Regional Office for Africa. Implementation of Option B+ for Prevention of Mother-To-Child Transmission of HIV: the Malawi experience. World Health Organization. 2014. Available on: https://apps.who.int/iris/handle/10665/112849. Accessed 6 Aug 2023.
Rayyan. Tool for Systematic Literature Reviews. 2021. https://www.rayyan.ai/. Accessed 6 Aug 2023.
KoboToolbox. KoboToolbox. https://www.kobotoolbox.org/. Accessed 6 Aug 2023.
Ottawa Hospital Research Institute. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 7 Jan 2023.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–8832 Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002; 21:1539–58.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Itoua C, Nsongola DM, Koulimaya CG, Moutounou GM, Koko PS, Ngakengni NY, et al. Adherence to anti-retroviral drugs in pregnant and lactating HIV Positive women in Brazzaville. East Afr Med J. 2015;92:495–9.
Alcaide ML, Ramlagan S, Rodriguez VJ, Cook R, Peltzer K, Weiss SM, et al. Self-report and dry blood spot measurement of antiretroviral medications as markers of adherence in pregnant women in rural South Africa. AIDS Behav. 2017;21:2135–40.
Abebe W, Gebremariam M, Molla M, Teferra S, Wissow L, Ruff A. Prevalence of depression among HIV-positive pregnant women and its association with adherence to antiretroviral therapy in Addis Ababa Ethiopia. PLoS One. 2022;17:e0262638.
Aferu T, Doang G, Zewudie A, Nigussie T. Adherence to Antiretroviral Therapy Among HIV-Positive Pregnant Women on followup at Mizan Tepi University Teaching and Tepi General Hospitals, Southwest Ethiopia. J Prim Care Community Health. 2020;11:2150132720902561.
Atanga PN, Ndetan HT, Fon PN, Meriki HD, Muffih TP, Achidi EA, et al. Using a composite adherence tool to assess ART response and risk factors of poor adherence in pregnant and breastfeeding HIV-positive Cameroonian women at 6 and 12 months after initiating option B. BMC Pregnancy Childbirth. 2018;18:418.
Brittain K, Remien RH, Mellins CA, Phillips TK, Zerbe A, Abrams EJ, et al. Determinants of suboptimal adherence and elevated HIV viral load in pregnant women already on antiretroviral therapy when entering antenatal care in Cape Town. South Africa AIDS Care. 2018;30:1517–23.
Calder CL, O’Hara H, Tabatabai M, Maxwell CJ, Marryshow S, Ahonkhai AA, et al. Adherence to Combination Antiretroviral Therapy among Pregnant Women Enrolled in a HIV Prevention Program in Rural North-central Nigeria. Int J MCH AIDS. 2020;9:81–92.
Erlwanger AS, Joseph J, Gotora T, Muzunze B, Orne-Gliemann J, Mukungunugwa S, et al. Patterns of HIV Care Clinic Attendance and Adherence to Antiretroviral Therapy Among Pregnant and Breastfeeding Women Living With HIV in the Context of Option B+ in Zimbabwe. J Acquir Immune Defic Syndr. 2017;75(Suppl 2):S198-206.
Fernández-Luis S, Lain MG, Serna-Pascual M, Domínguez-Rodríguez S, Kuhn L, Liberty A, et al. Optimizing the World Health Organization algorithm for HIV vertical transmission risk assessment by adding maternal self-reported antiretroviral therapy adherence. BMC Public Health. 2022;22:1312.
Gebretsadik GG, Gebretnsae H, Ftwi M, Tesfahunegn A. Alarm Clock-Based Reminder for Improving Low Adherence on Option B Plus Antiretroviral Therapy Among HIV Positive Pregnant and Lactating Mothers in Northern Ethiopia. HIV. 2020;12:687–95.
Haas AD, Msukwa MT, Egger M, Tenthani L, Tweya H, Jahn A, et al. Adherence to Antiretroviral Therapy During and After Pregnancy: Cohort Study on Women Receiving Care in Malawi’s Option B+ Program. Clin Infect Dis. 2016;63:1227–35.
Larsen A, Magasana V, Dinh T-H, Ngandu N, Lombard C, Cheyip M, et al. Longitudinal adherence to maternal antiretroviral therapy and infant Nevirapine prophylaxis from 6 weeks to 18 months postpartum amongst a cohort of mothers and infants in South Africa. BMC Infect Dis. 2019;19(Suppl 1):789.
Mukosha M, Chiyesu G, Vwalika B. Adherence to antiretroviral therapy among HIV infected pregnant women in public health sectors: a pilot of Chilenje level one Hospital Lusaka. Zambia Pan Afr Med J. 2020;35:49.
Nsubuga-Nyombi T, Sensalire S, Karamagi E, Aloyo J, Byabagambi J, Rahimzai M, et al. Multivariate analysis of covariates of adherence among HIV-positive mothers with low viral suppression. AIDS Res Ther. 2018;15:9.
Omonaiye O, Kusljic S, Nicholson P, Mohebbi M, Manias E. Post Option B+ implementation programme in Nigeria: Determinants of adherence of antiretroviral therapy among pregnant women with HIV. Int J Infect Dis. 2019;81:225–30.
Omonaiye O, Nicholson P, Kusljic S, Mohebbi M, Manias E. Medication-based Refill Adherence Among Pregnant Women Living With HIV in Nigeria. Clin Ther. 2020;42:e209–19.
Onono M, Odwar T, Abuogi L, Owuor K, Helova A, Bukusi E, et al. Effects of Depression, Stigma and Intimate Partner Violence on Postpartum Women’s Adherence and Engagement in HIV Care in Kenya. AIDS Behav. 2020;24:1807–15.
Phillips T, Brittain K, Mellins CA, Zerbe A, Remien RH, Abrams EJ, et al. A Self-Reported Adherence Measure to Screen for Elevated HIV Viral Load in Pregnant and Postpartum Women on Antiretroviral Therapy. AIDS Behav. 2017;21:450–61.
Phillips T, Cois A, Remien RH, Mellins CA, McIntyre JA, Petro G, et al. Self-Reported Side Effects and Adherence to Antiretroviral Therapy in HIV-Infected Pregnant Women under Option B+: A Prospective Study. PLoS ONE. 2016;11:e0163079.
Ramlagan S, Peltzer K, Ruiter RAC, Barylski NA, Weiss SM, Sifunda S. Prevalence and Factors Associated with Fixed-Dose Combination Antiretroviral Drugs Adherence among HIV-Positive Pregnant Women on Option B Treatment in Mpumalanga Province, South Africa. Int J Environ Res Public Health. 2018;15:161.
Ramlagan S, Rodriguez VJ, Peltzer K, Ruiter RAC, Jones DL, Sifunda S. Self-Reported Long-Term Antiretroviral Adherence: A Longitudinal Study Among HIV Infected Pregnant Women in Mpumalanga. South Africa AIDS Behav. 2019;23:2576–87.
Schnack A, Rempis E, Decker S, Braun V, Rubaihayo J, Busingye P, et al. Prevention of Mother-to-Child Transmission of HIV in Option B+ Era: Uptake and Adherence During Pregnancy in Western Uganda. AIDS Patient Care STDS. 2016;30:110–8.
Tarekegn M, Baru A, Seme A. Levels of option B+ ART drugs adherence and associated factors among pregnant women following ART services at public health facilities of East Shawa Zone, Oromia. Ethiopia Sex Reprod Healthc. 2019;22:100459.
Tesfaye DJ, Hibistu DT, Abebo TA, Asfaw FT, Lukas K, Laelago T, et al. Option B plus antiretroviral therapy adherence and associated factors among HIV positive pregnant women in Southern Ethiopia. BMC Pregnancy Childbirth. 2019;19:82.
Tsegaye D, Deribe L, Wodajo S. Levels of adherence and factors associated with adherence to option B+ prevention of mother-to-child transmission among pregnant and lactating mothers in selected government health facilities of South Wollo Zone, Amhara Region, northeast Ethiopia, 2016. Epidemiol Health. 2016;38:e2016043.
Zacharius KM, Basinda N, Marwa K, Mtui EH, Kalolo A, Kapesa A. Low adherence to Option B+ antiretroviral therapy among pregnant women and lactating mothers in eastern Tanzania. PLoS ONE. 2019;14:e0212587.
Zoungrana-Yameogo WN, Fassinou LC, Ngwasiri C, Samadoulougou S, Traoré IT, Hien H, et al. Adherence to HIV Antiretroviral Therapy Among Pregnant and Breastfeeding Women, Non-Pregnant Women, and Men in Burkina Faso: Nationwide Analysis 2019–2020. Patient Prefer Adherence. 2022;16:1037–47.
Aregbesola OH, Adeoye IA. Self-efficacy and antiretroviral therapy adherence among HIV positive pregnant women in South-West Nigeria: a mixed methods study. Tanzan J Health Res. 2018;20.
Nutor JJ, Slaughter-Acey JC, Afulani PA, Obimbo MM, Mojola SA. The Relationship Between Counseling and Adherence to Antiretroviral Therapy Among Pregnant and Breastfeeding Women Enrolled in Option B. AIDS Educ Prev. 2020;32:378–91.
Matthews LT, Orrell C, Bwana MB, Tsai AC, Psaros C, Asiimwe S, et al. Adherence to HIV antiretroviral therapy among pregnant and postpartum women during the Option B+ era: 12-month cohort study in urban South Africa and rural Uganda. J Int AIDS Soc. 2020;23:e25586.
Harington B, Diprete B, Jumbe A, Ngongondo M, Limarzi LWallie S, et al. Safety and efficacy of Option B+ ART in Malawi: few severe maternal toxicity events or infant HIV infections among pregnant women initiating tenofovir/lamivudine/efavirenz. TMIH. 2019;24:1221–8.
Tsegaye R, Etafa W, Wakuma B, Mosisa G, Mulisa D, Tolossa T. The magnitude of adherence to option B plus program and associated factors among women in eastern African countries: a systematic review and meta-analysis. BMC Public Health. 2020;20:1812.
Omonaiye O, Nicholson P, Kusljic S, Manias E. A meta-analysis of effectiveness of interventions to improve adherence in pregnant women receiving antiretroviral therapy in sub-Saharan Africa. Int J Infect Dis. 2018;74:71–82.
Wanga I, Helova A, Abuogi LL, Bukusi EA, Nalwa W, Akama E, et al. Acceptability of community-based mentor mothers to support HIV-positive pregnant women on antiretroviral treatment in western Kenya: a qualitative study. BMC Pregnancy Childbirth. 2019;19:288.
Igumbor JO, Ouma J, Otwombe K, Musenge E, Anyanwu FC, Basera T, et al. Effect of a Mentor Mother Programme on retention of mother-baby pairs in HIV care: A secondary analysis of programme data in Uganda. PLoS ONE. 2019;14:e0223332.
Momplaisir FM, Fortune K, Nkwihoreze H, Groves AK, Aaron E, Jemmott JB. Outcome expectancies toward adherence to antiretroviral therapy for pregnant and postpartum women with HIV. Womens Health (Lond Engl). 2021;17:17455065211061094.
Pellowski JA, Price DM, Harrison AD, Tuthill EL, Myer L, Operario D, et al. A systematic review and meta-analysis of antiretroviral therapy (ART) adherence interventions for women living with HIV. AIDS Behav. 2019;23:1998–2013.
Costa JM, Torres TS, Coelho LE, Luz PM. Adherence to antiretroviral therapy for HIV/AIDS in Latin America and the Caribbean: Systematic review and meta-analysis. J Int AIDS Soc. 2018;21:e25066.
Mûnene E, Ekman B. Association between patient engagement in HIV care and antiretroviral therapy medication adherence: cross-sectional evidence from a regional HIV care center in Kenya. AIDS Care. 2015;27:378–86.
Adu C, Mensah KA, Ahinkorah BO, Osei D, Tetteh AW, Seidu A-A. Socio-demographic factors associated with medication adherence among People Living with HIV in the Kumasi Metropolis. Ghana AIDS Research and Therapy. 2022;19:50.
Adugna Wubneh C, Dessalegn Mekonnen B, Wesenyeleh Delelegn M, Asmare AK. Adherence to option B+ and its association with disclosure status and counseling among HIV-positive pregnant and lactating women in Ethiopia: systematic review and meta-analysis. Public Health. 2022;211:105–13.
World Health Organization. Guidelines for managing advanced HIV disease and rapid initiation of antiretroviral therapy. Available on: https://www.who.int/publications-detail-redirect/9789241550062. Accessed 6 Jan 2023.
Abdu M, Walelgn B. Determinant factors for adherence to antiretroviral therapy among adult HIV patients at Dessie Referral Hospital, South Wollo, Northeast Ethiopia: a case–control study. AIDS Res Ther. 2021;18:39.
Boateng D, Kwapong GD, Agyei-Baffour P. Knowledge, perception about antiretroviral therapy (ART) and prevention of mother-to-child-transmission (PMTCT) and adherence to ART among HIV positive women in the Ashanti Region, Ghana: a cross-sectional study. BMC Womens Health. 2013;13:2.
Gakii J, Maoga WN, Menza N. Knowledge, attitude and perception of HIV, ART and PMTCT among HIV infected pregnant women in narok sub-county hospitals. 2019.
Berg KM, Demas PA, Howard AA, Schoenbaum EE, Gourevitch MN, Arnsten JH. Gender Differences in Factors Associated with Adherence to Antiretroviral Therapy. J Gen Intern Med. 2004;19:1111–7.
Fauk NK, Mwanri L, Hawke K, Mohammadi L, Ward PR. Psychological and Social Impact of HIV on Women Living with HIV and Their Families in Low- and Middle-Income Asian Countries: A Systematic Search and Critical Review. Int J Environ Res Public Health. 2022;19:6668.
Acknowledgements
We are extremely grateful to Madam Valérie DURIEUX for her participation in the development of this research strategy.
Funding
LCF received a fellowship from the Commission de la Coopération au Développement (CDD) from the Académie de Recherche et d’Enseignement Supérieur (ARES).
Author information
Authors and Affiliations
Contributions
FKS developed the idea for the study. LCF and DS collected, analyzed and wrote the first draft of the manuscript. TD, NN and FKS revised the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fassinou, L.C., Songwa Nkeunang , D., Delvaux, T. et al. Adherence to option B + antiretroviral therapy and associated factors in pregnant and breastfeeding women in Sub-Saharan Africa: a systematic review and meta-analysis. BMC Public Health 24, 94 (2024). https://doi.org/10.1186/s12889-023-17004-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17004-9