Abstract
Background
Despite growing interest in and commitment to integration, or integrated care, the concept is ill-defined and the resulting evidence base fragmented, particularly in low- and middle-income countries (LMICs). Underlying this challenge is a lack of coherent approaches to measure the extent of integration and how this influences desired outcomes. The aim of this scoping review is to identify measurement approaches for integration in LMICs and map them for future use.
Methods
Arksey and O’Malley’s framework for scoping reviews was followed. We conducted a systematic search of peer-reviewed literature measuring integration in LMICs across three databases and screened identified papers by predetermined inclusion and exclusion criteria. A modified version of the Rainbow Model for Integrated Care guided charting and analysis of the data.
Results
We included 99 studies. Studies were concentrated in the Africa region and most frequently focused on the integration of HIV care with other services. A range of definitions and methods were identified, with no single approach for the measurement of integration dominating the literature. Measurement of clinical integration was the most common, with indicators focused on measuring receipt of two or more services provided at a single point of time. Organizational and professional integration indicators were focused on inter- and intra-organizational communication, collaboration, coordination, and continuity of care, while functional integration measured common information systems or patient records. Gaps were identified in measuring systems and normative integration. Few tools were validated or publicly available for future use.
Conclusion
We identified a wide range of recent approaches used to measure integration in LMICs. Our findings underscore continued challenges with lack of conceptual cohesion and fragmentation which limits how integration is understood in practice.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Integration has gained prominence as an approach to strengthen health systems towards Universal Health Coverage (UHC) [1,2,3,4]. Specific to low- and middle-income countries (LMICs), integration is frequently focused on the integration of vertical programs for specific disease or service packages for specified populations, including HIV/AIDS, tuberculosis (TB), and reproductive health care [4, 5], with the goal of increasing access to and coverage of prioritized services [6, 7]. Recommendations for integration in LMIC health systems are often based on normative policy guidance, with little evidence on the effectiveness of integration to improve health outcomes.
Underlying this challenge is a scarcity of evidence on measuring and evaluating integration as an intermediate outcome. This results in a weak understanding of the contextual complexities associated with integration reforms, constrains implementation of integrated approaches, and limits the generalizability of outcomes to improve health services [5, 6, 8,9,10,11].
Existing measurement approaches for integration
We identified three previous reviews on the measurement of integration. A 2009 systematic review of integrated health care delivery identified 24 different methods, mainly focused on structural and process aspects [12]. A 2016 systematic review identified 209 index instruments, 84% of which were focused on clinical integration [13]. Finally, a 2017 knowledge synthesis review for health systems integration located 114 unique tools [14], primarily measuring care coordination, patient engagement, and team engagement [14].
Considered together, these findings indicate that while the available measurement approaches in published literature have increased, there remains a lack of cohesiveness and conceptual maturity in constructs, definitions, and measurement approaches. People-centered care and clinical integration dominate the literature, with most evidence originating from high-income countries (HICs). Few tools have been validated in LMICs [12,13,14].
Rationale
A scoping review methodology is appropriate when the goal is to map an evolving field for the purpose of dissemination to practitioners and to identify gaps [15]. A search for “integrated health service delivery” on PubMed shows rapid growth of published studies since 2014. A scoping review of integration measurement approaches is warranted to capture new measurement tools, document where conceptual maturity has evolved, and identify gaps.
We are specifically motivated by a practical example – how to measure the integration of rehabilitation into health systems? Recent recommendations to integrate rehabilitation services into health systems have been made on conceptual merits, without a requisite understanding of what integration means or how to measure when it has been achieved [16]. Conceptually, rehabilitation is well positioned for an integrated approach, requiring services across the life course [17]. There is limited access to rehabilitative care in many LMIC health systems and an opportunity to improve access to services through an integrated, rather than verticalized, approach. Understanding how other scholars have measured integration can both support the development and measurement of integration of rehabilitative care into health systems and generate lessons for other health services.
We have focused our review on LMIC settings for two reasons. First, there are continued gaps in the evidence on integration approaches in LMICs [4, 18]. Second, the differing integration models in LMICs versus HICs warrants specific exploration of measurement approaches relevant to these settings [4, 5].
Objectives
This review had three objectives. First, to identify measurement tools, instruments, and frameworks developed for or utilized in LMIC health systems and distill the specific constructs, indicators, and measurement approaches that accompany them. Second, to compare measurement approaches across integration type. Third, to identify gaps in measurement approaches and their validation. The intended outcomes are to catalogue available approaches to measuring integration that can be adapted by researchers and practitioners in LMICs, and to identify where further evidence is required.
Methods
We adopted Arksey and O’Malley’s six stages for scoping reviews [15] and followed the checklist of Preferred Reporting Items for Systematic Reviews and Meta-Analyses’ Extension for Scoping Reviews (PRISMA-ScR) provided in Supplement 1 [19, 20].
Conceptual framework: the rainbow model for integrated care
A modified version of the Rainbow Model for Integrated Care (RMIC) conceptual framework, first developed and utilized by Bautista et al. [13], was selected to guide the review and align findings to previous work. The RMIC is a conceptual framework for understanding integrated care through the lenses of primary health care (PHC) and people-centeredness. RMIC measurement tools have been validated in multiple settings [21,22,23], making the framework appropriate to guide a measurement-focused scoping review.
The framework delineates six types of integration [24], which we used to organize our analysis. At the macro-level, systems integration – either horizontally linking care across similar levels of the system or vertically linking different levels of care – requires a consistent set of formal or informal rules to ensure continuum of care [24]. At the meso-level, professional and organizational integration consider how care is delivered [25]. Organizational integration focuses on inter-organizational relationships and governance, while professional integration emphasizes inter-professional partnerships [24, 25]. Clinical integration exists at the micro-level and focuses on care coordination [24, 25]. Finally, normative and functional integration can occur at the micro-, meso-, and macro-level [24, 25]. Normative integration considers the existence of a shared mission, values, and culture, while functional integration emphasizes non-clinical services including financing, data systems, and management [24, 25].
Search strategy
A replicable search strategy was developed using previous reviews on integration as index articles to select and refine search terms [12,13,14, 26]. Development of the search strategy was iterative and built upon the search strategy developed by Bautista et al. to promote comparability [13]. The starting search date of 15 June 2014 was selected to limit the overlap between this review period and past publications, due to an uptick in publications beginning in this period. The end date for the search was 21 November 2021 (the date of the final search). The final search strategy included four concepts: (i) integration and related constructs; (ii) instruments; (iii) measurement; and (iv) LMICs.
The search strategy was tested and refined in PubMed and translated for Embase and Web of Science. Supplement 2 includes the search results and search strategy for PubMed. Titles and abstracts were imported into Covidence systematic review software [27], and the duplicates were removed.
Study screening and selection
Titles and abstracts were screened utilizing pre-determined inclusion and exclusion criteria described in Table 1. Like past reviews on integration, this review focuses on the process of integration, and we excluded papers focused solely on measuring integration outcomes [12, 13]. Unlike past reviews and for comprehensiveness, we included qualitative studies if they utilized an explicit framework, model, or theory to assess dimensions of integration. Given the diversity in terminology, we considered a paper eligible if aligned with the broad definition of integration developed by the World Health Organization (WHO) [28] and utilized either ‘integration’ or related terminology.
Two reviewers independently screened each title and abstract against the inclusion and exclusion criteria. Subsequently, the full text of each article was reviewed by three reviewers independently. All reviewers screened and charted a common set of index articles to promote consistency. When it was unclear whether to include or exclude an article per our criteria, the article was discussed by the entire research team against the review framework. If consensus was not reached, a senior member of the research team made the final determination.
Data charting and extraction
Data was charted per a standardized extraction form developed specifically for this review in Microsoft Excel [30]. The extraction form was organized by the review’s conceptual framework and is provided in Supplement 3. The objective of the review was to capture and synthesize all available evidence within an evolving field, so we did not review articles for quality. Results were analyzed by the type of integration per the RMIC, as this was determined to be the most salient aspect of the framework.
Patient and public involvement
None.
Results
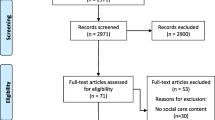
A total of 2,206 studies were located across databases. 322 duplicates were excluded. Titles and abstracts of the remaining 1,884 articles were reviewed. 432 articles were included for full text review and simultaneous data extraction. Data extraction was conducted using 99 articles (Fig. 1).
Study characteristics
Table 2 provides an overview of study characteristics for included studies, organized by the RMIC’s integration type.
Study population
The most common study populations in our sample were health care providers, followed by patients. Studies that included multiple participants included government, non-governmental organizations, health managers, researchers, donors, and communities.
Geography and income level
Our inclusion criteria included any LMIC; however, included studies clustered within specific income levels, regions, and countries (Fig. 2). Middle-income countries were more represented (n = 74) than low-income countries (n = 17). Within sub-Saharan Africa, 70.58% of papers were from five countries (Kenya, n = 10; South Africa, n = 8; Ethiopia, Swaziland, Malawi, n = 6). 45.45% of papers from Latin America and Caribbean were from Brazil, and 75% of papers from East Asia and Pacific were from China.
Types of services
Included studies were largely focused on a few health services. HIV services were commonly integrated with sexual and reproductive health (SRH) care (n = 9), family planning (FP) (n = 7), TB (n = 4) and non-communicable diseases (NCDs) (n = 4). PHC services, both alone (n = 11) and vertically integrated with secondary health care (n = 4), were the second most common.
Approaches to assessing integration
Table 3 maps included articles against each component of the review framework. We present the results by the type of integration as defined by the RMIC and identify commonly utilized constructs, indicators, and methods for each integration type. Supplement Three provides the full data extraction sheet.
Clinical integration (micro-level) Footnote 1
The RMIC defines clinical integration as, “the coordination of person-focused care in a single process across time, place, and discipline.” [25] 42 papers were determined to measure clinical integration alone, making it the most common type of integration measured by included studies.
Quantitative methods used to measure clinical integration
We identified some consistency in the indicators utilized for clinical integration. Most often, indicators for two or more services were developed specifically for the study and measured the extent to which those services were delivered jointly. The two most common indicators were variations on (1) testing, screening, or counseling a patient with one condition for the other condition or service need [32,33,34,35,36,37,38,39,40,41,42,43,44,45,46]; and (2) availability of services on the same day, whether via joint treatment by the same provider or in the same visit by different providers [38, 40, 41, 46,47,48,49,50,51,52,53,54,55,56,57,58].
Other indicators included variations on (3) internal and external referral practices [32, 41, 42, 47]; (4) common treatment or counseling spaces [41, 47, 50]; (5) availability or receipt of commodities, equipment, and or medications for two or more conditions [38, 44, 49, 50, 52, 59]; and (6) provider knowledge on two or more services [35, 39, 52, 55, 60].
Surveys to measure clinical integration
Eighteen papers developed or adapted survey instruments to measure clinical integration; of these, 10 papers surveyed health care providers [34, 35, 38, 40, 42, 46, 60,61,62,63], and eight surveyed patients [35, 43, 44, 48, 54, 59, 62, 64].
Papers measuring clinical integration often combined provider survey data with other methods to assess the extent of integration. For example, Pfaff et al. developed an integration indicator for the availability of NCD and anti-retroviral therapy (ART) services, which was accompanied by a series of facility readiness indicators and qualitative interviews to assess the ability of HIV programs to provide NCD care [38]. Sheahan et al. utilized provider surveys and facility audit data to develop a provider and facility integration index, which was analyzed longitudinally to understand the extent of integration in comparison to baseline facility and provider characteristics [46]. Similarly, Milford et al. conducted baseline and endline provider surveys to measure whether service integration improved after an HIV and SRH service integration training intervention [42].
Papers administering patient surveys focused on similar indicators but relied on patient experience or recall of how services were provided. For example, Church et al. and Biswas et al. used client exit surveys to assess integrated services and counseling received during patient visits [43, 64].
Use of secondary data sources
Fifteen papers relied on secondary data to measure clinical integration. Of these, 10 used facility-level data [32, 34, 35, 49, 50, 52, 55, 57, 58, 65], and five used patient medical records [33, 37, 39, 59, 66].
At the facility-level, Adamchak et al. determined the feasibility of measuring the integration of family planning (FP) and HIV services from existing health management information systems (HMIS) [32]. HMIS indicators included the proportion of HIV-related service clients screened for FP and the proportion of FP clients that received an HIV test at a family planning service delivery point. Kanyangarara et al. used data from existing facility surveys to measure the availability of integrated FP services in HIV treatment facilities [52].
Patient data included medical records and household surveys. Using patient records, Moucheraud et al. examined whether patients filled hypertension medication and ART during a single visit [59], while Mitiku et al. assessed the proportion of TB patients tested for HIV and vice versa [33].
Other quantitative methods
Four papers used economic analysis to compare the costs of integrated service models compared to non-integrated models [67,68,69,70]. We considered cost-effectiveness as a plausible approach for assessing the level of integration and therefore included it in the review. For example, Wall et al. compared the actual costs of an integrated HIV and FP program to the historical costs of providing separate services [67], and Vodicka et al. estimated costs using time in motion data for integrating cervical cancer screening into HIV care [68]. Finally, three papers used a facility audit checklist or protocol to assess how integrated services were provided [41, 46, 47].
Qualitative methods to measure clinical integration
Eleven papers used interviews to assess clinical integration [39,40,41, 45, 55, 62, 64, 65, 71,72,73]. For example, Irungu conducted in-depth provider interviews to assess adherence with integrated service delivery protocols for pre-exposure prophylaxis (PrEP) implementation within HIV care [45].
Four papers used focus group discussions to assess barriers, enablers, and patient experiences with specific programs [36, 71, 72, 74]. Three papers utilized observations to assess how integrated services were provided at the health facility [41, 47, 50]. For example, McGinn et al. conducted facility audits in Malawi to observe HIV and FP services with a checklist to assess whether integrated treatment guidelines were applied at the facility. Qualitative data was then transformed into a quantitative percentage score [41]. Finally, two papers used client flow analysis to track how patients moved through clinical services [56, 74].
Organizational integration (meso-level)
Organizational integration is defined by the RMIC as, “inter-organizational relationships […] including common governance mechanisms, to deliver comprehensive services to a defined population.” [25] 10 papers were categorized as measuring organizational integration alone [75,76,77,78,79,80,81,82,83,84]. Organizational integration measurement constructs focused on inter-organizational coordination of care and collaboration.
Quantitative and qualitative methods to measure organizational integration
Of the 10 papers measuring organizational integration, seven utilized surveys to measure organizational integration [77,78,79,80,81,82,83]. For example, Li et al. adapted a measurement instrument to measure governance, shared goals and vision, formalization and internalization across collaborating health care organization providing NCD care [77]. Thomas et al. applied a network density analysis to measure the density of organizational networks providing integrated HIV and FP services, comparing the links, density, centralization, and reciprocity of organizations that received a network strengthening initiative compared to one without intervention [79].
Two papers used quantitative approaches to develop new or adapted organizational integration constructs in a specific health system [76, 84]. For example, Seyedani et al. developed an adapted model for organizational integration for the Iranian health system [84]. Factor analysis derived five organizational integration aspects: learning organizations, inter-organizational strategies, organizational features, interest management, and coordination of care and information [84].
Finally, Wang et al. applied a mixed method approach [75]. Three indices were used to measure the effect of organizational integration on care coordination compared to best practices [75].
Professional integration (meso-level)
Professional integration is defined as, “inter-professional partnerships based on shared competences, roles, responsibilities and accountability to deliver a comprehensive continuum of care to a defined population” in the RMIC [25]. Six papers were deemed to measure professional integration alone [85,86,87,88,89,90]. These papers emphasize measurement constructs of communication and collaboration across providers, leadership, and collaboration.
Quantitative and qualitative methods to measure professional integration
All papers measuring professional integration were quantitative and utilized surveys of providers [85,86,87,88, 90]; one paper also included government officials and patients in the study population [89]. Constructs or indicators used to measure professional integration were similar across included papers and emphasized communication across medical professionals for referrals or treatment across levels of the health system [86, 89], leadership and decision making [88], teamwork [85,86,87], provider communication for coordination of care [87,88,89], and provider collaborative capacity [90]. For example, Li et al. measured the change in professional integration within an integrated community HIV and addiction program [85]. Providers were randomized to receive a training on HIV and addiction services, and baseline and endline surveys were administered to providers to measure the relative increase in provider collaboration across the treatment and control groups [85]. Tao et al. assessed professional integration by calculating coordination scores for patients and providers [89]. Similarly, Shaqura et al. developed a new tool to measure interprofessional collaboration, with survey items focused on leadership, mission, communication, coordination, and decision making [88].
Systems integration (macro-level)
The RMIC defines systems integration as, “a horizontal and vertically integrated system, based on a coherent set of (formal and informal) rules and policies between care providers and external stakeholders for the benefit of people and populations.” [25]. Four papers measured systems integration [91,92,93,94], generally focused on the presence of specific services across health system building blocks [95].
Quantitative and qualitative methods to measure systems integration
Two papers utilized quantitative tools to measure vertical [94] or horizontal [93] systems integration. For example, Mbah et al. developed a facility-level integration checklist, which measured the extent of integration between HIV and general laboratory services [93]. Indicators of integration included common training, equipment, standard operating procedures, physical location, and quality assurance processes [93].
Two papers employed mixed methods approaches. Deconinck et al. measured the integration of acute malnutrition interventions into health systems using 29 indicators [92] aligned with the WHO’s six health systems building blocks [95]. Mensa et al. collected data on the extent of integration of neglected tropical diseases into the heath system through qualitative interviews organized around health systems components [91]. Qualitative data was converted to an index with scoring at three levels of the health system [91].
Functional integration (micro-, meso-, and macro-levels)
Per the RMIC, functional integration focuses on support functions, such as financial, management, and information systems [25]. One paper was categorized as measuring functional integration alone [96]. Mossie (2021) assessed the use of a common medical record card for use across the maternal health and FP service continuum at the PHC (community) level [96]. The authors used interviews to understand whether common medical record card was utilized to improve coordination and continuity of care [96].
Normative integration (micro-, meso-, and macro-levels)
According to the RMIC, normative integration is, “the development and maintenance of a common frame of reference” [25]. Normative integration was considered in four papers alongside other types of integration [97,98,99,100], and focused on shared values, culture, and vision. For example, Xu assessed the ‘degree of sharing of organizational culture’ and ‘adherence to public health service goal’ across three different integration models [100].
Multiple types of integration
We considered a study as measuring multiple types of integration if the indicators or framework components cut across multiple integration types as defined by the RMIC. 29 papers were categorized as measuring multiple types of integration.
Quantitative and qualitative methods to measure multiple types of integration in a single study.
Of the 29 studies measuring multiple types of integration, clinical integration (n = 19) and professional integration (n = 19) were the most common, followed by systems (n = 15), organizational (n = 13), functional (n = 9), and normative (n = 4). The most common combinations identified were clinical and professional (n = 4) and clinical and systems (n = 4).
Quantitative methods to measuring multiple types of integration
Eighteen papers describe a survey or questionnaire; of those, providers were the most surveyed (n = 14) [98,99,100,101,102,103,104,105,106,107,108,109,110,111]. Tang et al. developed a survey tool to measure cooperative behavior of physicians across individual and organizational factors, which included a range of items from culture and leadership to training and referrals [99].
Patients (n = 6) [98, 103, 106, 112,113,114], and health care managers (n = 3) were also surveyed [103, 110, 115]. For example, De Almedia et al. surveyed patients about access to care, scheduling, satisfaction, and awareness, while health providers and managers were asked about care provision, referral instruments, medical records, and protocols [106].
Secondary data was utilized in four studies [23, 116, 117]. Miguel-Esponda et al. used patient records to determine fidelity to integration protocols, and interviews were conducted to assess the extent of penetration of mental health care into PHC [116].
Other methods included facility audits [97, 118] and social network analysis [119]. Afrizal et al. assessed different integration types using quantitative data from ANC registers and qualitative interview data from midwives implementing an integrated ANC scheme [97]. Van Rensburg et al. combined semi-structured interviews with social network analysis to assess the nature and extent of collaborative relationships between state and non-state service providers [119].
Qualitative methods to measuring multiple types of integration
For qualitative methods, nine papers conducted semi-structured interviews; providers were the most common participants (n = 8) [97, 99, 100, 102, 106, 113, 118, 120], followed by health care managers (n = 4) [97, 113, 118, 120], and patients (n = 2) [100, 113].
Other qualitative methods included patient journey mapping [115] and facility-level observations [110, 118]. Bousquat et al. combined patient journey mapping with a provider and health manager survey [115]. Constructs measured included administrative and organizational structures, organization, team service integration, and information continuity [115]. An accompanying therapeutic itineraries approach mapped patient journeys against continuity of care components [115].
Discussion
Through this review, we identified 99 studies measuring integration in the health care sector in LMICs. The multitude of frameworks and constructs used by included studies illustrates the complexity and contextual nature of integration. Our review supports the assertion that integration suffers from conceptual immaturity [121] with inconsistent terminology and definitions serving as barriers to consolidate and compare findings.
Comparing measurement approaches identified
Analyzing included studies by the review framework identified patterns in measurement approaches. Similar to past reviews [13], the largest number of papers in our sample were measuring clinical integration. Papers measuring clinical integration were more likely to incorporate patients as a study population and were more likely to utilize existing secondary data. Indicators prioritized the integration of two or more services into a ‘one-stop-shop’ or point of care model. Professional and organizational integration papers were more likely to utilize provider surveys and were the most likely to be categorized along the continuum of integration. Professional integration constructs emphasized teamwork and collaboration across providers, while organizational integration measured similar constructs across organizations. Papers focused on systems integration represented a range of constructs and measurement approaches that were specifically tailored to the context. Indicators for functional integration focused on the integration of information systems. Constructs for normative integration focused largely on shared value systems and were only provided in tandem with other types of integration.
Gaps identified
Concentration of evidence in specific services and geographies
While our review included all LMICs, 58.65% of papers came from seven countries (China, Brazil, Kenya, South Africa, Ethiopia, Swaziland, Malawi), and 41.41% of papers measured the integration of another service into HIV care. Despite recommendations to consider integration across the continuum of care, nearly all studies focused on curative services, and no papers measured the integration of physical rehabilitation or palliative services. A key takeaway is that the focus of integration efforts and the resulting measurement approaches are context-specific, both in terms of which conditions or services are integrated and in the broader health systems structures responsible for that integration. However, normative recommendations for integration are often defined as service or context neutral. The mismatch between context-specific integration evidence and broader normative recommendation warrants further empirical inquiry.
Emphasis on specific integration models
Categorizing measurement approaches by the RMIC’s integration types provided insights into the goals of integration models. Indicators for clinical integration were often the single focus of a study, designed for integrating vertical disease programs (especially HIV) and focused on increasing service accessibility and utilization. In contrast, all other integration types were more likely to be measured in combination. This reflected more expansive horizontal and vertical integration models across the continuum of care. Like past reviews, our review identified limited measurement approaches for functional, systems, and normative integration [13].
Previous work indicates that integration models in LMICs are more likely to focus on the integration of two or more services to improve access or uptake [5]. Our findings from the Africa region reflected this, with papers largely focused on clinical integration of HIV and other services. In contrast, papers from Latin America and Asia more frequently reflected professional and organizational integration types more commonly associated with HICs [5]. 77% of included studies in Bautista et al.’s 2017 review on integration came from HIC, the majority of which focused on clinical integration, highlighting variation of integration models across country income levels [13]. Additional research can identify which integration models are common across different regions and service types.
Integration of entire sectors or service categories into the health system is especially poorly researched and likely to be particularly complex. Only two studies in our review measured a whole-sector approach to integration (examining nutrition and neglected tropical diseases) and highlight the importance of developing indicators across levels and components of the health system [91, 92]. These examples may be particularly instructive for the recent calls to integrate rehabilitation into health systems [16] and emphasize the importance of measuring non-clinical components to integration.
The need for publicly available instruments
Compared to past reviews [13], few studies in our review reported validity or reliability measures for quantitative instrument development, and qualitative studies rarely reported trustworthiness (Supplement 3). Few tools were publicly available, challenging the ability of future researchers to build on and adapt approaches we have documented here. In other cases, methodologies – for example, qualitative interview data converted to quantitative integration scores – lacked adequate description for outside readers, rendering the methods of measurement irreplicable. Therefore, while the findings of this review provide ideas for future researchers, it points to the need for appropriate documentation of measurement methods and availability of tools for adaptation.
Understanding implementation challenges for these tools and shared learnings are also crucial to develop consensus around utility of the above-mentioned tools and approaches. This would help to reduce redundancy, support the development of a comparable evidence-base for comprehensive measurement of integration across levels of the health system, and facilitate adaptation of tools to make them relevant for specific contexts and services.
Strengths and limitations
Our broad definition of measurement was a strength. This allowed us to capture qualitative and mixed methods articles that assessed integration through perception or experiences of target groups, as well as novel methodologies such as social network analysis. The exclusion of non-English papers was a limitation and resulted in the exclusion of ten papers.
The use of the adapted RMIC as the basis of the review framework was both a strength and limitation. Despite the original focus of the RMIC on PHC, the integration types present in the RMIC were identifiable in most included papers. This allowed us to use an organizing heuristic for the review based on existing literature and provided a theory-based approach to knowledge synthesis on a fragmented topic. However, included papers often utilized different definitions or terminology, which made it challenging to categorize. Few papers reported sufficient detail to be categorized across all the review framework’s components.
Some papers aligned with broader definitions or models of integration put forward by the WHO rather than aligning clearly to the definition of integrated care for the RMIC. We included these papers in our review as they fit our inclusion criteria and provided insights into measurement approaches. However, categorizing these approaches against the RMIC required additional interpretation of both the original framework and included papers.
A related observation is that many papers from LMICs were assessing new models for integration and were operational in nature, while the original RMIC framework is conceptual. This manifested in the way included studies were organized, often defining measurement constructs by components of an integration model that cut across multiple integration types. For example, we categorized measurement of the referral pathway to promote care continuity differently depending on the wording of survey items – provider collaboration was categorized as professional integration, intra-organizational partnerships were categorized as organizational integration, macro-level referral policies were categorized as systems integration, and common information management system to manage referrals was categorized as functional integration. Therefore, similar studies seeking to measure care continuity through referrals could be categorized differently based on the specific measurement approach. This is a limitation, both of our review and the broader literature.
Finally, our search began in June 2014 to align with past reviews; however, previous reviews were limited to quantitative studies. There may be additional qualitative studies measuring integration prior to the start of our search which are not captured in an existing review on this topic.
Conclusion
This review aimed to categorize and describe measurement approaches for integration in LMICs. Our findings describe measurement approaches that can be adapted for future research and practice and identify critical conceptual and practical gaps towards strengthening measurement of integration in LMIC health systems.
Availability of data and materials
All data analyzed in this study is provided in Supplement 3. This includes the data extraction sheet and complete list of included papers.
Notes
In this and the following results sections, the number of papers is reported per method utilized. Some papers used multiple methods and are counted more than once.
References
Gröne O, Garcia-Barbero M, WHO European Office for Integrated Health Care Services. Integrated care: a position paper of the WHO European Office for Integrated Health Care Services. Int J Integr Care. 2001;1:e21.
World Health Organization. Universal health coverage (UHC). World Health Organization. 2020. https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc). Accessed 10 Nov 2020.
Integrated health services networks. Pan American Health Organization. https://www.paho.org/en/topics/integrated-health-services-networks. Accessed 14 Feb 2021.
Lê G, Morgan R, Bestall J, Featherstone I, Veale T, Ensor T. Can service integration work for universal health coverage? Evidence from around the globe. Health Policy. 2016;120(4):406–19.
Mounier-Jack S, Mayhew SH, Mays N. Integrated care: learning between high-income, and low- and middle-income country health systems. Health Policy Plan. 2017;32(Suppl 4):iv6-12.
Topp SM, Abimbola S, Joshi R, Negin J. How to assess and prepare health systems in low- and middle-income countries for integration of services - A systematic review. Health Policy Plan. 2018;33(2):298–312.
Chaitkin M, Blanchet N, Su Y, Husband R, Moon P, Rowan A, et al. Integrating Vertical Programs into Primary Health Care. Washington DC: Results for Development; 2018.
Nolte E. Evidence Supporting Integrated Care. In: Amelung V, Stein V, Goodwin N, Balicer R, Nolte E, Suter E, editors. Handbook Integrated Care. Cham: Springer International Publishing; 2017. p. 25–38.
Goddard M, Mason AR. Integrated care: a pill for all ills? Int J Health Policy Manag. 2017;6(1):1–3.
World Health Organization. People-centred and integrated health services: an overview of the evidence Interim Report. Geneva: World Health Organization; 2015.
Dudley L, Garner P. Strategies for integrating primary health services in low- and middle-income countries at the point of delivery. Cochrane Database of Systematic Reviews. 2011;7:CD003318.
Strandberg-Larsen M, Krasnik A. Measurement of integrated healthcare delivery: a systematic review of methods and future research directions. Int J Integr Care. 2009;9:e01.
Bautista MAC, Nurjono M, Lim YW, Dessers E, Vrijhoef HJ. Instruments measuring integrated care: a systematic review of measurement properties. Milbank Q. 2016;94(4):862–917.
Suter E, Oelke ND, da Silva Lima MA, Stiphout M, Janke R, Witt RR, et al. Indicators and measurement tools for health systems integration: a knowledge synthesis. Int J Integr Care. 2017;17(6):4.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
World Health Organization. Rehabilitation in health systems. Geneva: World Health Organization; 2017.
Mills J-A, Marks E, Reynolds T, Cieza A. Rehabilitation: Essential along the Continuum of Care. In: Jamison D, Gelbend H, Horton S, editors. Disease Control Priorities: Improving Health and Reducing Poverty. 3rd ed. Washington, D.C: The International Bank for Reconstruction and Development / The World Bank; 2017.
Dudley L, Garner P. Strategies for integrating primary health services in low- and middle-income countries at the point of delivery. Cochrane Database Syst Rev. 2011;7:CD003318.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Valentij PP, Pereira F, Sterner CW, Vrijhoef HJM, Ruwaard D, Hegbrant J, et al. Validation of the rainbow model of integrated care measurement Tools (RMIC-MTs) in renal care for patient and care providers. PLoS ONE. 2019;14(9):e0222593.
Nurjono M, Valentijn PP, Bautista MAC, Wei LY, Vrijhoef HJM. A prospective validation study of a rainbow model of integrated care measurement tool in Singapore. Int J Integr Care. 2016;16(1):1–6.
Huang Y, Zhu P, Chen L, Wang X, Valentijn P. Validation of the care providers version of the Rainbow Model of Integrated Care-measurement tool in Chinese primary care systems. BMC Health Serv Res. 2020;20:727.
Valentijn PP, Schepman SM, Opheij W, Bruijnzeels MA. Understanding integrated care: A comprehensive conceptual framework based on the integrative functions of primary care. Int J Integr Care. 2013;13:e010.
Valentijn PP, Boesveld IC, van der Klauw DM, Ruwaard D, Struijs JN, Molema JJW, et al. Towards a taxonomy for integrated care: A mixed-methods study. Int J Integr Care. 2015;15:e003.
Neill R, Hasan MZ, Das P, Venugopal V, Jain N, Arora D, et al. Evidence of integrated health service delivery during COVID-19 in low and lower-middle-income countries: protocol for a scoping review. BMJ Open. 2021;11(5):e042872.
Veritas Health Innovation. Covidence systematic review software. Melbourne: Veritas Health Innovation.
Waddington C, Egger D. Integrated health services - what and why? Geneva: World Health Organization; 2018.
World Bank Country and Lending Groups – World Bank Data Help Desk. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed 25 Oct 2020.
Microsoft Corporation. Microsoft Excel. Redmond: Microsoft Corporation.
World Bank Country and Lending Groups. World Bank. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed 31 Jan 2021.
Adamchak SE, Okello FO, Kaboré I. Developing a system to monitor family planning and HIV service integration: results from a pilot test of indicators. J Fam Plann Reprod Health Care. 2016;42(1):24–9.
Mitiku AM, Asfaw GZ, Tsegay HT, Zewdie BY, Tesfay AM. Levels and predictors of TB-HIV diagnostic service linkage and testing in government hospitals of southern zone of Tigray, Northern Ethiopia. Afr Health Sci. 2019;19(3):2335–46.
Ndagijimana A, Rugigana E, Uwizeye CB, Ntaganira J. One-stop TB-HIV services evaluation in Rwanda: comparison of the 2001–2005 and 2006–2010 cohorts. Public Health Action. 2015;5(4):209–13.
Wagner GJ, Ngo V, Glick P, Obuku EA, Musisi S, Akena D. INtegration of DEPression Treatment into HIV Care in Uganda (INDEPTH-Uganda): study protocol for a randomized controlled trial. Trials. 2014;15:248.
Young N, Achieng F, Desai M, Phillips-Howard P, Hill J, Aol G, et al. Integrated point-of-care testing (POCT) for HIV, syphilis, malaria and anaemia at antenatal facilities in western Kenya: a qualitative study exploring end-users’ perspectives of appropriateness, acceptability and feasibility. BMC Health Serv Res. 2019;19(1):74.
Sinai I, Cleghorn F, Kinkel HF. Improving management of tuberculosis in people living with HIV in South Africa through integration of HIV and tuberculosis services: a proof of concept study. BMC Health Serv Res. 2018;18:711.
Pfaff C, Scott V, Hoffman R, Mwagomba B. You can treat my HIV – But can you treat my blood pressure? Availability of integrated HIV and non-communicable disease care in northern Malawi. Afr J Prim Health Care Fam Med. 2017;9(1):1151.
Khan MA, Walley JD, Ali S, King R, Khan SE, Khan N, et al. Process evaluation of integrated diabetes management at primary healthcare facilities in Pakistan: a mixed-methods study. BJGP Open. 2018;2(4):bjgpopen18X101612.
Yugbaré Belemsaga D, Goujon A, Bado A, Kouanda S, Duysburgh E, Temmerman M, et al. Integration of postpartum care into child health and immunization services in Burkina Faso: findings from a cross-sectional study. Reprod Health. 2018;15(1):171.
McGinn EK, Irani L. Provider-initiated family planning within HIV services in Malawi: did policy make it into practice? Glob Health Sci Pract. 2019;7(4):540–50.
Milford C, Beksinska M, Greener LR, Mabude Z, Smit J. Implementation of a sexual and reproductive health service integration model: South African providers’ reports. Cogent Med. 2019;6(1):1592740.
Biswas KK, Pearson E, Shahidullah SM, Sultana S, Chowdhury R, Andersen KL. Integrating postabortion care, menstrual regulation and family planning services in Bangladesh: a pre-post evaluation. Reprod Health. 2017;14:37.
Demissie DB, Mmusi-Phetoe R. Integration of family planning services with HIV treatment for women of reproductive age attending ART clinic in Oromia regional state. Ethiopia Reprod Health. 2021;18:102.
Irungu EM, Odoyo J, Wamoni E, Bukusi EA, Mugo NR, Ngure K, et al. Process evaluation of PrEP implementation in Kenya: adaptation of practices and contextual modifications in public HIV care clinics. J Int AIDS Soc. 2021;24(9):e25799.
Sheahan KL, Speizer IS, Orgill-Meyer J, Curtis S, Weinberger M, Paul J, et al. Facility-level characteristics associated with family planning and child immunization services integration in urban areas of Nigeria: a longitudinal analysis. BMC Public Health. 2021;21:1379.
Mutemwa R, Mayhew SH, Warren CE, Abuya T, Ndwiga C, Kivunaga J. Does service integration improve technical quality of care in low-resource settings? An evaluation of a model integrating HIV care into family planning services in Kenya. Health Policy Plan. 2017;32(suppl_4):iv91-101.
Nguyen Bich D, Korthuis PT, Nguyen Thu T, van Dinh H, le Minh G. HIV patients’ preference for integrated models of addiction and HIV treatment in Vietnam. J Subst Abuse Treat. 2016;69:57–63.
Odjidja EN, Gatasi G, Duric P. Delivery of integrated infectious disease control services under the new antenatal care guidelines: a service availability and readiness assessment of health facilities in Tanzania. BMC Health Serv Res. 2019;19:153.
Obure CD, Jacobs R, Guinness L, Mayhew S, Vassall A. Does integration of HIV and sexual and reproductive health services improve technical efficiency in Kenya and Swaziland? An application of a two-stage semi parametric approach incorporating quality measures. Soc Sci Med. 2016;151:147–56.
Church K, Warren CE, Birdthistle I, Ploubidis GB, Tomlin K, Zhou W, et al. Impact of integrated services on HIV testing: a nonrandomized trial among Kenyan family planning clients. Stud Fam Plann. 2017;48:208.
Kanyangarara M, Sakyi K, Laar A. Availability of integrated family planning services in HIV care and support sites in sub-Saharan Africa: A secondary analysis of national health facility surveys. Reprod Health. 2019;16:60.
Mayhew S, Ploubidis GB, Sloggett A, Church K, Obure CD, Birdthistle I, et al. The integra Indexes of HIV and reproductive health integration. PLOS Oneq. 2016;11(1):e0146694.
Haskins JL, Phakathi SA, Grant M, Horwood CM. Integrating services for impact and sustainability: a proof-of-concept project in KwaZulu-Natal, South Africa. South African Family Practice. 2019;61(6):216–22.
Hassan S, Cooke A, Saleem H, Mushi D, Mbwambo J, Lambdin BH. Evaluating the integrated methadone and anti-retroviral therapy strategy in Tanzania using the RE-AIM framework. Int J Environ Res Public Health. 2019;16(5):728.
Birdthistle IJ, Mayhew SH, Kikuvi J, Zhou W, Church K, Warren CE, et al. Integration of HIV and maternal healthcare in a high HIV-prevalence setting: analysis of client flow data over time in Swaziland. BMJ Open. 2014;4(3):e003715.
Sheahan KL, Orgill-Meyer J, Speizer IS, Curtis S, Paul J, Weinberger M, et al. Development of integration indexes to determine the extent of family planning and child immunization services integration in health facilities in urban areas of Nigeria. Reprod Health. 2021;18(1):47.
Usman M, Anand E, Siddiqui L, Unisa S. Continuum of maternal health care services and its impact on child immunization in India: an application of the propensity score matching approach. J Biosoc Sci. 2021;53(5):643–62.
Moucheraud C, Hing M, Seleman J, Phiri K, Chibwana F, Kahn D, et al. Integrated care experiences and out-of-pocket expenditures: a cross-sectional survey of adults receiving treatment for HIV and hypertension in Malawi. BMJ Open. 2020;10(2):e032652.
Mutisya R, Wambua J, Nyachae P, Kamau M, Karnad SR, Kabue M. Strengthening integration of family planning with HIV/AIDS and other services: experience from three Kenyan cities. Reprod Health. 2019;16:62.
Milford C, Greener LR, Beksinska M, Greener R, Mabude Z, Smit J. Provider understandings of and attitudes towards integration: Implementing an HIV and sexual and reproductive health service integration model, South Africa. Afr J AIDS Res. 2018;17(2):183–92.
Milford C, Scorgie F, Rambally Greener L, Mabude Z, Beksinska M, Harrison A, et al. Developing a model for integrating sexual and reproductive health services with HIV prevention and care in KwaZulu-Natal. South Africa Reprod Health. 2018;15:189.
Paula CC de, Padoin SM de M, Silva CB da, Kleinubing RE, Ferreira T. Health care for children and adolescents with HIV: longitudinality assessment. Acta Paulista de Enfermagem. 2017;30(2):136–43.
Church K, Wringe A, Lewin S, Ploubidis GB, Fakudze P, Initiative I, et al. Exploring the feasibility of service integration in a low-income setting: a mixed methods investigation into different models of reproductive health and HIV care in Swaziland. PLoS ONE. 2015;10(5):e0126144.
Nelson AR, Cooper CM, Kamara S, Taylor ND, Zikeh T, Kanneh-Kesselly C, et al. Operationalizing integrated immunization and family planning services in rural Liberia: lessons learned from evaluating service quality and utilization. Glob Health Sci Pract. 2019;7(3):418–34.
Dadi TL, Medhin G, Kasaye HK, Kassie GM, Jebena MG, Gobezie WA, et al. Continuum of maternity care among rural women in Ethiopia: does place and frequency of antenatal care visit matter? Reprod Health. 2021;18:220.
Wall KM, Kilembe W, Inambao M, Hoagland A, Sharkey T, Malama K, et al. Cost-effectiveness of integrated HIV prevention and family planning services for Zambian couples. AIDS. 2020;34(11):1633–42.
Vodicka EL, Babigumira JB, Mann MR, Kosgei RJ, Lee F, Mugo NR, et al. Costs of integrating cervical cancer screening at an HIV clinic in Kenya. Int J Gynecol Obstet. 2017;136(2):220–8.
Shiri T, Birungi J, Garrib A v., Kivuyo SL, Namakoola I, Mghamba J, et al. Patient and health provider costs of integrated HIV, diabetes and hypertension ambulatory health services in low-income settings — an empirical socio-economic cohort study in Tanzania and Uganda. BMC Med. 2021;19:230.
Mayhew SH, Ploubidis GB, Sloggett A, Church K, Obure CD, Birdthistle I, et al. Innovation in evaluating the impact of integrated service-delivery: the integra indexes of HIV and reproductive health integration. PLoS ONE. 2016;11(1):e0146694.
Hamon JK, Krishnaratne S, Hoyt J, Kambanje M, Pryor S, Webster J. Integrated delivery of family planning and childhood immunisation services in routine outreach clinics: findings from a realist evaluation in Malawi. BMC Health Serv Res. 2020;20:777.
Zimba CC, Akiba CF, Matewere M, Thom A, Udedi M, Masiye JK, et al. Facilitators, barriers and potential solutions to the integration of depression and non-communicable diseases (NCDs) care in Malawi: a qualitative study with service providers. Int J Ment Health Syst. 2021;15(1):59.
Mayhew SH, Sweeney S, Warren CE, Collumbien M, Ndwiga C, Mutemwa R, et al. Numbers, systems, people: how interactions influence integration. Insights from case studies of HIV and reproductive health services delivery in Kenya. Health Policy Plan. 2017;32(Suppl 4):iv67-81.
Erhardt-Ohren B, Schroffel H, Rochat R. Integrated family planning and routine child immunization services in Benin: a process evaluation. Matern Child Health J. 2020;24(6):701–8.
Wang X, Birch S, Zhu W, Ma H, Embrett M, Meng Q. Coordination of care in the Chinese health care systems: a gap analysis of service delivery from a provider perspective. BMC Health Serv Res. 2016;16:571.
Wu X, Li S, Xu N, Wu D, Zhang X. Establishing a balanced scorecard measurement system for integrated care organizations in China. Int J Health Plann Manage. 2019;34(2):672–92.
Li XM, Rasooly A, Peng B, JianWang, Xiong SY. An analysis on intersectional collaboration on non-communicable chronic disease prevention and control in China: a cross-sectional survey on main officials of community health service institutions. BMC Health Serv Res. 2017;17:711.
Li H, Wei X, Wong MCS. Changes of the perceived quality of care for older patients with hypertension by community health centers in shanghai. BMC Fam Pract. 2017;18(1):114.
Thomas JC, Reynolds HW, Alterescu X, Bevc C, Tsegaye A. Improving referrals and integrating family planning and HIV services through organizational network strengthening. Health Policy Plan. 2016;31(3):302–8.
Ferrer APS, Brentani AVM, Sucupira ACSL, Navega ACB, Cerqueira ES, Grisi SJFE. The effects of a people-centred model on longitudinality of care and utilization pattern of healthcare services—Brazilian evidence. Health Policy Plan. 2014;29(Suppl 2):ii107-113.
Yuan S, Wang F, Zhao Y, Liu Y. Assessing perceived quality of primary care under hospital-township health centre integration: a cross-sectional study in China. Int J Health Plann Manage. 2020;35(1):e196-209.
León-Arce HG, Mogollón-Pérez A-S, Vargas I, Vázquez M-L. Changes in knowledge and use of clinical coordination mechanisms between care levels in healthcare networks of Colombia. Int J Health Plann Manage. 2021;36(1):134–50.
He J, Chen D, Tang Z, Cong L, Tian Y, Xie C, et al. How the health institution combinative contracting mechanism influences community residents’ patient experiences in Shanghai: a comparative study of data from two cross-sectional surveys. Int J Health Plann Manage. 2019;34(3):1036–54.
Seyedamini B, Riahi L, Farahani MMM, Tabibi SJ, Asl IM. The effective organizational factors in the health system integration. JIMS8M: The Journal of Indian Management Strategy. 2018;23(3):55.
Li L, Lin C, Liang L-J, Nguyen DB, Pham LQ, Le TA, et al. Community capacity building for HIV and addiction service integration: an intervention trial in Vietnam. AIDS Behav. 2022;26(1):123–31.
Sheiman I, Shevsky V. Concentration of health care providers: Does it contribute to integration of service delivery? Risk Manag Healthc Policy. 2019;12:153–66.
Sheiman I, Shevski V. Evaluation of health care delivery integration: the case of the Russian Federation. Health Policy. 2014;115(2-3):128–37.
Shaqura II, Baroud R, Sari AA. Collaboration among healthcare professionals at the public hospitals in Gaza: a quantitative study. J Integr Care. 2020;30(1):106–19.
Tao W, Zeng W, Yan L, Yang H, Wen J, Li W. The health service capacity of primary health care in West China: Different perspectives of physicians and their patients. BMC Health Serv Res. 2019;19:143.
Soko TN, Jere DL, Wilson LL. Healthcare workers’ perceptions on collaborative capacity at a referral hospital in Malawi. Health SA. 2021;26:1561.
Mensah EO, Aikins MK, Gyapong M, Anto F, Bockarie MJ, Gyapong JO. Extent of integration of priority interventions into general health systems: a case study of neglected tropical diseases program in the Western Region of Ghana. PLoS Negl Trop Dis. 2016;10(5):e0004725.
Deconinck H, Hallarou M, Criel B, Donnen P, Macq J. Integrating acute malnutrition interventions into national health systems: Lessons from Niger. BMC Public Health. 2016;16:249.
Mbah H, Negedu-Momoh OR, Adedokun O, Ikani PA, Balogun O, Sanwo O, et al. Implementing and measuring the level of laboratory service integration in a program setting in Nigeria. PLoS ONE. 2014;9(9):e107277.
Macinko J, Jimenez G, Cruz-Peñate M. Primary care performance in Dominica. Rev Panam Salud Publica. 2015;37(2):104-12.
World Health Organization. Everybody’s business– strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva: World Health Organization; 2007.
Mossie MY, Pfitzer A, Yusuf Y, Wondimu C, Bazant E, Bansal V, et al. Counseling at all contacts for postpartum contraceptive use: can paper-based tools help community health workers improve continuity of care? A qualitative study from Ethiopia. Gates Open Res. 2021;3:1652.
Afrizal SH, Hidayanto AN, Handayani PW, Besral B, Martha E, Markam H, et al. Evaluation of integrated antenatal care implementation in primary health care: a study from an urban area in Indonesia. J Integr Care. 2020;28(2):99–117.
Vázquez M-L, Vargas I, Unger J-P, de Paepe P, Mogollón-Pérez AS, Samico I, et al. Evaluating the effectiveness of care integration strategies in different healthcare systems in Latin America: the EQUITY-LA II quasi-experimental study protocol. BMJ Open. 2015;5(7):e007037.
Tang W, Wei L, Zhang L. Analysing a Chinese regional integrated healthcare organisation reform failure using a complex adaptive system approach. Int J Integr Care. 2017;17:3.
Xu J, Pan R, Pong RW, Miao Y, Qian D. Different models of hospital-community health centre collaboration in selected cities in China: A cross-sectional comparative study. Int J Integr Care. 2016;16(1):8.
Uyei J, Coetzee D, MacInko J, Weinberg SL, Guttmacher S. Measuring the degree of integrated tuberculosis and HIV service delivery in Cape Town, South Africa. Health Policy Plan. 2014;29(1):42–55.
Lovero KL, Lammie SL, van Zyl A, Paul SN, Ngwepe P, Mootz JJ, et al. Mixed-methods evaluation of mental healthcare integration into tuberculosis and maternal-child healthcare services of four South African districts. BMC Health Serv Res. 2019;19:83.
Marotta C, Lochoro P, Pizzol D, Putoto G, Mazzucco W, Saracino A, et al. Capacity assessment for provision of quality sexual reproductive health and HIV-integrated services in Karamoja. Uganda Afr Health Sci. 2020;20(3):1053–65.
Gallego-Ardila AD, Pinzón-Rondón ÁM, Mogollón-Pérez AS, Cardozo CX, Vargas I, Vázquez ML. Care coordination in two of Bogota’s public healthcare networks: a cross-sectional study among doctors. Int J Care Coord. 2019;22:127–39.
Vázquez ML, Vargas I, Garcia-Subirats I, Unger JP, de Paepe P, Mogollón-Pérez AS, et al. Doctors’ experience of coordination across care levels and associated factors. A cross-sectional study in public healthcare networks of six Latin American countries. Soc Sci Med. 2017;182:10–9.
de Almeida PF, dos Santos AM. Primary Health Care: Care coordinator in regionalized networks? Rev Saude Publica. 2016;50:80.
Uchôa SA da C, Arcêncio RA, Fronteira I, Coêlho AA, Martiniano CS, Brandão ICA, et al. Potential access to primary health care: What does the national program for access and quality improvement data show? Rev Lat Am Enfermagem. 2016;24:e672.
Rodrigues LBB, dos Santos CB, Goyatá SLT, Popolin MP, Yamamura M, Deon KC, et al. Assessment of the coordination of integrated health service delivery networks by the primary health care: COPAS questionnaire validation in the Brazilian context. BMC Fam Pract. 2015;16:87.
Seyedamini B, Riahi L, Farahani M, Tabibi S, Asl A. The effect of clinical factor on the health system integration. Int Arch Health Sci. 2019;6:6(1):1-11.
Athié K, Menezes AL do A, da Silva AM, Campos M, Delgado PG, Fortes S, et al. Perceptions of health managers and professionals about mental health and primary care integration in Rio de Janeiro: a mixed methods study. BMC Health Serv Res. 2016;16(1):532.
D’Avila OP, Harzheim E, Hauser L, Pinto LF, de Castilhos ED, Hugo FN. Validation of the Brazilian version of Primary Care Assessment Tool (PCAT) for Oral Health - PCATool Brazil Oral Health for Professionals. Ciencia e Saude Coletiva. 2021;26(6):2097–108.
Qiu C, Chen S, Yao Y, Zhao Y, Xin Y, Zang X. Adaption and validation of Nijmegen continuity questionnaire to recognize the influencing factors of continuity of care for hypertensive patients in China. BMC Health Serv Res. 2019;19:79.
Xia J, Rutherford S, Ma Y, Wu L, Gao S, Chen T, et al. Obstacles to the coordination of delivering integrated prenatal HIV, syphilis and hepatitis B testing services in Guangdong: using a needs assessment approach Health systems and services in low and middle income settings. BMC Health Serv Res. 2015;15:117.
Ollé-Espluga L, Vargas I, Mogollón-Pérez A, Soares-de-Jesus RPF, Eguiguren P, Cisneros A-I, et al. Care continuity across levels of care perceived by patients with chronic conditions in six Latin-American countries. Gac Sanit. 2021;35(5):411–9.
Bousquat A, Giovanella L, Campos EMS, de Almeida PF, Martins CL, Mota PHDS, et al. Primary health care and the coordination of care in health regions: Managers’ and users’ perspective. Ciencia e Saude Coletiva. 2017;22(4):1141–54.
Miguel-Esponda G, Bohm-Levine N, Rodríguez-Cuevas FG, Cohen A, Kakuma R. Implementation process and outcomes of a mental health program integrated in primary care clinics in rural Mexico: a mixed-methods study. Int J Ment Health Syst. 2020;14:21.
Fujita M, Poudel KC, Green K, Wi T, Abeyewickreme I, Ghidinelli M, et al. HIV service delivery models towards “Zero AIDS-related Deaths”: a collaborative case study of 6 Asia and Pacific countries. BMC Health Serv Res. 2015;15:176.
Castro SM, Cubillos L, Uribe-Restrepo JM, Suárez-Obando F, Meier A, Naslund JA, et al. Assessing the integration of behavioral health services in primary care in Colombia. Adm Policy Ment Health Ment Health Serv Res. 2020;47(3):435–42.
van Rensburg AJ, Petersen I, Wouters E, Engelbrecht M, Kigozi G, Fourie P, et al. State and non-state mental health service collaboration in a South African district: a mixed methods study. Health Policy Plan. 2018;33(4):516–27.
Aleluia IRS, Medina MG, de Almeida PF, Vilasbôas ALQ. Care coordination in primary health care: an evaluative study in a municipality in the Northeast of Brazil. Ciencia e Saude Coletiva. 2017;22(6):1845–56.
Lewis RQ, Rosen R, Goodwin N, Dixon J. Where next for integrated care organisations in the English NHS? London: the Nuffield Trust; 2010.
Acknowledgements
We would like to acknowledge Chris Waterworth, Manjula Marella, and Fleur Smith from the University of Melbourne School of Population and Global Health for their constructive comments on this paper, and Welch Library Informationist Donna Hesson for her assistance in developing the search strategy.
Funding
This publication is made possible by the support of the American people through the United States Agency for International Development (USAID). The contents are the sole responsibility of ReLAB-HS and do not necessarily reflect the views of USAID or the United States Government. The funder played no role in the development of this manuscript.
Author information
Authors and Affiliations
Contributions
RN, NZ, and AB designed the study. RN and NZ designed the search strategy and executed the search. RN, LA, and ZK reviewed the articles, and extracted the data. RN, NZ, LA, ZK, WP, and AB participated in drafting and critical revision of the manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist.
Additional file 2.
List of databases and results of search. PubMed Search Strategy.
Additional file 3.
Data Extraction Sheet for Integration measurement and its applications in LMIC country health systems: a scoping review.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Neill, R., Zia, N., Ashraf, L. et al. Integration measurement and its applications in low- and middle-income country health systems: a scoping review. BMC Public Health 23, 1876 (2023). https://doi.org/10.1186/s12889-023-16724-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-16724-2