Abstract
This review follows an established methodology for integrating human rights to address knowledge gaps related to the health and non-health outcomes of mandatory waiting periods (MWPs) for access to abortion. MWP is a requirement imposed by law, policy, or practice, to wait a specified amount of time between requesting and receiving abortion care. Recognizing that MWPs “demean[] women as competent decision-makers”, the World Health Organization recommends against MWPs. International human rights bodies have similarly encouraged states to repeal and not to introduce MWPs, which they recognize as operating as barriers to accessing sexual and reproductive healthcare. This review of 34 studies published between 2010 and 2021, together with international human rights law, establishes the health and non-health harms of MWPs for people seeking abortion, including delayed abortion, opportunity costs, and disproportionate impact. Impacts on abortion providers include increased workloads and system costs.
Similar content being viewed by others
Background
A mandatory waiting period (MWP) is a requirement imposed by law, policy, or practice, to wait a specified amount of time between requesting and receiving abortion care [1]. This is additional to the delays or waits that are generally built into the provision of non-emergency health care, including abortion, within health systems. While MWPs are not common, they are mandated by law and policy in several national and sub-national jurisdictions [2]. These MWPs vary widely across different settings [3]. In some cases, they can be satisfied in one visit, with the ‘clock’ beginning to run when telephone or other remote contact is made with a provider. In other settings mandatory waiting periods operate as ‘two visit’ requirements, with an in-person visit being required before the time begins to run. Some jurisdictions vary the application of MWP by gestational age. Sometimes referred to as ‘waiting periods’, ‘reflection periods’ or ‘cooling-off periods’ the World Health Organization (WHO) has recognized that MWPs “demean[] women as competent decision-makers” ([4], pg. 96). Reflecting this, the WHO recommends against MWPs [1]. International human rights bodies have similarly encouraged states to repeal and not to introduce MWPs, which they recognize as operating as barriers to accessing sexual and reproductive healthcare [5].
The aim of this review is to address knowledge gaps related to the health and non-health outcomes of MWPs. The review followed a methodology for integrating human rights in guideline development that has been described elsewhere [6]. This methodological approach is well-suited to interventions that are complex and can have multiple components interacting synergistically or dissynergistically, may be non-linear in their effects, and are often context dependent [7]. Such complex interventions often interact with one another so that outcomes related to one individual or community may be dependent on others, and may be impacted positively or negatively by the people, institutions and resources and how they are arranged within the larger system in which they are implemented [7]. As such, this review is not a classic systematic review per se but rather aims to synthesize evidence from existing studies (i.e. data extracted from included studies) and international human rights law (i.e. standards articulated in and by international human rights law sources and bodies) according to a methodology designed for this purpose [6]. This review was conducted as part of the evidence base for the WHO’s Abortion Care Guideline (2022) [1]. It is one of seven such reviews undertaken by the same research team and pursuing a common methodology.
Throughout this review we use the terms women, pregnant women, women and girls, and pregnant people interchangeably to refer to all those who are or can become pregnant, regardless of their gender identity.
Methods
Identification of studies and data extraction
This review examined the impact of the intervention of MWPs on two populations: (i) people seeking abortion, and (ii) healthcare providers. Legal, policy, and human rights experts co-developed the study outcomes and search strategy. Our outcomes of interest included both health and non-health outcomes that, based on a preliminary assessment of the literature [8], could be linked to the effects of MWPs. Our a priori outcomes included delayed abortion, opportunity costs, self-managed abortion, workload implications, system costs, perceived imposition on personal ethics or conscience, perceived impact on relationship with patient, referral to another provider, unlawful abortion, continuation of pregnancy, and stigmatization.
Our search strategy contained a combination of MeSH and key words. We searched the databases PubMed, HeinOnline, JStor, and the search engine Google Scholar. As the second edition of the WHO’s Safe Abortion Guidance included data up until 2010, we limited our search to papers published in English after 31 December 2010 and up to 2 December 2019. An updated search of the same databases was undertaken in July 2021. We did not restrict our search by study design. We included (comparative and non-comparative) quantitative studies, qualitative and mixed-methods studies, reports, PhD theses, and economic or legal analyses that undertook original data collection or analysis, but excluded masters theses and abstracts.
The full review team was made up of 6 members (MF, AF, FdL, AC, MR and AL). AL and FdL developed the PICO. Two reviewers (MF and AF) conducted an initial screening of the literature. Titles and abstracts were first screened for eligibility using the Covidence® tool; full texts were then reviewed. A third reviewer (FdL) confirmed that these manuscripts met inclusion criteria. Two reviewers (FdL and AC) extracted data. Any discrepancies were reviewed and discussed with two additional reviewers (AL and MR). The review team resolved discrepancies through consensus.
In accordance with our previously-published methodology for the effective integration of human rights as evidence in systematic reviews for guideline development [6], we identified and analyzed international human rights law as it related to reproductive rights in order to identify relevant human rights standards. Once data had been extracted from the included studies, we integrated them with the identified human rights standards. This allowed us to develop a full understanding of the implications of MWPs abortion law and policy including (a) which human rights standards are engaged by MWPs, (b) whether the studies suggest that MWPs have positive or negative effects on the enjoyment of rights, and (c) where no data is identified from the manuscripts against outcomes of interest, whether human rights law provides evidence that can further elucidate the impacts and effects of MWPs. This is summarized in Tables 2 and 3 below.
Analysis
We organized data from the included studies by reference to our study outcomes and presented this in evidence tables. These tables presented the association of each study on the outcome together with an overall conclusion from the data relevant to the outcome of interest. We then applied human rights standards to these outcomes to develop an understanding of the effects of criminalization that combines the evidence from human rights law (i.e. the applicable standards) and the included studies. In other words, we assessed whether the evidence from the included studies indicated that MWPs had effects that were incompatible with established requirements of international human rights law [6]. To summarize the effect of the intervention, across all study designs, we used and applied a visual representation of effect direction. The direction of the evidence was illustrated by a symbol which indicated whether, in relation to that particular outcome, the evidence extracted from a study suggested an increase (▲), decrease (⊽), or no change in the outcome (○). The symbol did not indicate the magnitude of the effect [6].
Results
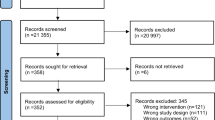
The search generated 10,063 citations after duplicates were removed. We screened the titles and abstracts and conducted a full text screening of 391 manuscripts. We excluded those manuscripts that did not have a clear connection with the intervention and our pre-defined outcomes, resulting in 34 manuscripts being included in the final analysis (Fig. 1. Prisma flow diagram).
Prisma Flow diagram. *Consider, if feasible to do so, reporting the number of records identified from each database or register searched (rather than the total number across all databases/registers). **If automation tools were used, indicate how many records were excluded by a human and how many were excluded by automation tools
All manuscripts described data from the United States of America [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42]. The characteristics of included manuscripts are presented in Table 1. The included studies contained information relevant for the outcomes: delayed abortion [14, 15, 19, 30, 31, 40,41,42], continuation of pregnancy [9, 10, 22,23,24,25, 27, 29, 35, 37, 41, 42], opportunity costs [14, 15, 9, 11,12,13, 16,17,18, 20, 21, 25, 26, 28, 32,33,34,35, 40, 41], disproportionate impact [9, 21, 37, 40,41,42], workload implications [30], and system costs [9, 26, 22, 36, 35, 37, 38, 41, 39]. No evidence was identified linking the intervention to the outcomes unlawful abortion, self-managed abortion, disqualification from lawful abortion, referral to another provider, stigmatization of providers, and impact on the provider-patient relationship.
Impact of the intervention on abortion seekers
A summary of the impacts of the intervention on abortion seekers and the application to human rights are presented in Table 2. Evidence identified per study and outcome are presented in Supplementary Table 1.
Evidence from six studies suggests that MWPs contribute to abortion delays [15, 19, 40, 31, 41, 42], including in waiting times for appointments [15, 19] and for women who need to travel to access abortion [40], with delays being greater where MWPs are longer (72 hours compared to 24 hours [31], for example) or where they require two visits [41, 42]. These delays are in excess of the MWP itself. In some cases MWPs cause delays that limit available abortion management options [14]. The delays associated with MWPs can be increased where the MWP is combined with mandated scripted counselling, provision of which requires the reorganization of physician time [30]. The right to the maximum attainable standard of physical and mental health (‘right to health’) requires that reproductive care be available, accessible and of good quality [43]. Such delays, which are attributable to a law and policy intervention and not, for example, to resource scarcity, raise questions of compatibility of MWPs with the right to health. This is exacerbated by the expectation in human rights law that abortion regulation would be evidence-based and proportionate [44], and the requirement not to regulate abortion in a way that violates women’s and girls’ right to life, jeopardizes their lives, subjects them to physical or mental pain or suffering, discriminates against them, or arbitrarily interferes with their privacy [45]. Given this, MWPs are prima facie disproportionate as a matter of human rights law.
Evidence on the effect of MWPs on continuation of pregnancy is mixed. Seven studies suggest that MWPs do not contribute to any change to abortion rates [22], unintended pregnancy rates [24, 27] or birth rates [29] in general, one of which suggests MWPs are associated with decreased non-marital birth rates [22]. However, evidence from six studies suggests that MWPs may contribute to continuation of pregnancy through increased birth rates [42], decreased abortion rates [25], or failure to return for the second visit [35]. Where MWPs are associated with continuation of pregnancy studies showed differential impacts depending on age [9, 37], race or ethnicity [25, 37], resources [41], and distance travelled [41] to access abortion. In studies where no effect on birth rates was detected, the MWPs did not require an in-person visit [10], or was part of a multi-part TRAP law which imposed multiple restrictions [23]. The evidence from five studies suggests that MWPs impose disproportionate burdens across sub-populations of people seeking abortion. Evidence from three studies suggests that Black and Hispanic women, especially minors [37] and younger women [42], are particularly impacted by MWPs [9, 37, 42], while other studies suggest that there are disproportionate burdens for women who have fewer resources [21, 41, 42] and have to travel to access abortion care [21, 40,41,42].
While the evidence of the effect of MWPs on continuation of pregnancy is mixed, it is clear that where such effects exist they impact disproportionately on identifiable sub-populations. This aligns with the broader evidence from this review on the disproportionate impact of MWPs. This is inconsistent with the right to equality and non-discrimination, as well as the right to health. The United Nations Working Group on the issue of discrimination against women in law and in practice has noted that “[b] arriers to accessing lawful abortion that are not based on medical needs … are discriminatory” [46]. MWPs fall into this classification.
Evidence from twenty studies suggests that MWPs contribute to opportunity costs [14, 15, 9, 11,12,13, 16,17,18, 20, 21, 25, 26, 28, 32,33,34,35, 40, 41] for people who seek abortion. Studies found that abortion seekers and providers perceive MWPs as restricting care [14, 11] or making abortion seem unattainable [21], contributing to emotional [14, 12, 32, 34] and logistical burdens [14] including abortion travel [17], additional visits [15], delays [15, 40, 20, 33], increased travel time [15, 13], distance [16, 18] and costs [15, 13, 28, 32, 34, 35, 40], and unwanted disclosure of pregnancy [35]. Evidence from two studies suggest that MWPs are not associated with incidence of postpartum depression [26] and for most women, MWPs do not impact women’s certainty in the abortion decision [33]. Such opportunity costs reduce in practice the availability of abortion and thus have negative implications for the right to health.
Impact of the intervention on healthcare providers
A summary of the impacts of the intervention on healthcare providers and the application to human rights are presented in Table 3. Evidence identified per study and outcome are presented in Supplementary Table 2.
Evidence from one study [30] suggests that MWPs contribute to increased workload, even where the first ‘visit’ or trigger for the waiting period can be done remotely, which may lead to additional staffing costs and logistical challenges. Importantly, this study considered a MWP that was combined with a requirement for mandated scripted counselling provided by a prescribed health professional. Identified workload implications should be understood in this light.
Evidence from four studies suggests that MWPs contribute to system costs. One study found that MWPs were associated with increased odds of reporting an unwanted birth among minors [9], while other studies identified an association with an increase in child homicides [36], racial disparities in teen birth rates [37], and (combined with other regulatory policies) a decrease in the proportion of medication abortions [39]. Evidence from further studies suggest that MWPs are not associated with any change in the incidence of postpartum depression [26], or with preterm birth [38]. One study found that MWPs were associated with a decrease in nonmarital birth rates [22]. In system cost terms, the studies suggest that fewer women return for an abortion after a 72-hour MWP [35] leading to increased continued pregnancy rates with system cost impacts, and that two-visit MWP requirements are associated with adolescents and women with fewer resources returning for the abortion.
Discussion
As with most non-emergency health care provision, delays are built into the provision of abortion meaning that the imposition of additional MWPs is both harmful and unnecessary [47]. Policy-makers and legislators who support MWPs sometimes argue that they are designed to ensure and support certainty for women who seek abortion, and to minimize post-abortion regret. However, as a general matter, women who decide to end their pregnancies reach that decision quickly [48] and experience a high level of decisional certainty [49]. There is no significant increase in decisional certainty where an MWP is imposed [50], and more recent research reinforces the finding that MWPs delay abortion and impose opportunity costs on women [51], which in turn have disproportionate impacts on poor women and those who live further away from clinics [52]. Post-abortion regret is very rare. Instead, in the United States (where all the reviewed studies were set) post-abortion relief is the most commonly felt emotion among women five years after abortion [53], while emotional difficulty relating to abortion is rooted in social disapproval, romantic relationship loss, and ‘head versus heart’ conflict [54]. MWPs do not address and cannot aid in resolving these experiences. Indeed, they may exacerbate them by reinforcing perceptions of social disapproval. Where women are unsure or seek to revisit their decision, providers are well-equipped to support this through the provision of additional time [55]; legal or policy mandates requiring such a ‘reflection period’ are not necessary to ensure that women can reach a decision in the time that is right for them.
Human rights bodies have made it clear that states should repeal laws and policies that impede access to sexual and reproductive health care, including MWPs. They have noted the effects of MWPs on rural women [5] and identified MWPs as interventions that create barriers to access to sexual and reproductive health care [56]. The evidence from this review bears out that characterization of MWPs, which impose barriers to accessing care without clinical function or benefit. MWPs are also not justifiable as modes of managing resource scarcity. Indeed, their implications for health professionals’ workloads suggests they may have the opposite effect.
In addition, evidence identified in this review suggests that women who seek abortion broadly experience and perceive MWPs as burdensome, emotionally damaging, and negative in their effects. The UN Human Rights Committee has made clear that “[m] easures introduced to regulate abortion may not violate women’s and girls’ right to life, jeopardize their lives, subject them to physical or mental pain or suffering, discriminate against them, or arbitrarily interfere with their privacy” ([45], para. 8). This review suggests that MWPs fall foul of this requirement.
Limitations
This review has limitations. The most obvious limitation is that all the studies reviewed took place in the United States. While some studies were set in the United States generally [9, 11, 16, 18,19,20, 22,23,24,25,26,27,28,29, 36, 37, 42, 38], others were conducted across one or more states, those being Alabama [40, 41], Arizona [12, 21, 39], Kansas [12] Michigan [17], Missouri [34], New Mexico [17], North Carolina [30, 31], Oklahoma [12], Tennessee [13], Texas [10], and Utah [14, 15, 32, 33, 35]. While the dynamics of abortion law and policy that apply in the United States are particular, the effects of MWPs as a law and policy intervention are not limited to this particular setting. Indeed, at national level most MWPs are contained in European countries’ laws [3]. Thus, research on MWPs and their impact on access to abortion in more settings would be welcome. In addition, MWPs are highly variable and the nature and severity of their effects may differ depending on, for example, how they are triggered (by an in person visit, by telephone consultation, or by completion of prescribed formalities, for example) or gestational age [3]. Research taking these variables into account would further enrich the evidence base. Furthermore, in several included studies MWPs were introduced as part of, or operated in the context of, a multi-part and complex law and policy intervention, including so-called TRAP laws [57]. Thus, while these studies considered the impact of MWPs this was in their broader regulatory context and, in some cases, as part of a broader consideration of the effects of a TRAP law per se. Although the methodology adopted in this review acknowledges the interactions of multiple interventions and seeks to understand the studied intervention in its context [6, 7], studies that specifically consider the impacts of MWPs in settings with such omnibus packages of restrictive law and policy interventions would likely be illuminating.
As a general matter, the realization of human rights applicable to abortion-related interventions is not a research area that readily lends itself to randomized controlled trials or comparative observational studies; rather, studies are often conducted without comparisons. While this may be considered a limitation from a standard methodological perspective for systematic reviews, it does not limit the ability to identify human rights law implications of law and policy interventions. Thus, while standard tools for assessing risk of bias or quality, including GRADE [58], or the use of plausibility as an inclusion criteria, were unsuitable, given the objective of fully integrating human rights implications into our understanding of the effects of provider restrictions as a regulatory intervention, it was appropriate to engage with a wide variety of sources. Similarly, given the methodological approach adopted [6] we did not use plausibility as an inclusion criteria.
Conclusion
The evidence from the reviewed studies and international human rights law points clearly towards the inappropriateness of MWPs in abortion law and policy. As noted by the CESCR Committee, “[s]tates should repeal and refrain from introducing measures that create barriers to [sexual and reproductive health] goods and services” [56]. These include MWPs.
Availability of data and materials
All data generated or analyzed during this study are included in the published article and its supplementary information files.
References
The World Health Organization, “Abortion Care Guideline” (2022).
World Health Organization, Global abortion policies database (2018) https://abortion-policies.srhr.org/ accessed [29 Oct 2021].
Lavelanet A, Johnson BR, Ganatra B. Global abortion policies database: a descriptive analysis of the regulatory and policy environment related to abortion. Best Pract Res Clin Obstet Gynaecol. 2020;62:25–35.
World Health Organization, “Safe Abortion: Technical and Policy Guidance for Health Systems” 2nd (2012).
CEDAW, General recommendation No. 34 on the rights of rural women (2016) (UN Doc. CEDAW/C/GC/34).
de Londras F, Cleeve A, Rodriguez M, Lavelanet A. Integrating rights and evidence: a technical advance in abortion guideline development. BMJ Glob Health. 2021;6:e004141. https://doi.org/10.1136/bmjgh-2020-004141.
Petticrew M, Knai C, Thomas J, et al. Implications of a complexity perspective for systematic reviews and guideline development in health decision making. BMJ Glob Health. 2019;4:e000899. https://doi.org/10.1136/bmjgh-2018-000899.
Burris S, Ghorashi A, Foster Cloud L, Rebouché R, Skuster P, Lavelanet A. Identifying data for the empirical assessment of law (IDEAL): a realist approach to research gaps on the health effects of abortion law. BMJ Glob Health. 2021;6:e005120. https://doi.org/10.1136/bmjgh-2021-005120.
Coles M, Makinob K, Stanwood N, et al. How are restrictive abortion statutes associated with unintended teen birth? J Adolesc Health. 2010;47:160–7.
Colman S, Joyce T “Regulating abortion: Impact on patients and providers in Texas” (2010) NBER Working Paper No. 15825.
Cooney C, Hercher L, Bajaj K. Genetic counselors’ perception of the effect on practice of Laws restricting abortion. J Genet Counsel. 2017:1059–69.
Dennis A, Douglas-Durham E, Burns B. Experiences with health care and public assistance in states with highly restrictive abortion policies: state brief: Oklahoma. Ibis Reprod Health. 2014.
Ely G, Rouland Polmanteer RS, Caron A. Access to abortion Services in Tennessee: does distance traveled and geographic location influence return for a second appointment as required by the mandatory waiting period policy? Health Soc Work. 2019;44(1):13–21.
Ehrenreich K, Kaller S, Raifman S, Grossman D. Women's experiences using telemedicine to attend abortion information visits in Utah: a qualitative study. Womens Health Issues. 2019a.
Ehrenreich K, Marston C. Spatial dimensions of telemedicine and abortion access: a qualitative study of women’s experiences. Reprod Health. 2019b;16:94.
Fuentes L, Jerman J. Distance traveled to obtain clinical abortion Care in the United States and Reasons for clinic choice. J Women's Health. 2019.
Jerman J, Frohwirth L, Kavanaugh M, Blades N. Barriers to abortion care and their consequences for patients traveling for services: qualitative findings from two states. Perspect Sex Reprod Health. 2017;49(2):95–102.
Jones R, Jerman J. How far did US women travel for abortion services in 2008? J Women's Health. 2013;22(8):706–13.
Jones R, Jerman J. Time to appointment and delays in accessing care among U.S. abortion patients. Guttmacher Institute. 2016:1–22.
Jones R, Jerman J. Characteristics and circumstances of U.S. women who obtain very early and second trimester abortions. PLoS One. 2017;12(1):e0169969.
Karasek D, Roberts S, Weitz T. Abortion patients’ experience and perceptions of waiting periods: survey evidence before Arizona’s two-visit 24-hour mandatory waiting period law. Womens Health Issues. 2016;26(1):60–6.
Medoff M. Nonmarital births and state abortion policies. Soc Work Public Health. 2010a;25(5):454–69.
Medoff M. State abortion policies, targeted regulation of abortion provider Laws, and abortion demand. Rev Policy Res. 2010b;27(5):577–94.
Medoff M. Unintended pregnancy and abortion access in the United States. Int J Popul Access. 2012;Article ID:254315.
Medoff M. Race, restrictive state Abortion Laws and Abortion demand. Rev Black Polit Econ. 2014a;41:225–40.
Medoff M. The relationship between restrictive state abortion Laws and Postpartum depression. Soc Work Public Health. 2014b;29(5):481–90.
Medoff M. Unintended pregnancy and state abortion policy: rational choice or random behavior? J Policy Pract. 2014c;13:258–75.
Medoff M. The impact of state abortion policy on the Price of an abortion. Behav Soc Issues. 2015;24:56–67.
Medoff M. State abortion policy and unintended birth rates in the United States. Soc Indic Res. 2016;129:589–600.
Mercier R, Buchbinder M, Bryant A, Britton L. The experiences and adaptations of abortion providers practicing under a new TRAP law: a qualitative study. Contraception. 2015;91:507–12.
Morse J, Charm S, Bryant A, et al. The impact of a 72-hour waiting period on Women’s access to abortion Care at a Hospital-Based Clinic in North Carolina. 2018;79(4):NCMJ 205-209.
Roberts SCM, Turok DK, Belusa E, et al. Utah's 72-hour waiting period for abortion: experiences among a clinic-based sample of women. Perspect Sex Reprod Health. 2016;48(4):1–22.
Roberts SCM, Belusa E, Turok DK, et al. Do 72-hour waiting periods and two-visit requirements for abortion affect Women's certainty? A prospective cohort study. Womens Health Issues. 2017;27(4):1–25.
Ruhr LR, “Abortion decision-making and the impact of the 72-hour waiting period” (2016) University of Missouri-Columbia, Unpublished Thesis.
Sanders JN, Conway H, Jacobson J, et al. The longest wait: examining the impact of Utah’s 72-hour waiting period for abortion. Womens Health Issues. 2016;26(5):483–7.
Sen B, Wingate MS, Kirby R. The relationship between state abortion-restrictions and homicide deaths among children under 5 years of age: a longitudinal study. Soc Sci Med. 2012;75:156–64.
Tosh J “State Adolescent Reproductive Health Policies and their Impact on Teen Pregnancy Outcomes” (2015) University of Central Florida, Unpublished thesis.
Wallace ME, Evans MG, Theall K. The status of Women’s reproductive rights and adverse birth outcomes. Womens Health Issues. 2017;27(2):121–8.
Williams SG, Roberts S, Kerns J. Effects of legislation regulating abortion in Arizona. Womens Health Issues. 2018;28(4):297–300.
White K, deMartelly V, Grossman D, Turan JM. Experiences accessing abortion Care in Alabama among women traveling for services. Womens Health Issues. 2016;26(3):298–304.
White K, Turan JM, Grossman D. Travel for abortion Services in Alabama and Delays Obtaining Care. Womens Health Issues. 2017;27(5):523–9.
Myers C “Cooling off or Burdened? The Effects of Mandatory Waiting Periods on Abortions and Births” (2021) IZA DP No. 14434.
CESCR, General comment no. 14: The right to the highest attainable standard of health (Article 12 of the International Covenant on Economic, Social and Cultural Rights) (2000) (UN Doc. E/C.12/2000/4).
UN Special Rapporteur on the Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health, Interim Report to the General Assembly (2011) (UN Doc. A/66/254).
Human Rights Committee, General comment No. 36 on article 6 of the International Covenant on Civil and Political Rights, on the right to life (2018) (UN Doc. CCPR/C/GC/36).
Human Rights Council, Report of the United Nations Working Group on the Issue of Discrimination against Women in Law and in Practice (2016) (UN Doc. A/HRC/32/44).
Silva M, McNeill R, Ashton T. Ladies in waiting: the timeliness of first trimester services in New Zealand. Reprod Health. 2010;7(1 article 19):1–8.
Ashton JR. Patterns of discussion and decision-making amongst abortion patients. J Biosoc Sci. 1980;12(3):247–59. https://doi.org/10.1017/s0021932000012797.
Foster DG, Gould H, Taylor J, Weitz TA. Attitudes and decision making among women seeking abortions in one U.S. clinic. Perspect Sex Reprod Health. 2012;44(2):17–124. https://doi.org/10.1363/4411712.
Jovel I, Cartwright A, Ralph L, Upadhyay U. Abortion waiting periods and decision certainty among people searching online for abortion care. Obstet Gynecol. 2021;137(4):597–605. https://doi.org/10.1097/AOG.0000000000004313.
Lindo J, Pineda-Torres M. New evidence on the effects of mandatory waiting periods for abortion. J Health Econ. 2021;80:102533.
Sheldon W, Ely G, Rouland R. Does Tennessee's mandatory waiting period law systematically prevent residents of the Most economically disadvantaged zip codes from accessing abortion? An exploratory analysis. J Health Care Poor Underserved. 2021;32(2):1034–46.
Rocca C, Samari G, Foster D, et al. Emotions and decision rightness over five years following an abortion: an examination of decision difficulty and abortion stigma. Soc Sci Med. 2020;248:112704.
Kimport K. (Mis) Understanding Abortion Regret. Symb Interact. 2012;35(2):105–22.
Rowlands S, Thomas K. Mandatory waiting periods before abortion and sterilization: theory and practice. Int J Women's Health. 2020;12:577–86. https://doi.org/10.2147/IJWH.S257178.
CESCR, General comment no. 22 on the Right to sexual and reproductive health (article 12 of the International Covenant on Economic, Social and Cultural Rights) (2016) (UN Doc. E/C.12/GC/22).
Cohen DS, Joffe C. Obstacle course: the everyday struggle to get an abortion in America. Oakland: University of California Press; 2020.
Alonso-Coello P, Schünemann HJ, Moberg J, et al. GRADE evidence to decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1. Introduction. BMJ. 2016;353:i2016.
Acknowledgments
This work was supported by the UNDP-UNFPA-UNICEF-WHO-World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), a cosponsored programme executed by the World Health Organization (WHO). Professor de Londras also acknowledges the support of the Leverhulme Trust through the Philip Leverhulme Prize.
Funding
This work was supported by the a cosponsored program executed by the World Health Organization (WHO). Professor de Londras also acknowledges the support of the Leverhulme Trust through the Philip Leverhulme Prize. The funders did not design the study, collect, analyze or interpret data, or write the manuscript.
Author information
Authors and Affiliations
Contributions
AL managed the study. AL and FdL designed the review. AF and MF identified and extracted studies. AC and MR analyzed the data. AC undertook visualization. FdL prepared the draft manuscript. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors confirm there are no applicable competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Evidence table: Impact on the intervention on abortion seekers. Supplementary Table 2. Evidence Table: The impact of the intervention on health professionals.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
de Londras, F., Cleeve, A., Rodriguez, M.I. et al. The impact of mandatory waiting periods on abortion-related outcomes: a synthesis of legal and health evidence. BMC Public Health 22, 1232 (2022). https://doi.org/10.1186/s12889-022-13620-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13620-z