Abstract
Objectives
To investigate the impact of the COVID-19 pandemic along the U.S.-Mexico border region and evaluate the relationship of COVID-19 related mortality, socioeconomic status, and vaccination.
Methods
We used indirect standardization to age-adjust mortality rates and calculate standardized mortality ratios [SMR] in both countries. To examine the impact of socioeconomic factors, we calculated the Human Development Index (HDI) by county/municipality. We performed linear regression to understand the relationship between mortality, vaccination, and HDI. We used choropleth maps to visualize the trends seen in the region.
Results
Between January 22nd, 2020 and December 1st, 2021, surges of cases and deaths were similar in dyad cities along the U.S.-Mexico border visualizing the interconnectedness of the region. Mortality was higher in U.S. counties along the border compared to the national average (SMR 1.17, 95% CI 1.15–1.19). In Mexico, border counties had a slightly lower mortality to the national average (SMR 0.94, 95% CI 0.93–0.95). In U.S. border states, SMR was shown to negatively correlate with human development index (HDI), a socioeconomic proxy, resulting in a higher SMR in the border region compared to the rest of the counties. Conversely in Mexican border states, there was no association between SMR and HDI. Related to vaccination, U.S. counties along the border were vaccinated at a greater percentage than non-border counties and vaccination was negatively correlated with HDI. In Mexico, states along the border had a higher ratio of vaccinations per person than non-border states.
Conclusions
The U.S.-Mexico border is a divide of incredible importance not only to immigration but as a region with unique social, economic, environmental, and epidemiological factors that impact disease transmission. We investigated how the COVID-19 pandemic followed trends of previously studied diseases in the corridor such as tuberculosis, HIV, and influenza H1N1. These data state how targeted intervention along the U.S.-Mexico border region is a necessity when confronting COVID-19 and have implications for future control of infectious diseases in the region.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
The U.S.-Mexico border is a divide of incredible importance. Each day, $1.7 billion dollars of goods and services traverses the two countries in addition to hundreds of thousands of people, cars, trucks, and rail containers [1]. Much of the attention the geographic corridor receives revolves around immigration, both legal and illegal. However, the U.S.-Mexico border is a complex region with unique social, economic, and environmental qualities. Residents in this area are often at a disadvantage in terms of education, socioeconomic status, income inequality, and healthcare access that leads to poorer health outcomes [2]. SARS-CoV-2 is an RNA virus in the Coronaviridae family that leads to Coronavirus Disease 2019 (COVID-19) and caused a global pandemic since early 2021 [3]. COVID-19 is transmitted primarily through respiratory droplets and aerosols [4]. The disease’s clinical manifestations can range from an asymptomatic carrier state, a non-specific febrile illness, mild respiratory disease, or acute hypoxic respiratory failure that may lead to death [5]. Little has been reported on the epidemiology of COVID-19 along the U.S.-Mexico border.
The unique factors at the U.S.-Mexico border established the region as an important point of infectious disease dynamics before the COVID-19 pandemic began surfacing throughout the world. For example, assessments of tuberculosis genotype clusters from 2005 to 2010 revealed border areas as regions of high prevalence with spread between U.S.-born and Mexico-born persons [6]. Characteristics of the U.S.-Mexico border have shaped residents’ vulnerability to HIV as well. Regions bordering the U.S. such as Baja California have consistently had a higher HIV/AIDS incidence than the national average [7]. The example most prominent in recent memory, though, is the 2009 H1N1 pandemic. The influenza season of 2009–2010 yielded another iteration of the notorious H1N1 influenza strain likely originating in swine from Mexico. Patients 1 and 2 of the outbreak were both from border counties (San Diego and Imperial respectively) [8]. Though there do not seem to be any population studies examining H1N1 cases throughout the border, there have been retrospective pieces on how the border highlighted existing inequalities [9].
Socioeconomic determinants of health have contributed significantly to many public health emergencies throughout history and are being revisited during the COVID-19 pandemic [10]. There is ongoing research and evidence that the COVID-19 pandemic displays previously known trends of disproportionately impacting marginalized economic and racial groups [11,12,13,14]. Similar trends may be occurring during the COVID-19 pandemic, yet, little to no information has been published to highlight the regional epidemic along the U.S.-Mexico border [15]. To investigate this hypothesis, we compared COVID-19 case rates, mortality data, and vaccination data from U.S.-Mexico border and non-border regions, and tested the relationship of COVID-19 mortality with a socioeconomic indicator, the Human Development Index. We then contrasted disparities in these epidemiologic markers, discussed the interrelationship of the COVID-19 epidemic on both sides of the border, and explored potential reasons of differing outcomes along the border.
Methods
Data sources
This was an ecological analysis at the county/municipal level for the U.S.-Mexico border region. We extracted data from the COVID-19 Data Repository at Johns Hopkins University [16], U.S. National Center for Health Statistics [17], and the Mexican Ministry of Health’s Department of Epidemiology (Dirección General de Epidemiología) [18] for COVID-19 case and death counts. The data we extracted ranged from the beginning of the pandemic to December 1st, 2021. The data included county level U.S. data with confirmed, active, and recovered cases, deaths, the incident rate, and the case fatality ratio (recorded deaths/cases). The Mexican Ministry of Health dataset includes health unit, institution, care location, sex, birth date, residence, municipality, and many others. We extracted sociodemographic indicators from the American Community Survey 2019 (ACS) [19] and the Mexican National Institute of Statistics and Geography (Instituto Nacional de Estadísticia y Geografía) 2020 (INEGI) [20]. We obtained U.S. vaccination data by county from the Centers for Disease Control Data Repository [21], which was updated daily. These data included vaccination numbers and percentages for single and complete vaccination series, and stratification by age groups. The Mexican vaccination data was obtained via scrapping the Mexican Health Secretary’s (Secretaría de Salud) website [22]. All data was downloaded as aggregates at the county/municipal level and was determined to be non-human subjects research by the UCLA Institutional Review Board (IRB).
Measures
To examine the impact of socioeconomic factors, we calculated the Human Development Index (HDI) by county/municipality. The HDI was created by the United Nations Development Program (UNDP) [23]. HDI is a measure which assesses health, knowledge, and standard of living and compiles them into a singular score. The output of standardized scores then can allow researchers to compare various policies, programs, and events and their relation to socioeconomic factors. ACS provided information on lifespan, high school achievement, and average income. INEGI provided information on lifespan, years of schooling, and average income. We calculated HDI by first creating dimension indices which scale various factors between 0 and 1. The bounds as defined by UNDP are 20–85 years for life expectancy, 0–18 years for expected schooling or 0–15 years for mean schooling, and 100 to 75,000 for GNI per capita. Based on the available data for education systems, we calculated the U.S. and Mexican HDI differently [24]. The U.S. educational index was calculated by weighting for high school achievement. The Mexican educational index was calculated by weighting for average number of school years attained. Given these bounds, the data from ACS and INEGI was scaled between 0 and 1. After scaling, the geometric mean of the 3 outputs was calculated resulting in the final HDI metric.
COVID-19 cases and deaths were based on definitions from the originating data sources. In the U.S., the COVID-19 Data Repository at Johns Hopkins University aggregated data from local health jurisdictions at state and county levels. Local health jurisdictions report cases based on U.S. Centers for Disease Controls and Prevention (CDC) guidelines [25]. As such, positive COVID-19 cases are defined as either a laboratory-confirmed case or a probable case when a case either (1) meets clinical criteria and epidemiologic evidence with no confirmatory lab testing performed for COVID-19, (2) meets presumptive lab evidence and either clinical criteria or epidemiologic evidence, or (3) meets vital records criteria with no confirmatory lab testing performed for COVID-19. In Mexico, positive COVID-19 cases were defined as cases that either had a positive confirmatory test, or were classified as positive by epidemiologic association or by a ruling committee (only for deaths) [26].
To compare COVID-19 mortality rates, we standardized rates to adjust for differences in differing age demographics in a population. We created age-adjusted standardized mortality ratios by indirect standardization. Indirect standardization only requires that we know the age-specific mortality rates for the overall population, total number of deaths (or cases) of the study population, and the age structure of the study population [27]. As the JHU data only provides this level of detail (number of cases/number of deaths), indirect standardization was the only feasible method. Age-specific COVID-19 mortality rates were not available to calculate direct standardized rates. Given this information, we performed indirect standardization by multiplying the population size by the age-specific death rate resulting in the expected number of deaths. We then divided the observed number of deaths by the previously calculated product resulting in the standardized mortality ratio (SMR) [28].
Analysis
We used the R [29] packages epitools [30] and ggplot2 [31] in order to conduct the analysis and visualization for this project. We plotted time series heatmaps of rates by dyads of bordering county/municipality. We divided the data into phases based on seasons and peaks in COVID-19 cases. These sets included the early pandemic (before 6/1/2020), summer ‘20 (6/1/2020–9/1/2020), fall ‘20 (9/1/2020–12/1/2020), winter ‘20-‘21 (12/1/2020–2/1/2021), spring ‘21 (2/1/2021–6/1/2021), and summer and fall ’21 (6/1/2021–12/1/2021). We mapped calculated SMRs and vaccination rates using choropleth maps. We created descriptive statistics to compare the impact of COVID-19 in border and non-border regions of the U.S. and Mexico. These statistics were able to provide numerical context to the visual differences observed in our mapping. We performed linear regression to measure the association of COVID-19 SMR to HDI and vaccination to HDI of the region. We used a pre-defined alpha of < 0.05 for statistical significance.
Results
We compiled data from the 25 U.S. counties and 40 Mexican municipalities along the border and temporally and cumulatively analyzed the dataset to understand the dynamics of COVID-19 in the region. Between the start of data collection and December 1st, 2021 there were 1,473,977 cases and 47,906 deaths in the binational border region.
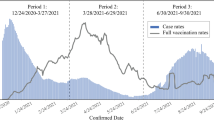
Using weekly death rates scaled to the per capita metric of 100,000 people, we created a heatmap visualizing surges of cases in border counties and municipalities. Neighboring cities experienced lagging peaks of COVID-19 deaths with the preceding peak usually occurring on the Mexican side of the border. This trend occurred both during waves in the spring and summer of 2020 and the fall and winter of 2020–2021 (Fig. 1).
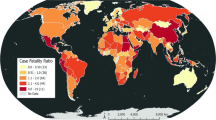
Using SMR, we created choropleth maps for the U.S. and Mexico by county or municipality. The resulting maps highlighted geographic disparities in the border region compared to non-border regions (Fig. 2). We then created maps by season to visualize the changing hotspots of COVID-19 throughout the pandemic (Fig. 3).
Scaled case rates were similar comparing border to non-border areas in the U.S. (14,857.3 vs. 14,183.6) and Mexico (2,794.5 vs. 3,670.5). However, age-adjusted death rates were greater in border regions both in the U.S. (288.55 vs. 251.37) and Mexico (282.67 vs. 235.17). Additionally, SMR were greater in border regions both in the U.S. (1.17 vs. 1.02) and Mexico (0.94 vs. 0.78) (Table 1). Separating the pandemic into seasons, we found that border regions had a greater SMR compared to non-border regions until approximately February 2021 when the trend reversed (Table 2).
Comparison of COVID-19 SMR by country and border proximity throughout the pandemic
Further investigating reasons for the SMR disparities, we plotted HDI against SMR in order to understand correlations between death and socioeconomic conditions. In US border states, there was a negative correlation between SMR and HDI resulting in a higher SMR in the border region compared to the rest of the counties (p < 0.001). Conversely in Mexican border states, there was a positive association between SMR and HDI (p < 0.01) (Fig. 4).
As the pandemic progressed, vaccination became an important component to combatting the pandemic. We created vaccination maps with choropleth techniques to visualize regions of lower or higher vaccination status (Fig. 5). The resulting maps revealed that U.S. border counties appeared to have higher rates of complete vaccination series compared to non-border counties in those states. Comparing the totals, we found that U.S. border county residents were vaccinated at a higher percentage (61.3% vs. 58.7%) than non-border counties. Comparing counties, those along the border had a higher mean vaccination rate (62.6% vs. 44.4%, p < 0.001) than non-border counties. Similar to the regression of HDI against SMR, we plotted the rates for border and non-border counties against HDI which revealed that there was a negative correlation between vaccination rates and HDI (p = 0.02) which was opposite to the trend seen nationwide (p < 0.001) (Fig. 6).
We also created maps with choropleth techniques to visualize vaccination states of Mexican states (Fig. 7). As data was not disaggregated at the municipality level we did not have the granularity of the U.S. data. Our analysis revealed that in total, border states in Mexico had a higher ratio of vaccinations per person (0.88 vs. 0.81) compared to non-border states. However, there was no significant difference between the mean ratios when comparing border and non-border states (0.88 vs. 0.84, p = 0.64).
Discussion
We analyzed standardized COVID mortality rates along the U.S. Mexico border. We found that along the U.S.-Mexico border region there were higher COVID-19 mortality rates than non-border areas. Despite differing policies on either side of the border, proximal cities experienced linked waves of COVID-19 in terms of peaks and troughs. To inform the disparity between border and non-border areas, we plotted standardized mortality ratio (SMR) against human development index (HDI), a socioeconomic proxy. In US border states, there was a negative correlation between SMR and HDI resulting in a higher SMR in the border region compared to the rest of the counties. However, in Mexican border states, there was no association between SMR and HDI. In the U.S. border states, there was a negative correlation between SMR and vaccination percentage opposite to national trends. Additionally, in both the U.S. and Mexico, border regions were more vaccinated than non-border regions. Our findings overall highlight the importance of targeted regional interventions that consider both sides of the border in unison, and counter the notion that nations can isolate themselves through strict border policies.
Waves of COVID-19 were seen in border cities usually beginning on the Mexican side and surging on the U.S. side shortly after. Reasons for this trend are unclear but may lie in the unidirectional policies that existed surrounding border travel. Starting in March 2020, the U.S. government enacted restrictions on inbound traffic limited to “essential travel”. Reasons deemed as “essential” were citizen or lawful resident return, medical, educational, work, emergency or public health, cross-border trade, government or diplomatic, or military [32]. Conversely, the Mexican government did not impose any inbound travel restrictions [33]. This resulted in U.S. citizens and permanent residents being able to cross the border freely, while Mexican citizens were not able to cross into the U.S. Furthermore, the rates at which state and municipality restrictions were implemented varied between the U.S. and Mexico [34]. In March, California was one of the first states in the U.S. to enact statewide stay-at-home orders, while physical distancing orders in bordering Tijuana and Mexicali were not in effect until weeks later [35]. As initial cases in Mexico were likely imported from the U.S., the heavy interaction between individuals on the Mexican side early in the epidemic lead to Tijuana and Mexicali being early epidemic centers for Mexico like what New York was in the U.S. [35, 36] Later in April, as case counts remained low in California and as restrictions began to lift, cases were likely imported from Mexicali to bordering Imperial County and southern San Diego leading to pressure on hospital centers in those areas. A similar phenomenon occurred on the eastern border leading to high mortality rates in Laredo and Brownsville (Fig. 3).
Reasons for disparities in COVID indicators at the border areas compared to non-border areas are likely sociostructural. The U.S. border region is predominantly populated by Latino individuals and much has been reported on the U.S. side of the increased risk of COVID-19 in Latino and Black communities [37]. Yet, the virus does not have special receptors to target based on race or ethnicity, and it has yet to be proven if there is a particular genetic susceptibility in these racial/ethnic groups that increases these populations’ risk. Hence, the increased risk of disease acquisition is most likely due to sociostructural factors that lead to situations of numerous and prolonged interactions with other individuals that allow for disease transmission. For example, high density housing leads to rapid spread of the virus [38]. Additionally, many individuals due to their documentation status did not qualify for certain economic benefits to mitigate the economic impact of the epidemic. This forced these vulnerable individuals to continue working and be at high-risk for SARS-CoV-2 acquisition. U.S. border counties are amongst the poorest in the country, this tied with high rates of undocumented individuals in these areas, lead to a large segment of the population who lack basic primary and preventative medical care [39]. For mortality outcomes, pre-existing conditions like diabetes or kidney disease play a significant role in Latino communities and has been consistently associated with a higher risk of mortality from COVID [40].
On the Mexican side additional challenges were present. Testing was severely limited to the point where Mexico was last in testing per capita out of all OECD nations early in the pandemic [41]. This was evident in our data, where mortality rates in Mexico were similar to those in the U.S.; but, case rates in Mexico were on an order of magnitude lower than those in the U.S. This points to a severe lack of testing on the Mexican side, and only limited to symptomatic and sicker individuals. Health infrastructure is severely lacking along the border [42]. Lacking access on the Mexican side of the border is possibly leading many individuals to cross the border to access hospital centers in the U.S. also likely inflating that sides case mortality rates [43]. However, border municipalities have a higher development index then the rest of Mexico. This is partly due to the high number of high-density maquiladoras (factories) that manufacture products, including health products for the U.S. market. These maquiladaroas were pressured by the U.S. to continue operating. In turn, these maquiladoras were early centers for COVID-19 clusters as workers cited not having adequate personal protective equipment and an inability to physically distance within their work environments [44]. Workers’ rights groups have striked as result of these conditions and now that vaccines are available, specific efforts are being made to vaccinate workers in maquiladoras [45].
The COVID-19 pandemic had important economic implications in Central America that lead to waves of asylum seekers migrating to the U.S.-Mexico border [15]. Prior to the pandemic, the US instituted a Remain at Home Policy where asylum seekers remained in a third country (in this case Mexico) while their application was being reviewed. This led to refugees remaining along the U.S.-Mexico border in dense migrant camps [15]. Migration across the border has been a point of contention in the political realm of the U.S. with concerns that cases were being imported. While individuals crossing the border were likely not responsible for COVID-19 surges throughout the U.S. [46], the conditions asylum seekers experience are cause for concern and led to difficulties in protecting these individuals from outbreaks in congregate settings [15, 47]. There have been efforts to vaccinate individuals migrating to the U.S. [48], but policies still restrict asylum seekers from entering despite recent opening of the U.S.-Mexico border to vaccinated individuals [49].
Wide sweeping vaccination which cuts across all populations in a society is an essential component to handling any infectious disease. Vaccination for COVID-19 in the first year of availability was variable geographically throughout the U.S. In our data we observed an inverse correlation between vaccination rates and HDI at the border which went against national trends. Possible explanations for these observations lie in states’ and counties’ efforts to target vulnerable socioeconomic groups for increased vaccination resources. Arizona created a subset 1 S which listed groups such as minorities, tribal communities, and uninsured individuals as priorities during all phases of vaccination [50]. California enacted a plan using a Healthy Places Index to divide zip codes throughout the state in four quartiles. Allocation was then conducted 70% by age and 30% by sector with a double allotment for the lowest quartile [50]. New Mexico included a caveat which, based on the CDC’s Social Vulnerability Index (SVI), reallocated up to 25% of supply to higher SVI areas or regions with > 10,000 cases per 100,000 [50]. Texas’ plan included identification of vulnerable groups such as minorities, those experiencing homelessness, and those with disabilities who could contribute to the vaccine allocation decision making process [50]. However, after initial vaccine rollout, local Texas jurisdictions argued that vaccination clinics were predominantly located in wealthier and whiter areas [51,52,53]. Dallas attempted to modify plans and target Black and Latino neighborhoods; however Texas health officials stated this practice was unacceptable and threatened to cut off all supply [52]. Houston and Austin also enacted policies which identified vulnerable areas based on socioeconomic status, zip code, and COVID-19 burden [54, 55]. With more supply than demand, Texas health officials voted to no longer allocate vaccinations starting on May 10, 2021, and instead created a system in which providers could order shipments [56]. As of writing, many of the racial gaps in vaccination have narrowed or closed [57]. Of note, it is to the authors’ knowledge that many Mexican nationals or residents crossed into the U.S. to get vaccinations early during the vaccination rollout [58]. Potential reasons included inability to access vaccines in Mexico or to access vaccines that were not available in Mexico (e.g., Pfizer or Moderna) at the time. The magnitude of this phenomena is unknown and may overestimate vaccination coverage, especially in the border regions.
On the Mexican side of the border, vaccination began with a rapid start but since slowed. The country was first in Latin America to begin vaccination and doses administered peaked in July. However, poor supply chain and mismanagement of planning seem to have plagued further coverage [59]. Based on our analysis we observed that states along the U.S. border had higher ratios of vaccine doses. This information correlates with the broad push to vaccinate border residents and reopen border traffic and commerce. The U.S. government offered a multitude of doses to support the northern region of Mexico [60]. Additionally, starting in November, vaccines were offered to migrants as a part of the Remain in Mexico program [61].
Limitations of our study lie in the data sourcing and how representative it is of COVID-19 morbidity and mortality. We hoped to avoid testing limitations by focusing specifically on mortality. However, due to healthcare access and public health policies individuals may not be counted or missed [62]. Additionally, the methods through which counties, municipalities, states, and countries count deaths due to COVID-19 vary and can be incredibly complex [63]. When investigating reasons for disparities in COVID-19 outcomes, our metrics for socioeconomic conditions were not perfect comparisons due to differing education systems in the U.S. and Mexico and many other variables likely play a role into COVID-19 related mortality. For example, forced migration is an important factor in healthcare disparities and outcomes that was not assessed. Lastly, Mexican vaccination data more granular than national statistics are severely limited which impacts our ability to investigate its contribution to COVID-19’s spread in the region.
Conclusions
Overall, border residents and migrants are frequently placed in a precarious situation of handling diseases in a disadvantaged setting for a variety of reasons. Interventions are needed to avoid further mortality due to COVID-19 or future pandemics. Healthcare infrastructure in the forms of treatment, testing, and vaccination is needed, especially on the Mexican side of the border. Further, siloing binational communities is not the answer to avoid excess mortality in the border region. The border has an important interplay that is beneficial to communities on both sides of the border, where curtailing these relationships may ultimately do more harm than good. We believe that coordination from public health officials and policy makers is key to avoid repeating the consequences that these areas have suffered early in the epidemic. These coordinated efforts should be spearheaded by a group of binational leaders who understand the border region, such as the U.S.-Mexico Border Health Commission, instead of distant leaders in state capitals. Only a coordinated effort between both sides of the border will have an impact. Disease activity on a border cities counterpart poses more risk than the overall disease burden of a state, and if concerted efforts are not taken in unison, the other city will always be a reservoir for continued disease transmission and continued case clusters, and ultimately deaths.
Availability of data and materials
All data and code to run the analysis are available at: https://github.com/davigood1/Border-Covid-gh.
Abbreviations
- SMR:
-
Standardized mortality ratio
- HDI:
-
Human Development Index
- IRB:
-
Institutional Review Board
- ACS:
-
American Community Survey
- INEGI:
-
Instituto Nacional de Estadísticia y Geografía
- UNDP:
-
United Nations Development Program
References
Swanson A. Avocado Shortages and Price Spikes: How Trump’s Border Closing Would Hit U.S. The New York Times. 2019;6.
Homedes N. Achieving Health Equity and Social Justice in the US-Mexico Border Region. In: Social Justice in the US-Mexico Border Region. Dordrecht: Springer Netherlands; 2012. p. 127–44.
Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nature Reviews Microbiology. 2021;6(3):141–54.
Tadj A, Sidi Mohammed Lahbib S. Our Overall Current Knowledge of Covid 19: An Overview. Microbes, Infect Chemother. 2021;1:e1262.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020;26(20):2052.
Baker BJ, Moonan PK. Characterizing tuberculosis genotype clusters along the United States-Mexico border. Int J Tuberc Lung Dis. 2014;18(3):289–91. Available from: https://pubmed.ncbi.nlm.nih.gov/24670563.
Strathdee SA, Magis-Rodriguez C, Mays VM, Jimenez R, Patterson TL. The emerging HIV epidemic on the Mexico-U.S. border: an international case study characterizing the role of epidemiology in surveillance and response. Ann Epidemiol. 2012;22(6):426–38. Available from: https://pubmed.ncbi.nlm.nih.gov/22626001.
Emergence of a Novel Swine-Origin Influenza A (H1N1) Virus in Humans. New England J Med. 2009;360(25):2605–15.
Sparke M, Anguelov D. H1N1, globalization and the epidemiology of inequality. Health Place. 2012;18(4):726–36.
Krishnan L, Ogunwole SM, Cooper LA. Historical Insights on Coronavirus Disease 2019 (COVID-19), the 1918 Influenza Pandemic, and Racial Disparities: Illuminating a Path Forward. Ann Internal Med. 2020;173(6):474–81.
Wu T. The socioeconomic and environmental drivers of the COVID-19 pandemic: A review. Ambio. 2021;50(4):822–33.
Antonio-Villa NE, Fernandez-Chirino L, Pisanty-Alatorre J, Mancilla-Galindo J, Kammar-García A, Vargas-Vázquez A, et al. Comprehensive Evaluation of the Impact of Sociodemographic Inequalities on Adverse Outcomes and Excess Mortality During the Coronavirus Disease 2019 (COVID-19) Pandemic in Mexico City. Clin Infect Dis. 2022;9(5):785–92.
Tan AX, Hinman JA, Abdel Magid HS, Nelson LM, Odden MC. Association Between Income Inequality and County-Level COVID-19 Cases and Deaths in the US. JAMA Network Open. 2021;4(5):e218799.
Magesh S, John D, Li WT, Li Y, Mattingly-app A, Jain S, et al. Disparities in COVID-19 Outcomes by Race, Ethnicity, and Socioeconomic Status. JAMA Network Open. 2021;4(11):e2134147.
Cuneo CN, Janeway H. From Icebox to Tinderbox — A View from the Southern Border. New England Journal of Medicine. 2020;383(13):e81.
Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–4.
National Center for Health Statistics. Provisional COVID-19 Deaths by Sex and Age. Hyattsville; 2022 [cited 2022 Feb 24]. Available from: https://data.cdc.gov/NCHS/Provisional-COVID-19-Deaths-by-Sex-and-Age/9bhg-hcku.
Gobierno de México. Covid-19 México: Casos diarios por Municipio. Aguascalientes City; 2022 [cited 2022 Feb 24]. Available from: https://datos.covid-19.conacyt.mx/#DownZCSV.
United States Census Bureau. 2019 American Community Survey. 2019.
Instituto Nacional de Estadísticia y Geografía. Censo de Población y Vivienda 2020. 2020.
National Center for Immunization and Respiratory Diseases. COVID-19 Vaccinations in the United States,County. 2022 [cited 2022 Feb 24]. Available from: https://data.cdc.gov/Vaccinations/COVID-19-Vaccinations-in-the-United-States-County/8xkx-amqh.
Zepeda R. Vacunados MX. Github; 2022 [cited 2022 Feb 24]. Available from: https://github.com/RodrigoZepeda/VacunadosMX.
United Nations Development Programme. Human Development Index (HDI). 2022 [cited 2022 Feb 24]. Available from: https://hdr.undp.org/en/content/human-development-index-hdi.
Anderson J, Gerber J. A human development index for the United States-Mexico border. J Borderlands Stud. 2004;19(2):1–26.
National Center for Immunization and Respiratory Diseases (NCIRD) D of VD. Information for Health Departments on Reporting Cases of COVID-19. Centers for Disease Control and Prevention. 2022.
Secretaría de Salud. Lineamiento Estandarizado para la Vigilancia Epidemiológica y por Laboratorio de la Enfermedad Respiratoria Viral. Ciudad de México; 2021.
Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M. Age standardization of rates: a new WHO standard. Geneva: World Health Organization. 2001;9(10):1–14.
Rodríguez G. Direct and Indirect Standardization. Pop 502 Research Methods in Demography: Princeton University. 2017 [cited 2022 Feb 24]. Available from: https://data.princeton.edu/eco572/Standardization.pdf.
R Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2020 [cited 2022 Feb 24]. Available from: https://www.R-project.org/.
Aragon TJ, Fay MP, Wollschlaeger D, Omidpanah A. epitools: Epidemiology Tools. Pullman; 2020.
Wickham H. ggplot2: Elegant Graphics for Data Analysis. New York: Springer-Verlag New York; 2016.
U.S. Embassy & Consulates in Mexico. Travel Restrictions – Fact Sheet. 2021 [cited 2022 Feb 24]. Available from: https://mx.usembassy.gov/travel-restrictions-fact-sheet/.
Valle AM, Knaul FM. Mexico, facing its third COVID-19 wave, shows the dangers of weak federal coordination. The Conversation. 2021 Aug 18 [cited 2022 Feb 24]; Available from: https://theconversation.com/mexico-facing-its-third-covid-19-wave-shows-the-dangers-of-weak-federal-coordination-164995.
Knaul F, Arreola-Ornelas H, Porteny T, Touchton M, Sánchez-Talanquer M, Méndez Ó, et al. Not far enough: Public health policies to combat COVID-19 in Mexico’s states. PLOS ONE. 2021;16(6):e0251722.
Tariq A, Banda JM, Skums P, Dahal S, Castillo-Garsow C, Espinoza B, et al. Transmission dynamics and forecasts of the COVID-19 pandemic in Mexico, March-December 2020. PLOS ONE. 2021;21(7):e0254826.
Gurbuz O, Aldrete RM, Vargas E. Cross-Border Transportation as a Disease Vector in COVID-19. El Paso; 2020.
Rodriguez-Diaz CE, Guilamo-Ramos V, Mena L, Hall E, Honermann B, Crowley JS, et al. Risk for COVID-19 infection and death among Latinos in the United States: examining heterogeneity in transmission dynamics. Ann Epidemiol. 2020;52:46-53.e2.
Vijayan T, Shin M, Adamson PC, Harris C, Seeman T, Norris KC, et al. Beyond the 405 and the 5: Geographic Variations and Factors Associated With Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Positivity Rates in Los Angeles County. Clin Infect Dis. 2021;2(9):e2970-5.
Bastida E, Brown HS, Pagán JA. Persistent Disparities in the Use of Health Care Along the US–Mexico Border: An Ecological Perspective. Am J Public Health. 2008;98(11):1987–95.
Parra-Bracamonte GM, Lopez-Villalobos N, Parra-Bracamonte FE. Clinical characteristics and risk factors for mortality of patients with COVID-19 in a large data set from Mexico. Ann Epidemiol. 2020;52:93-98.e2.
Suárez V, Suarez Quezada M, Oros Ruiz S, Ronquillo De Jesús E. Epidemiology of COVID-19 in Mexico: from the 27th of February to the 30th of April 2020. Revista clinica espanola. 2020;220(8):463–71.
Moya EM, Chavez-Baray SM, Monroy MS. Health Institutions at the U.S.-Mexico Border. In: Payan T, Cruz PL, editors. Binational Commons: Institutional Development and Governance on the US-Mexico Border. Tucson: University of Arizona Press; 2020. p. 191–217.
Shoichet CE. People with coronavirus are crossing the US-Mexico border for medical care. CNN health. 2020 Jun 29 [cited 2022 Feb 25]; Available from: https://www.cnn.com/2020/06/29/health/border-hospitals-coronavirus/index.html.
Wattenbarger M. US-Mexico border factories pressured to stay open despite Covid-19 risk. The Guardian. 2020 May 14 [cited 2022 Feb 25]; Available from: https://www.theguardian.com/world/2020/may/14/us-mexico-border-factories-coronavirus.
Galindo Y, McClain T, Gurmilan H, Orozco G. Cross Border Effort to Vaccinate 10,000 Maquiladora Workers. UC San Diego Health: Newsroom. 2021 [cited 2022 Feb 25]. Available from: https://health.ucsd.edu/news/releases/Pages/2021-05-25-cross-border-effort-to-vaccinate-ten-thousand-maquiladora-workers.aspx.
Rose J. Some Republicans Claimed Migrants Fueled A COVID-19 Surge. Doctors Say It’s Not True. National Public Radio. 2021 [cited 2022 Feb 25]. Available from: https://www.npr.org/2021/08/09/1026207555/some-republicans-claimed-migrants-fueled-a-covid-19-surge-doctors-say-its-not-tr.
Reynolds CW, Ramanathan V, Lorenzana E, Das PJ, Sagal KM, Lozada-Soto KM, et al. Challenges and Effects of the COVID-19 Pandemic on Asylum Seeker Health at the U.S.-Mexico Border. Health Equity. 2021;5(1):169–80.
Diaz L, Garrison C, Daniel FJ, McCool G. Hundreds of migrants vaccinated against coronavirus in U.S.-Mexico border city. Reuters. 2021 [cited 2022 Feb 25]. Available from: https://www.reuters.com/world/us/hundreds-migrants-vaccinated-against-coronavirus-us-mexico-border-city-2021-08-03/.
Cooke K, Rosenberg M, O’hara C. U.S. borders reopen, but not for asylum seekers stuck in Mexico. Reuters. 2021 [cited 2022 Feb 25]. Available from: https://www.reuters.com/world/americas/us-borders-reopen-not-asylum-seekers-stuck-mexico-2021-11-09/.
Schmidt H, Weintraub R, Williams MA, Miller K, Buttenheim A, Sadecki E, et al. Equitable allocation of COVID-19 vaccines in the United States. Nat Med. 2021;27(7):1298–307.
Lopez A. Austin Leaders Want Equity In Vaccination Rates. So Far That Hasn’t Happened. KUT 90.5 NPR. 2021 [cited 2022 Feb 25]. Available from: https://www.kut.org/covid-19/2021-05-12/austin-leaders-want-equity-in-vaccination-rates-so-far-that-hasnt-happened.
Platoff E, Garnham JP. Dallas County axes plan to prioritize vaccinating communities of color after state threatens to slash allocation. The Texas Tribune. 2021 [cited 2022 Feb 25]; Available from: https://www.texastribune.org/2021/01/20/dallas-vaccine-plan-communities-of-color/.
Morris A. Dallas County Judge Clay Jenkins spars with the state over North Texas COVID-19 vaccine allocations. The Dallas Morning News. 2021 Feb 26 [cited 2022 Feb 25]; Available from: https://www.dallasnews.com/news/politics/2021/02/26/dallas-county-judge-clay-jenkins-spars-with-the-state-over-north-texas-covid-19-vaccine-allocations/.
Harris County Public Health. Harris County: COVID-19 Vaccine Equity Strategy Summary. Houston; 2021 [cited 2022 Feb 25]. Available from: https://publichealth.harriscountytx.gov/Portals/27/Documents/Vaccine%20Equity%20Report_FINAL.pdf?ver=SRtTOxKs5jLL28AibVi_Og%3d%3d.
Austin Public Health. COVID-19 Equity Efforts. austintexas.gov. 2021 [cited 2022 Feb 25]. Available from: https://www.austintexas.gov/covidequity.
Press Officer D. Texas Shifts From COVID-19 Vaccine Allocation to Ordering. Texas Department of State Health Services. 2021 [cited 2022 Feb 25]. Available from: https://dshs.texas.gov/news/releases/2021/20210506.aspx.
Ndugga N, Hill L, Artiga S, Haldar S. Latest Data on COVID-19 Vaccinations by Race/Ethnicity. Kaiser Family Foundation. 2022.
Carrie Kahn. Some Mexicans Travel To U.S. For COVID Vaccines As Their Country’s Rollout Stumbles. NPR. 2021.
Navarro A, Quinn D. Mexico Sinks to Bottom of Pack After Fast Vaccination Start. Bloomberg. 2021 [cited 2022 Feb 25]; Available from: https://www.bloomberg.com/news/articles/2021-10-15/mexico-sinks-to-bottom-of-pack-after-fast-vaccination-start.
Secretaría de Relaciones Exteriores. Mexico presents vaccination strategy for the northern border to accelerate reopening. 2021 [cited 2022 Feb 25]. Available from: https://www.gob.mx/sre/prensa/mexico-presents-vaccination-strategy-for-the-northern-border-to-accelerate-reopening.
Harrison C, Horwitz L, Zissis C. Timeline: Tracking Latin America’s Road to Vaccination. Americas Society/Council of the Americas. 2022 [cited 2022 Feb 25]. Available from: https://www.as-coa.org/articles/timeline-tracking-latin-americas-road-vaccination.
Reuters Fact Check. Fact Check-False claims that nobody has been ‘discovered dead at home’ from COVID-19. Reuters. 2021 Sep 23 [cited 2022 Feb 25]; Available from: https://www.reuters.com/article/factcheck-dead-home/fact-check-false-claims-that-nobody-has-been-discovered-dead-at-home-from-covid-19-idUSL1N2QP20D.
Boyle P. How are COVID-19 deaths counted? It’s complicated. Association of American Medical Colleges. 2021.
Acknowledgements
We are appreciative of the numerous open data sources from Johns Hopkins University, the U.S. National Center for Health Statistics, the Mexican Ministry of Health’s Department of Epidemiology (Dirección General de Epidemiología), the American Community Survey, and the Mexican National Institute of Statistics and Geography (Instituto Nacional de Estadísticia y Geografía) 2020 (INEGI) that made this project possible.
Funding
This project was assisted by a grant from the David Geffen School of Medicine at UCLA through the Short Term Training Program.
Author information
Authors and Affiliations
Contributions
JNF analyzed and interpreted the data, produced the data visualizations, and wrote the manuscript. ABM, provided expert input on data visualization and manuscript editing. DGM was a major contributor to all steps of the project and in the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Filosa, J.N., Botello-Mares, A. & Goodman-Meza, D. COVID-19 needs no passport: the interrelationship of the COVID-19 pandemic along the U.S.-Mexico border. BMC Public Health 22, 1081 (2022). https://doi.org/10.1186/s12889-022-13513-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13513-1