Abstract
Background
There is limited evidence about lifetime burden of child malnutrition. This study aimed to estimate the lifetime impact of being underweight or overweight/obese during childhood in Vietnam.
Methods
We developed a life table model in combination with a Markov model for Vietnamese children aged 5–19 years and simulated until they reached 75 years of age or died using published data. The starting year was 2019 and the model estimated number of deaths, years of life lived and quality-adjusted life years (QALY) with an annual discount rate of 3%. We performed scenario, one-way, and probabilistic sensitivity analyses to assess the impact of uncertainties in input parameters.
Results
The model estimated 9.68 million deaths (6.44 million men and 3.24 million women), 622 million years of life lived (317 million men and 305 million women), and 601 million QALYs (308 million men and 293 million women). Scenario analyses showed that the reduction in either underweight or overweight/obesity alone, and reduction in both underweight and overweight/obesity resulted in fewer deaths, more years of life lived and more QALYs gained. In the scenario where everyone was a healthy weight, the model estimated 577,267 fewer deaths (6.0% less), 2 million more years of life lived (0.3% more), and 3 million QALYs gained (0.6% more) over base-case results which represents current situation in Vietnam.
Conclusions
Our results suggest that addressing underweight and overweight/obesity will contribute to reducing deaths and increasing years of life lived and QALYs. Policies and interventions in alignment with Sustainable Development Goals to address underweight and overweight/obesity are necessary to achieve health for all.
Similar content being viewed by others
Background
Optimal health and nutrition during childhood and adolescence underpin personal, national and international development. Malnutrition during childhood and adolescence increases the risk of morbidity and mortality, impairs cognitive development and reduces work productivity in later life [1,2,3]. In particular, improving nutrition among children and adolescents 5 to 19 years is crucial as it affects the timing and pattern of puberty, adult height, muscle, as well as risk of non-communicable diseases in later life. It is critical periods to ensure a healthy transition to adulthood [1, 4].
While undernutrition problems still remain as a major public health concern in low-and middle-income countries, overweight and obesity have increased globally [5]. The double burden of malnutrition, which is the coexistence of undernutrition and overweight/obesity, has increased in the poorest low-and middle-income countries [6]. In particular, overweight and obesity have increased, mainly due to rapid changes in the food system including the availability of cheap ultra-processed food and beverages, and major reductions in physical activity [6]. Actions to simultaneously prevent or reduce the risk of nutritional deficiencies and obesity have been proposed to address malnutrition in a more holistic way [7].
In Vietnam, rapid economic development and urbanization have also shifted the health and nutritional status of the population. The National Nutrition Strategy for Vietnam envisions reduced child malnutrition including both stunting and overweight/obesity [8], however, studies have shown that double burden of malnutrition in children still exists [9, 10]. The General Nutrition Survey in Vietnam discovered that the prevalence of stunting has decreased from 23.4% in 2010 to 14.8% in 2020 but the prevalence of overweight and obesity has increased from 8.5% to 19% over the same period among children aged 5–19 years [11]. However, there is limited evidence about the long-term impact of this changing picture of child and adolescent malnutrition, which is necessary for policy makers to understand the magnitude of burden, formulate policy and design intervention programs. When lifetime data are not available, modeling can be a useful way to quantify and structure the decision problem to maximize population health within available resources [12, 13]. A few modeling studies have estimated impacts of childhood overweight and obesity from Germany, the United States and Thailand, highlighting long-term burden regarding costs and quality-adjusted life years (QALY) [14,15,16,17]. However, the lifetime burden of undernutrition such as stunting, wasting or being underweight has not been included, and the long-term impact of child malnutrition in Vietnam is unknown. Therefore, this study aimed to estimate the lifetime burden of being underweight or overweight/obese during childhood in terms of deaths, years of life lived and QALY at the population level in Vietnam.
Methods
Model description
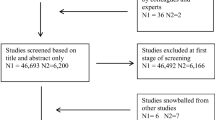
We developed a state-of-the-art life table model in combination with a Markov model with four health states, including underweight, healthy weight, overweight/obesity and death (Fig. 1). The Markov model is a commonly used analytical framework where individuals move between health states over time, and costs and health outcomes are aggregated accordingly for a modelled cohort [18]. We developed age and sex-specific life tables for Vietnamese children aged 5–19 years and simulated until they reached 75 years of age or died. The life expectancy at birth in Vietnam was 75 years in 2019 according to the World Bank [19]. The modeled population was classified into underweight, healthy weight, overweight/obese weight statuses at the starting point of the model, and then transitioned between weight status categories until 75 years of age or death. The model estimated number of deaths, years of life lived and QALYs with an annual discount rate of 3%. The discount rate applied was derived from the WHO Guide to Cost-effectiveness Analysis [20] and recent cost-effectiveness studies in Vietnam [21, 22] to account for outcomes that occur in the future.
Data sources
Demographic profile and mortality
The model inputs with data sources are shown in Table 1 and all values of each parameter are listed in Additional file 1. The demographics of the model population by sex and 5-year age groups were from the Vietnam General Statistics Office [23]. We derived the all-cause mortality rates by sex and 5-year age group from the life table for Vietnam published by the WHO Global Health Observatory data repository 2019 (Additional file 1: Table 1-C) [24]. The mortality rates by single age were extrapolated using exponential functions as a best fit.
The mortality risk for underweight and overweight/obesity groups in adults were derived from the contemporary meta-analysis by the Global BMI Mortality Collaboration [29]. We applied differential mortality risks for adults by weight status categories using data from East Asia, as Vietnam-specific data were not available (Additional file 1: Table 1-D). Due to lack of data, we were not able to apply differential mortality risks for underweight and overweight/obesity groups in children. Therefore, our assumptions for those under the age of 20 are conservative.
Weight status and transition probabilities
The model consists of underweight, healthy weight, and overweight/obesity based on the WHO reference [31, 32]. The prevalence of underweight, healthy weight and overweight/obesity in Vietnam by sex and age were from the NCD Risk Factor Collaboration (Additional file 1: Table 1-A) [25, 26]. Underweight is defined as a BMI-for age below -2 Z-scores and overweight/obesity is defined as a BMI-for age above 1 Z-scores for children aged 5—19 years. In adults, underweight is defined as a BMI less than 18.5 kg/m2 and overweight/obesity is defined as a BMI greater than or equal to 25 kg/m2.
We used two cohort data sources to estimate the transition probabilities between different weight status (Additional file 1: Table 1-B). For those aged 5–22 years, we used Vietnam data from the Young Lives study [27] and for adults aged 23 years and over, we used data from the China Health and Nutrition Survey [28] as Vietnam-specific data were not available for adults. Briefly, Young Lives is an international longitudinal study which aims to investigate the changing nature of childhood poverty in four low-and-middle-income countries, including Vietnam, Ethiopia, India and Peru with around 3,000 participants in each country [27]. The China Health and Nutrition Survey is an ongoing open cohort to cover key public health risk factors and health outcomes, demographic, social and economic factors with around 18,764 participants [28]. Survey descriptions can be found elsewhere [27, 28].
We combined overweight and obese categories given that the prevalence of obesity was less than 3% in the Young Lives study. Estimating the transition probabilities was not possible due to the small sample size in the obesity group in the Young Lives study [27]. For instance, the sample size to estimate the change in weight status within the obese group was only 2 boys and 1 girl aged 15 years. Combining overweight and obesity has been applied to another study which also used the data from the Young Lives study to model trajectories in stunting and overweight status in children in Ethiopia, India, Peru and Vietnam [33]. In a modelling study of Nigerian women, malnutrition was classified into underweight (severe thinness and undernourished) and overweight (overweight and obesity) [34].
Quality of adjusted life years
Quality of life data were derived from a Vietnamese study [30]. For those aged 18–34 years, the utility scores were estimated from general population of 562 adults in Vietnam using the EQ-5D-5L instrument, but due to unavailability of weight data, the same utility values regardless of weight status were applied by sex and age groups. In the same Vietnamese study [30], weight data were available for different population in Ho Chi Minh City (n = 1,296), so utility values by sex, age groups and weight status for those aged 35 years and over were estimated accordingly. We applied utility values of 1 for children aged 5–17 years as utility data for children were not available. Utility values are presented in Additional file 1: Table 1-E. Utility scores as described above were then multiplied with years of life lived to generate QALYs.
Scenario analyses
Several scenario analyses were conducted to demonstrate the impact of being underweight or overweight/obese under various scenarios. The scenarios included a reduction in the prevalence of underweight and overweight/obesity, and changes in transition probabilities to underweight or overweight/obesity by 10%, 20% and 50%. Scenario analyses also estimated the outcomes from having no underweight and overweight/obesity in the population (i.e., an entirely healthy weight population) to estimate the total impact of malnutrition. To reflect the increasing trends in overweight/obesity, the model simulated a 10% increase in overweight/obesity. We also varied discount rates as 0%, 4% and 5%.
Sensitivity analyses
We performed one-way and probabilistic sensitivity analyses to assess the impact of uncertainties in input parameters on outcomes. As for one-way sensitivity analyses, we varied values of prevalence of underweight and overweight/obesity, transition probabilities between weight status and QALYs one by one based on lower and upper 95% confidence intervals (CI). We conducted probabilistic sensitivity analysis through second order Monte Carlo simulations by varying values of prevalence of underweight and overweight/obesity, transition probabilities between weight status, mortality risks, and utilities simultaneously. We ran the Monte Carlo simulation for 10,000 iterations through random sampling from values represented by different distributions to consider uncertainty in the model inputs. We assumed a uniform distribution for prevalence and transition probabilities, a lognormal distribution for mortality risks, and a beta distribution for utility scores as indicated in Additional file 1.
We used Microsoft Excel 2016 and @Risk 8.2 to construct the model and conduct scenario and sensitivity analyses. The model is validated through face validity and internal validity to reduce errors and better represent reality.
Ethical considerations
Ethics approval was not required as this study used publicly available data to construct the model. Regarding secondary data used in the study, ethics approvals for the Young Lives study were obtained in each study country and by the Social Sciences and Humanities Inter-Divisional Research Ethics Committee at the University of Oxford [27, 35]. The China Health and Nutrition Survey was approved by institutional review boards at the University of North Carolina at Chapel Hill and the National Institute of Nutrition and Food Safety [36]. The quality of life study in Vietnam was approved by the Ethical Review Board for Biomedical Research at the Hanoi University of Public Health [30]. All methods were carried out in accordance with relevant guidelines and regulations, and the study participants or caregivers of minors provided their informed consent [27, 30, 35, 36].
Results
The model simulated 22,058,773 Vietnamese children aged 5–19 years (11,444,303 boys and 10,614,470 girls) as presented in Table 2. The prevalence of underweight ranged from 12% to 18% in boys and 6% to 19% in girls depending on ages. The prevalence of overweight/obesity ranged from 7% to 22% in boys and 6% to 11% in girls depending on ages. There were more girls with healthy weight than boys across all the age groups.
Deaths, years of life lived, quality adjusted life years
As a base-case with current prevalence of underweight and overweight/obesity and transition probabilities between weight status for Vietnamese children aged 5–19 years simulated until they reached 75 years of age, the model estimated 9.68 million deaths (6.44 million men and 3.24 million women), 622 million years of life lived (317 million men and 305 million women), and 601 million QALYs (308 million men and 293 million women) (Table 3). There were more deaths, years of life lived and QALYs among healthy weight groups than underweight or overweight/obese groups reflecting the greater size of the healthy weight group population.
Scenario analyses
Scenario analyses demonstrated the changes in impact of being underweight or overweight/obese. Study outcomes under various scenarios are presented in Table 4 and the percentage difference compared to the base-case results are summarized in Additional file 2. The reduction in either underweight or overweight/obesity alone, and reduction in both underweight and overweight/obesity resulted in fewer deaths, more years of life lived and more QALYs gained. Reducing both underweight and overweight/obesity had a greatest impact on outcomes followed by reducing overweight/obesity alone and underweight alone. The total number of deaths decreased to 9.6 million, 9.5 million, 9.3 million when the prevalence of underweight and overweight/obesity and transition probabilities to underweight and overweight/obesity were reduced by 10%, 20% and 50%, respectively compared to the base-case results (9.7 million). In the scenario where everyone was a healthy weight, the model estimated 9.1 million deaths, which is 577,267 fewer deaths or 6.0% less (5.4% men and 7.0% women), 624 million years of life lived, which is 2 million more years of life lived or 0.3% more (0.5% men and 0.2% women), and 604 million QALYs, which is 3 million more QALYs gained or 0.6% more (0.4% men and 0.7% women) than base-case results. A 10% increase in overweight/obesity estimated 116,654 more deaths (1.2%), 494,474 fewer years of life lived (0.08%), and 897,866 fewer QALYs gained (0.15%) than base-case results. Compared to the base-case results with an annual discount rate of 3%, the model estimated 181 million fewer years of life lived and 174 million fewer QALYs with an annual discount rate of 5%.
Sensitivity analyses
One-way sensitivity analyses showed that transition probabilities of being or staying underweight or overweight/obese have a greater impact on years of life lived and QALYs than the prevalence of underweight and overweight/obesity (Table 5). Using the values of lower CI of prevalence of underweight and overweight/obesity or transition probabilities of being/staying underweight and overweight/obesity resulted in fewer deaths, more years of life lived, and more QALYs than base-case results.
Probabilistic sensitivity analyses estimated the mean and 95% CI for deaths, years of life lived and QALYs by sex (Table 6). In total, it estimated 9.7 million deaths (95% CI 9 to 10 million), 621 million years of life lived (95% CI 620 to 623 million) and 600 million QALYs (95% CI 571 to 617 million).
Discussion
This study shows the lifetime impact of being underweight or overweight/obese for children in Vietnam in 2019. The model estimated 9.68 million deaths, 622 million years of life lived, and 601 million QALYs under the current prevalence of underweight and overweight/obesity among children who were followed up to age 75 years. The model also provided various estimations to quantify the impact of child underweight and overweight/obesity under different scenarios. Compared to the hypothetical scenario with an entirely healthy weight population, modeling of the current child weight status in Vietnam estimated the 577,267 excess deaths, 2 million fewer years of life lived, and 3 million fewer QALYs due to being underweight or overweight/obesity. The findings highlight the preventable losses and opportunity for possible gains from tackling underweight and overweight/obesity at the population level in Vietnam.
There is limited evidence on long-term impact of being underweight or overweight/obese especially in low-and middle-income countries, including Vietnam. Our study highlights the adverse consequences of underweight or overweight/obesity through several scenario analyses in Vietnam. The number of deaths would decrease by 1.3% (1.3% men and 1.5% women), 3.5% (3.1% men and 4.1% women) and 6.0% (5.4% men and 7.0% women) under the scenarios where no one was underweight, no one was overweight/obese and everyone was healthy weight, respectively. Our results are not directly comparable with previous studies from other countries due to differences in population, health systems and socioeconomic factors in their specific contexts. Still, a few studies pointed to the adverse health and economic consequences of being underweight or overweight/obese. A review paper from Brazil on long-lasting effects of undernutrition reported consistent findings, including a higher risk of diabetes in adulthood, hypertension, dyslipidemia and a lowered working capacity of manual workers, among other physiological impairments [37]. Similarly, a meta-analysis found that the hazard ratio for all-cause mortality was 1.51 for underweight (BMI 15.0 to 18.5), 1.07 to 1.20 for overweight (BMI 25.0 to 30.0) and 1.45 to 2.76 for obesity (BMI 30 to 60) in Asia, Australia and New Zealand, Europe, and North America [29]. In addition, a modelling study from Georgia showed that a 1%-point reduction in both overweight and obese adolescents could reduce lifetime medical care costs by $586 million and increase lifetime QALYs by 47,138 [17]. In Germany, the excess lifetime direct cost per person of inpatient and outpatient treatment cost due to overweight and obesity during childhood was €4,262 for men and €7,028 for women [14], and the excess lifetime indirect costs per person such as opportunity cost of lost productivity was €4,209 for men and €2,445 for women [15]. The use of an estimate of US $19,000 as the incremental lifetime medical cost of an obese child relative to a normal weight child was recommended in the United States [38]. Furthermore, another modeling study from the United States found that lifetime medical care costs would decrease by US$586 million and lifetime QALYs would increase by 47,138 with a 1%-point reduction in both overweight and obese adolescents [17]. These studies all highlighted adverse effects of being underweight or overweight/obese during childhood.
Reduction in deaths and increases in years of life lived and QALYs were greatest when reducing both underweight and overweight/obesity followed by reducing overweight/obesity alone and underweight alone. Vietnam is undergoing changes in health and nutrition outcomes due to economic development and urbanization. The increasing prevalence of nutrition-related chronic disease and westernization of the traditional Vietnamese diet have been reported [39, 40]. Given that undernutrition and food insecurity still exist in Vietnam with climate change risks [41,42,43], more emphasis on solving the double burden of malnutrition is required. Double-duty actions which aim to tackle both undernutrition and problems of overweight/obesity simultaneously have been proposed, based on the rationale that all forms of malnutrition share common drivers, including early life nutrition, dietary diversity, food environments and socioeconomic factors [7]. In low-and middle-income countries like Vietnam with persistent undernutrition problems and rising overweight and obesity, undernutrition focused programs may unintentionally increase risks for obesity [7]. Hawkes et al. proposed ten double-duty actions regarding breastfeeding, growth monitoring, food fortification and supplements, cash and food transfers, school feeding programs, nutrition and agriculture programs, food system policies, and food environments to address all forms of malnutrition [7].
This study has some limitations as the model is based on secondary data, and as modeling studies are generally underpinned by several assumptions. We used best source available, yet due to data paucity in Vietnam, the model relied on data from China for transition probabilities between weight status for adults. We could not apply mortality risks by weight status among children due to lack of data, and for mortality risks among adults, we used data from East Asia. In addition, overweight and obesity were not separated and considered as one weight status category ‘overweight/obesity’ due to limited availability of data for children with obesity in Vietnam. It may have affected study findings by under- or over-estimation, which is commonly described in other modelling studies [16, 44,45,46]. However, we performed a number of sensitivity and scenario analyses to illustrate how the results change if certain model inputs are altered. For instance, we conducted scenario analyses by altering transition probabilities to underweight or overweight/obesity by 10%, 20% and 50% to see improved outcomes by reducing the prevalence of underweight and overweight/obesity. The model would produce better estimations when country specific and more reliable data become available. As a life table modeling study, another limitation is that mortality rates and transition probabilities remain constant throughout the model time horizon, which has been also indicated in previous modeling study [44]. Lastly, our estimations were limited to population-level data and did not provide disaggregated outcomes by socioeconomic factors or health conditions due to data unavailability. Future research can estimate study outcomes by socioeconomic groups or other health conditions to have a broader understanding of impact of being underweight or overweight/obese with an equity perspective.
Despite the limitations, this study can provide useful information for policy makers to understand the magnitude of lifetime impact of child underweight and overweight/obesity. Through several scenario analyses, the model estimated possible health benefits from tackling underweight and overweight/obesity and burden from the rise in overweight/obesity. The government can utilize the data for their priority setting, resource allocation and program development. Improving child health and nutrition will contribute to achieving the National Nutrition Strategy in Vietnam and global Sustainable Development Goals, in particular ‘Goal 2: Zero Hunger’ and ‘Goal 3: Good Health and Well-being.’ Another strength of this study is that the model captured both underweight and overweight/obesity. The model structure is transferable to other low-and middle-income countries where both underweight and overweight/obesity risk child development. Other countries can replicate the model and estimate their own situation by changing input parameters, including prevalence of underweight and overweight/obesity and mortality rates. It would be a useful way to quantify the burden of malnutrition at the population level within limited resources. The model structure in Excel is available in Additional file 3 for further use. The model can be made freely available as an online platform tool so researchers from low-and middle-income countries can have access to the model and adapt to their local contexts and available data.
Conclusions
This study quantified the lifetime impact of being underweight or overweight/obesity during childhood in Vietnam. Extensive scenario analyses showed that the reduction in underweight and overweight/obesity could result in fewer deaths, more years of life lived and more QALYs gained. Considering rapid changes with economic development, urbanization and nutrition transitions in Vietnam, tackling childhood underweight and overweight/obesity will be more crucial in improving health and nutrition. National policies such as the National Nutrition Strategy 2021–2030 for Vietnam and interventions in accordance with Sustainable Development Goals to address underweight and overweight/obesity are required for better life for every child and healthy society in Vietnam.
Availability of data and materials
The model structure in Excel is available in Additional file 3.
Abbreviations
- CI:
-
Confidence interval
- QALY:
-
Quality-adjusted life years
References
NCD Risk Factor Collaboration (NCD-RisC). Height and body-mass index trajectories of school-aged children and adolescents from 1985 to 2019 in 200 countries and territories: a pooled analysis of 2181 population-based studies with 65 million participants. Lancet. 2020;396(10261):1511–24. https://doi.org/10.1016/s0140-6736(20)31859-6.
Christian P, Smith ER. Adolescent undernutrition: global burden, physiology, and nutritional risks. Ann Nutr Metab. 2018;72(4):316–28. https://doi.org/10.1159/000488865.
Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. 2020;395(10217):75–88. https://doi.org/10.1016/s0140-6736(19)32472-9.
Norris SA, Frongillo EA, Black MM, Dong Y, Fall C, Lampl M, et al. Nutrition in adolescent growth and development. Lancet. 2022;399(10320):172–84. https://doi.org/10.1016/s0140-6736(21)01590-7.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–51. https://doi.org/10.1016/s0140-6736(13)60937-x.
Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020;395(10217):65–74. https://doi.org/10.1016/s0140-6736(19)32497-3.
Hawkes C, Ruel MT, Salm L, Sinclair B, Branca F. Double-duty actions: seizing programme and policy opportunities to address malnutrition in all its forms. Lancet. 2020;395(10218):142–55. https://doi.org/10.1016/s0140-6736(19)32506-1.
Socialist Republic of Vietnam. National nutrition strategy for 2011–2020, with a vision toward 2030. 2012.
Mai TMT, Pham NO, Tran TMH, Baker P, Gallegos D, Do TND, et al. The double burden of malnutrition in Vietnamese school-aged children and adolescents: a rapid shift over a decade in Ho Chi Minh City. Eur J Clin Nutr. 2020;74(10):1448–56. https://doi.org/10.1038/s41430-020-0587-6.
Le Nguyen BK, Le Thi H, Nguyen Do VA, Tran Thuy N, Nguyen Huu C, Thanh Do T, et al. Double burden of undernutrition and overnutrition in Vietnam in 2011: results of the SEANUTS study in 0·5-11-year-old children. Br J Nutr. 2013;110(Suppl 3):S45-56. https://doi.org/10.1017/s0007114513002080.
Vietnam National Institute of Nutrition. Main findings of general nutrition survey 2019–2020. 2021.
Briggs A, Sculpher M. An introduction to Markov modelling for economic evaluation. Pharmacoeconomics. 1998;13(4):397–409. https://doi.org/10.2165/00019053-199813040-00003.
Brennan A, Akehurst R, Modelling in health economic evaluation. What is its place? What is its value? Pharmacoeconomics. 2000;17(5):445–59. https://doi.org/10.2165/00019053-200017050-00004.
Sonntag D, Ali S, Lehnert T, Konnopka A, Riedel-Heller S, König HH. Estimating the lifetime cost of childhood obesity in Germany: results of a Markov model. Pediatr Obes. 2015;10(6):416–22. https://doi.org/10.1111/ijpo.278.
Sonntag D, Ali S, De Bock F. Lifetime indirect cost of childhood overweight and obesity: a decision analytic model. Obesity (Silver Spring). 2016;24(1):200–6. https://doi.org/10.1002/oby.21323.
Techakehakij W. Assessing long-term QALYs gain from averting and reversing overweight and obesity in childhood. Qual Life Res. 2016;25(10):2611–8. https://doi.org/10.1007/s11136-016-1285-7.
Wang LY, Denniston M, Lee S, Galuska D, Lowry R. Long-term health and economic impact of preventing and reducing overweight and obesity in adolescence. J Adolesc Health. 2010;46(5):467–73. https://doi.org/10.1016/j.jadohealth.2009.11.204.
York Health Economics Consortium. Markov Model 2016 [Available from: https://yhec.co.uk/glossary/markov-model/ [Accessed 1 Jul 2021].
World Bank. Life expectancy at birth, Vietnam [Available from: https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=VN [Accessed 1 Jul 2021].
Edejer T-T-T, Baltussen R, Adam T, Hutubessy R, Acharya A, Evans DB, et al. Making Choices in Health: WHO Guide to Cost-effectiveness Analysis. Geneva: World Health Organization; 2003.
Nguyen DT, Luong KN, Phan HT, Tran AT, Dao ST, Poudel AN, et al. Cost-Effectiveness of Population-Based Tobacco Control Interventions on the Health Burden of Cardiovascular Diseases in Vietnam. Asia Pac J Public Health. 2021:1010539521999873. https://doi.org/10.1177/1010539521999873.
Taylor C, Hoek AC, Deltetto I, Peacock A, Ha DTP, Sieburg M, et al. The cost-effectiveness of government actions to reduce sodium intake through salt substitutes in Vietnam. Arch Public Health. 2021;79(1):32. https://doi.org/10.1186/s13690-021-00540-4.
General Statistics Office. Completed results of the 2019 Viet Nam population and housing census. 2020.
WHO Global Health Observatory data repository. Life table for Vietnam [Available from: https://apps.who.int/gho/data/view.main.61830?lang=en [Accessed 1 Jul 2021].
NCD Risk Factor Collaboration (NCD-RisC). Child & Adolescent Body-Mass Index [Available from: https://ncdrisc.org/data-downloads-adiposity-ado.html [Accessed 1 Jul 2021].
NCD Risk Factor Collaboration (NCD-RisC). National Adult Body-Mass Index [Available from: https://ncdrisc.org/data-downloads-adiposity.html [Accessed 1 Jul 2021].
Favara M, Crivello G, Penny M, Porter C, Revathi E, Sánchez A, et al. Cohort profile update: the young lives study. Int J Epidemiol. 2021. https://doi.org/10.1093/ije/dyab111.
Popkin BM, Du S, Zhai F, Zhang B. Cohort profile: the China health and nutrition survey–monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol. 2010;39(6):1435–40. https://doi.org/10.1093/ije/dyp322.
Global BMI Mortality Collaboration, Di Angelantonio E, Bhupathiraju Sh N, Wormser D, Gao P, Kaptoge S, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776–86. https://doi.org/10.1016/s0140-6736(16)30175-1.
Mai VQ, Giang KB, Minh HV, Lindholm L, Sun S, Sahlen KG. Reference data among general population and known-groups validity among hypertensive population of the EQ-5D-5L in Vietnam. Qual Life Res. 2021;31(2):539–50. https://doi.org/10.1007/s11136-021-02959-2.
WHO. Growth reference data for 5–19 years [Available from: https://www.who.int/tools/growth-reference-data-for-5to19-years [Accessed 1 Jul 2021].
WHO Global Health Observatory data repository. Body Mass Index (BMI) [Available from: https://www.who.int/data/gho/data/themes/theme-details/GHO/body-mass-index-(bmi) [Accessed 1 Jul 2021].
Schott W, Aurino E, Penny ME, Behrman JR. The double burden of malnutrition among youth: trajectories and inequalities in four emerging economies. Econ Hum Biol. 2019;34:80–91. https://doi.org/10.1016/j.ehb.2019.05.009.
Owoeye SM, Oseni BM, Gayawan E. Estimating lifetime malnourished period and its statistics based on the concept of Markov chain with reward. Heliyon. 2020;6(5):e04073-e. https://doi.org/10.1016/j.heliyon.2020.e04073.
Barnett I, Ariana P, Petrou S, Penny ME, le Duc T, Galab S, et al. Cohort profile: the Young Lives study. Int J Epidemiol. 2013;42(3):701–8. https://doi.org/10.1093/ije/dys082.
Zhang B, Zhai FY, Du SF, Popkin BM. The China Health and Nutrition Survey, 1989–2011. Obes Rev. 2014;15 Suppl 1(0 1):2–7.https://doi.org/10.1111/obr.12119.
Martins VJB, Toledo Florêncio TMM, Grillo LP, do Carmo P Franco M, Martins PA, Clemente APG, et al. Long-lasting effects of undernutrition. Int J Environ Res Public Health. 2011;8(6):1817–46. https://doi.org/10.3390/ijerph8061817.
Finkelstein EA, Graham WC, Malhotra R. Lifetime direct medical costs of childhood obesity. Pediatrics. 2014;133(5):854–62. https://doi.org/10.1542/peds.2014-0063.
Harris J, Nguyen PH, Tran LM, Huynh PN. Nutrition transition in Vietnam: changing food supply, food prices, household expenditure, diet and nutrition outcomes. Food Security. 2020;12(5):1141–55. https://doi.org/10.1007/s12571-020-01096-x.
Nguyen TT, Trevisan M. Vietnam a country in transition: health challenges. BMJ Nutr Prev Health. 2020;3(1):60–6. https://doi.org/10.1136/bmjnph-2020-000069.
Beal T, Le DT, Trinh TH, Burra DD, Huynh T, Duong TT, et al. Child stunting is associated with child, maternal, and environmental factors in Vietnam. Matern Child Nutr. 2019;15(4):e12826. https://doi.org/10.1111/mcn.12826.
Kim C, Alvarez C, Sattar A, Bandyopadhyay A, Azzarri C, Moltedo A, et al. Production, Consumption, and Food Security in Viet Nam Diagnostic Overview. Washington, D.C.: International Food Policy Research Institute and Food and Agriculture Organization; 2021.
Huong NTL, Yao S, Fahad S. Assessing household livelihood vulnerability to climate change: the case of Northwest Vietnam. Hum Ecol Risk Assess. 2019;25(5):1157–75. https://doi.org/10.1080/10807039.2018.1460801.
Satyana RPU, Uli RE, Magliano D, Zomer E, Liew D, Ademi Z. Assessing the impact of smoking on the health and productivity of the working-age Indonesian population using modelling. BMJ Open. 2020;10(11):e041832. https://doi.org/10.1136/bmjopen-2020-041832.
Afroz A, Hird TR, Zomer E, Owen A, Chen L, Ademi Z, et al. The impact of diabetes on the productivity and economy of Bangladesh. BMJ Glob Health. 2020;5(6). https://doi.org/10.1136/bmjgh-2020-002420.
Ademi Z, Marquina C, Zomer E, Bailey C, Owen A, Pang J, et al. The economic impact of familial hypercholesterolemia on productivity. J Clin Lipidol. 2020;14(6):799-806.e3. https://doi.org/10.1016/j.jacl.2020.08.004.
Acknowledgements
At the time of submission, YB is supported by the Australian Government Research Training Program (RTP) Scholarship. ZA is supported by a Monash Bridging Fellowship. JF is supported by the Finkel Professorial Fellowship which is funded by the Finkel Family Foundation. TT is supported by a Monash Strategic Bridging Fellowship. The sponsors had no role in study design and publication of the study.
Funding
None.
Author information
Authors and Affiliations
Contributions
YB, AO, JF, TT and ZA conceptualized the study and built the model. YB performed the analyses with technical support from ZA, and all authors contributed to data interpretation and model validation. YB drafted the first manuscript and other authors reviewed and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was not required as this study used publicly available data to construct the model. Regarding secondary data used in the study, ethics approvals for the Young Lives study were obtained in each study country and by the Social Sciences and Humanities Inter-Divisional Research Ethics Committee at the University of Oxford. The China Health and Nutrition Survey was approved by institutional review boards at the University of North Carolina at Chapel Hill and the National Institute of Nutrition and Food Safety. The quality of life study in Vietnam was approved by the Ethical Review Board for Biomedical Research at the Hanoi University of Public Health. All methods were carried out in accordance with relevant guidelines and regulations, and the study participants or caregivers of minors provided their informed consent.
Consent for publication
Not applicable.
Competing interests
Jane Fisher is a Senior Board Member for BMC Women's Health and had no role in the peer review process of this article. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 1.
Model inputs.
Additional file 2:
Supplementary Figure 1. Differences in study outcomes ((A) deaths, (B) years of life lived, (C) QALYs) between various scenarios and base-case results.
Additional file 3:
The model structure in Excel.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Baek, Y., Owen, A.J., Fisher, J. et al. Lifetime impact of being underweight or overweight/obese during childhood in Vietnam. BMC Public Health 22, 645 (2022). https://doi.org/10.1186/s12889-022-13061-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13061-8