Abstract
Introduction
Long-term exposure to ambient air pollution is related to major cardiovascular risk factors including diabetes, hypertension, hyperlipidemia and overweight, but with few studies in high-concentration nations like China so far. We aimed to investigate the association between long-term exposure to ambient fine particulate matter (particles with an aerodynamic diameter ≤ 2.5 μm, PM2.5) and major cardiovascular risk factors in China.
Methods
Adult participants with selected biochemical tests were recruited from the Chinese Physiological Constant and Health Condition (CPCHC) survey conducted from 2007 to 2011. Gridded PM2.5 data used were derived from satellite-observed data with adjustment of ground-observed data. District-level PM2.5 data were generated to estimate the association using multivariate logistic regression model and generalized additive model.
Results
A total of 19,236 participants from the CPCHC survey were included with an average age of 42.8 ± 16.1 years, of which nearly half were male (47.0%). The annual average PM2.5 exposure before the CPCHC survey was 33.4 (14.8–53.4) μg/m3, ranging from 8.0 μg/m3 (Xiwuqi) to 94.7 μg/m3 (Chengdu). Elevated PM2.5 was associated with increased prevalence of hypertension (odds ratio (OR) =1.022, 95% confidence interval (95%CI): 1.001, 1.043) and decreased prevalence of overweight (OR = 0.926, 95%CI: 0.910, 0.942). Education significantly interacted with PM2.5 in association with all the interesting risk factors. Each 10 μg/m3 increment of PM2.5 was associated with increased prevalence of diabetes (OR = 1.118, 95%CI: 1.037, 1.206), hypertension (OR = 1.101, 95%CI: 1.056, 1.147), overweight (OR = 1.071, 95%CI: 1.030, 1.114) in participants with poor education, but not in well-educated population. PM2.5 exposure was negatively associated with hyperlipidemia in all participants (OR = 0.939, 95%CI: 0.921, 0.957). The results were robust in all the sensitivity analyses.
Conclusion
Association between long-term PM2.5 exposure and cardiovascular risk factors might be modified by education. PM2.5 was associated with a higher prevalence of diabetes, hypertension, and overweight in a less-educated population with time-expose dependency. Long-term exposure to PM2.5 might be associated with a lower prevalence of hyperlipidemia.
Similar content being viewed by others
Introduction
Despite the improvements in the air quality of China, air pollution still plays an important role in public health issues during the past decades. The ambient fine particulate matter (particles with an aerodynamic diameter ≤ 2.5 μm, PM2.5) might contribute to 1.1 million (95%CI: 1.0 million to 1.8 million) deaths in China [1], with the most common reason as cardiovascular disease (CVD) mortality [2, 3]. As strong predictors for 10-year risk of CVD [4], the prevalence of hypertension, diabetes, dyslipidemia and overweight was 24.3, 4.3, 49.3 and 32.0%, respectively [5], according to the analysis of 23,010 subjects from Chinese Physiological Constant and Health Condition (CPCHC) conducted from 2007 to 2011. Intervention of risk factors mentioned above would undoubtedly decrease the burden of cardiovascular disease.
Association between the cardiovascular risk factors and PM2.5 was vastly investigated, but the result remained inconsistent, with some reporting positive association and some reporting non-association even negative association [6,7,8,9,10,11,12,13]. Moreover, most research was conducted in North America and Europe where annual PM2.5 is below 35μg/m3, with only a few studies conducted in developing countries like China, which often suffer a much higher concentration and greater domestic variability [14]. Even those conducted in developing countries were region-based [5], hardly covering the full PM2.5 spectrum and effects of ethnicity. Meanwhile, previous research suggested that education was a strong modifier of health effects of air pollution [15, 16], and studies exploring the association between PM2.5 and cardiovascular risk factors in China mainly focused on population with preliminary or below education attainment [12, 17,18,19,20]. Considering evidence for the increasing prevalence of diabetes, hypertension, hyperlipidemia and overweight in those newly industrialized countries were emerging [21,22,23,24], it was of great significance to explore the potential associations between PM2.5 and these metabolic disorders in a nationwide population-based database.
Hence, we aimed to investigate the association between long-term exposure to PM2.5 and the prevalence of major cardiovascular risk factors, including hypertension, diabetes, hyperlipidemia and overweight. Because of the air pollution exposure connected with the social-economic status of the population, the modification effect of education level as an indicator of social-economic status was also analyzed.
Methods
Study participants
Participants from the Chinese Physiological Constant and Health Condition (CPCHC) survey were included. Details about CPCHC survey have been reported before [5, 25,26,27]. Briefly, the CPCHC survey was a cross-sectional, population-based survey covering 82,806 participants from 6 provinces in the north, south, east and west of China (Sichuan, Heilongjiang, Hunan, Inner Mongolia, Yunnan and Ningxia) from 2007 to 2011. Participants were selected under the principle of multistage stratified random cluster sampling, and 35% of them finished the biochemical examination. Adult participants (older than 18 years old) of CPCHC were included. Participants with incomplete information on age, sex, education, ethnicity, smoking status, drinking status, intensity of physical activity, diet types or with missing data on BMI, waist circumference (WC), systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting blood glucose (FBG), serum level of triglyceride, cholesterol, high-density lipoprotein cholesterol (LDL-C), low-density lipoprotein cholesterol (HDL-C) were excluded. Before data collection, we obtained the written informed consent from each participant. The protocol was in line with the Helsinki Declaration and approved by the ethic review board of the Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences.
Data collection and definitions
We designed a standard questionnaire to gather the necessary information, including age, sex, education, ethnicity, smoking status, drinking status, intensity of physical activity and diet types. A participant was categorized as less-educated if one only received preliminary or below education or no schooling. The minority is composed of ethnic groups other than Han ethnicity. Current smoker and current drinker were defined as participants with self-reported responses of “yes” to the question “Do you smoke cigarettes now?” and “Do you drink now?” respectively. A lower threshold of cigarettes smoked was one, and the minimal drinking amount for liquor was 150 g or less, 1 bottle or less for beer, and 50 g or less for other alcoholic beverages. Intensity of physical activity was defined as low, moderate, or high according to the self-reported labor or sports intensity on average. Diet types include sugar-rich diet, salt-rich diet, spicy diet, fat-rich diet, light diet, and each was defined as self-reported “yes” to the questions “Are your daily diet sugar-rich?”, “Are your daily diet salt-rich?”, “Are your daily diet spicy?”, “Are your daily diet fat-rich?”, “Are your daily diet light?”, respectively. Residence (urban, rural) and region (south, north) were determined by the surveyed location.
Meanwhile, physical examination included measurement of height, weight, BMI, WC, SBP and DBP. BMI was defined as weight (kg) divided by square of height (m2). WC was measured in a standing position with soft inelastic tape at the end of a gentle expiration. We asked each participant to rest quietly for at least 10 min before blood pressure measurement by trained medical personnel using an electric sphygmomanometer (OMRON, HEM-7000). The documented blood pressure was average value of the three-time test. We asked each participant to fast overnight before the biochemical test. The cholesterol, HDL-C, LDL-C, and triglycerides were measured by Beckman AU Series Automatic Biochemical Analyzer (Japan) and Sekisui Medical (Japan) reagents, while FBG by Beckman AU reagents.
Diabetes was diagnosed as FBG ≥7.0 mmol/L, or with current anti-diabetes drug use. Hypertension was diagnosed as an average SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg, or with anti-hypertensive drug use. Hyperlipidemia was diagnosed as cholesterol ≥5.2 mmol/L. Overweight was diagnosed as BMI ≥ 24 kg/m2.
A directed acyclic graph (DAG, Fig. S1) was used to identify potential confounding variables using DAGitty v1.0 software. The covariates included in data analysis were as followed: age (year), sex, education (preliminary school or below, middle school, high school, college or above), ethnicity (Han, Yi, Hui, Mongolian, Tibetan, Korean, Tujia, Miao, others), smoking status (current smoker, nonsmoker), drinking status (current drinker, nondrinker), intensity of physical activity (low, moderate, high), diet types (sugar-rich diet, salt-rich diet, spicy diet, fat-rich diet, light diet), residence (urban, rural), region (south, north).
Air pollution exposure measurements
We obtained PM2.5 data from the website of Atmospheric Composition Analysis Group (http://fizz.phys.dal.ca/~atmos/martin/?page_id=140). The detailed process of PM2.5 data generation was the same as reported [28, 29]. The gridded PM2.5 data recording annual average PM2.5 concentration was transformed from GEOSChem model and satellite observations of aerosol optical depth (AOD), with a resolution of 0.1° × 0.1° (latitude times longitude). A PM2.5 dataset ranging from 2000 to 2016 was then corrected by the raw data with ground-based PM2.5 data in China from May 2014 to December 2016, using the geographically weighted regression (GWR) method. The gridded PM2.5 data from 2001 to 2010 in China used in this study were then processed using ArcMap (version 10.6.1, ESRI Inc). District-level annual average PM2.5 data 1 year, 2 years, 3 years, 4 years and 5 years before the CPCHC survey was generated to represent the exposure level for residents in each surveyed city.
Statistical analysis
Continuous variables with normal distribution were presented as the mean (standard deviation) and compared by independent sample t-test. Skewed distributed variables were presented as the median (interquartile range) and analyzed by the Mann-Whitney U test. Categorical data were presented as percentages and compared by the χ2 test.
Logistic regression analyses were used to estimate the association between 5-year PM2.5 (each 10 μg/m3 increase) and major cardiovascular risk factors, including diabetes, hyperlipidemia, hypertension and overweight. In crude model, no covariates were included. In multivariate logistic regression model, age, sex, education, ethnicity, smoking status, drinking status, intensity of physical activity and diet types were included as covariates. Interaction was tested by introducing interaction terms into the overall model using likelihood ratio test. Generalized additive model was used to explore the exposure-response relationship between PM2.5 and major cardiovascular risk factors. A series of sensitivity analyses were conducted. First, we constructed regression models adjusted by introducing covariates stepwise. Second, we used PM2.5 exposure defined from 1-year to 5-year exposure value as well as dichotomous PM2.5 exposure to assess the association between PM2.5 and cardiovascular risk factors. We dichotomized PM2.5 exposure with a cutoff value at 35 μg/m3 because an annual mean PM2.5 concentration of 35 μg/m3 was the interim targets level by WHO Air quality guidelines [30]. Third, stratification analyses according to disease status (yes or no), residence or region were conducted and a cross-product term were also added into the overall model to test for interaction. The P-values were two-sided, and P < 0.05 were considered statistically significant. All statistical analyses were performed with R (Version 4.0.3, R Core Team).
Results
82,806 participants were in enrolled in the CPCHC survey (Fig. 1). Among 36,623 participants who were selected to participate in biochemical tests, 29,919 of them completed a standard questionnaire surveying demographic information (age, sex, education, ethnicity, etc.) and lifestyles (smoking status, drinking status, intensity of physical activity, diet types, etc.). Excluding 1091 participants with missing data on BMI, WC, SBP or DBP and 322 participants without data on FBG, TG, TC, LDL-C or HDL-C, the remaining 19,236 participants whose age older than 18 years old were selected for the present study.
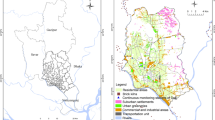
The mean age was 42.8 ± 16.1 years (Table 1). 53.0% of the studied population were female. 22.2% of the participants attained preliminary school or below education, and 58.6% of the studied population attained at least a high school education. Most of the participants were Han ethnicity (62.9%), nonsmoker (78.9%), nondrinker (76.9%), and moderate physical activity (53.8%). A small proportion of the participants reported diet types as spicy diet (22.0%), light diet (18.7%), sugar-rich diet (13.0%), salt-rich diet (10.7%), or fat-rich diet (9.0%). Nearly half of the participants were urban residents (50.8%) and came from southern China (53.2%). In general, 755 (3.9%), 4383 (22.8%), 5391 (28.0%) and 7727 (40.2%) of the participants had diabetes, hypertension, hyperlipidemia, and overweight, respectively. The median concentration of PM2.5 was 33.4 (IQR 14.8–53.4) μg/m3 in the surveyed cities, covering northern, southern, eastern and western China (Fig. S2). Chengdu was reported with the highest concentration (94.7 μg/m3), while the lowest level of PM2.5 exposure was documented in Xiwuqi (8.0 μg/m3) (Fig. S3). The prevalence of hypertension and hyperlipidemia were significantly lower in the urban region (Table S1). The prevalence of hypertension and overweight were significantly lower in southern China, but the prevalence of hyperlipidemia was higher (Table S2).
In general, each 10 μg/m3 increment of 5-year PM2.5 exposure was associated with hypertension (OR = 1.022, 95%CI: 1.001, 1.043), hyperlipidemia (OR = 0.939, 95%CI: 0.921, 0.957), and overweight (OR = 0.926, 95%CI: 0.910, 0.942), after adjustment of age, sex, education, ethnicity, smoking, drinking, intensity of physical activity and diet types (Fig. 2). Education was the only covariate that significantly interacted with PM2.5 on association with all the interesting risk factors (P for interaction: diabetes< 0.001, hypertension < 0.001, hyperlipidemia = 0.004, overweight < 0.001, respectively.) (Fig. 3). In general, PM2.5 was associated with increased prevalence of diabetes (OR = 1.118, 95%CI: 1.037, 1.206), hypertension (OR = 1.101, 95%CI: 1.056, 1.147) and overweight (OR = 1.071, 95%CI: 1.030, 1.114) in population with preliminary or below education attainment, but decreased prevalence of hyperlipidemia (OR = 0.915, 95%CI: 0.878, 0.953). The exposure-response analysis revealed that PM2.5 had near-linear relationship with diabetes, hypertension and hyperlipidemia in less-educated population, but the prevalence of overweight was firstly increased and then decreased with the increase of PM2.5 exposure (Fig. 4). The corresponding relationship in the general population, as well as in the well-educated population, was different from the less-educated, especially the association between PM2.5 and diabetes in the less-educated, the general, and the well-educated population, which were positive, null and inverse respectively (Figs. S4, S5).
Association between PM2.5 exposure and cardiovascular risk factors prevalence. The odds ratios and relevant 95% CI were scaled to each 10 μg/m3 PM2.5 exposure and calculated by multivariable logistic regression in crude model, and further adjusted for age, sex, education, ethnicity, smoking status, drinking status, intensity of physical activity, and diet types in adjusted model
Association between PM2.5 exposure and cardiovascular risk factors prevalence stratified by covariates. Population was stratified by age, sex, education, ethnicity, smoking status, drinking status, intensity of physical activity, and diet types. The odds ratios and relevant 95% CI were scaled to each 10 μg/m3 PM2.5 exposure and calculated by multivariable logistic regression, and further adjusted for age, sex, education, ethnicity, smoking status, drinking status, intensity of physical activity, and diet types. The significance of interaction effect was tested by introducing an interaction term in the regression model
Exposure-response relationship between PM2.5 exposure and cardiovascular risk factors prevalence in population with preliminary or below education. (A) diabetes; (B) hypertension; (C) hyperlipidemia; (D) being overweight. The exposure-response relationship was calculated by generalized additive model, and further adjusted by age, sex, ethnicity, smoking status, drinking status, intensity of physical activity, diet types. Knots used in the generalized additive model was 3. P value was denoted in each panel
In sensitivity analyses, we introduced the covariates stepwise in the regression models, and the regression result tended to be stable after being adjusted by age, sex, education and ethnicity, and model 7 was used in this study which included age, sex, education, ethnicity, smoking status, drinking status, intensity of physical activity and diet types (Fig. S6). The PM2.5 exposure values defined by different time duration were highly correlated, and the model stayed stable after changing the PM2.5 exposure used in the regression model (Fig. S7). Meanwhile, the association between binary PM2.5 exposure and cardiovascular risk factors was similar to the results of continuous PM2.5 exposure (Fig. S8). Stratified by disease status, we found that the general trend of PM2.5 association with each risk factor was generally stable. However, hypertension (P for interaction < 0.001 for hyperlipidemia; P for interaction = 0.009 for overweight) and overweight (P for interaction = 0.039 for diabetes; P for interaction = 0.041 for hypertension; P for interaction < 0.001 for hyperlipidemia) were the risk factors that interacted with PM2.5 (Fig. 5). Residence strongly interacted with PM2.5 on all the risk factors (Fig. S9), but region significantly interacted with PM2.5 only on hypertension (Fig. S10). Besides, in models adjusted for age, sex, education, ethnicity, smoking, drinking, the intensity of physical activity, diet types, and residence, the results remained robust compared to models without residence adjustment (Figs. S11, S12, S13, S14).
Association between PM2.5 exposure and cardiovascular risk factors prevalence stratified by cardiovascular risk factors. The odds ratios and relevant 95% CI were scaled to each 10 μg/m3 PM2.5 exposure and calculated by multivariable logistic regression, and further adjusted for age, sex, education, ethnicity, smoking status, drinking status, intensity of physical activity, and diet types
Discussion
In this study, we firstly used a multi-provincial and cross-ethnical study in China to demonstrate that long-term high concentration PM2.5 exposure (8.0–94.7 μg/m3) was positively associated with diabetes, hypertension, and overweight in the participants with poor education, but not in the well-educated population of Chinese adults. After adjusting for several potential confounders, the negative association between PM2.5 exposure and hyperlipidemia remained robust and significant among 19,236 multiethnic Chinese adults.
Our findings suggest that higher long-term PM2.5 exposure was positively associated with diabetes, hypertension, and overweight in the participants with poor education. Significant positive association between PM2.5 and diabetes, hypertension and overweight was also reported in several cohort studies, including a few Chinese cohorts [7, 9, 31,32,33], and regions with lower PM2.5 concentration, like American [34, 35], Canadian [36, 37], and Korean [38]. Our results were also consistent with several cross-sectional studies among the Chinese population [12, 17,18,19,20]. Participants with preliminary or below education attainment accounted for 63.23, 63.5, 59.5, 69.2 and 68.1% on Yang’s study on diabetes [20], Liu’s study on diabetes [19], Lin’s study on hypertension [17], Liu’s study hypertension [18], and Yang’s study on overweight [12].
However, we did not observe significant association between PM2.5 and diabetes or hypertension in participants with middle school or above education attainment. This discrepancy may partly be due to education was a strong modifier of the health effects of air pollution [15]. As an important indicator of socio-economic status (SES), education may modify the health effects of air pollution in several ways. First, the less-educated were more associated with higher pollution exposure in their working environment, such as mining, heavy industrial, construction and other outdoor jobs. Second, smoke produced by traditional biofuel burning and insufficient ventilation in kitchen may aggravate household pollution, which is also more common in the low SES population. Evidence also exists suggesting that individuals with lower education are generally more exposed to more PM2.5 pollution than those with higher education in the workday, or the workplace, even at home [39]. Third, lower education groups might lack access to medical care and awareness of disease, resulting in worse health outcomes [40]. Fourth, lower SES was related to higher stress levels, thus affecting the neuroendocrine dysfunction and leading to development of diabetes and hypertension [16, 41]. Several other cohort studies also investigated the association between diabetes and hypertension but made null conclusions, including American cohorts [6, 8], and German cohort [42], which may partly be due to modification of education attainment. We also reported that PM2.5 would decrease the prevalence of overweight in better-educated groups, which was consistent with a previous study revealing populations with high SES were less likely to be obese and vice versa [43]. Income-level and peer effects can partly explain the modification of education on obesity [44]. Dose-response curve revealed a non-linear effect of PM2.5 on overweight, which was also reported in previous literature. According to de Bont et al. [45], the association between PM2.5 and obesity was most evident for PM2.5 from 20 to 28 μg/m3 but not higher, a range lower than the median value than our research. This could be attributed to both the dosage saturation effect and other social factors. In the past few decades, air pollution, especially PM2.5 has drawn extensive attention in China due to information spread by social media, television, newspaper, etc. Corresponding initiatives against air pollution might thus result in better health conditions, especially those who perceived earlier and took it carefully, which coincided with the high-educated population in this study. Nonetheless, such a protective effect might be absent in lower PM2.5 exposure region, which might explain the non-linear effect. Similar effect could be observed for hypertension, which also showed a protective trend at the high end of the PM2.5 spectrum. However, caution should be taken as this subgroup has smaller sample size. More investigation should be taken before any definite conclusion.
We also observed that health effect of PM2.5 was different between the male and the female. The difference between males and female was explored in previous studies [15, 46, 47], but the patterns remained inconsistent. Region interacted with PM2.5 on the prevalence of hypertension, which might be explained by the association between region and temperature, while the lower outdoor temperature is strongly associated with a higher prevalence of hypertension [48, 49]. Urban-rural disparities in the prevalence of diabetes [50], hypertension [51], dyslipidemia [52] and overweight [53] in China have been reported. Urban or rural residence strongly interacted with PM2.5 on the prevalence of each cardiovascular risk factor. Residence was also an indicator of SES as education, and educational attainment and residence were also highly correlated in this study (data not shown). The rural-to-urban migration trend [54] and urbanization degree would change the risk of acquiring chronic diseases [55], but relevant data were not recorded in CPCHC survey, which may result in biased estimation of rural-urban effect. These results may have occurred by chance or may reveal underlying challenges in analyses of air pollution where multiple, highly correlated attributes of air pollutions of an individual’s environment can potentially play a role.
Only a few studies investigated the relationship between long-term PM2.5 exposure and cholesterol or hyperlipidemia, and the findings remained inconsistent [10, 11, 13, 56,57,58]. In this study, we demonstrated that PM2.5 exposure was associated with decrease in the prevalence of hyperlipidemia in both low and high educational groups. However, no significant association was reported in a cross-sectional study in the USA [58], and a 12-month PM2.5 exposure cohort study of midlife American women [10]. Meanwhile, previous studies conducted in different provinces of China revealed a significant positive association between PM2.5 exposure and cholesterol level [11, 56, 57]. The inconsistency among those studies may result from the following reasons. Firstly, annual PM2.5 was below 35μg/m3 in most research mentioned above, much lower than our research. Even previous studies conducted in China were province-based and had not covered the full spectrum of PM2.5 concentrations considered in our analyses. This may suggest the association between PM2.5 and lipid might be concentration-dependent. Secondly, sex may influence the health effect of PM2.5, and our analysis for female participants revealing null association as in the midlife-American women study [10]. Thirdly, ethnicity may be a strong mediator of metabolic syndrome [59], but previous Chinese studies included only participants in eastern China, including Taiwan [56], Liaoning [57], and Henan [11], and the majority of participants were Han ethnicity. Health-related behaviors and lifestyle factors of different ethnicity would shape different lipid profiles, thus modifying the effect of air pollution [60]. Mao et al. also reported that increased PM2.5 pollution was associated with decreased TG in the rural population of China [11], which also indicated the difficulty to explore the health effect of PM2.5.
The mechanisms underlying PM2.5 and cardiovascular risk factors have been vastly studied. Inhalation of particulate matter by lung can lead to autonomous nervous system imbalance, lung inflammation and alveolocapillary translocation. It was also followed by releasing of catecholamines and systemic inflammation, resulting in various subclinical and clinical disorders, including diabetes and hypertension, as indicated in our study focusing on participants with preliminary or below school education [61]. Recent experimental evidence suggested that long-term and heavy PM2.5 exposure would reduce total cholesterol level and triglyceride level, leading to lipid peroxidation and dyslipidemia, which may partly explain the discrepancy between our study and previous conclusions [62]. Another recent study on mice revealed that female mice were more susceptible to ambient PM2.5 exposure-induced hepatic cholesterol accumulation, indicating that health effect of PM2.5 may be sex-dependent [63]. The mechanisms underlying the association between PM2.5 and cholesterol and body weight should be furthered explored.
To our best knowledge, this is the largest multi-provincial and multi-ethnic study in developing countries to date and covered the broadest PM2.5 spectrum, providing evidence for health effect of PM2.5 in both high concentration and low concentration. Previous studies conducted in American and European countries fail to cover the impact of high PM2.5 concentration (>35μg/m3) on CVD risk factors. This research also demonstrated population with lower education might be especially susceptible to PM2.5 association with CVD risk factors.
Limitations
We acknowledge that our study has several limitations. Firstly, designed as a cross-sectional study, we cannot establish a cause-effect relationship between PM2.5 and cardiovascular risk factors. Secondly, we only evaluated the effect of PM2.5 based on data at district-level but not at individual-level. The association of other air pollutants should be explored and more precise measurement of personal exposure method should be developed. Thirdly, we only tested the fast glucose once and combined with the medical history of diabetes, did not measure the glycosylated hemoglobin and postprandial blood glucose, which might misestimate the prevalence of diabetes. Meanwhile, covariates including current smoking status, current drinking status, intensity of physical activity and diet types were self-reported and misclassification bias was inevitable, which may influence the association between PM2.5 and cardiovascular risk factors. Fourthly, although many potentials confounders were taken into consideration, we did not acquire adequate socioeconomic factors other than education and comorbid diseases, which may modify the exposure-outcome associations. Fifthly, the effects of other air pollutants, such as PM1, PM10, and NO2, are also deserved exploration. Due to lack of accessibility to other air pollutants measurement, health effects of PM1, PM10, and NO2, were not analyzed in this study.
Conclusion
Long-term PM2.5 exposure was associated with higher prevalence of diabetes, hypertension, and overweight in the less-educated general population, which contributed to the cardiovascular disease. The robust protection effect of high-concentration PM2.5 exposure in hyperlipidemia needs more studies.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the global burden of diseases study 2015. Lancet. 2017;389(10082):1907–18. https://doi.org/10.1016/S0140-6736(17)30505-6.
Franklin BA, Brook R, Arden Pope C, 3rd. Air pollution and cardiovascular disease. Curr Probl Cardiol. 2015;40(5):207–38. https://doi.org/10.1016/j.cpcardiol.2015.01.003.
Hoek G, Krishnan RM, Beelen R, Peters A, Ostro B, Brunekreef B, et al. Long-term air pollution exposure and cardio- respiratory mortality: a review. Environ Health. 2013;12(1):43. https://doi.org/10.1186/1476-069X-12-43.
Ueda P, Woodward M, Lu Y, Hajifathalian K, al-Wotayan R, Aguilar-Salinas CA, et al. Laboratory-based and office-based risk scores and charts to predict 10-year risk of cardiovascular disease in 182 countries: a pooled analysis of prospective cohorts and health surveys. Lancet Diabetes Endocrinol. 2017;5(3):196–213. https://doi.org/10.1016/S2213-8587(17)30015-3.
Wu J, Cheng X, Qiu L, Xu T, Zhu G, Han J, et al. Prevalence and clustering of major cardiovascular risk factors in China: a recent cross-sectional survey. Medicine (Baltimore). 2016;95(10):e2712. https://doi.org/10.1097/MD.0000000000002712.
Puett RC, Hart JE, Schwartz J, Hu FB, Liese AD, Laden F. Are particulate matter exposures associated with risk of type 2 diabetes? Environ Health Perspect. 2011;119(3):384–9. https://doi.org/10.1289/ehp.1002344.
Qiu H, Schooling CM, Sun S, Tsang H, Yang Y, Lee RSY, et al. Long-term exposure to fine particulate matter air pollution and type 2 diabetes mellitus in elderly: a cohort study in Hong Kong. Environ Int. 2018;113:350–6. https://doi.org/10.1016/j.envint.2018.01.008.
Wallwork RS, Colicino E, Zhong J, Kloog I, Coull BA, Vokonas P, et al. Ambient fine particulate matter, outdoor temperature, and risk of metabolic syndrome. Am J Epidemiol. 2017;185(1):30–9. https://doi.org/10.1093/aje/kww157.
Huang K, Yang X, Liang F, Liu F, Li J, Xiao Q, et al. Long-term exposure to fine particulate matter and hypertension incidence in China. Hypertension. 2019;73(6):1195–201. https://doi.org/10.1161/HYPERTENSIONAHA.119.12666.
Wu XM, et al. Associations between fine particulate matter and changes in lipids/lipoproteins among midlife women. Sci Total Environ. 2019;654:1179–86. https://doi.org/10.1016/j.scitotenv.2018.11.149.
Mao S, Chen G, Liu F, Li N, Wang C, Liu Y, et al. Long-term effects of ambient air pollutants to blood lipids and dyslipidemias in a Chinese rural population. Environ Pollut. 2020;256:113403. https://doi.org/10.1016/j.envpol.2019.113403.
Yang, Z., Song Q., Li J., Zhang Y., Air Pollution as a Cause of Obesity: Micro-Level Evidence from Chinese Cities. Int J Environ Res Public Health, 2019. 16(21), 16, 21, DOI: https://doi.org/10.3390/ijerph16214296.
Yang BY, Guo Y, Markevych I, Qian Z(M), Bloom MS, Heinrich J, et al. Association of Long-term Exposure to ambient air pollutants with risk factors for cardiovascular disease in China. JAMA Netw Open. 2019;2(3):e190318. https://doi.org/10.1001/jamanetworkopen.2019.0318.
Shaffer Rachel M, et al. Improving and Expanding Estimates of the Global Burden of Disease Due to Environmental Health Risk Factors. Environmental Health Perspectives. 127(10):105001.
Kan H, London SJ, Chen G, Zhang Y, Song G, Zhao N, et al. Season, sex, age, and education as modifiers of the effects of outdoor air pollution on daily mortality in Shanghai, China: the public health and air pollution in Asia (PAPA) study. Environ Health Perspect. 2008;116(9):1183–8. https://doi.org/10.1289/ehp.10851.
Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40(3):804–18. https://doi.org/10.1093/ije/dyr029.
Lin H, Guo Y, Zheng Y, di Q, Liu T, Xiao J, et al. Long-term effects of ambient PM (2.5) on hypertension and blood pressure and attributable risk among older Chinese adults. Hypertension. 2017;69(5):806–12. https://doi.org/10.1161/HYPERTENSIONAHA.116.08839.
Liu C, Chen R, Zhao Y, Ma Z, Bi J, Liu Y, et al. Associations between ambient fine particulate air pollution and hypertension: a nationwide cross-sectional study in China. Sci Total Environ. 2017;584-585:869–74. https://doi.org/10.1016/j.scitotenv.2017.01.133.
Liu C, Yang C, Zhao Y, Ma Z, Bi J, Liu Y, et al. Associations between long-term exposure to ambient particulate air pollution and type 2 diabetes prevalence, blood glucose and glycosylated hemoglobin levels in China. Environ Int. 2016;92-93:416–21. https://doi.org/10.1016/j.envint.2016.03.028.
Yang Y, et al. Ambient fine particulate pollution associated with diabetes mellitus among the elderly aged 50 years and older in China. Environ Pollut. 2018;243(Pt B):815–23.
Zhang N, Yang X, Zhu X, Zhao B, Huang T, Ji Q. Type 2 diabetes mellitus unawareness, prevalence, trends and risk factors: National Health and nutrition examination survey (NHANES) 1999-2010. J Int Med Res. 2017;45(2):594–609. https://doi.org/10.1177/0300060517693178.
He J. Hypertension in China: a large and increasing public health challenge. J Hypertens. 2016;34(1):29–31. https://doi.org/10.1097/HJH.0000000000000818.
Gan W, Liu Y, Luo KH, Liang SS, Wang H, Li M, et al. The prevalence change of hyperlipidemia and hyperglycemia and the effectiveness of yearly physical examinations: an eight-year study in Southwest China. Lipids Health Dis. 2018;17(1):70. https://doi.org/10.1186/s12944-018-0724-6.
Wang Y, Pan L, Wan S, Yi H, Yang F, He H, et al. Increasing prevalence of overweight and obesity in Yi farmers and migrants from 2007 to 2015 in China: the Yi migrant study. BMC Public Health. 2018;18(1):659. https://doi.org/10.1186/s12889-018-5577-4.
Xu T, Zhu G, Liu J, Han S. Gender-specific prevalence and associated risk factors of high normal blood pressure and hypertension among multi-ethnic Chinese adolescents aged 8–18 years old. Blood Press. 2015;24(3):189–95. https://doi.org/10.3109/08037051.2015.1025474.
Wu, J., Qiu L., Cheng X.Q., Xu T., Wu W., Zeng X.J., Ye Y.C., Guo X.Z., Cheng Q., Liu Q., Liu L., Xu C.L., Zhu G.J., Hyperuricemia and clustering of cardiovascular risk factors in the Chinese adult population. Sci Rep, 2017. 7(1), 7, 1, DOI: https://doi.org/10.1038/s41598-017-05751-w.
Li, D.-D., Xu T., Cheng X.Q., Wu W., Ye Y.C., Guo X.Z., Cheng Q., Liu Q., Liu L., Zhu G.J., Wu J., Qiu L., Serum Gamma-Glutamyltransferase Levels are Associated with Cardiovascular Risk Factors in China: A Nationwide Population-Based Study. Sci Rep, 2018. 8(1), 8, 1, DOI: https://doi.org/10.1038/s41598-018-34913-7.
van Donkelaar A, Martin RV, Brauer M, Boys BL. Use of satellite observations for long-term exposure assessment of global concentrations of fine particulate matter. Environ Health Perspect. 2015;123(2):135–43. https://doi.org/10.1289/ehp.1408646.
van Donkelaar A, Martin RV, Li C, Burnett RT. Regional estimates of chemical composition of fine particulate matter using a combined geoscience-statistical method with information from satellites, models, and monitors. Environ Sci Technol. 2019;53(5):2595–611. https://doi.org/10.1021/acs.est.8b06392.
World Health Organization, O. and T. Environmental Health, WHO Air quality guidelines for particulate matter, ozone, nitrogen dioxide and sulfur dioxide : global update 2005 : summary of risk assessment. 2006, World Health Organization: Geneva.
Lao XQ, Guo C, Chang LY, Bo Y, Zhang Z, Chuang YC, et al. Long-term exposure to ambient fine particulate matter (PM (2.5)) and incident type 2 diabetes: a longitudinal cohort study. Diabetologia. 2019;62(5):759–69. https://doi.org/10.1007/s00125-019-4825-1.
Liang F, Yang X, Liu F, Li J, Xiao Q, Chen J, et al. Long-term exposure to ambient fine particulate matter and incidence of diabetes in China: a cohort study. Environ Int. 2019;126:568–75. https://doi.org/10.1016/j.envint.2019.02.069.
Li CY, et al. Association Between Long-term Exposure to PM2.5 and Incidence of Type 2 Diabetes in Taiwan: A National Retrospective Cohort Study. Epidemiology. 2019;30(Suppl 1):S67–s75.
Coogan PF, White LF, Jerrett M, Brook RD, Su JG, Seto E, et al. Air pollution and incidence of hypertension and diabetes mellitus in black women living in Los Angeles. Circulation. 2012;125(6):767–72. https://doi.org/10.1161/CIRCULATIONAHA.111.052753.
Park SK, Adar SD, O'Neill MS, Auchincloss AH, Szpiro A, Bertoni AG, et al. Long-term exposure to air pollution and type 2 diabetes mellitus in a multiethnic cohort. Am J Epidemiol. 2015;181(5):327–36. https://doi.org/10.1093/aje/kwu280.
Chen H, Burnett RT, Kwong JC, Villeneuve PJ, Goldberg MS, Brook RD, et al. Risk of incident diabetes in relation to long-term exposure to fine particulate matter in Ontario. Canada Environ Health Perspect. 2013;121(7):804–10. https://doi.org/10.1289/ehp.1205958.
Chen H, Burnett RT, Kwong JC, Villeneuve PJ, Goldberg MS, Brook RD, et al. Spatial association between ambient fine particulate matter and incident hypertension. Circulation. 2014;129(5):562–9. https://doi.org/10.1161/CIRCULATIONAHA.113.003532.
Lee S, Park H, Kim S, Lee EK, Lee J, Hong YS, et al. Fine particulate matter and incidence of metabolic syndrome in non-CVD patients: a nationwide population-based cohort study. Int J Hyg Environ Health. 2019;222(3):533–40. https://doi.org/10.1016/j.ijheh.2019.01.010.
Rotko T, et al. Sociodemographic descriptors of personal exposure to fine particles (PM2.5) in EXPOLIS Helsinki. J Expo Anal Environ Epidemiol. 2000;10(4):385–93. https://doi.org/10.1038/sj.jea.7500104.
Samal D, Greisenegger S, Auff E, Lang W, Lalouschek W. The relation between knowledge about hypertension and education in hospitalized patients with stroke in Vienna. Stroke. 2007;38(4):1304–8. https://doi.org/10.1161/01.STR.0000259733.43470.27.
Pickering T. Cardiovascular pathways: socioeconomic status and stress effects on hypertension and cardiovascular function. Ann N Y Acad Sci. 1999;896(1):262–77. https://doi.org/10.1111/j.1749-6632.1999.tb08121.x.
Weinmayr G, et al. Long-term exposure to fine particulate matter and incidence of type 2 diabetes mellitus in a cohort study: effects of total and traffic-specific air pollution. Environ Health. 2015;14(1):53. https://doi.org/10.1186/s12940-015-0031-x.
Strak M, Janssen N, Beelen R, Schmitz O, Karssenberg D, Houthuijs D, et al. Associations between lifestyle and air pollution exposure: potential for confounding in large administrative data cohorts. Environ Res. 2017;156:364–73. https://doi.org/10.1016/j.envres.2017.03.050.
Kim YJ. The long-run effect of education on obesity in the US. Econ Hum Biol. 2016;21:100–9. https://doi.org/10.1016/j.ehb.2015.12.003.
de Bont J, Casas M, Barrera-Gómez J, Cirach M, Rivas I, Valvi D, et al. Ambient air pollution and overweight and obesity in school-aged children in Barcelona. Spain Environ Int. 2019;125:58–64. https://doi.org/10.1016/j.envint.2019.01.048.
Yang BY, Qian Z, Howard SW, Vaughn MG, Fan SJ, Liu KK, et al. Global association between ambient air pollution and blood pressure: a systematic review and meta-analysis. Environ Pollut. 2018;235:576–88. https://doi.org/10.1016/j.envpol.2018.01.001.
He D, Wu S, Zhao H, Qiu H, Fu Y, Li X, et al. Association between particulate matter 2.5 and diabetes mellitus: a meta-analysis of cohort studies. J Diabetes Investig. 2017;8(5):687–96. https://doi.org/10.1111/jdi.12631.
Lewington S, Li L, Sherliker P, Guo Y, Millwood I, Bian Z, et al. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: the China Kadoorie biobank. J Hypertens. 2012;30(7):1383–91. https://doi.org/10.1097/HJH.0b013e32835465b5.
Su D, du H, Zhang X, Qian Y, Chen L, Chen Y, et al. Season and outdoor temperature in relation to detection and control of hypertension in a large rural Chinese population. Int J Epidemiol. 2014;43(6):1835–45. https://doi.org/10.1093/ije/dyu158.
Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362(12):1090–101. https://doi.org/10.1056/NEJMoa0908292.
Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE million persons project). Lancet. 2017;390(10112):2549–58. https://doi.org/10.1016/S0140-6736(17)32478-9.
Opoku S, Gan Y, Fu W, Chen D, Addo-Yobo E, Trofimovitch D, et al. Prevalence and risk factors for dyslipidemia among adults in rural and urban China: findings from the China National Stroke Screening and prevention project (CNSSPP). BMC Public Health. 2019;19(1):1500. https://doi.org/10.1186/s12889-019-7827-5.
Hu L, Huang X, You C, Li J, Hong K, Li P, et al. Prevalence of overweight, obesity, abdominal obesity and obesity-related risk factors in southern China. PLoS One. 2017;12(9):e0183934. https://doi.org/10.1371/journal.pone.0183934.
Wang Y, Pan L, Wan S, Yi H, Yang F, He H, et al. Association of socioeconomic status and overweight/obesity in rural-to-urban migrants: different effects by age at arrival. Front Public Health. 2020;8:622941. https://doi.org/10.3389/fpubh.2020.622941.
Miao J, Wu X. Urbanization, socioeconomic status and health disparity in China. Health Place. 2016;42:87–95. https://doi.org/10.1016/j.healthplace.2016.09.008.
Chuang KJ, Yan YH, Chiu SY, Cheng TJ. Long-term air pollution exposure and risk factors for cardiovascular diseases among the elderly in Taiwan. Occup Environ Med. 2011;68(1):64–8. https://doi.org/10.1136/oem.2009.052704.
Yang BY, Bloom MS, Markevych I, Qian Z(M), Vaughn MG, Cummings-Vaughn LA, et al. Exposure to ambient air pollution and blood lipids in adults: the 33 communities Chinese health study. Environ Int. 2018;119:485–92. https://doi.org/10.1016/j.envint.2018.07.016.
Kim JS, Chen Z, Alderete TL, Toledo-Corral C, Lurmann F, Berhane K, et al. Associations of AIR pollution, obesity and cardiometabolic health in young adults: the Meta-AIR study. Environ Int. 2019;133(Pt A):105180. https://doi.org/10.1016/j.envint.2019.105180.
Wang C, Wei D, Wang B, Zhang J, Zhang K, Ma M, et al. Effect of lifestyle on the prevalence of the metabolic syndrome among farmers, migrants with Yi ethnicity and Han population in Sichuan province of China. Asia Pac J Clin Nutr. 2010;19(2):266–73.
Ruixing Y, Fengping H, Shangling P, Dezhai Y, Weixiong L, Tangwei L, et al. Prevalence of hyperlipidemia and its risk factors for the middle-aged and elderly in the Guangxi Hei Yi Zhuang and Han populations. J Investig Med. 2006;54(4):191–200. https://doi.org/10.2310/6650.2006.05050.
Hamanaka RB, Mutlu GM. Particulate matter air pollution: effects on the cardiovascular system. Front Endocrinol (Lausanne). 2018;9:680. https://doi.org/10.3389/fendo.2018.00680.
Zhang T, et al. Exposure to PM2.5 affects blood lipid levels in asthmatic rats through notch signaling pathway. Lipids Health Dis. 2019;18(1):160.
Li R, et al. Sex-dependent effects of ambient PM2.5 pollution on insulin sensitivity and hepatic lipid metabolism in mice. Part Fibre Toxicol. 2020;17(1):14.
Acknowledgments
We thank Dr. Ziyad Al-Aly, the Director of the Clinical Epidemiology Center, and the Chief of Research and Education Service at Veterans Affairs St. Louis Health Care System, Washington University School of Medicine in St. Louis, for his helpful discussions and suggestions. Parts of this work were previously presented at American Society of Nephrology (ASN) kidney week 2020.
Funding
This work was partly supported by Key Research and Development Program of Ningxia Hui Autonomous Region (2018BFG02010 to C.L.); Special Fund for Key Basic Research Project of the Ministry of Science and Technology of China (2006FY110300 to Z.G.); the Capital Specialized Clinical Application Project (Z171100001017196 to C.L.); the Capital’s Funds for Health Improvement and Research (CFH, 2020–2-4018 to C. L, 2020–1-4014 to Q.L); Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (CIFMS 2016-I2M-2-004 to C.L.); National Natural Scientific Foundation, China (81970607, 81470937 to C.L.).
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Jianfeng Lin and Hua Zheng: Methodology, Formal analysis, Investigation, Writing - Original draft preparation. Peng Xia: Investigation, Formal analysis. Yang Li: Methodology, Formal analysis, Investigation. Yali Zheng: Investigation, Writing - Original draft preparation. Tao Xu and Guangjin Zhu: Investigation, Validation, Funding acquisition. Xinqi Cheng, Wei Wu, Chaochao Ma and Ling Qiu: Resources, Writing - Reviewing & Editing, Supervision, Funding acquisition. Limeng Chen: Conceptualization, Resources, Data Curation, Writing - Reviewing & Editing, Project administration, Funding acquisition.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was performed in accordance with the Helsinki Declaration and approved by the local Ethic Committee of Peking Union Medical College Hospital. Informed written consent has been obtained from our patients as specified in the ICMJE Reccomendations.
Consent for publication
Not applicable.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lin, J., Zheng, H., Xia, P. et al. Long-term ambient PM2.5 exposure associated with cardiovascular risk factors in Chinese less educated population. BMC Public Health 21, 2241 (2021). https://doi.org/10.1186/s12889-021-12163-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-021-12163-z