Abstract
Background
CD4 cell and viral load count are highly correlated surrogate markers of human immunodeficiency virus (HIV) disease progression. In modelling the progression of HIV, previous studies mostly dealt with either CD4 cell counts or viral load alone. In this work, both biomarkers are in included one model, in order to study possible factors that affect the intensities of immune deterioration, immune recovery and state-specific duration of HIV-infected women.
Methods
The data is from an ongoing prospective cohort study conducted among antiretroviral treatment (ART) naïve HIV-infected women in the province of KwaZulu-Natal, South Africa. Participants were enrolled in the acute HIV infection phase, then followed-up during chronic infection up to ART initiation. Full-parametric and semi-parametric Markov models were applied. Furthermore, the effect of the inclusion and exclusion viral load in the model was assessed.
Results
Inclusion of a viral load component improves the efficiency of the model. The analysis results showed that patients who reported a stable sexual partner, having a higher educational level, higher physical health score and having a high mononuclear component score are more likely to spend more time in a good HIV state (particularly normal disease state). Patients with TB co-infection, with anemia, having a high liver abnormality score and patients who reported many sexual partners, had a significant increase in the intensities of immunological deterioration transitions. On the other hand, having high weight, higher education level, higher quality of life score, having high RBC parameters, high granulocyte component scores and high mononuclear component scores, significantly increased the intensities of immunological recovery transitions.
Conclusion
Inclusion of both CD4 cell count based disease progression states and viral load, in the time-homogeneous Markov model, assisted in modeling the complete disease progression of HIV/AIDS. Higher quality of life (QoL) domain scores, good clinical characteristics, stable sexual partner and higher educational level were found to be predictive factors for transition and length of stay in sequential adversity of HIV/AIDS.
Similar content being viewed by others
Background
HIV infection is one of the leading causes of death from infectious diseases and remains a serious global public health issue [1, 2]. AIDS, the last progression stage of HIV infection, leads to severe damage of the body’s immune system [3]. The progression of HIV/AIDS is highly variable between populations and individuals and is determined by immunological, genetic, environmental and virological factors [4]. CD4 cell and viral load counts have remained the two strongest correlates and surrogate markers of HIV disease progression regularly used in the clinical setting to monitor the infection [5].
Although the main markers of HIV disease progression are both viral load and CD4 count, relatively few HIV/AIDS disease progression modelling studies include the longitudinal measurements of viral load biomarker along with clinical states of HIV/AIDS disease progression [6, 7]. This might be due to the unavailability of viral load data, particularly from middle and low-income countries, because of the higher costs of viral load testing [8]. Modelling of CD4 count progression, which takes into account the viral load biomarker, may better capturer the complete disease progression. Researchers further argue that modeling of disease progression of HIV/AIDS is important: to understand HIV pathogenesis and in the development of treatment strategies [9]; to refine the management of treatment-naive patients [10]; to determine at what threshold it is most clinically effective and less costly to begin ART [10]; to improve the empirical basis for epidemiological and prognostic models of the impact and cost-effectiveness of ART [11].
Modelling of disease progression of HIV/AIDS has been studied by several authors. Mangal [12] evaluated the effects of regional and age-specific differences on mortality and CD4+ cell progression of HIV/AIDS, using a hidden Markov model. Binquet et al. [13] estimated the impact of CD8 cell count, weight loss, drug use, gender, viral load and haemoglobin on the progression of HIV using multi-state Markov process. Oliveira et al. [14] studied the degrees of chronicity of HIV/AID using a multi-state process and went further to examine the impact of covariates; adherence, age and disease duration on CD4 cell count progression. Gillis et al. [15] further investigated the effects of age, gender, ethnicity, and people who had injected drugs, on the transitioning among the five viral load and CD4 cell counts based states. Recently, Shoko and Chikobvu [16] analyzed the effects of gender, TB co-infection, and age on transmission intensities, using the Markov model. Another study [17] in South Africa examined the effects of baseline viral load, gender, age and non-adherence to treatment on disease progression based on viral load followed by the death state using the Markov model. All these studies, however, did not model the length of stay in each state. In addition, although the factors related to disease progression of HIV are multiple and complex, no previous study directly examined the effects of several clinical variables (ie: white blood cell parameters, RBC parameters, blood chemistry parameters, and QOL domain scores) on both the length of stay and transitions of sequential events. This study thus gives a deeper insight on assessing the effect of several prognostic factors on both the transitions and length of stay of sequential adversity of HIV/AIDS.
In this study, full-parametric and semi-parametric multi-state Markov models are used to model the transitions and length of stay of sequential adverse events of HIV/AIDS. Multi-state Markov models are a powerful tool for studying chronic diseases and the factors associated with transitions between states of progression [14]. These models can accommodate competing risk factors, censored data, recurrent outcomes, multiple outcomes and frailty [18]. We classified the sequential adverse events by the degree of chronicity based on the CD4 counts (a marker for characterizing the clinical stages), with progression classes defined by patients going through normal, mild, advanced and severe clinical stages [19]. More importantly, we presented full and semi-parametric multi-state Markov models on both the length of stay and transitions between sequential states, thus making this research different from previous studies. In addition to that, among the determinants of the progression of HIV/AIDS, both the CD4 cell counts and viral load counts are included in the same model. As discussed by Chikobvu and Shoko [17], the effects of multi-collinearity on the CD4 cell count transitions can be corrected using the principal component approach.
Methods
Data description
The data is from an ongoing prospective cohort study conducted by the Centre for the AIDS Program of Research in South Africa (CAPRISA) among ART naïve HIV-infected women. The original study, CAPRISA_002, which started in 2004, enrolled a cohort of HIV uninfected women whose age was greater than 18 years with the aim to describe immunologic, clinical and virologic characteristics of HIV-1 disease [20]. The study enrollment was conducted from August 2004 to December 2017. A participant who seroconverted during the HIV uninfected stage of CAPRISA_002 and other CAPRISA prevention and seroincidences trials (including the CAPRISA_004 trials), were enrolled into the Acute HIV Infection phase, and then followed-up during chronic infection and up to ART initiation. Participants were recruited at two sites in KwaZulu-Natal-South Africa, a rural site in Vulindlela and an urban site in the city of Durban. Women without well documented estimated date of HIV infection, and those who did not have at least two follow-up clinical attribute measurements were excluded from our analyses. Finally, 219 participants were included in the study. Further information about the above mentioned ongoing prospective HIV cohort study (CAPRISA_002), including women eligibility criteria and the enrollment procedures were reported in [20,21,22].
Variables and measurements
CAPRISA initially enrolled HIV-negative (phase I) women into different study cohorts. The women who seroconverted were enrolled into the acute infection phase (i.e. phase II: weekly visits up to 3 months post-infection), early infection phase (i.e. phase III: monthly visits from 3 to 12 months), established infection phase (i.e. phase IV: quarterly visits for more than 12 months) and on ART phase (i.e. phase V). Samples for immunological, virological and clinical attributes (such as viral load, WBC parameters, RBC parameters, blood chemistry parameters, CD4 cell count, etc.) were measured at each visit [23]. These longitudinal immunologic, virologic and clinical measurements, were recorded for several followed-up visits. There was a total of 8760 follow-up visits recorded from 219 HIV infected women. Of these patients, 9.2% of them were co-infected with TB and all were black females, with a median age of 25 years (Interquartile range, IQR, 22–30). Over half (69.9%) reported having completed grades 11/12 of schooling. The median baseline CD4 count of the participants included in the analysis was 519.0 cells/mm3 (IQR 419–655.5 cells/mm3). The VL count of the participants ranged from 1.47 log10 copies/ml to 6.81 log10 copies/ml with the first quartile of 3.56 log10 copies/ml, a median of 4.23 log10 copies/ml and the third quartile of 4.79 log10 copies/ml.
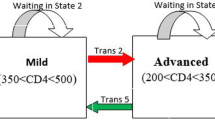
The main outcome variables in this current paper are immune deterioration, immune recovery and state-specific duration of stay of HIV-infected women. During the follow-up period, a patient could go through several states defined as normal, mild, advanced and severe disease states (See Fig. 1). The World Health Organization immunological classifications were used to assess the degree of severity of HIV infection of patients in the study. These HIV infection states are: no adverse events (normal) (CD4≥ 500), mild (350≤CD4≤499), advanced (200≤CD4≤349) and severe (CD4 < 200) [19].
The effect of numerous possible factors on the intensities of immune deterioration, immune recovery and state-specific duration of stay of HIV-infected women, were evaluated including, (1) demographic variables, (2) risk variables, (3) past opportunistic illness/infections and (4) clinical attributes and (5) health-related quality of life domain scores (HR-QoL). The WHO QoL instrument [24], was used to measure the HR-QoL of the participants. Therefore, the HR-QoL scales contain the following four domains score. The first domain is the physical health scores, that measure the impact of the disease on the activities of daily living, dependence on therapeutic substances, presence of pain, fatigue, lack of energy and initiative and perceived working capacity. The second is the psychological wellbeing score domain, that assesses the patient’s thoughts about body appearance, positive and negative feelings, self-esteem and personal beliefs, higher cognitive functions, spirituality, anxiety, suicide and depression. The third is the social relationships domain, which assesses personal relationships, social contacts, social support and sexual activity. The fourth domain is devoted to the level of independence and assesses areas such as mobility, activities of daily living, dependence on treatments and work capacity (See Fig. 2).
Statistical method
Factor analysis
Since our data have a large number of clinical variables, we used exploratory factor analysis in order to group and minimize the number of variables. Accordingly from the 24 clinical variables in the study, we managed to group them in order to create 9 latent variables, defined as granulocytes components, mononuclear components, eosinophils component, RBC component, red blood cell indices, liver abnormality component, electrolyte component, lipid component and protein component. (See Table 1).
Multi-state Markov modelling
Let a Markov chain process {S(t), t ∈ T}, T = [0, τ] for τ < ∞, that has finite space, denoted by E = {1, 2, 3, 4}, be a representation of the transition process, where for each patient, a multi-state process is observed. This Markov chain process has an initial probability, denoted by P(S(0) = m), m ∈ E, which evolves over time and with a history (HE), which contains the states previously visited, durations and times of transitions [25, 26]. The transition probability of the individual being in state j at time t, given that the individual was in state m at time z, is defined by
The corresponding transition intensity is defined by
Where \( {\sum}_{j\in E}{h}_{mj}(t)=0 \) and \( {h}_{mm}(t)=-{\sum}_{m\ne j}{h}_{mj}(t) \). It is worth noting that the transition probabilities depend only on the elapsed time, not on the times since the baseline of the study.
Besides modeling the ordinal transitional state of the CD4 progression, our object is to examine the effect of covariates or risk factors namely the education, marital status, age, sex under the influence of alcohol, TB-co infection status, anemia status, white blood cell parameters, RBC parameters, HR-QoL domain scores and weight on such transitions. We denote this set of covariates by X.
We employ both fully-parametric and semi-parametric multi-state models in our analysis. In both model types
where. \( {h}_{mj}^0(t) \) represents the baseline intensity from state m to state j and Xmj representing a set of covariates, while αmj is the effect of the covariates on the hazard intensity hmj. The transition m to j is defined as immunological deterioration if m < j, as immunological recovery if m > j; as the probability of staying in the same diseasing state if m = j. In other words, the state labeling is 1 for normal, 2 for mild, 3 for advanced and 4 for severe states (See Fig. 1).
In the semi-parametric case, the log-linear effect of the covariates, αmj are estimated by the maximum partial likelihood and the corresponding baseline intensity, \( {h}_{mj}^0(t) \), is left unspecified and estimated non-parametrically, similar to the Cox (1972) model.
In the fully-parametric cases, the baseline intensity, \( {h}_{mj}^0(t) \), is given by a fully-parametric function of time, so that each transition-specific model is a standard parametric survival model. The log-linear effect of the covariates, αmj, are estimated by full maximum likelihood and standard errors are obtained by standard asymptotic theory. In the current study, we used different parametric and semi-parametric models including the Exponential distribution and Weibull distribution.
Principal component analysis
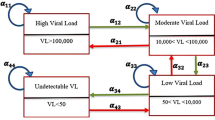
Principal component analysis (PCA) is a statistical procedure that uses an orthogonal transformation to convert a set of observations, of possibly correlated variables, into a set of values of linearly uncorrelated variables. In this paper, a principal component variable is created by fitting a regression model of log10-transformed viral load values (yi) on CD4 cell counts (xi) to improve the efficiency of the model above. In order to create two new uncorrelated components, as explained by Chikobvu and Shoko [17], we carried out regression analysis to estimate the intercept (β0) and slope (β1) parameters in the model: yi = β0 + β1xi+εi. We then define a viral load orthogonal variable (VLO)= εi= yi − (β0 + β1xi).
VLO in the model explains the component of disease progression of HIV/AIDS that cannot be explained by the CD4 counts alone. In order to deal with multicollinearity of CD4 cell count and viral load count, the orthogonal viral load component was used. The residual from the fitted model was included with the original HIV/AIDS data to form the new viral load component.
Model diagnostics
The estimates of full and semi-parametric multi-state models were compared with non-parametric estimates to assess model fit (as discussed by Ieva et al. [27] and Titman and Sharples [28]). Besides selecting the best fit model for our data, the effect of CD4 count with viral load adjustment on the HIV/AIDS disease progression was also analyzed. This was done by fitting a multi-state model for the effects of possible factors (education, marital status, TB-co infection status, anemic status, age, sex under the influence of alcohol, white blood cell parameters, RBC parameters, HR-QoL domain scores, and weight) on disease progression of HIV/AIDS, based on CD4 count. Notably, we excluded the orthogonal viral load component in the first model. In the second model, viral load component was included in the modified first model. A comparison of these two models was based on their likelihood ratio test (LRT) and Akaike information criteria (AIC).
All of the analyses were implemented using R-3.6.2 (https://cran.r-project.org/bin/windows/base/) flexsurv, survival and mstate packages in order to fit fully-parametric Markov, Semi-parametric Markov and to estimate the nonparametric Aalen-Johansen model, respectively. For visual graphical presentation of the estimates proc. SGPLOT in SAS 9.4 (https://www.sas.com/en_us/software/sas9.html) was used.
Results
Estimated transition probability and length of stay
The plot in Fig. 3 displays the non-parametric Aalen-Johansen estimator of the transition and waiting probabilities. As expected, the probability of transition from severe to advanced states of the diseases did not increase much throughout follow-up, while the transition probability from advanced to severe disease states of the patients increased with increasing years since enrollment. The plots further clearly demonstrate that the overall probability of staying in the same diseasing state had decreased throughout the follow-up periods. Patients with lower CD4 count (particularly those in the severe disease state) had a higher probability of staying in the same state throughout follow-up periods, compared to those with higher CD4 cells counts. (See Fig. 3).
Model assessment
We applied three Markov multi-state models, including Exponential, Weibull and the Semi-parametric multi-state model. The overall goodness of fit of the models is presented in Fig. 4, which shows the estimates of full and semi-parametric models to be overlaid on the nonparametric Aalen-Johansen estimates. As seen from this plot, we noted that the Weibull model accounted for the decrease in the hazard of waiting and transition probability better compared to the Exponential and the Sem-parametric models. The model selection criteria in Table 2 also confirmed this finding.
The AIC and LRT from Table 3 showed that the model defined by CD4 cell counts states with the viral load orthogonal adjustment gives the best fit to the data (ie. improve the efficiency of the model). (See Table 3).
Predictors of immune deterioration and immune recovery
The results in Table 4 show that after adjusting for other covariates in the model, an increase in Hb and haematocrit component increases the intensities of transition from mild to normal disease state (aHR = 1.12; 95% CI: 1.01–1.25). Similarly, after adjusting other covariates, an increase in RBC indices score increases the intensities of transition from mild to normal disease state (aHR = 1.16; 95% CI: 1.04–1.30). The result further showed that patients with high mononuclear component scores, significantly reduced immune deterioration from normal to mild (aHR = 0.77; 95% CI: 0.67–0.88), mild to advanced (aHR = 0.63; 95% CI: 0.55–0.73) and advanced to severe (aHR = 0.64; 95% CI: 0.50–0.83) disease state. Moreover, an increase in granulocytes component scores reduces the intensities of immune deterioration transitions.
After adjusting for other covariates in the model, an increase in liver abnormality score reduces the intensities of transition from advanced to mild disease state (aHR = 0.86; 95% CI: 0.76–0.98). Anemic patients had also significantly increased the intensity of immune deterioration from mild to advanced disease state (aHR = 1.31; 95% CI: 1.04–1.66) as compared to non-anemic patients. The result further showed that having TB co-infection significantly accelerates the transition time from normal to mild (aHR = 2.08; 95% CI: 1.02–4.71) and advance to severe (aHR = 1.86; 95% CI: 1.05–4.61) disease stages, compared to those without TB co-infection. (See Table 4).
With regard to HR-QoL variables, patients with high physical health scores significantly increased the intensities of immunological recovery from severe to advanced (aHR = 1.25; 95%CI: 1.01–1.58) and mild to normal disease state (aHR = 1.17; 95% CI: 1.07–1.29). Similarly, an increase in level of independence score reduces the intensities of transition from normal to mild (aHR = 0.87; 95% CI: 0.83–0.91) and advanced to severe disease state (aHR = 0.94; 95% CI: 0.88–0.99). Furthermore, having high psychological well-being scores, is significantly associated with reduced intensities of transitions from normal to mild (aHR = 0.83; 95% CI: 0.76–0.91) and mild to advanced (aHR = 0.91; 95% CI: 0.82–0.99) disease state (See Table 4).
With regard to socio-demographic variables, patients with higher educational levels (grade > 11) had statistically significantly reduced intensities of transitions from normal to mild (aHR = 0.44; 95% CI: 0.25–0.77), mild to advanced (aHR = 0.51; 95% CI: 0.29–0.87) and advanced to severe (aHR = 0.41; 95% CI: 0.23–0.73) disease state, as compared to those with low level of education (grade < 8). Patients who reported stable sexual partners (aHR = 1.31; 95% CI: 1.01–4.92) and no sexual partner (aHR = 1.27; 95% CI: 1.01–2.70), had significantly increased immune recovery, from severe to advanced disease state, as compared to those who reported many sexual partners. Furthermore, as the weight of women in the study increased, the intensities of immune deterioration from normal to mild and mild to advanced disease state, decreased (See Table 4).
Predictors of state-specific duration of stay of HIV patients
After adjusting for education, marital status, TB-co infection, anemic status, age, sex while drunk, granulocytes component, RBC indices, HR-QoL domain scores, and weight, an increase in mononuclear component score increases the likelihood that a patient stayed in normal disease state (aHR = 1.27; 95% CI: 1.18–1.38) and mild disease state (aHR = 1.12; 95% CI: 1.04–1.21), (Table 5). The result further showed that patients with higher physical health scores were more likely to stay longer in normal (aHR = 1.07; 95% CI: 1.01–1.14) and mild disease state (aHR = 1.12; 95% CI: 1.05–1.21), but significantly reduced the waiting time in a severe disease state (aHR = 0.85; 95% CI: 0.73–0.99). Similarly, we noted that those having high psychological well-being scores and high social relationship scores were less likely to stay longer in severe disease state. (See Table 5).
After adjusting for education, marital status, TB-co infection, anemic status, age, sex while drunk, granulocytes component, RBC indices, HR-QoL domain scores, and weight, patients who reported stable sexual partnership (aHR = 1.51; 95% CI: 1.01–2.25) and no sexual partner (aHR = 1.71; 95% CI: 1.14–2.78) were more likely to stay longer in a normal disease state as compared to those who reported many sexual partners. Furthermore, patients with higher educational levels (grade > 11) were more likely to stay longer in the normal disease state (aHR = 4.80; 95% CI: 2.02–11.40), as compared to those with lower education (< 8 grade). (See Table 5).
Discussion
We have presented both full-parametric and semi-parametric multi-state models, to model the transition intensity and length of stay of sequential adverse events of HIV/AIDS. We also improved the selected model, the Weibull multi-state model, by including an orthogonal viral load component, derived from PCA. The new orthogonal viral load component helped to explain the determinants of transitions and length of stay in sequential adverse events, which could not be explained by the CD4 count alone. This further improved the efficiency and predictive accuracy of the model. Results from the Akaike information criteria and likelihood ratio test showed that the model defined by CD4 cell counts states with the viral load orthogonal component, fitted significantly better than the model with the exclusion of orthogonal viral load components, as it was done by [17, 29].
Among the different hematological parameters for HIV infected patients, as expected, a latent variable related to basophils counts and total lymphocytes was significantly associated with the intensities of immunological deterioration transitions, and this confirms that HIV infection targets T-cells. Many studies also suggested that total lymphocytes can adequately serve as a surrogate biomarker for predicting CD4 count progression [30,31,32]. The latent variable related to RBC indices was significantly associated with CD4 count progression, which is in agreement with findings reported in previous studies [33,34,35]. The RBC indices result also shows that it could be used as a reliable marker of the prognosis in HIV- patient and that a therapeutic approach is imperative for a patient with anemia. Thus, hematological parameters such as basophils counts, total lymphocytes and red blood cell indices (i.e. MCV and MCH) could thus help health workers identify patients with poor immunological and clinical responses in the absence of CD4 count. Furthermore, the latent variable related to alanine aminotransferase and aspartate aminotransferase was significantly associated with the intensities of immunological deterioration transitions, and this confirms that the infection is the underlying cause of the increased activities of liver enzymes [36, 37]. A study in Ethiopia also reported similar findings [38], showing that lower CD4 count level (CD4 < 200 cells/mm3) was associated with elevated liver enzymes. Thus, there is a need to monitor alanine aminotransferase and aspartate aminotransferase levels before initiation of ART mainly in high-risk patients to reduce side effect concerns.
We found that hematological abnormalities such as anemia had a significantly accelerated immune deterioration effect. This may be attributed to the fact that anemia is commonly due to the under-production of erythrocytes by the bone marrow cells [39]. The bone marrow cells are also responsible for the production of CD4 cell counts through the myeloid cells [40]. Poor production of myeloid cells can, therefore, result in decreased production of both erythrocytes and CD4 cells. A study done in Ethiopia [41] reported similar findings that having low CD4+ T cells count level (<200cells/mm3) and being HAART-naïve, were significantly associated with anemia. Other researchers [42,43,44] further reported that more severe levels of anemia are found among HIV positive patients presenting with low CD4 count level.
We observed that TB co-infection accelerated the deterioration of immunological functions, a finding that is in accordance with the literature [45,46,47,48], where TB co-infection has a negative impact on the immune response to HIV, accelerating the progression from HIV infection to AIDS. Consequently, caution is needed for risk assessment measures to monitor and screen patient’s pre-ART initiation in African clinical settings, to curtail potential risks associated with an increased probability of accelerating the deterioration of immunological functions. Furthermore, in agreement with the world health organization treatment guidelines [49], which recommends ART in all PLHIV regardless of CD4 cell count, early identification of patients with poor clinical characteristics and initiation of treatment will improve programmatic success and treatment prognosis.
HIV patients who reported many sexual partners had significantly increased intensities of immune deterioration transitions. Moreover, patients who reported stable or no sexual partners were more likely to spend a long time in a normal disease state, as compared to those who reported many sexual partners. Indeed it has been reported [50] that patients with higher sexual risk-taking behaviors (such as many sexual partners) were significantly linked to depression, physically and psychologically impairment among patients living with HIV. Chronic depression and low quality of life scores may be associated with increased probability of experiencing immunological deterioration [51, 52], showing that at least part of the effect of many sexual partners on incomplete immunological recovery, is mediated through QoL and depression.
Patients with higher educational levels had significantly reduced rates of immune deterioration. Other researchers [53, 54] also found that higher education promotes a better rate of change of immune recovery, possibly due to better knowledge about their treatment and disease, access to health services, or functional status. We have also observed that patients having higher educational levels were significantly associated with longer time spent in normal disease states. This might be attributed to patients having higher educational levels were significantly associated with good sanitation and hygiene practices [55]. Good sanitation and hygiene practices decrease the risk of diarrhea, which can increase CD4 count [56]. This shows the effect of educational level on the time spent in healthier states (particularly the normal disease state), is mediated through good sanitation and hygiene practices. Another possibility may be that higher educational level often provides financial benefits and thus better access to nutritious food. This may be attributed to the fact that nutritious food significantly increases the time spent in healthier states.
Having high body weight significantly reduces the intensities of immunological deterioration transitions. This finding is consistent with higher weight was significantly related to higher CD4 cell count levels [57, 58]. Recent studies have also shown that patients with higher BMI at pre-HAART possess higher CD4 cell count and CD4/CD8 ratio compared to normal or underweight adults [59, 60].
A significant positive relationship between QoL domain scores and intensities of recovery of HIV infected patients is noted in our study. Previous studies [61,62,63] had reported a significant positive relationship between CD4 cell count recovery and HR-QoL scores of HIV infected patients. In contrast, studies [64, 65] from sub-Saharan Africa showed that there was no significant relationship between CD4 count level and HR-QoL scores. Possible explanations for this controversial finding might be that our data was from a cohort of acutely infected patients and followed up repeatedly over an extended ART-free period. We have also observed that patients having higher physical health scores were significantly associated with longer time spent in normal disease states. This may explain the observed positive progression in the physical health domain score and the CD4 cell counts. Furthermore, having high mononuclear component scores were significantly associated with longer time spent in normal disease states.
This study has some limitations, including missing data, which are expected for a study conducted on data collected from patients’ files with many variables and a long term follow-up period. Moreover, some clinical covariates that influence the intensities of immune deterioration and immune recovery, may not have been included, for example, CD4/CD8 ratio and hepatitis status. Furthermore, the study findings were limited to adult females.
Conclusions
From a clinical perspective, the study has revealed that having higher QoL domain scores, good clinical characteristics, stable sexual partners and higher educational levels, were found to be the significant predictive factors for intensities of immune deterioration, immune recovery and state-specific length of stay of HIV-infected women. Furthermore, we found that the identification of factors, such as QoL measurement items, clinical attributes, marital status, and educational status, associated with the current state of the patient, were important contributing factors to extend the survival of the patients and could potentially guide clinical interventions.
From a methodological perspective, by treating the collinearity of the viral load and CD4 cell counts using orthogonal; transformation, the Weibull multi-state Markov model gives a better fit and insight than the semi-parametric methods. Moreover, our study will help researchers to uncover the critical areas of correcting and dealing with multicollinearity when including both CD4 cell and viral load count in parametric multi-state modelling of HIV/AIDS, that many researchers have not been able to explore. Other more robust parametric distributions other than the Weibull are also a possible area of further research.
Availability of data and materials
The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- AIDS :
-
Acquired Immune Deficiency Syndrome
- HB:
-
Hemoglobin
- V B12:
-
Vitamin B12
- BP:
-
Blood pressure
- LDH:
-
Lactate dehydrogenase
- PR:
-
Pulse rate
- RBC:
-
Red blood cells
- HR-QoL:
-
Health-related quality of life
- CAPRISA:
-
Center of the AIDS Programme of Research in South Africa
- OI:
-
Opportunistic infections
- ARV :
-
Antiretroviral (drug)
- ART:
-
Antiretroviral therapy
- HIV:
-
Human immunodeficiency virus
- MCHC:
-
Mean corpuscular haemoglobin concentration
- MCV:
-
Mean corpuscular volume
- MCH:
-
Mean corpuscular haemoglobin
- RDW:
-
Red cell distribution width
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
References
Moraga P, Collaborators GCoD. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–210.
World Health Organization (WHO). Global Health Estimates 2016: Disease burden by cause, age, sex, by country and by region, 2000–2016. Geneva, Switzerland: WHO; 2018.
Hare CB. HIV InSite Knowledge Base Chapter-January. In: Clinical overview of HIV disease; 2006.
Haynes BF, Pantaleo G, Fauci AS. Toward an understanding of the correlates of protective immunity to HIV infection. Science. 1996;271(5247):324–8.
Maartens G, Celum C, Lewin SR. HIV infection: epidemiology, pathogenesis, treatment, and prevention. Lancet. 2014;384(9939):258–71.
Case KK, Ghys PD, Gouws E, Eaton JW, Borquez A, Stover J, Cuchi P, Abu-Raddad LJ, Garnett GP, Hallett TB. Understanding the modes of transmission model of new HIV infection and its use in prevention planning. Bull World Health Organ. 2012;90:831–838A.
Herbeck JT, Mittler JE, Gottlieb GS, Mullins JI. An HIV epidemic model based on viral load dynamics: value in assessing empirical trends in HIV virulence and community viral load. PLoS Comput Biol. 2014;10(6):e1003673.
Lecher S. Progress with scale-up of HIV viral load monitoring—seven sub-Saharan African countries, January 2015–June 2016. MMWR Morb Mortal Wkly Rep. 2016;65:1332–5.
Sabin CA, Mocroft A, Cozzi Lepri A, Phillips AN. Cofactors and markers of disease progression in human immunodeficiency virus infection. J R Stat Soc. 1998;161(2):177–89.
Organization WH. Antiretroviral therapy for HIV infection in adults and adolescents: recommendations for a public health approach-2010 revision. 2010.
Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373(9657):48–57.
Mangal TD. Joint estimation of CD4+ cell progression and survival in untreated individuals with HIV-1 infection. AIDS (London, England). 2017;31(8):1073.
Binquet C, Le Teuff G, Abrahamovicz M, Mahboubi A, Yazdanpanah Y, Rey D, Rabaud C, Chirouze C, Berger J, Faller J. Markov modelling of HIV infection evolution in the HAART era. Epidemiol Infect. 2009;137(9):1272–82.
RdVCd O, Shimakura SE, Campos DP, Victoriano FP, Ribeiro SR, Veloso VG, Grinsztejn B, Carvalho MS. Multi-state models for defining degrees of chronicity related to HIV-infected patient therapy adherence. Cad Saude Publica. 2013;29:801–11.
Gillis J, Loutfy M, Bayoumi AM, Antoniou T, Burchell AN, Walmsley S, Cooper C, Klein MB, Machouf N, Montaner JS. A multi-state model examining patterns of transitioning among states of engagement in care in HIV-positive individuals initiating combination antiretroviral therapy. J Acquir Immune Defic Syndr (1999). 2016;73(5):531.
Shoko C, Chikobvu D. Time-homogeneous Markov process for HIV/AIDS progression under a combination treatment therapy: cohort study, South Africa. Theor Biol Med Model. 2018;15(1):3.
Chikobvu D, Shoko C. A Markov model to estimate mortality due to HIV/AIDS using CD4 cell counts based states and viral load: a principal component analysis approach. Biomed Res. 2018;29(15):3090–8.
Abner EL, Nelson PT, Schmitt FA, Browning SR, Fardo DW, Wan L, Jicha GA, Cooper GE, Smith CD, Caban-Holt AM. Self-reported head injury and risk of late-life impairment and AD pathology in an AD center cohort. Dement Geriatr Cogn Disord. 2014;37(5–6):294–306.
Organization WH. WHO case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and children. 2007.
van Loggerenberg F, Mlisana K, Williamson C, Auld SC, Morris L, Gray CM, Karim QA, Grobler A, Barnabas N, Iriogbe I. Establishing a cohort at high risk of HIV infection in South Africa: challenges and experiences of the CAPRISA 002 acute infection study. PLoS One. 2008;3(4):e1954.
Garrett N, Norman E, Leask K, Naicker N, Asari V, Majola N, Karim QA, Karim SSA. Acceptability of early antiretroviral therapy among South African women. AIDS Behav. 2018;22(3):1018–24.
Karim QA, Karim SSA, Frohlich JA, Grobler AC, Baxter C, Mansoor LE, Kharsany AB, Sibeko S, Mlisana KP, Omar Z. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329(5996):1168–74.
Mlisana K, Werner L, Garrett NJ, McKinnon LR, van Loggerenberg F, Passmore J-AS, Gray CM, Morris L, Williamson C, Abdool Karim SS. Rapid Disease Progression in HIV-1 Subtype C–Infected South African Women. Clin Infect Dis. 2014;59(9):1322–31.
WHOQoL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28(3):551–8.
Hamidi O, Tapak L, Poorolajal J, Amini P. Identifying risk factors for progression to AIDS and mortality post-HIV infection using illness-death multistate model. Clin Epidemiol Glob Health. 2017;5(4):163–8.
Beyersmann J, Latouche A, Buchholz A, Schumacher M. Simulating competing risks data in survival analysis. Stat Med. 2009;28(6):956–71.
Ieva F, Jackson CH, Sharples LD. Multi-State modelling of repeated hospitalisation and death in patients with Heart Failure: the use of large administrative databases in clinical epidemiology. Stat Methods Med Res. 2017;26(3):1350–72.
Titman AC, Sharples LD. Model diagnostics for multi-state models. Stat Methods Med Res. 2010;19(6):621–51.
Shoko C, Chikobvu D, Bessong PO. A Markov Model to Estimate Mortality Due to HIV/AIDS Using Viral Load Levels-Based States and CD4 Cell Counts: A Principal Component Analysis Approach. Infect Dis Ther. 2018;7(4):457–71.
Kwantwi LB, Tunu BK, Boateng D, Quansah DY. Body mass index, haemoglobin, and total lymphocyte count as a surrogate for CD4 count in resource limited settings. J biomark. 2017;2017:7907352.
Obirikorang C, Quaye L, Acheampong I. Total lymphocyte count as a surrogate marker for CD4 count in resource-limited settings. BMC Infect Dis. 2012;12(1):128.
Tinarwo P, Zewotir T, Yende-Zuma N, Garrett NJ, North D. An Evaluation to Determine the Strongest CD4 Count Covariates during HIV Disease Progression in Women in South Africa. Infect Dis Ther. 2019;8(2):269–84.
De Santis GC, Brunetta DM, Vilar FC, Brandao RA, de Albernaz Muniz RZ, de Lima GMN, Amorelli-Chacel ME, Covas DT, Machado AA. Hematological abnormalities in HIV-infected patients. Int J Infect Dis. 2011;15(12):e808–11.
Obirikorang C, Yeboah FA. Blood haemoglobin measurement as a predictive indicator for the progression of HIV/AIDS in resource-limited setting. J Biomed Sci. 2009;16(1):102.
Vanisri H, Vadiraja N. Relationship between Red blood cell parameters and immune status in HIV infected females. Indian J Pathol Oncol. 2016;3(2):255–9.
Nagu T, Kanyangarara M, Hawkins C, Hertmark E, Chalamila G, Spiegelman D, Mugusi F, Fawzi W. Elevated alanine aminotransferase in antiretroviral-naïve HIV-infected African patients: magnitude and risk factors. HIV Med. 2012;13(9):541–8.
Quaye O, Kuleape JA, Bonney EY, Puplampu P, Tagoe EA. Imbalance of antioxidant enzymes activities and trace elements levels in Ghanaian HIV-infected patients. PLoS One. 2019;14(7):e0220181.
Shiferaw MB, Tulu KT, Zegeye AM, Wubante AA. Liver enzymes abnormalities among highly active antiretroviral therapy experienced and HAART naïve HIV-1 infected patients at Debre Tabor Hospital, North West Ethiopia: a comparative cross-sectional study. AIDS Res Treat. 2016;2016:1985452.
Moore RD, Forney D. Anemia in HIV-infected patients receiving highly active antiretroviral therapy. J Acquir Immune Defic Syndr (1999). 2002;29(1):54–7.
Calles, NR, Evans, D, Terlonge, D. Pathophysiology of the human immunodeficiency virus. In: HIV Curriculum for the Health Professional. Houston, TX: Baylor International Pediatric AIDS Initiative, Baylor College of Medicine; 2006:11–22.
Deressa T, Damtie D, Workineh M, Genetu M, Melku M. Anemia and thrombocytopenia in the cohort of HIV-infected adults in Northwest Ethiopia: a facility-based cross-sectional study. EJIFCC. 2018;29(1):36.
Volberding PA, Levine AM, Dieterich D, Mildvan D, Mitsuyasu R, Saag M, Group AiHW. Anemia in HIV infection: clinical impact and evidence-based management strategies. Clin Infect Dis. 2004;38(10):1454–63.
Parinitha S, Kulkarni M. Haematological changes in HIV infection with correlation to CD4 cell count. Australas Med J. 2012;5(3):157.
Ferede G, Wondimeneh Y. Prevalence and related factors of anemia in HAART-naive HIV positive patients at Gondar University Hospital, Northwest Ethiopia. BMC Blood Disord. 2013;13(1):8.
Pawlowski A, Jansson M, Sköld M, Rottenberg ME, Källenius G. Tuberculosis and HIV co-infection. PLoS Pathog. 2012;8(2):e1002464.
Siika AM, Yiannoutsos CT, Wools-Kaloustian KK, Musick BS, Mwangi AW, Diero LO, Kimaiyo SN, Tierney WM, Carter JE. Active tuberculosis is associated with worse clinical outcomes in HIV-infected African patients on antiretroviral therapy. PLoS One. 2013;8(1):e53022.
Skogmar S, Schön T, Balcha TT, Jemal ZH, Tibesso G, Björk J, Björkman P. CD4 cell levels during treatment for tuberculosis (TB) in Ethiopian adults and clinical markers associated with CD4 lymphocytopenia. PLoS One. 2013;8(12):e83270.
Cingolani A, Cozzi Lepri A, Castagna A, Goletti D, De Luca A, Scarpellini P, Fanti I, Antinori A, d'Arminio Monforte A, Girardi E. Impaired CD4 T-cell count response to combined antiretroviral therapy in antiretroviral-naive HIV-infected patients presenting with tuberculosis as AIDS-defining condition. Clin Infect Dis. 2011;54(6):853–61.
World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. 2nd ed. Geneva, Switzerland: WHO; 2016.
Vu T, Boggiano V, Tran B, Nguyen L, Tran T, Latkin C, Ho C, Ho R. Sexual risk behaviors of patients with HIV/AIDS over the course of antiretroviral treatment in Northern Vietnam. Int J Environ Res Public Health. 2018;15(6):1106.
Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schuman P, Boland RJ, Moore J, Group HERS. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. JAMA. 2001;285(11):1466–74.
Rivera-Rivera Y, Vazquez-Santiago FJ, Albino E, Sanchez MD, Rivera-Amill V. Impact of depression and inflammation on the progression of HIV disease. J Clin Cell Immunol. 2016;7(3):423.
Seyoum A, Temesgen Z. Joint longitudinal data analysis in detecting determinants of CD4 cell count change and adherence to highly active antiretroviral therapy at Felege Hiwot Teaching and Specialized Hospital, North-west Ethiopia (Amhara Region). AIDS Res Ther. 2017;14(1):14.
Jiang H, Xie N, Cao B, Tan L, Fan Y, Zhang F, Yao Z, Liu L, Nie S. Determinants of progression to AIDS and death following HIV diagnosis: a retrospective cohort study in Wuhan, China. PLoS One. 2013;8(12):e83078.
Yallew WW, Terefe MW, Herchline TE, Sharma HR, Bitew BD, Kifle MW, Tetemke DM, Tefera MA, Adane MM. Assessment of water, sanitation, and hygiene practice and associated factors among people living with HIV/AIDS home based care services in Gondar city, Ethiopia. BMC Public Health. 2012;12(1):1057.
Yates T, Lantagne D, Mintz E, Quick R. The impact of water, sanitation, and hygiene interventions on the health and well-being of people living with HIV: a systematic review. J Acquir Immune Defic Syndr. 2015;68:S318–30.
Crum-Cianflone NF, Roediger M, Eberly LE, Ganesan A, Weintrob A, Johnson E, Agan BK, Group IDCRPHW. Impact of weight on immune cell counts among HIV-infected persons. Clin Vaccine Immunol. 2011;18(6):940–6.
Shuter J, Chang CJ, Klein RS. Prevalence and predictive value of overweight in an urban HIV care clinic. J Acquir Immune Defic Syndr (1999). 2001;26(3):291–7.
Li X, Ding H, Geng W, Liu J, Jiang Y, Xu J, Zhang Z, Shang H. Predictive effects of body mass index on immune reconstitution among HIV-infected HAART users in China. BMC Infect Dis. 2019;19(1):373.
Womack J, Tien PC, Feldman J, Shin JH, Fennie K, Anastos K, Cohen MH, Bacon MC, Minkoff H. Obesity and immune cell counts in women. Metabolism. 2007;56(7):998–1004.
Weinfurt KP, Willke RJ, Glick HA, Freimuth WW, Schulman KA. Relationship between CD4 count, viral burden, and quality of life over time in HIV-1-infected patients. Med Care. 2000;38(4):404–10.
Venter E, Gerike G, Bekker P. Nutritional status, quality of life and CD4 cell count of adults living with HIV/AIDS in the Ga-Rankuwa area (South Africa). S Afr J Clin Nutr. 2009;22(3):124–9.
Call S, Klapow J, Stewart K, Westfall A, Mallinger A, DeMasi R, Centor R, Saag M. Health-related quality of life and virologic outcomes in an HIV clinic. Qual Life Res. 2000;9(9):977–85.
Ingumbor J, Steward A, Holzemer W. Comparison of the health related quality of life, CD4 count and viral load of AIDS patients with HIV who have been on treatment for 12 months in rural South Africa; 2013.
Mwesigire DM, Martin F, Seeley J, Katamba A. Relationship between CD4 count and quality of life over time among HIV patients in Uganda: a cohort study. Health Qual Life Outcomes. 2015;13(1):1.
Acknowledgments
We would like to acknowledge Dr. Nonhlanhla Yende-Zuma, Dr. Nigel Garrett and the entire CAPRISA Acute Infection team including research leaders who formulated the research ideas that generated such rich data, thank you very much for allowing us to use this dataset. We also thank the participants for their involvement in this study. We would also like to thank the School of Mathematics, Statistics and Computer Science, University of KwaZulu-Natal, South Africa for providing their guidance and support.
Funding
This study was supported through the DELTAS Africa Initiative SSACAB (Grant No. 107754/Z/15/Z). The DELTAS Africa Initiative is an independent funding scheme of the African Academy of Sciences (AAS) Alliance for Accelerating Excellence in Science in Africa (AESA) and is supported by the New Partnership for Africa’s Development Planning and Coordinating Agency (NEPAD Agency) and the UK Government. DELTAS Africa Initiative SSACAB did not have any role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
ZGD designed the study, collected the data, analyzed the data and wrote the article. TZ designed the study, advised on analysis and edited the manuscript. HM and DN reviewed the study designed and critically edited the manuscript. All authors read and approved the final manuscript.
Authors’ information
ZGD is a Ph.D. student and TZ, HM, and DN are senior professors at the University of KwaZulu-Natal.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in this study were approved by the Research Ethics Committee of the University of KwaZulu-Natal and Centre for the AIDS Programme of Research in South Africa (CAPRISA). Written informed consent was obtained from all participants, and ethical approval for the original study was granted by the University of KwaZulu-Natal (E013/04), the University of Cape Town (025/2004), and the University of the Witwatersrand (M040202).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dessie, Z.G., Zewotir, T., Mwambi, H. et al. Modelling immune deterioration, immune recovery and state-specific duration of HIV-infected women with viral load adjustment: using parametric multistate model. BMC Public Health 20, 416 (2020). https://doi.org/10.1186/s12889-020-08530-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-020-08530-x