Abstract
Background
Osteoporosis is a skeletal disease associated with high morbidity, mortality and increased economic costs. Early prevention during adolescence appears to be one of the most beneficial practices. Exercise is an effective approach for developing bone mass during puberty, but some sports may have a positive or negative impact on bone mass accrual. Plyometric jump training has been suggested as a type of exercise that can augment bone, but its effects on adolescent bone mass have not been rigorously assessed. The aims of the PRO-BONE study are to: 1) longitudinally assess bone health and its metabolism in adolescents engaged in osteogenic (football), non-osteogenic (cycling and swimming) sports and in a control group, and 2) examine the effect of a 9 month plyometric jump training programme on bone related outcomes in the sport groups.
Methods/Design
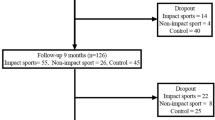
This study will recruit 105 males aged 12–14 years who have participated in sport specific training for at least 3 hours per week during the last 3 years in the following sports groups: football (n = 30), cycling (n = 30) and swimming (n = 30). An age-matched control group (n = 15) that does not engage in these sports more than 3 hours per week will also be recruited. Participants will be measured on 5 occasions: 1) at baseline; 2) after 12 months of sport specific training where each sport group will be randomly allocated into two sub-groups: intervention group (sport + plyometric jump training) and sport group (sport only); 3) exactly after the 9 months of intervention; 4) 6 months following the intervention; 5) 12 months following the intervention. Body composition (dual energy X-ray absorptiometry, air displacement plethysmography and bioelectrical impedance), bone stiffness index (ultrasounds), physical activity (accelerometers), diet (24 h recall questionnaire), pubertal maturation (Tanner stage), physical fitness (cardiorespiratory and muscular), bone turnover markers and vitamin D will be measured at each visit.
Discussion
The PRO-BONE study is designed to investigate the impact of osteogenic and non-osteogenic sports on bone development in adolescent males during puberty, and how a plyometric jump training programme is associated with body composition parameters.
Similar content being viewed by others
Background
Osteoporosis is a common skeletal disease associated with high morbidity and mortality [1]. Approximately 2.7 million European men and women suffer an osteoporotic fracture every year [2]. The economic burden of osteoporosis in Europe is higher than most types of cancer (except lung cancer), or chronic cardiorespiratory diseases [2,3] and represents a direct annual cost of ~ €31.7 billion to health care and social services [1]. In order to improve the outcome for osteoporosis, primary prevention remains the most important policy action in public health. Although contested [4], it is generally accepted that acquiring a high bone mass during childhood and adolescence is a key determinant of adult skeletal health [5-7]. Approximately 60% of osteoporotic cases in adult life are related to low bone mineral content (BMC) in adolescence with up to 50% of total body (TB) bone mass achieved during this period of life [8,9]. Peak bone mass attainment typically occurs between the second and third decade of life, with 80-90% acquired by late adolescence, although this is skeletal site dependent [6,10]. Although bone mass is ~ 60-80% genetically determined [11], there are other factors strongly related with bone mass development. Environmental and lifestyle factors such as physical activity (PA) [12] and nutrition, i.e. calcium intake [13] and vitamin D [14], are known to have important osteogenic effects and have been the key focus in several interventions.
Exercise as a tool to improve bone health
Exercise has been proposed as a key factor for developing healthy bones in childhood and adolescence [15,16], mainly when high-impact and weight-bearing PA occurs [15] above a certain intensity and duration [15,17,18]. Longitudinal studies have shown that habitual PA is positively associated with bone health in children and adolescents because of its impact on bone development [19,20]. The long-term positive effects of PA during adolescence remain into young adulthood with active males aged 24.2 years having 8 and 10% higher BMC at TB and femoral neck (FN) respectively compared to non-active peers, even when adjusted for maturation and size [21]. Research conducted on former professional football players showed that exercise is not only an important factor in the accretion of, but also in the maintenance, of bone mineral density (BMD) [22]. It has been shown that moderate and readily accessible weight-bearing exercise before puberty may increase femoral volumetric BMC, by increasing cortical thickness, and therefore bone strength [23]. In addition, bone development is dependent on the impact of mechanical load and processes that trigger bone modelling and remodelling [24], and possibly on structural adaptations related with trabecular microarchitecture [25].
Sport participation and bone health
It has been shown that sport participation is crucial for healthy bone development, however not all sports have a positive influence on the skeletal mass. According to their characteristics, sports can be described as osteogenic (weight-bearing exercise) and non-osteogenic (non weight-bearing exercise). Apart from numerous health benefits [26], football is considered as an osteogenic sport both in childhood and adolescence as bone mass is augmented [27-30]. In contrast, sports such as cycling [31-40] or swimming [41-46] are associated with no change or a reduction in bone mass when compared to controls. This could be a barrier for obtaining a high peak bone mass which may compromise future bone health [40,41,46,47].
Plyometric exercise intervention to increase bone health
To achieve the benefits of exercise and gain acceptance, PA models must be effective, simple to administer, feasible, inexpensive, short in duration and possible to perform at any location (i.e. at home, at the sports centre). Plyometric jump training (PJT) may be a judicious choice and experimental studies using animal models have repeatedly shown that short, discrete bouts of exercise interspersed with rest periods is more effective than a single longer bout of exercise for improving bone mass and strength [48].
Research in early puberty has shown that a novel and easily implemented 8-month PJT (Bounce at the Bell; ~3 min/day) enhanced bone mass at the weight bearing proximal femur [49]. Mackelvie et al. showed that a 7-month jumping intervention (10 min, 3 times/week) was associated with more bone at the FN and lumbar spine (LS) in early pubertal girls [50], and these results were maintained after 2 years [51]. In addition, prepubertal Asian and Caucasian boys of average or low body mass index (BMI) augmented bone mineral accrual at several regions after a 7-month jumping intervention (10 min, 3 times/week). However, there are a lack of studies analysing the effect of PJT in the adolescent population, which is crucial as adolescence is the period associated with the greatest increments in BMC and BMD [52]. In addition, this has not been studied in adolescents engaged in different sports (osteogenic vs. non osteogenic), which is important to examine if peak bone mass during adolescence may be maximized and therefore reduce the risk for developing osteoporosis in adulthood.
Bone turnover markers and vitamin D
Bone development depends on its metabolic activity, which includes bone formation, resorption and, as a consequence bone turnover [53]. The relationship of PA and sport participation with bone metabolism markers has been shown previously in adolescents [54,55]. An increase in the concentrations of bone formation and resorption markers can be observed in non-osteogenic sports, such as swimming, but a comparison between osteogenic and non-osteogenic sports has not been investigated previously [56].
The role of vitamin D in bone metabolism is important due to contribution of vitamin D in calcium homeostasis and bone mineralization processes during growth. Evidence shows that adequate vitamin D levels are necessary to acquire bone mass and interact with exercise to enhance bone growth [57,58]. The magnitude of the benefits in boys and girls differ at sites of the skeleton and may depend on the baseline levels of vitamin D and on previous loading experience [59]. A positive interaction between PA and vitamin D on BMD in adolescents has been described [60,61] however the association between vitamin D with osteogenic and non-osteogenic sports has not been justified.
Objectives
The objectives of the PRO-BONE study are: 1) to longitudinally assess, over 3 years, bone health and its metabolism in adolescents engaged in osteogenic (football) and non-osteogenic (cycling and swimming) sports, and 2) after 12 months of sport participation to examine whether a short and inexpensive 9 months PJT intervention programme is positively associated with bone-related variables and its metabolism in adolescent footballers, cyclists and swimmers.
The secondary aim of the study is to examine whether the PJT programme stimulus is enough to counteract the expected negative consequences of these non-osteogenic sports in bone health and to follow-up the bone-related variables and its metabolism over 12 months after the PJT programme.
Methods/Design
Study design
PRO-BONE is a longitudinal design and involves four cohorts of males aged 12–14 years at the beginning of the study. These four cohorts consist of footballers, cyclists, swimmers and controls that will be followed over a period of 33 months. The timeline of the PRO-BONE study can be seen in Figure 1.
Sample size
The sample size has been calculated according to the primary interest variable, TB BMD (of cyclists (aged 15.5 years) [39] in order to achieve 90% of statistical power to detect differences in the contrast of the null hypothesis H0: μ1 = μ2 through bilateral student t, difference between two dependent means (matched pairs). Taking into account a significance level of 5% and assuming that the mean of the reference group 1.133 units (SD = 0.127) and the mean of the experimental group is 1.002 units (SD = 0.093), it will be necessary to include 9 participants in the reference group and 9 participants in the experimental group, totalling 18 participants. It is known that the number of participants to recruit depends also on potential withdrawals [or could use drop-outs]: n’ = n/(1-p), so that if the withdrawals were 40% the number of participants to be recruited would be n’ = 9/(1–0.4) = 15 in each group (e.g. 15 INT cyclists + 15 CON cyclists = 30 cyclists). Therefore, cyclists (n = 30), footballers (n = 30), swimmers (n = 30) and controls (n = 15) will be recruited, yielding a total N = 105.
Recruitment of the participants
Participants and parents/guardians will be contacted via advert flyers, posters and social media to participate in this study and by contacting sport clubs and schools from the South West of England. Where possible, a meeting will be held to explain the project as well as to answer any questions. At the end of this meeting, consent/assent forms and information sheets will be given out and participants and parents/guardians will have 15 days to return the consent/assent forms. After these 15 days, a reminder (phone call or email) will be provided to those not sending the consent/assent to check if they wish to participate. Seven more days will be given to those that agreed to participate and in the 2nd reminder, they will be asked to send the interest and consent/assent forms signed.
Participants will be screened for eligibility, based on the inclusion/exclusion criteria outlined below, by a member of the research team depending on the information provided in the interest form. If eligible, the baseline assessment will be scheduled for the participant. All participants and parents involved in this project will be carefully informed about the risks and benefits of the study and will be required to sign the approved assent and consent forms before their visit to the laboratory at the Children’s Health and Exercise Research Centre (CHERC, University of Exeter).
Inclusion and exclusion criteria
Inclusion criteria include: 1) Males 12–14 years old, engaged (≥3 h/week) in osteogenic (football) and/or non-osteogenic (swimming and cycling) sports in the last 3 years or more; 2) Male adolescents 12–14 years old not engaged in any of these sports (≥3 h/week) in the last 3 or more years (control group).
Exclusion criteria include: 1) participation in another clinical trial; 2) any acute infection lasting until < 1 week before inclusion; 3) medical history of diseases or medications affecting bone metabolism or the presence of an injury (before inclusion) that may affect participation in their respective sports and/or any variable considered in the present study (i.e. doing the PJT); 4) non-Caucasian participants. The latter is included since there are differences in body composition (bone, fat and fat-free mass) and biochemical markers (i.e. osteocalcin) between ethnic groups [62].
Ethics approval
The methods and procedures of the PRO-BONE study have been checked and approved by: the Ethics Review Sector of Directorate-General of Research (European Commission, ref. number 618496), the Sport and Health Sciences Ethics Committee (University of Exeter, ref. number 2014/766) and the National Research Ethics Service Committee (NRES Committee South West – Cornwall & Plymouth, ref. number 14/SW/0060). All data and information obtained will be confidential and access to database will be restricted to the researchers of the study. All measurements will be carried out by qualified and experienced researchers that will undergo a Disclosure and Barring Service check for approval to work with young people.
Study protocol and measurements
Body composition
Anthropometry
Stature (cm), seated height (cm) and body mass (kg) will be measured by using a stadiometer (Harpenden, Holtain Ltd, Crymych, UK; precision 0.1 cm; range 60–210 cm), a sitting height table (Harpenden, Holtain Ltd., Crymych, UK; precision 0.1 cm; range 32–109 cm) and an electronic scale (Seca 877, Seca Ltd, Birmingham, UK; precision 100 g; range 2–200 kg) respectively. Body mass index (BMI) will be calculated as body mass (kg) divided by the height (m) squared.
Waist circumference will measured at the midpoint between the lowest rib cage and the top of the iliac crest. Hip circumference will be measured around the widest portion of the buttocks. All measurements will be undertaken by the same trained researcher using the type Seca 201 measuring tape (Seca Ltd, Birmingham, UK; precision 0.1 cm; range 0–205 cm). All anthropometrical measurements will be performed three times and the mean will be calculated. Pubertal maturation will be self-reported by the participants during each visit using adapted drawings of the five stages (Tanner) of pubertal hair development [63].
Dual-energy x-ray absorptiometry
Dual-energy x-ray absorptiometry scanner (GE Lunar Healthcare Corp., Madison, WI, USA) will be used to scan participants at four sites due to the evidence of site specific impact of sports participation [64-66]: 1) LS (mean of L1-L4), 2) right hip, 3) left hip, 4) TB. The DXA equipment will be calibrated at the start of each testing day by using a LS phantom as recommended by the manufacturer. The body will be segmented in accordance to standard procedures to evaluate regional bone mass and fat distribution. The scan modes will be automatically selected by the scanner software (standard or thick). All DXA scans and analyses will be performed using the GE enCORE software (2006, version 14.10.022).
Participants will be asked to remain still and they will be scanned in the supine position. The BMC (g) and BMD (g/cm2) with aged-matched Z-scores and age-matched % will be obtained. For LS regions area (cm2), width (cm) and height (cm) will be recorded and for TB regions, fat mass (g), lean mass (kg) and body fat (% and kg) will be obtained. Information about hip strength index, fat mass ratios (trunk/total, legs/total, arms and legs/trunk), android and gynoid regions will also be obtained and have been previously validated in adolescents [67].
This technique uses ionizing radiation that raises ethical issues particularly for child participants. However, this technique uses a minimal radiation dose (similar to spending a day outside in the sunshine), and has been widely used for research purposes with child participants worldwide. The estimated lifetime risks of using GE Lunar Prodigy DXA measurements in the paediatric population was found to be negligible [68].
Air displacement plethysmography
Body volume will be measured with BodPod (Body Composition System, Life Measurement Instruments, Concord, California, USA) as it can effectively predict visceral adipose tissue in children [69] and determine the changes of body fat percentage over time [70]. Two measurements will be performed and if there is a difference of more than 150 mL in body volume, a third measurement will be taken. The equipment will be calibrated at the commencement of each testing day following the manufacturer’s guidelines and using a cylinder of specific volume (49.887 L). Participants will wear clothing according to the manufacturer’s recommendation (a swimsuit and a swim cap) to rule out air trapped in clothes and hair. Participants will be weighed on the BodPod calibrated digital scale and then will enter into the BodPod chamber. During the measurements participants will be asked to remain in a seated position and to breathe normally. A mean value for body volume will be obtained following the manufacturer’s recommendations [71] and this value will be integrated into the calculation of lung volume. Percentage of TB fat mass will be calculated using the equation reported by Siri [72,73].
Imaging bone ultrasonometer
Qualitative ultrasound measurements will be performed with a Lunar Achilles Insight and the OsteoReport PC software version 5.x + (TM Insight GE Healthcare, Milwaukee, WI, USA). This portable device measures bone stiffness using ultrasound waves and is considered a valid and radiation-free method to assess bone health in children [74,75]. The same device will be used throughout the study and calibration will be carried out prior to each visit. A standard procedure will be followed according to manufacturer’s instructions. Participants will be placed on a stable chair in a comfortable position directly in front of the Achilles device. The position of the leg will rest lightly against the calf support so the foot, calf and thigh are aligned with the centre of the calf support and the positioner.
The qualitative ultrasound device provides three outcome variables, the broadband ultrasound attenuation (BUS), the speed of sound (SOS) and the stiffness index (SI). The BUA indicates the absorption of sound waves measured in decibels per megahertz. The SOS shows the stiffness of a material by the ratio of the traversed distance to the transit time, expressed in meters per second. And the SI is calculated by a linear combination of BUA and SOS: SI = (0.67 x BUA) + (0.28 × SOS) – 420. The real-time image of the calcaneus and the region of interest ensure that the measurement is precise [74]. Both feet will be measured twice and the mean of the two measurements will be calculated and used for statistical analyses.
Bioelectrical impedance analysis
The portable BIA device (Tanita BF-350, Tokyo, Japan; range 2–200 kg; precision 100 g; body fat % range 1-75%; body fat% increments 0.1%) will estimate the percentage of body fat by using the values of resistance and reactance. Participants will be measured in a fasting state and will remove any metal objects and socks prior the measurements. They will be positioned on the posterior surface barefoot according to manufacturer’s instructions. Despite the reported prediction measurement error, BIA is considered a practical method to assess body fat in addition to DXA and BodPod in adolescents [76,77].
Biochemical markers and blood collection
The measurement of bone turnover markers, in addition to the measurement of bone mass, is an interesting option to obtain a more dynamic picture of bone tissue, with the advantage that can be repeated at short intervals [78]. Therefore, the combination of both measures (bone mass and bone metabolism) is essential to obtain a better understanding on changes in the skeletal mass. In this regard, the International Osteoporosis Foundation and the International Federation of Clinical Chemistry recommended the use of serum procollagen type 1 aminoterminal propeptide (P1NP) and isomer of the Carboxi-terminal telopeptide of type 1 collagen (CTX-1) as markers for formation and resorption, respectively [79]. The role of vitamin D in bone metabolism is important due to contribution of vitamin D in calcium homeostasis and bone mineralization processes during growth. Assessment of vitamin D levels can be achieved by measuring the serum 25-hydroxyvitamin D [25(OH)D] in the blood [80]. For the scope of the present study 25(OH)D will be analysed as it has been shown to interact with PA to improve bone mass in adolescents [14].
Blood samples will be collected between 8:00 am and 9:00 am following a 12-hour fast period. A research team experienced in sampling techniques will collect capillary blood samples (~1.2 mL) from a pre-warmed hand into heparin fluoride coated microvettes (CB 300 tubes, Sarstedt Ltd, Leicester, UK) that will be placed immediately on ice. The microvettes will be centrifuged at 1000 × G per min for 15 minutes at 4°C and plasma will be separated in Eppendorf tubes of at least 60 μL, 110 μL and 60 μL and stored at −80°C for future analysis of P1NP, CTX-1 and 25(OH)D respectively. The CTX-1 and 25(OH)D biochemical markers will be analysed by using IDS-iSYS CrossLaps (Immunodiagnostic Systems Ltd, UK) and total P1NP by using ELISA kit (MyBioSource, San Diego, California, USA).
Physical fitness assessment
A battery of tests will be used to assess attributes of physical fitness that may play an important role in the development of skeletal mass and strength during growth and maturation. Cardiorespiratory fitness (aerobic performance) will be estimated using the 20 m shuttle run test [81], which has been shown to be both reliable and valid in youth [82]. The participants will be tested at the end of the day following a standardized warm up. They will be asked to run between two lines set 20 m apart by following the pace of the audio signals produced from a CD player. The starting speed will be 8.5 km∙h−1 and will be increased by 0.5 km∙h−1 each minute. The participants will be encouraged to continue the test until they reach maximal effort. The test will end when the participant fails to reach the line two consecutive times. The last completed shuttle will indicate the score of the test.
The standing long jump test and the Abalakov jump test will be performed at least half an hour before the 20 m shuttle run test and following a standardized warm up and with 2 minutes rest between the two tests. The starting position of the standing long jump test will be exactly behind a line and with feet at shoulder’s width apart. Participants will be allowed to swing their arms during the eccentric contraction phase and they will be advised to jump as far as possible in order to land with both feet on a non- slippery hard surface. The distance (cm) will be measured between the starting line and the participant’s heels. Participants will perform the Abalakov jump test on a jump mat (Probotics Inc., Huntsville, USA) after having received instructions as to how much can they bend their knees and the position of their arms, they will be asked to jump as high as possible. Then, they will be placed in a standing position with their feet shoulder width apart at the jump mat. For both muscular tests the participants will perform 1 familiarization effort and 2 maximal effort jumps. The mean height and distance (in cm) of the maximal efforts will be used as criterion of measure. The reliability of both tests in adolescents was previously described and is acceptable to be used in this population [83]. The order of all the measurements for each testing day can be seen in Figure 2.
Physical activity measurements
PA will be measured using two different methods: 1) International Physical Activity Questionnaire and 2) a wrist accelerometer (GENEActiv, GENEA, UK). The validity and reliability of the accelerometer and of the International Physical Activity Questionnaire has been established previously in children and adolescents [84,85]. GENEActiv accelerometers are waterproof so are valid for the swimmers too. Both methods will be used in order to obtain more precise data as, for example, accelerometers do not properly measure PA in cyclists as bouts of activity are not detected [86]. A diary to complement accelerometer data will be administered to the participants to obtain additional information such as calcium and protein intake.
Dietary assessment
Assessment of dietary intakes of calcium, vitamin D and milk will be completed by using two non-consecutive 24-h dietary recall questionnaires. CompEat Pro software (Nutrition systems, VIS Visual Information Systems Ltd., UK) will be used for the analysis.
Jumping intervention
Following 12 months of sport specific training, the randomisation process will start in each sport group and participants will be divided into two sub-groups to perform a PJT programme as follows: 1) intervention programme groups, (sport + PJT) and 2) sport groups (sport only). It has been shown that 7 to 9 month PJT programmes can effectively improve BMC and/or BMD at different skeletal sites in children and adolescents and to maintain the benefits for 3 years after the intervention [52,87]. Therefore, a progressive PJT (~10 min/day) will be performed by intervention groups 3 to 4 times/week (depending on progression) as shown in Table 1. Before the intervention, trained staff will ensure that participants fully understand and correctly execute the different jumps and a research assistant will meet with the participants to observe, demonstrate and review the jumps. Participants will be instructed to perform a number of countermovement jumps (CMJ) and squat jumps (SJ) on a hard surface. Jumps will be performed before and after school and before going to bed. The CMJ will be performed by bending the knees prior to the jump. The CMJ activates the stretch-shortening cycle in the muscles, resulting in greater power production in the legs compared to a SJ. For the SJ participants will squat down until the knees are bent at 90 degrees, then they will immediately jump vertically as high as possible, landing back on the ground on both feet simultaneously. For this technique, the participant starts from a stationary semi-squatting position, or pauses at the lower level of the squat before jumping upwards. This removes the factor of the stretch-shortening cycle. The reliability and validity of the CMJ and SJ has been previously reported [88,89].
These jumps are associated with important ground reaction forces, i.e. for a countermovement it is about 5 times body weight (BW), compared to 3.5 times BW for jumping jacks. Similarly, the highest rates of change in force are 493 times BW/s for the CMJ, as shown in an independent sample of boys and girls [90]. A diary will be used to record the number of jumps performed each day. Both the intensity and number of jumps will be increased progressively in 3 levels of 12 weeks each. Intensity will be modified using ankle weights (from 1 kg at level 1 to 2.5 kg at level 3). With this an increase in BW between 2 to 5 kg will be achieved. In this regard, it has been shown that adolescents with higher BMI have higher levels of bone mass, because of the higher lean mass that they develop as a consequence of their higher fat mass [91].
Discussion
PRO-BONE will assess the longitudinal impact of osteogenic (football) and non-osteogenic (cycling and swimming) sports on bone development in adolescents aged 12–14 years old. In addition, it will investigate whether a simple, feasible and inexpensive PJT programme can improve bone development and if the effects will be maintained a year after finishing the PJT programme. Several investigations have been conducted in order to improve bone health through exercise, strength, jumping or even combinations among them [92]. However, to achieve impact and gain acceptance, the intervention must be effective, simple to administer, feasible, inexpensive, short in duration and possible to perform at any place [49]. PRO-BONE has been designed to meet all these requirements and follow-up its effects after the withdrawal of the intervention.
Previous research has shown that exercise is positively associated with bone health [93]. However, there are some sports that due to the impact generated at the skeletal sites may have a minimal or negative effect on BMC and BMD [40,56]. As recent data have shown, jump training is associated with increases in BMC and BMD and may play an important role in the prevention of osteoporosis [94]. It is well known that early prevention is the most effective tool, therefore, it is crucial to analyse the effect of PJT at an early stage (i.e. adolescence). In this sense, it is important to examine if PJT can counteract the potential negative consequences of non-osteogenic sports on bone health and if there is enough stimuli to increase BMC and BMD in adolescents engaged in osteogenic sports.
PRO-BONE will employ different and well known technological devices and methods such as DXA, BodPod, imaging bone ultrasonometer and triaxial accelerometers among others. In addition, the PJT will include a progression in intensity with ankle weights to maximize the potential to augment bone. PRO-BONE is timely as there is a lack of studies analysing the effects of PJT on bone health during the crucial this period of life. It represents a golden opportunity to measure how a simple, feasible and inexpensive PJT is associated with bone health in adolescents engaged in different sports. It will also show if the effect of this intervention differs between sports, expecting a greater effect in cyclists and swimmers than footballers. In addition, PRO-BONE will allow us to compare within each group and investigate changes in body composition in groups doing the PJT plus training vs groups only training. Finally, PRO-BONE will examine whether PJT has any additional effect on footballers. Football is considered one of the most osteogenic sports, but this type of intervention has not yet been studied.
Abbreviations
- BMC:
-
Bone mineral content
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- 25(OH)D:
-
25-hydroxyvitamin D
- BIA:
-
Bioelectrical impedance analysis
- BodPod:
-
Air displacement plethysmography
- BW:
-
Body weight
- SOC:
-
Football players
- SWI:
-
Swimmers
- CYC:
-
Cyclists
- CON:
-
Control
- DXA:
-
Dual energy x-ray absorptiometry
- PJT:
-
Plyometric jump training
- CMJ:
-
Counter movement jump
- SJ:
-
Squad jump
- P1NP:
-
Procollagen type 1 aminoterminal propeptide
- CTX-1:
-
Carboxi-terminal telopeptide of type I collagen
- LS:
-
Lumbar spine
- FN:
-
Femoral neck
- TB:
-
Total body
References
Kanis JA, Johnell O. Requirements for DXA for the management of osteoporosis in Europe. Osteoporos Int. 2005;16(3):229–38.
Kanis JA, Burlet N, Cooper C, Delmas PD, Reginster JY, Borgstrom F, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2008;19(4):399–428.
Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12):1726–33.
Gafni RI, Baron J. Childhood bone mass acquisition and peak bone mass may not be important determinants of bone mass in late adulthood. Pediatrics. 2007;119 Suppl 2:S131–6.
Rizzoli R, Bianchi ML, Garabedian M, McKay HA, Moreno LA. Maximizing bone mineral mass gain during growth for the prevention of fractures in the adolescents and the elderly. Bone. 2010;46(2):294–305.
Baxter-Jones AD, Faulkner RA, Forwood MR, Mirwald RL, Bailey DA. Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass. J Bone Miner Res. 2011;26(8):1729–39.
Davies JH, Evans BA, Gregory JW. Bone mass acquisition in healthy children. Arch Dis Child. 2005;90(4):373–8.
Perez-Lopez FR, Chedraui P, Cuadros-Lopez JL. Bone mass gain during puberty and adolescence: deconstructing gender characteristics. Curr Med Chem. 2010;17(5):453–66.
Baroncelli GI, Bertelloni S, Sodini F, Saggese G. Osteoporosis in children and adolescents: etiology and management. Paediatr Drugs. 2005;7(5):295–323.
Henry YM, Fatayerji D, Eastell R. Attainment of peak bone mass at the lumbar spine, femoral neck and radius in men and women: relative contributions of bone size and volumetric bone mineral density. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2004;15(4):263–73.
Zofkova I. Role of genetics in prediction of osteoporosis risk. Vnitr Lek. 2011;57(1):78–84.
Branca F, Valtuena S. Calcium, physical activity and bone health–building bones for a stronger future. Public Health Nutr. 2001;4(1A):117–23.
Vicente-Rodriguez G, Ezquerra J, Mesana MI, Fernandez-Alvira JM, Rey-Lopez JP, Casajus JA, et al. Independent and combined effect of nutrition and exercise on bone mass development. J Bone Miner Metab. 2008;26(5):416–24.
Valtuena J, Gracia-Marco L, Vicente-Rodriguez G, Gonzalez-Gross M, Huybrechts I, Rey-Lopez JP, et al. Vitamin D status and physical activity interact to improve bone mass in adolescents. Osteoporos Int: The HELENA Study; 2012.
Vicente-Rodriguez G. How does exercise affect bone development during growth? Sports Med. 2006;36(7):561–9.
Boreham CA, McKay HA. Physical activity in childhood and bone health. Br J Sports Med. 2011;45(11):877–9.
Gracia-Marco L, Moreno LA, Ortega FB, Leon F, Sioen I, Kafatos A, et al. Levels of physical activity that predict optimal bone mass in adolescents the HELENA study. Am J Prev Med. 2011;40(6):599–607.
Heinonen A: Biomechanics. In., 1st edn. Edited by Khan K; McKay H; Kannus P et al.: Champaign (IL). Physical activity and bone health: Human Kinetics; 2001: 23–34.
Gustavsson A, Thorsen K, Nordstrom P. A 3-year longitudinal study of the effect of physical activity on the accrual of bone mineral density in healthy adolescent males. Calcified Tissue Int. 2003;73(2):108–14.
DA Bailey MH, Mirwald RL, Crocker PR, Faulkner RA. A six year longitudinal study of the relationship of PA to BMAccrual in growing children.pdf> J Bone Miner Res. 1999;14(10):1672–9.
Baxter-Jones AD, Kontulainen SA, Faulkner RA, Bailey DA. A longitudinal study of the relationship of physical activity to bone mineral accrual from adolescence to young adulthood. Bone. 2008;43(6):1101–7.
Uzunca K, Birtane M, Durmus-Altun G, Ustun F. High bone mineral density in loaded skeletal regions of former professional football (soccer) players: what is the effect of time after active career? Br J Sports Med. 2005;39(3):154–7.
Bradney M, Pearce G, Naughton G, Sullivan C, Bass S, Beck T, et al. Moderate exercise during growth in prepubertal boys: changes in bone mass, size, volumetric density, and bone strength: a controlled prospective study. J Bone Miner Res. 1998;13(12):1814–21.
Wolff I, van Croonenborg JJ, Kemper HC, Kostense PJ, Twisk JW. The effect of exercise training programs on bone mass: a meta-analysis of published controlled trials in pre- and postmenopausal women. Osteoporos Int. 1999;9(1):1–12.
Seeman E. An exercise in geometry. J Bone Miner Res. 2002;17(3):373–80.
Krustrup P, Dvorak J, Junge A, Bangsbo J. Executive summary: the health and fitness benefits of regular participation in small-sided football games. Scand J Med Sci Sports. 2010;20 Suppl 1:132–5.
Ara I, Vicente-Rodriguez G, Perez-Gomez J, Jimenez-Ramirez J, Serrano-Sanchez JA, Dorado C, et al. Influence of extracurricular sport activities on body composition and physical fitness in boys: a 3-year longitudinal study. Int J Obes (Lond). 2006;30(7):1062–71.
Vicente-Rodriguez G, Ara I, Perez-Gomez J, Serrano-Sanchez JA, Dorado C, Calbet JA. High femoral bone mineral density accretion in prepubertal soccer players. Med Sci Sports Exerc. 2004;36(10):1789–95.
Krustrup P, Hansen PR, Andersen LJ, Jakobsen MD, Sundstrup E, Randers MB, et al. Long-term musculoskeletal and cardiac health effects of recreational football and running for premenopausal women. Scand J Med Sci Sports. 2010;20 Suppl 1:58–71.
Calbet JA, Dorado C, Diaz-Herrera P, Rodriguez-Rodriguez LP. High femoral bone mineral content and density in male football (soccer) players. Med Sci Sports Exerc. 2001;33(10):1682–7.
Rico H, Revilla M, Villa LF, Gomez-Castresana F, Alvarez del Buergo M. Body composition in postpubertal boy cyclists. J Sports Med Phys Fitness. 1993;33(3):278–81.
Stewart AD, Hannan J. Total and regional bone density in male runners, cyclists, and controls. Med Sci Sports Exerc. 2000;32(8):1373–7.
Duncan CS, Blimkie CJ, Cowell CT, Burke ST, Briody JN, Howman-Giles R. Bone mineral density in adolescent female athletes: relationship to exercise type and muscle strength. Med Sci Sports Exerc. 2002;34(2):286–94.
Duncan CS, Blimkie CJ, Kemp A, Higgs W, Cowell CT, Woodhead H, et al. Mid-femur geometry and biomechanical properties in 15- to 18-yr-old female athletes. Med Sci Sports Exerc. 2002;34(4):673–81.
Warner SE, Shaw JM, Dalsky GP. Bone mineral density of competitive male mountain and road cyclists. Bone. 2002;30(1):281–6.
Nichols JF, Palmer JE, Levy SS. Low bone mineral density in highly trained male master cyclists. Osteoporos Int. 2003;14(8):644–9.
Barry DW, Kohrt WM. BMD decreases over the course of a year in competitive male cyclists. J Bone Miner Res. 2008;23(4):484–91.
Rector RS, Rogers R, Ruebel M, Hinton PS. Participation in road cycling vs running is associated with lower bone mineral density in men. Metabolism. 2008;57(2):226–32.
Olmedillas H, Gonzalez-Aguero A, Moreno LA, Casajus JA, Vicente-Rodriguez G. Bone related health status in adolescent cyclists. PLoS One. 2011;6(9):e24841.
Olmedillas H, Gonzalez-Aguero A, Moreno LA, Casajus JA, Vicente-Rodriguez G. Cycling and bone health: a systematic review. BMC Med. 2012;10:168.
Andreoli A, Celi M, Volpe SL, Sorge R, Tarantino U. Long-term effect of exercise on bone mineral density and body composition in post-menopausal ex-elite athletes: a retrospective study. Eur J Clin Nutr. 2012;66(1):69–74.
Ferry B, Lespessailles E, Rochcongar P, Duclos M, Courteix D. Bone health during late adolescence: effects of an 8-month training program on bone geometry in female athletes. Joint Bone Spine. 2013;80(1):57–63.
Greenway KG, Walkley JW, Rich PA. Does long-term swimming participation have a deleterious effect on the adult female skeleton? Eur J Appl Physiol. 2012;112(9):3217–25.
Ferry B, Duclos M, Burt L, Therre P, Le Gall F, Jaffre C, et al. Bone geometry and strength adaptations to physical constraints inherent in different sports: comparison between elite female soccer players and swimmers. J Bone Miner Metab. 2011;29(3):342–51.
Dias Quiterio AL, Carnero EA, Baptista FM, Sardinha LB. Skeletal mass in adolescent male athletes and nonathletes: relationships with high-impact sports. J Strength Cond Res. 2011;25(12):3439–47.
Tenforde AS, Fredericson M. Influence of sports participation on bone health in the young athlete: a review of the literature. PM R. 2011;3(9):861–7.
Scofield KL, Hecht S. Bone health in endurance athletes: runners, cyclists, and swimmers. Curr Sports Med Rep. 2012;11(6):328–34.
Robling AG, Burr DB, Turner CH. Recovery periods restore mechanosensitivity to dynamically loaded bone. J Exp Biol. 2001;204(Pt 19):3389–99.
McKay HA, MacLean L, Petit M, MacKelvie-O’Brien K, Janssen P, Beck T, et al. “Bounce at the Bell”: a novel program of short bouts of exercise improves proximal femur bone mass in early pubertal children. Br J Sports Med. 2005;39(8):521–6.
Mackelvie KJ, McKay HA, Khan KM, Crocker PR. A school-based exercise intervention augments bone mineral accrual in early pubertal girls. J Pediatr. 2001;139(4):501–8.
MacKelvie KJ, Khan KM, Petit MA, Janssen PA, McKay HA. A school-based exercise intervention elicits substantial bone health benefits: a 2-year randomized controlled trial in girls. Pediatrics. 2003;112(6 Pt 1):e447.
Witzke KA, Snow CM. Effects of plyometric jump training on bone mass in adolescent girls. Medicine and science in sports and exercise. 2000;32(6):1051–7.
Jurimae J. Interpretation and application of bone turnover markers in children and adolescents. Curr Opin Pediatr. 2010;22(4):494–500.
Lima F, De Falco V, Baima J, Carazzato JG, Pereira RM. Effect of impact load and active load on bone metabolism and body composition of adolescent athletes. Med Sci Sports Exerc. 2001;33(8):1318–23.
Gracia-Marco L, Ortega FB, Jiménez-Pavón D, Rodríguez G, Valtueña J, Díaz-Marténez ÁE, et al. Contribution of bone turnover markers to bone mass in pubertal boys and girls. J Pediatr Endocrinol Metab. 2011;24:11–2.
Gomez-Bruton A, Gonzalez-Aguero A, Gomez-Cabello A, Casajus JA, Vicente-Rodriguez G. Is bone tissue really affected by swimming? a systematic review. PLoS One. 2013;8(8):e70119.
Stear SJ, Prentice A, Jones SC, Cole TJ. Effect of a calcium and exercise intervention on the bone mineral status of 16-18-y-old adolescent girls. Am J Clin Nutr. 2003;77(4):985–92.
Valtuena J, Gracia-Marco L, Vicente-Rodriguez G, Gonzalez-Gross M, Huybrechts I, Rey-Lopez JP, et al. Vitamin D status and physical activity interact to improve bone mass in adolescents The HELENA Study. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2012;23(8):2227–37.
Specker B, Vukovich M. Evidence for an interaction between exercise and nutrition for improved bone health during growth. Med Sport Sci. 2007;51:50–63.
Pettifor JM, Prentice A. The role of vitamin D in paediatric bone health. Best Pract Res Clin Endocrinol Metab. 2011;25(4):573–84.
Constantini NW, Dubnov-Raz G, Chodick G, Rozen GS, Giladi A, Ish-Shalom S. Physical activity and bone mineral density in adolescents with vitamin D deficiency. Med Sci Sport Exer. 2010;42(4):646–50.
Bachrach LK, Hastie T, Wang MC, Narasimhan B, Marcus R. Bone mineral acquisition in healthy Asian, Hispanic, black, and Caucasian youth: a longitudinal study. J ClinEndocrinol Metab. 1999;84(12):4702–12.
Tanner JM, Whitehouse RH. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976;51(3):170–9.
Ginty F, Rennie KL, Mills L, Stear S, Jones S, Prentice A. Positive, site-specific associations between bone mineral status, fitness, and time spent at high-impact activities in 16-to 18-year-old boys. Bone. 2005;36(1):101–10.
Magkos F, Kavouras SA, Yannakoulia M, Karipidou M, Sidossi S, Sidossis LS. The bone response to non-weight-bearing exercise is sport-, site-, and sex-specific. Clin J Sport Med. 2007;17(2):123–8.
Ishikawa S, Kim Y, Kang M, Morgan DW. Effects of weight-bearing exercise on bone health in girls: a meta-analysis. Sports Med. 2013;43(9):875–92.
Crabtree NJ, Arabi A, Bachrach LK, Fewtrell M, El-Hajj Fuleihan G, Kecskemethy HH, et al. Dual-energy X-ray absorptiometry interpretation and reporting in children and adolescents: the revised 2013 ISCD Pediatric Official Positions. J Clin Densitom. 2014;17(2):225–42.
Damilakis J, Solomou G, Manios GE, Karantanas A. Pediatric radiation dose and risk from bone density measurements using a GE Lunar Prodigy scanner. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2013;24(7):2025–31.
Winsley RJ, Fulford J, MacLeod KM, Ramos-Ibanez N, Williams CA, Armstrong N. Prediction of visceral adipose tissue using air displacement plethysmography in children. Obes Res. 2005;13(12):2048–51.
Elberg J, McDuffie JR, Sebring NG, Salaita C, Keil M, Robotham D, et al. Comparison of methods to assess change in children’s body composition. Am J Clin Nutr. 2004;80(1):64–9.
McCrory MA, Gomez TD, Bernauer EM, Mole PA. Evaluation of a new air displacement plethysmograph for measuring human body composition. Med Sci Sports Exerc. 1995;27(12):1686–91.
Siri WE. Body composition from fluid spaces and density: analysis of methods. In: Brozek J, Henschel A, editors. Techniques for measuring body composition. Washington, DC: National Academy of Sciences, National Research Council; 1961. p. 223–34.
Siri WE. Body composition from fluid spaces and density: analysis of methods. 1961. Nutrition. 1993;9(5):480–91. discussion 480, 492.
Jaworski M, Lebiedowski M, Lorenc RS, Trempe J. Ultrasound bone measurement in pediatric subjects. Calcif Tissue Int. 1995;56(5):368–71.
Baroncelli GI. Quantitative ultrasound methods to assess bone mineral status in children: technical characteristics, performance, and clinical application. Pediatr Res. 2008;63(3):220–8.
Talma H, Chinapaw MJ, Bakker B, HiraSing RA, Terwee CB, Altenburg TM. Bioelectrical impedance analysis to estimate body composition in children and adolescents: a systematic review and evidence appraisal of validity, responsiveness, reliability and measurement error. Obesity reviews: an official journal of the International Association for the Study of Obesity. 2013;14(11):895–905.
Wu YT, Nielsen DH, Cassady SL, Cook JS, Janz KF, Hansen JR. Cross-validation of bioelectrical impedance analysis of body composition in children and adolescents. Phys Ther. 1993;73(5):320–8.
Jurimae J, Maestu J, Jurimae T. Bone turnover markers during pubertal development: relationships with growth factors and adipocytokines. Med Sport Sci. 2010;55:114–27.
Vasikaran S, Cooper C, Eastell R, Griesmacher A, Morris HA, Trenti T, et al. International osteoporosis foundation and international federation of clinical chemistry and laboratory medicine position on bone marker standards in osteoporosis. Clin Chem Lab Med. 2011;49(8):1271–4.
Pérez-López F. Vitamin D and adolescent health. Adolescent Health, Medicine and Therapeutics. 2010;1:1–8.
Leger LA, Mercier D, Gadoury C, Lambert J. The multistage 20 metre shuttle run test for aerobic fitness. J Sports Sci. 1988;6(2):93–101.
Castro-Pinero J, Artero EG, Espana-Romero V, Ortega FB, Sjostrom M, Suni J, et al. Criterion-related validity of field-based fitness tests in youth: a systematic review. Br J Sports Med. 2010;44(13):934–43.
Ortega FB, Artero EG, Ruiz JR, Vicente-Rodriguez G, Bergman P, Hagstromer M, et al. Reliability of health-related physical fitness tests in European adolescents. The HELENA Study. Int J Obes (Lond). 2008;32 Suppl 5:S49–57.
Phillips LR, Parfitt G, Rowlands AV. Calibration of the GENEA accelerometer for assessment of physical activity intensity in children. J Sci Med Sport. 2013;16(2):124–8.
85. Helmerhorst HJF, Brage S, Warren J, Besson H, Ekelund U: A systematic review of reliability and objective criterion-related validity of physical activity questionnaires. Int J Behav Nutr Phy 2012, 9
Slootmaker SM, Schuit AJ, Chinapaw MJ, Seidell JC, van Mechelen W. Disagreement in physical activity assessed by accelerometer and self-report in subgroups of age, gender, education and weight status. Int J Behav Nutr Phys Act. 2009;6:17.
Gunter K, Baxter-Jones AD, Mirwald RL, Almstedt H, Fuller A, Durski S, et al. Jump starting skeletal health: a 4-year longitudinal study assessing the effects of jumping on skeletal development in pre and circum pubertal children. Bone. 2008;42(4):710–8.
Acero RM, Fernandez-del Olmo M, Sanchez JA, Otero XL, Aguado X, Rodriguez FA. Reliability of squat and countermovement jump tests in children 6 to 8 years of age. Pediatr Exerc Sci. 2011;23(1):151–60.
Markovic G, Dizdar D, Jukic I, Cardinale M. Reliability and factorial validity of squat and countermovement jump tests. J Strength Cond Res. 2004;18(3):551–5.
McKay H, Tsang G, Heinonen A, MacKelvie K, Sanderson D, Khan KM. Ground reaction forces associated with an effective elementary school based jumping intervention. Br J Sports Med. 2005;39(1):10–4.
Gracia-Marco L, Ortega FB, Jimenez Pavon D, Rodriguez G, Castillo MJ, Vicente Rodriguez G, et al. Adiposity and bone health in Spanish adolescents The HELENA. study Osteoporos Int. 2012;23(3):937–47.
Guadalupe-Grau A, Perez-Gomez J, Olmedillas H, Chavarren J, Dorado C, Santana A, et al. Strength training combined with plyometric jumps in adults: sex differences in fat-bone axis adaptations. J Appl Physiol. 2009;106(4):1100–11.
Hind K, Burrows M. Weight-bearing exercise and bone mineral accrual in children and adolescents: a review of controlled trials. Bone. 2007;40(1):14–27.
MacKelvie KJ, McKay HA, Petit MA, Moran O, Khan KM. Bone mineral response to a 7-month randomized controlled, school-based jumping intervention in 121 prepubertal boys: associations with ethnicity and body mass index. J Bone Miner Res. 2002;17(5):834–44.
Acknowledgements
The authors gratefully acknowledge the sport coaches, school teachers and the CHERC research team for their help to run the study.
Funding
This project is funded by the European Union Seventh Framework Programme ([FP7/2007-2013] under grant agreement n°. PCIG13-GA-2013-618496.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LGM (principal investigator), ARB and CAW contributed to the draft of the study. DV wrote the initial draft of the manuscript under the supervision of LGM, ARB and CAW. BSM, KMK will contribute to perform the analysis of the data obtained. All authors have read and approved this work.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Vlachopoulos, D., Barker, A.R., Williams, C.A. et al. Effect of a program of short bouts of exercise on bone health in adolescents involved in different sports: the PRO-BONE study protocol. BMC Public Health 15, 361 (2015). https://doi.org/10.1186/s12889-015-1633-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-015-1633-5