Abstract
Background
Cognitive Behaviour Therapy (CBT) is one of the most successful therapeutic approaches for treating anxiety and depression. Clinical trials show that for some clients, internet-based CBT (eCBT) is as effective as other CBT delivery modes. However, the fidelity of these effects may be weakened in real-world settings where clients and providers have the freedom to choose a CBT delivery mode and switch treatments at any time. The purpose of this study is to measure the CBT attendance rate and identify client-level characteristics associated with delivery mode selection and having reliable and clinically significant improvement (RCSI) of treatment in each delivery mode in a real-world CBT outpatient program.
Methods
This is a retrospective cohort analysis of electronic medical records collected between May 1, 2019, and March 31, 2022, at Ontario Shores Centre for Mental Health Sciences. Regression models were used to investigate the impact of individual client characteristics on participation and achieving RCSI of different CBT delivery modes.
Results
Our data show a high attendance rate for two and more CBT sessions across all modalities (98% of electronic, 94% of group, 100% of individual, and 99% of mixed CBT). Individuals were more likely to enter mixed and group CBT modality if they were younger, reported being employed, and reported higher depression severity at the baseline. Among the four modalities of CBT delivery, group CBT clients were least likely to have RCSI. Of those who started sessions, clients were significantly more likely to experience RCSI on the Patient Health Questionnaire (PHQ)-9 and the Generalized Anxiety Disorder (GAD)-7 if they were employed, reported more severe symptoms at baseline, and were living in the most deprived neighborhoods.
Conclusions
This study will contribute to the body of knowledge about the implementation and treatment planning of different CBT delivery modes in real-world settings. With the changing clinical environment, it is possible to advocate for the adoption of the eCBT intervention to improve therapy practices and achieve better treatment success. The findings can help guide future CBT program planning based on client socio-demographic characteristics, allowing the optimal therapy type to be targeted to the right client at the right time.
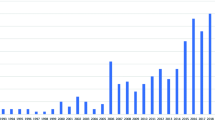
Similar content being viewed by others
Introduction and background
Anxiety and depression are two common mental health conditions that have been successfully treated using cognitive behavioural therapy (CBT), a widely used therapeutic method. The research literature has established the effectiveness of several CBT delivery methods, including individual, group, and internet-based therapy with coaching [1,2,3,4]. There is evidence that CBT is an effective treatment for variety of mental disorders such as generalized anxiety disorder [5], depression [6], panic disorder [7]. There is also strong evidence that suggests internet-based cognitive behavioural therapy (eCBT) is equally as effective as individual treatment for depression [3, 8] and anxiety [9]. The Internet is a good way to spread preventive measures because the units of delivery are cheaper and easy to use [10]. eCBT has become an important modality during the COVID-19 pandemic as access to individual treatment is limited. Understanding the challenges in delivering different CBT modalities will be essential for improving depression and anxiety treatments and implementation of stratified care in specialized mental health centres.
The use of CBT therapies in real-world settings requires further study because a large portion of this evidence relies on controlled experimental settings. The main drawback of these clinical trials is that the implementation of the interventions typically involves a high degree of fidelity to recommended practises and client adherence. This level of fidelity and adherence is likely to be lower in real-world contexts and less is known on what client characteristics are associated with entering therapy modalities and which client variables are connected with completing treatment [11,12,13].
Past empirical studies assessed CBT initiation and dropout rates using variety of client related factors, yet they have limited agreement on the strength of the evidence for these factors. As discussed by El Alaoui et al. [5], this may be the result of a variety of factors, including variations in dropout definition, sample size and features, and statistical techniques for analysing the prognostic significance of baseline variables. This study assesses the relationship between client characteristics on participation in and completion of treatment in different CBT modalities (eCBT, group, individual, mixed) to identify factors that may influence client success in different CBT modalities. The aim is to identify opportunities for further optimization of treatment assignment.
Materials and methods
Study setting
This study used retrospective cohort design, and administrative data were taken from the electronic medical records (EMRs) at Ontario Shores Centre for Mental Health Sciences in Ontario, Canada. Ontario Shores is a specialized mental health hospital in Ontario, Canada that serves a regional population of 2.8 million people. The hospital has 18 care units, 346 inpatient beds, and has over 94,000 outpatient visits annually. The proposed research will support the evaluation and continuous improvement of a multi-modal CBT program at Ontario Shores. Interventions in this program are provided by more than 30 clinicians (social workers, nurses, occupational therapists, and psychologists) across 30 sites.
Ontario Shores Anxiety and Mood Program (AMD) offers individual, group, eCBT (or internet-based CBT with coaching) and mixed modality that is a combination of two or three of these modalities offered to the patient. Individual therapy comprises 60-minute face-to-face structured psychotherapy sessions with a dedicated therapist. Group therapy involves in-person structured psychotherapy led by a single therapist and attended by two or more clients. To address mild to moderate depression and anxiety, Ontario Shores introduced eCBT on May 1, 2019. This modality incorporates coaching sessions, self-help learning modules, informational resources, and assigned homework to reinforce key concepts and impart mental health skills. Clients participating in eCBT, akin to other modalities, have the option to complete assessments throughout the program to monitor progress and enhancements. Aligned with the BC-CBT framework, this therapeutic approach seamlessly integrates in-person sessions with digital and online components for a comprehensive and flexible treatment experience.
Modality selection is determined by a client’s diagnosis, symptoms, and personal preferences. Based on the shared decision-making principals, mental healthcare providers will discuss the different potential treatment options with the client and come to an agreement on the best modality.
Data
Clinical staff members gathered and entered outpatient data inputted into the EMRs (a system called Meditech) at each client interaction. The outpatient records were collected for clients with an initial pre-session evaluation and at least one session of individual, group, or eCBT offered by Ontario Shores. The study utilised data acquired between May 1, 2019, and March 31, 2021, with a one-year follow-up through March 31, 2022, to assess the treatment completion of all clients. We looked back two years to ensure that the first client encounter had been included. For all clients, the first encounter date is the date of their initial pre-session evaluation prior to starting CBT treatment. The EMR data included demographic information from individuals who received eCBT, group CBT, individual CBT, or a combination of these treatments, as well as information from Integrated Community Access Program (ICAP) clinics that provide psychotherapy and medication for individuals with anxiety and mood disorders. At the time of data collection, our exclusion criteria were limited to 31 records pertaining to 5 distinct individuals for whom a confidential flag had been applied. Furthermore, we did not have access to data on services provided by the Ontario Structured Psychotherapy Program, which is a parallel dissemination of CBT occurring in the province during this period with unique treatment and data acquisition protocols.
Outcome measures
Outcome measures included CBT modality selection (i.e., individual, group, eCBT, mixed) and reliable and clinically significant improvement (RCSI) in symptoms of anxiety and depression from baseline to end of follow-up. In practice, healthcare providers will choose the best available modality and advise patients, accordingly, taking the client’s diagnosis and symptoms into consideration. Symptoms of anxiety were measured using the 7-item Generalized Anxiety Disorder (GAD-7) scale [14]. Depressive symptoms were measured using the 9-Question Patient Health Questionnaire (PHQ-9) [15]. Both measures have been validated previously and are commonly employed in clinical settings [16, 17]. The RCSI has been calculated by data and analytics professionals to support treatment planning and routine outcome monitoring inside the Ontario Shores Hospital. In the context of the CBT program, RCSI was defined as a shift in PHQ-9 of > = 6 points from baseline to final scores at the treatment’s conclusion, with an initial PHQ-9 score of > = 10. Similarly, GAD-7 changes > = 5 points from baseline to final scores at the end of treatment, where the first GAD-7 score was > = 8, signifying successful treatment [18, 19].
Data preparation
Our primary sample included 16,510 sessions for 1,098 unique client records who received CBT sessions in the Ontario Shores Mood and Anxiety clinics during the study period. In total, 6,864 electronic CBT, 3,996 group CBT, and 8,808 individual CBT sessions have been provided. All our sample started treatment and 97% completed two or more sessions.
Data management steps included excluding part of independent variables with more than 20% missing information. The decision to exclude variables with high percentages of missing information was primarily driven by the acknowledgment of poor data quality in out-patient databases. Imputing or attempting to fill in missing values for these variables might lead to biased or unreliable results, and therefore, it was deemed more appropriate to remove them from the list of variables considered for analysis. The variables retained in the analysis have undergone this careful data management process to enhance the overall validity of our research findings. We excluded sociodemographic characteristics with high percentage of missing information, such as education (98% missing) and racial identity (29% missing) as well as clinical variables such as primary diagnoses (28% missing) and secondary diagnoses (40% missing). For variables with low levels of missing data, including living arrangement (1%), employment status (6%), Canadian Index of Multiple Deprivation (CIMD) (5%), baseline GAD-7 (6%), and baseline PHQ-9 (less than 1%), we opted for Multiple Imputation (MI). This approach addresses missing values statistically, enhancing the completeness of the dataset and ensuring robustness in subsequent analyses. The MI process involved generating substitute values tailored to the type of each independent variable. In the end, no observations were dropped due to missing data.
Specifically, Bayesian linear regression was applied for continuous variables such as baseline client outcomes, logistic regression for dichotomous variables like living and employment status, and Polytomous logistic regression for categorical variables such as neighborhood deprivation. This approach ensured a comprehensive imputation strategy considering the diverse nature of the dataset’s variables. We utilized RStudio’s “mice” function within the “mice” package to implement MI.
Statistical analysis
Descriptive statistics were performed to compile client variables relevant to each CBT modality that were obtained from the client’s screening (i.e., age, sex, employment, and living status).
We estimated a multinomial logit regression for n = 1,098 clients to determine what client characteristics are related to entering each therapy modalities (Individual, group, eCBT, and mixed). We chose eCBT as the basis category due to its higher frequency. Using “multinom” function from “nnet” RStudio package, we modelled modality choice as a function of client age (adults between the ages of 17–70), sex at birth (male or female), living situation (alone or in a household), employment situation (employed or unemployed), Canadian Index of Multiple Deprivation (in five quantiles), baseline GAD-7, and baseline PHQ-9. The CIMD is a composite index that assesses various dimensions of deprivation and socioeconomic well-being across different geographic areas in Canada. Developed by Statistics Canada, the CIMD integrates multiple indicators related to income, education, employment, housing, and living conditions [20] to provide a comprehensive measure of deprivation. The index assigns quantitative scores to geographic areas based on the levels of deprivation observed. Higher scores indicate higher levels of deprivation, while lower scores suggest better socioeconomic conditions.
To answer our second research question on the predictors of having RCSI, we estimated a logistic regression model using “glm” function for post-treatment RSCI outcome in the PHQ-9 and GAD-7 measures. The outcomes were modelled as a function of CBT modality (Individual, group, eCBT, and mixed), age (adults between the ages of 17 and 70), sex at birth (male or female), living situation (alone or with others), employment situation (employed or unemployed), CIMD deprivation Index (in five quantiles), and baseline GAD-7 and PHQ-9 scores.
Results
Baseline data
Table 1 shows descriptive statistics for clients receiving electronic (n = 563), group (n = 143), individual (n = 256), and mixed CBT (n = 136). The findings are based on the completed (n = 711) imputed data (n = 387) for all 1,098 clients receiving CBT at Ontario Shores between May 1, 2019, and March 31, 2022. The analysis of baseline PHQ-9 and GAD-7 scores reveals a consistent pattern across most Cognitive Behavioral Therapy (CBT) modalities. However, an exception is observed in the case of eCBT. In the eCBT group, the average baseline GAD-7 score was 12 (SD = 5.1), compared to an average of 14 in the other groups (F-statistic = 9.209, p = 5.55e-06. This places the average score within the category of ‘Moderate anxiety’ (10–14 range) according to the GAD-7 scoring guidelines [14]. In the eCBT group, the average baseline PHQ-9 score was 13 (SD = 5.8), compared to an average of 16 to 18 in the other groups (F-statistic = 25.45, p = 1.21e-15) This information suggests that individuals participating in or being assigned to eCBT may, on average, exhibit more moderate levels of depression compared to counterparts in other CBT modalities.
Among all modalities, clients undergoing individual CBT exhibited the highest attendance rate averaging 25 sessions. Clients on average were young females living with others in a moderate socioeconomically deprived neighborhood (Q2 and Q3). They were mostly unemployed, and they had moderate anxiety (10–14 GAD-7 scores risk level) and moderately severe depression (15–19 PHQ-9 scores risk level) on average, with the eCBT cohort scoring the lowest symptom severity. At the end of treatment, more than half of the clients have attained RCSI (56% individual CBT, followed by 55% group, 53% electronic, and 51% mixed CBT).
Multinomial regression findings
To answer our first research question on the characteristics associated with entering each CBT modality, we developed a multinomial logistic regression with modality type as the dependent variable. Table 2 displays coefficient results of each CBT modality in comparison to our baseline modality which is eCBT. Employment was associated with lower probability of receiving individual CBT (OR = 0.49, 95% CI [0.35–0.68]), mixed CBT (OR = 0.5, 95% CI [0.33–0.75]), and group CBT (OR = 0.64, 95% CI [0.44–0.95]). Older age was a predictor of entering into the mixed modality (OR = 1.02, 95% CI [1.01–1.04]) and group CBT (OR = 1.02, 95% CI [1.00-1.03]) versus eCBT. Although the results of CIMD neighborhood deprivation index were inconsistent, living in the fifth quantile (Q5), which identifies the most deprived neighborhood [20], was associated with participation in mixed CBT (OR = 2.24, 95% CI [1.08–4.63]). Compared to eCBT, the severity of the client’s depressive symptoms at baseline was a positive predictor of receiving individual (OR = 1.15, 95% CI [1.11–1.20]), mixed (OR = 1.08, 95% CI [1.03–1.13]), and group CBT (OR = 1.06, 95% CI [1.02–1.11]).
Logistic regression findings on reliable improvement outcome
Table 3 shows the results of a logistic regression analysis on the post-treatment RCSI outcome. From our sets of demographic variables employment (OR = 1.35, 95% CI [1.03–1.77]) was significant in predicting treatment success in terms of having RCSI. As expected, both baseline PHQ-9 (OR = 1.11, 95% CI [1.07–1.15]) and GAD-7 (OR = 1.07, 95% CI [1.04–1.11]) are significantly associated with RCSI. Regarding the modality type, participating in individual (OR = 0.69, 95% CI [0.49–0.98]) and mixed CBT (OR = 0.67, 95% CI [0.44–1.01]) modalities decreased the probabilities of having RCSI relative to eCBT. Despite the inconsistency of the CIMD quantile results, living in the most deprived neighborhood (Q5) (OR = 0.60, 95% CI [0.38–0.94]) decreased the likelihood of having post-treatment RCSI.
Discussion
The purpose of this study is to investigate the relationship between client-level characteristics and participation in different CBT modalities. Furthermore, we examine the predictors of CBT post-treatment RCSI using a retrospective cohort design. In line with previous studies such as Luo et al. (2020) [22], our findings revealed that electronic CBT, along with the other three modes of CBT delivery, had a high attendance rate (showing low early dropout rates), with approximately 80% of clients completing at least six sessions or more. Post-treatment RCSI of PHQ-9 and GAD-7 was present in about 50% of the CBT attendees. Our adjusted findings show lower relative odds of RCSI in more traditional therapy options (individual, group) compared to eCBT, and absolute (unadjusted) differences in probability of RCSI was similar across modalities (from 53% in eCBT to 56% in individual). A notable initial finding reveals a significant variation in the average number of sessions across different modalities, spanning from 9 sessions for eCBT to 25 sessions for individual CBT. It is important to note that while eCBT can be effective for many individuals, it may not be suitable for everyone. Certain conditions or personal circumstances may require the support and guidance of a therapist in a traditional therapy setting. The consultation with a mental health professional can determine the most appropriate form of therapy for client’s specific needs.
There is a large body of literature on CBT treatment initiation or dropout prediction [23,24,25,26] that focuses on dropout rates based on demographic and clinical variables. This study adds to this literature by investigating the individual-level predictors of treatment across a variety of CBT delivery modes to inform program planning. While our findings are descriptive, they suggest that clients with higher baseline PHQ-9 scores (indicating more severe symptoms) are referred to more intensive CBT (e.g., individual, group and mixed). Despite the importance of baseline GAD-7 scores, they were not independently important and associated with treatment modality when adjusting for PHQ-9. There are few differences in other client characteristics across the four treatment modalities. Though, one finding that merits further investigation is that being employed increased the likelihood of receiving eCBT for depression and anxiety disorders. Older clients were also more likely to receive mixed and group CBT therapy.
Our study on the Ontario Shores CBT program highlights the significance of considering clients’ socio-demographic variables, such as employment status, when assessing the success rates of CBT treatment across different modalities. Incorporating predictive algorithms based on sociodemographic factors can offer valuable insights for making informed decisions regarding the appropriate type of psychotherapy treatment for clients.
Regarding modality type, our findings indicate that clients with more severe symptoms are referred into higher intensity CBT and are less likely to respond to treatment. This suggest that there is opportunity to look to other treatments in cases of non-response. In this population, eCBT was at least as effective as more conventional therapies. While this is descriptive, it may imply that there are additional opportunities to optimize care by referring more clients to eCBT given it is less resource intensive.
Study limitation
In our study, certain limitations must be addressed. Firstly, we encountered data quality issues for this study and were unable to work with a broader range of important patient and treatment related variables; consequently, four independent variables were eliminated from our analysis. Secondly, the exclusion of individuals with confidential EMRs was necessary to safeguard requested privacy. Additionally, at the time of data pooling, the unique treatment and data acquisition protocols of OSP led to its exclusion.
The choice of the methodology from authors was based on the nature of our data. We did not consider longitudinal models as all patient characteristics were collected at admission to the CBT program, and most were time-invariant. We collected GAD-7 and PHQ-9 scores longitudinally to calculate the RCSI outcome. However, many clients received only two measurements over their length-of-stay – typically at admission at end-of-treatment. Thus, we had limited ability to capture and analyze changes or over time.
One additional question regarding the data was whether the COVID-19 pandemic had an impact on the outcomes. Using a sample of 116 people who participated in each of the 4 modalities, we performed a sensitivity analysis to count for any demographic variations in comparison to the larger sample to verify this matter (details in the appendix section). Our research cannot establish causality; its findings are primarily descriptive. Given this is an observational study, our results should not be interpreted causally due to unobserved confounding.
This study is limited to a single hospital in Ontario, Canada, and the results may not be applicable to other settings. Ontario Shores offers a variety of CBT treatment alternatives for patients diagnosed with depression and anxiety, including eCBT from May 2019 that made the treatment more accessible and less expensive since the onset of COVID-19. Based on our original findings, eCBT appears to be effective for a specific population, and there may be a case for expanding its use. It is important to note that this is a real-world intervention implemented in an uncontrolled clinical setting, the collection of assessment data was not always consistent. Thus, we used the last available scores for each client to assess RCSI prior to patients leaving the program. The one-year follow-up allowed us to follow all clients from admission to the end of their treatment as clients had variable treatment duration and they may have achieved RCSI prior to their final assessment and that the goal is not to assess long term sustained remission of the condition, but only the state of symptoms at the end of treatment.
Conclusions
The results indicate that there is a room for optimization of the selection process regards to different CBT types for clients admitted with depression and anxiety disorders. Baseline symptoms of depression is an important predictor of treatment success and modality selection. However, those who receive eCBT are more likely to see reliable improvement in their symptoms. This might suggest opportunity to use baseline client characteristics as a predictor of optimal treatment selection. Further research is needed to assess the generalizability of the results and incorporate a broader range of clinical and individual factors, such as client medications, diagnosis, and preferences, into models that shape practitioners’ program recommendations and predict the outcomes of the entrance and modality options.
Data availability
This study utilised electronic health data and client chart reviews acquired at each client encounter at Ontario Shores Hospital. Officers at Ontario Shores have preserved the integrity and confidentiality of the dataset. The data that support the findings of this study are available from Ontario Shores Centre for Mental Health Sciences but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.
Abbreviations
- CBT:
-
Cognitive Behaviour Therapy
- EMRs:
-
Electronic Medical Records
- ICAP:
-
Integrated Community Access Program
- RCSI:
-
Post-treatment Reliable and Clinically Significant Improvement in the PHQ-9 and GAD-7 measures
- LOS:
-
length of stay
- MI:
-
Multiple Imputation
- CIMD:
-
Canadian Index of Multiple Deprivation
- eCBT:
-
Internet-based Cognitive Behaviour Therapy
- UP:
-
Unified protocol
- PHQ-9:
-
9 items Patient Health Questionnaire
- GAD-7:
-
7 items General Anxiety Disorder questionnaire
References
Fordham B, Sugavanam T, Edwards K, Stallard P, Howard R, Das Nair R, et al. The evidence for cognitive behavioural therapy in any condition, population or context: a meta-review of systematic reviews and panoramic meta-analysis. Psychol Med. 2021;51(1):21–9.
Norlund F, Wallin E, Olsson EMG, Wallert J, Burell G, von Essen L, et al. Internet-based cognitive behavioral therapy for symptoms of depression and anxiety among patients with a recent myocardial infarction: the u-care heart randomized controlled trial. J Med Internet Res. 2018;20(3):e88.
Karyotaki E, Efthimiou O, Miguel C, Bermpohl FM, genannt, Furukawa TA, Cuijpers P, et al. Internet-based cognitive behavioral therapy for Depression. JAMA Psychiatry. 2021;78(4):361.
Mohr DC, Ho J, Duffecy J, Sokol L, Burns MN, Reifler D, et al. Effect of Telephone-Administered vs Face-to-face cognitive behavioral therapy on adherence to Therapy and Depression outcomes among Primary Care patients a Randomized Trial. JAMA. 2012;60611(21):2278–85.
Alaoui S, El, Ljótsson B, Hedman E, Kaldo V, Andersson E, Rück C, et al. Predictors of symptomatic change and adherence in internet-based cognitive behaviour therapy for social anxiety disorder in routine psychiatric care. PLoS ONE. 2015;10(4):1–18.
Wu Z, Wang C, Dai Y, Xiao C, Zhang N, Zhong Y. The effect of early cognitive behavior therapy for first-episode treatment-naive major depressive disorder. J Affect Disord. 2022;308:31–8.
Seki Y, Nagata S, Shibuya T, Yoshinaga N, Yokoo M, Ibuki H, et al. Erratum to: a feasibility study of the clinical effectiveness and cost-effectiveness of individual cognitive behavioral therapy for panic disorder in a Japanese clinical setting: an uncontrolled pilot study. BMC Res Notes. 2017;9(1):86.
Mamukashvili-Delau M, Koburger N, Dietrich S, Rummel-Kluge C. Efficacy of computer- and/or internet-based cognitive-behavioral guided self-management for depression in adults: a systematic review and meta-analysis of randomized controlled trials. BMC Psychiatry. 2022;22(1):1–18.
Axelsson E, Hedman-Lagerlöf E. Cognitive behavior therapy for health anxiety: systematic review and meta-analysis of clinical efficacy and health economic outcomes. Expert Rev Pharmacoeconomics \& Outcomes Res. 2019;19(6):663–76.
Sander L, Paganini S, Lin J, Schlicker S, Ebert DD, Buntrock C, et al. Effectiveness and cost-effectiveness of a guided internet- and mobile-based intervention for the indicated prevention of major depression in patients with chronic back pain-study protocol of the PROD-BP multicenter pragmatic RCT. BMC Psychiatry. 2017;17(1):36.
Newton AS, Wozney L, Bagnell A, Fitzpatrick E, Curtis S, Jabbour M, et al. Increasing Access to Mental Health Care with Breathe, an internet-based program for anxious adolescents: study protocol for a pilot randomized controlled trial. JMIR Res Protocols. 2016;5(1):e18.
Karsberg SH, Pedersen MU, Hesse M, Thylstrup B, Pedersen MM. Group versus individual treatment for substance use disorders: a study protocol for the COMDAT trial. BMC Public Health. 2021;21(1):413.
Kingston D, Janes-Kelley S, Tyrrell J, Clark L, Hamza D, Holmes P, et al. An integrated web-based mental health intervention of assessment-referral-care to reduce stress, anxiety, and depression in hospitalized pregnant women with medically high-risk pregnancies: a feasibility study protocol of hospital-based implementation. JMIR Res Protocols. 2015;4(1):e9.
Williams N. The GAD-7 questionnaire. Occup Med. 2014;64(3):224.
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. J Gen Intern Med. 2001;16(9):606–13.
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, et al. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care. 2008;46(3):266–74.
Delgadillo J, McMillan D, Lucock M, Leach C, Ali S, Gilbody S. Early changes, attrition, and dose–response in low intensity psychological interventions. Br J Clin Psychol. 2014;53(1):114–30.
Robinson L, Kellett S, Delgadillo J. Dose-response patterns in low and high intensity cognitive behavioral therapy for common mental health problems. Depress Anxiety. 2020;37(3):285–94.
Matheson F, Moloney G, VanIngen T. Ontario Agency for Health Protection and Promotion (Public Health Ontario). 2016 Ontario marginalization index: user guide. Public Health Ont. 2022.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x. PMID: 11556941; PMCID: PMC1495268.
Luo C, Sanger N, Singhal N, Pattrick K, Shams I, Shahid H, et al. A comparison of electronically delivered and face to face cognitive behavioural therapies in depressive disorders: a systematic review and meta-analysis. EClinicalMedicine. 2020;24:100442.
Keefe JR, Chambless DL, Barber JP, Milrod BL. Predictors, and moderators of treatment dropout in cognitive-behavioral and psychodynamic therapies for panic disorder. Psychother Res. 2021;31(4):432–42.
O’Keeffe S, Martin P, Target M, Midgley N. I just stopped going: a mixed methods investigation into types of Therapy Dropout in adolescents with Depression. Front Psychol. 2019;10(FEB):1–14.
Schmidt ID, Forand NR, Strunk DR. Predictors of Dropout in Internet-based cognitive behavioral therapy for Depression. Cogn Therapy Res. 2019;43(3):620–30.
Lawler K, Earley C, Timulak L, Enrique A, Richards D. Dropout from an internet-delivered cognitive behavioral therapy intervention for adults with depression and anxiety: qualitative study. JMIR Formative Res. 2021;5(11):1–19.
Acknowledgements
Ontario Shores Centre for Mental Health Sciences (Ontario Shores) is a public teaching hospital providing a range of specialized assessment and treatment services to those living with complex and serious mental illness like depression and anxiety. The findings of this study and the paper’s conclusions are those of the authors and do not represent the Ontario Shores Centre for Mental Health Sciences. The authors also wish to thank the staff and information officers at Ontario Shores that help us to acquire the information for this research study.
Funding
This study was funded by the Green Shield Canada, Mitacs joint postdoctoral fellowship program between Ontario Tech University and Ontario Shores Hospital. The Ontario Shores Hospital has provided the data and consultation regarding all patient characteristics used in this study. Funding sources had no role in the study design, analysis, or interpretation of findings.
Author information
Authors and Affiliations
Contributions
The contributions of each author to this research article are as follows: Afsaneh Roshanghalb contributed significantly to this research article. She conducted a comprehensive literature review, analysing existing research and theoretical frameworks to provide a solid foundation for the study. She took the lead in preparing the initial draft of the manuscript. Additionally, she played a crucial role in data analysis and interpretation, utilizing statistical techniques and regression models. Afsaneh was responsible for aggregating the data and creating visualizations to effectively communicate the study’s results.Bojay Hansen played a vital role in data pooling, data collection and management. He actively participated in the writing and revision process of the methodology section, ensuring its accuracy and clarity.David Rudoler provided guidance and oversight. He actively contributed to the interpretation of findings and the synthesis of results. David also made significant contributions to the writing and revision of the discussion and conclusion sections of the manuscript. Michael W. Best conceived the original research idea and was actively involved in the implementation of the study, specifically in the collection of relevant data from the real-world CBT outpatient program. He contributed to the interpretation of the results and provided valuable insights during the writing and revision process. All authors have read and approved the final version of the manuscript. They have actively contributed to the intellectual content of the research, ensuring its accuracy and scientific rigor.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was subject to acquiring and continuing ethics review by the research ethics board (REB) at Ontario Shores Centre for Mental Health Sciences for using information from electronic health data and client chart review forms throughout the life of the project. The informed consent is waived by ethics committee considering the retrospective nature of the study. It has been approved by Becky Greenberg, RN, PhD, Chair, Ontario Shores Centre for Mental Health Sciences Research Ethics Board on August 17th, 2022. The quantitative analysis and access to the datasets were approved by the Research Ethics Board at Ontario Shores Centre for Mental Health Sciences. The REB approval number is 22-030-D, which was received on August 17th, 2022.
Consent for publication
Not available.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Roshanghalb, A., Hansen, B., Rudoler, D. et al. Predicting CBT modality, treatment participation, and reliable improvements for individuals with anxiety and depression in a specialized mental health centre: a retrospective population-based cohort study. BMC Psychiatry 24, 390 (2024). https://doi.org/10.1186/s12888-024-05817-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-05817-w