Abstract
Objective
To review the relationship between adiponectin levels and autism spectrum disorders (ASDs) in children.
Background
ASDs are associated with pervasive social interaction and communication abnormalities. Researchers have studied various pathophysiological mechanisms underlying ASDs to identify predictors for an early diagnosis to optimize treatment outcomes. Immune dysfunction, perhaps mediated by a decrease in anti-inflammatory adipokine, adiponectin, along with changes in other adipokines, may play a central role in increasing the risk for ASDs. However, other factors, such as low maternal vitamin D levels, atherosclerosis, diabetes, obesity, cardio-metabolic diseases, preterm delivery, and oxytocin gene polymorphism may also contribute to increased risk for ASDs.
Methods
Searches on the database; PubMed, Google Scholar, and Cochrane using keywords; adiponectin, adipokines, ASD, autism, autistic disorder, included English-language studies published till September 2022. Data were extracted on mean differences between adiponectin levels in children with and without ASDs.
Results
The search yielded six studies providing data on adiponectin levels in young patients with ASDs. As can be seen from Table 1, four of the six studies were positive for an inverse correlation between ASD and adiponectin levels. In addition, two of the four positive and one negative studies found low adiponectin levels associated with and the severity of autistic symptoms. However, results from one reviewed study were insignificant.
Conclusion
Most studies reviewed yielded lower adiponectin levels in children with ASDs as well as the severity of autistic symptoms.
Similar content being viewed by others
Background
Autism Spectrum Disorders (ASDs) have been diagnosed in 1% of children worldwide [1], implying that 1 in every 68 children has autism, with boys having a significantly higher risk for this disorder than girls [2]. The growing number of young patients with ASDs over the recent years, with increasing levels of mental, physical, socioeconomic, and emotional stressors, not only directly impacts autistic patients [3], but also increases the caretaker burden [4, 5]. Therefore, there is an urgent need for timely diagnosis to initiate early treatment interventions to optimize long-term outcomes in patients with ASDs [6].
Researchers have studied various pathophysiological mechanisms underlying ASD to develop early predictors for identifying at-risk patients and initiating timely treatment interventions. It is considered a complex genetic disorder having diverse familial inheritance patterns and an estimated possible involvement of up to 1000 genes [7]. Epigenetic mechanisms such as DNA methylation function at the intersection of genetic, environmental, and protective factors [8]. ASD pathogenesis is centered on altered neural connections and synaptic function. For instance, Numerous of the 207 SFARI genes that are syndromic and category 1 high risk (for ASD) encode for proteins that are essential for synaptic function in the brain. Nutritional factors, such as lower maternal vitamin D levels, have also been implicated with a greater risk of ASD in the offspring [9]. In addition, congenital and maternal infections have been correlated with ASD [10,11]. However, the link between ASD and activated immune responses in mother [12], cytokine storm [13], maternal antibodies, and auto-antibodies [14] stand out. In this context, the cytokines released from the adipocytes may play a significant role in the mediation of ASDs [15]. Beyond its energy-preserving abilities, adipose tissue is often forgotten in its role as an endocrine organ that mobilizes inflammatory reactions through the production of adipokines [16]. Not only does adipose tissue control inflammation, but it also prevents metabolic disturbances and maintains homeostasis [17], which makes it worthy of attention in its association with ASDs. Like cytokines, adipokines can also be anti- and proinflammatory, such as adiponectin and tumor growth factor-beta (TGF-β) are anti-inflammatory, and tumor necrosis factor α (TNF-α), interleukin 6 (IL-6), leptin, resistin, angiotensinogen, and plasminogen activator inhibitor-1 promote inflammation [18]. An altered ratio between anti-inflammatory [19] and proinflammatory adipokines has been reported in autistic children [20]. Of these, a reduction in the most abundant anti-inflammatory adipokine, adiponectin, has been documented to play a central role in ASDs and associated disorders, such as atherosclerosis [21], diabetes [22], obesity [23], panic disorders [24], and cardio-metabolic diseases [25].
In the past, some researchers have investigated the correlation of blood levels of adipokines with ASDs. They report elevated levels of leptin, ghrelin, resistin, and visfatin, along with decreased levels of adiponectin, retinol-binding protein 4, and progranulin were found to be associated with an increased risk of or were correlated with ASD [26]. We aim to write a review that is not only more updated than the previous reviews but also has a primary focus on adiponectin. Further, this paper also discusses the probable role of adiponectin in the pathogenesis of ASDs. The review also provides a synopsis of similar data for other adipokines and biologically plausible factors underlying ASDs.
Methods
We followed PRISMA guidelines to perform the data review. Data searches were performed on PubMed, Google Scholar, and Cochrane using the keywords; adiponectin, ASD, autism, autistic disorder, and a combination of these. The initial screening revealed (Autism Spectrum Disorder = 45,662 results, adiponectin = 22,928, and serum adiponectin = 7,440, but the focused search narrowed down to relevant articles, for example, the detailed search strategy used to get those 12 articles (on PubMed) was, “(“arthropod struct dev“[Journal] OR “agron sustain dev“[Journal] OR “asd“[All Fields] OR (“autism spectrum disorder“[MeSH Terms] OR (“autism“[All Fields] AND “spectrum“[All Fields] AND “disorder“[All Fields]) OR “autism spectrum disorder“[All Fields])) AND (“adiponectin“[MeSH Terms] OR “adiponectin“[All Fields] OR “adiponectin s“[All Fields] OR “adiponectine“[All Fields] OR “adiponectins“[All Fields] OR “GBP-28“[All Fields] OR “apM1“[All Fields] OR “AdipoQ“[All Fields] OR “Acrp30“[All Fields])”.
Inclusion criteria
All English-language studies published with data on the relationship between blood adiponectin levels and ASDs were selected. Data were extracted as the mean difference between blood adiponectin levels in children with and without ASDs. Since the mean differences were already adjusted, no meta-regression analysis was attempted. Observational studies, including cross-sectional or prospective studies, were eligible for this review. However, case reports, case series, duplicates, and reviews were excluded.
Sensitivity analysis
Quality assessments were conducted using the Newcastle-Ottawa Scale (NOS) [27] for the prospective studies, while the Modified Newcastle-Ottawa Quality Assessment Scale [28] was employed for the cross-sectional studies. Two reviewers independently (T, M, and A, M) conducted the analysis, and the discrepancies were sorted through discussion, till a consensus was reached.
Results
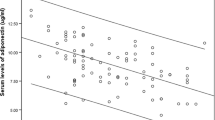
The screening and selection strategy for the studies is outlined in Fig. 1. Six studies were identified, meeting the inclusion criteria. Extracted data from these studies were pooled for analysis (Table 1). Subjects’ composition for each study is as follows: The first study [29] had a sample size of 62 males, 31 with autism, and 31 healthy age-matched controls. There was a statistically significant (p = 0.005) decrease in adiponectin levels in the group of males having autism (11.0 ± 4.0) as compared to healthy males (14.5 ± 5.3). In addition, an inverse association was also found between adiponectin levels and domain A scores on Autism Diagnostic Interview-Revised (ADI-R) [30]. Next study [31] compared 35 children with autism and 35 healthy controls with a one-year follow-up. No significant association was observed between ASDs or autistic symptoms and adiponectin levels. Essa et al. 2011 [32] had a sample size of 38 (19 Autistic and 19 normal children). There were significantly lower levels of adiponectin in Omani children with ASDs as compared to controls (p < 0.0001). The study by Rodrigues et al. [33] had a sample size of 49, (ASD = 30, Neurotypical = 19). Although no significant difference in adiponectin levels was found between neurotypical (12.91 ± 0.12) and autistic children (12.20 ± 0.38), the study did find a negative correlation between adiponectin levels and autistic scores on the Social Responsiveness Scale (SRS) [34]. Raghavan et al. 2018 [35] had a total sample of 847 [Neurotypical = 792; ASD = 55]. This study reported a significant inverse relationship between adiponectin levels and risk for ASDs. The childhood levels were only significantly correlated with risk for ASDs after controlling for age and other covariates. Quan et al. 2021 [36] compared 88 children with ASD with 88 normal children. The difference in adiponectin levels between the two groups was significant (t = 7.169, p < 0.001). This study also documented an inverse correlation between blood adiponectin levels and scores on Childhood Autism Rating Scale (CARS) [37] (Table 1). One of the reviewed studies [32] was of low quality, two were of moderate quality [31, 33], and three studies [29, 35, 36] were of decent quality (Table 2).
Discussion
This, to our knowledge, is the first systematic review to investigate the association between adiponectin levels and the risk of ASDs. Out of six studies reviewed, four studies reported a negative correlation between autism and adiponectin levels [29, 32, 35, 36]. Lower adiponectin levels in subjects with autism than the matched controls were first reported by Fujita-Shimizu and colleagues [29] with no group differences in body weight, height, waist circumference, or BMI (Table 1). However, the next study [31] did not observe any significant differences in adiponectin levels between ASD patients and controls. But the study by Essa et al. [32] replicated the findings from the first study in Omani children and showed an inverse relationship between adiponectin levels and those with ASD. The study by Rodrigues et al. [33] was another study that did not show a negative relationship between adiponectin levels and ASD patients. The next study [35] was the first to prospectively report an inverse association between ASD risk and adiponectin levels in the blood during early childhood. However, the association between early childhood adiponectin and ASD was less robust and achieved significance only after stepwise adjustments for potential confounders. The correlation between adiponectin and ASD parallels an increase in adipose tissue that switched into a negative correlation after birth [38]. Other studies have also reported a positive relationship of adipose tissue with adiponectin [39] converting into a negative association with adiponectin in early childhood [40, 41]. The last study by Quan et al. [36] replicated findings from prior studies [29, 32], reporting lower adiponectin levels in patients with ASDs than controls.
Although Rodrigues et al. [33] did not find a negative association between adiponectin levels and ASDs in their study subjects, they did report an inverse correlation between blood adiponectin levels and severity of autistic symptoms, as assessed with the Social Responsiveness Scale (SRS) [42]. Fujita-Shimizu and Colleagues [29] also reported an inverse correlation between adiponectin levels and autistic symptoms of abnormalities in social interactions, as assessed with the Autism Diagnostic Interview-Revised (ADI-R) [30]. Interestingly, the adiponectin levels were not correlated with autistic symptoms of repetitive behaviors and restricted interests but with social [29]. These findings suggest that low adiponectin levels may not affect all autistic symptoms. Another reviewed study [36], supported an inverse correlation between adiponectin levels and symptom severity as assessed with Childhood Autism Rating Scale (CARS) [37]. However, in one of the reviewed studies, adiponectin levels were not associated with ASDs or the severity of autistic symptoms [31].
In addition to adiponectin, autism has also been associated with changes in other adipokines, such as leptin. The study by Blardi et al. [31] found higher blood levels of leptin in autistic patients than in controls over one year without any differences in adiponectin levels, which is consistent with findings from an earlier study [43]. However, gender differences in leptin levels in females [44] were not reported in the study by Blardi et al. [31]. Also, increased leptin levels were not associated with obesity, suggesting that leptin may have effects beyond adipose tissue and energy balance [31]. The inverse relationship between adiponectin and ASDs has also been reported in other neurodevelopmental disorders, such as Fragile X Syndrome [45]. These findings suggest that adiponectin may have a larger role in neurodevelopment rather than merely regulating energy expenditure or serving as a biomarker for the onset of metabolic syndrome [46, 47]. Any imbalance in adiponectin-mediated anti-inflammatory effects [48] and/or leptin-mediated proinflammatory effects [49, 50] may alter the immune response increasing the risk for ASDs. This immune dysfunction is supported by an inverse relationship between leptin and adiponectin in autistic children [33, 47]. In addition, like adiponectin, leptin can have direct brain effects as it can cross the blood–brain barrier [51]. Another adipokine involved in ASDs may be resistin, which has more potent proinflammatory effects than leptin [52]. Although one of the reviewed studies [33] reported decreased levels of resistin, other studies have reported an increase in resistin levels20, supporting a more enhanced inflammatory response underlying ASDs [51]. In addition to ASDs, altered levels of adipokines have also been reported in other brain disorders, such as bipolar disorder [53] and Alzheimer’s dementia [54]. These variations in adipokine levels across different neuropsychiatric disorders may reflect biological differences underlying these diseases. Further, the clinical heterogeneity observed in autism may be attributed to the diverse content in its etiology because there has been a significant correlation between the variation (decrease) in blood adiponectin levels and the severity of clinical symptoms as in the study by Quan et al. [36] where higher blood adiponectin levels were associated with milder clinical severity. This warrants further, focused, research on the neurobiology and undiscovered mechanisms, that affect clinical severity on the social responsiveness scale.
Although the biological mechanisms underlying adiponectin changes are not fully understood, prior studies have hypothesized multiple explanations. One of the most plausible explanations in the reviewed studies is provided by an inflammatory basis of ASDs [29, 32, 33, 35, 36]. In this context, the anti-inflammatory role of adiponectin in suppressing proinflammatory cytokines, such as TNF-α, IL-6 [55, 56], and Interferon (IFN)-γ [56, 57], that are elevated in ASD [56, 58, 59].
According to recent research, oxidative stress and variation in genes encoding antioxidant enzymes may have a role in the development of ASD [60]. A study showed that adiponectin leads to a decrease in mitochondrial ROS formation and oxidative DNA damage thereby lowering the odds of developing ASDs. It also improves mitochondrial dysfunction by boosting Bcl-2 levels and inhibiting the production of active caspase-3 and Bax [61]. The biological relevance of adiponectin’s role in ASD could also be explained by the disturbances in the metabolic pathways like folate, tetrahydrobiopterin, and glutathione-dependent redox metabolism that are seen in children with ASDs [62]. Adiponectin protects against inflammatory reactions linked to metabolic abnormalities (metaflammation) such as obesity or insulin resistance [57], hence playing a role against the metabolic derangements in ASDs.
Adiponectin has also been proposed to promote neuroplasticity, perhaps mediated by a similar mechanism as the ketamine-induced nitric oxide synthase signal pathway, which also mediates rapid antidepressant effects [55, 63]. Adiponectin crosses the blood-brain barrier [64], and modifies neuronal activity in several brain regions where it has neuroprotective and neurotrophic effects. Studies have shown that adiponectin can mediate its neuroprotective effects in the hippocampus [65], hypothalamus, cortex, and pituitary glands [55, 63] by entering the brain circulation [63, 66]. For example, in the hippocampus, adiponectin is involved in neurogenesis, dendritic spine remodeling, and hippocampal stem cell proliferation [65, 66]. Abnormal development of the dentate gyrus of the hippocampus is likely implicated in the pathophysiology of ASD [67]. In addition, these hippocampal changes may play an important role in maintaining mental health. A study found that an increase in adiponectin levels exerts powerful antidepressant and anxiolytic effects, particularly by fighting against neuroinflammation [68]. In this context, decreased adiponectin levels have been associated with clinically significant affective episodes [69] and increased sympathomimetic activity, as observed in depression [70]. While an increase in adiponectin has been associated with antidepressant and anxiolytic effects, perhaps due to its anti-inflammatory effects [68].
Overall, having such a broad-spectrum proforma and being the most abundant adipokine, adiponectin may contribute to metabolic and immune homeostasis via adipocyte-brain communications [63]. However, findings from this review warrant a cautious interpretation as they are based on six small sample studies. Since all reviewed studies were observational, no causality relationship can be claimed, particularly in the presence of multiple confounding factors.
Conclusions
This review provides preliminary evidence for the ASDs and severity of autistic symptoms associated with altered levels of adipokines, particularly adiponectin. However, the inconsistent results from some studies could be explained by the biological heterogeneity across ASDs, smaller study samples, and less-than-optimal study designs. These shortcomings can be addressed by prospective longitudinal studies in larger samples with a broader age spectrum to validate the results from this review. An even better strategy would be to develop neurobiological and genetic predictors for early diagnosis and treatment response to optimize disease prognosis by using a translational neuroscience approach.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Grove J, Ripke S, Als TD, et al. Identification of common genetic risk variants for autism spectrum disorder. Nat Genet. 2019;51(3):431–44.
Baio J, Wiggins L, Christensen DL, et al. Prevalence of Autism Spectrum Disorder among children aged 8 years - Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2014. MMWR Surveill Summ. 2018;67(6):1–23.
Bolte S, Girdler S, Marschik PB. The contribution of environmental exposure to the etiology of autism spectrum disorder. Cell Mol Life Sci. 2019;76(7):1275–97.
Pandey S, Sharma C. Perceived Burden in caregivers of children with Autism Spectrum Disorder. J Nepal Health Res Counc. 2018;16(2):184–9.
Zhou T, Wang Y, Yi C. Affiliate stigma and depression in caregivers of children with Autism Spectrum disorders in China: effects of self-esteem, shame and family functioning. Psychiatry Res. 2018;264:260–5.
Elder JH, Kreider CM, Brasher SN, Ansell M. Clinical impact of early diagnosis of autism on the prognosis and parent-child relationships. Psychol Res Behav Manag. 2017;10:283–92.
Ramaswami G, Geschwind DH. Genetics of autism spectrum disorder. Neurogenetics, part I. Elsevier; 2018. pp. 321–9.
Yasuda Y, Matsumoto J, Miura K, Hasegawa N, Hashimoto R. Genetics of autism spectrum disorders and future direction. J Hum Genet [Internet]. 2023 [cited 2023 A.
Chen J, Xin K, Wei J, Zhang K, Xiao H. Lower maternal serum 25(OH) D in first trimester associated with higher autism risk in Chinese offspring. J Psychosom Res. 2016;89:98–101.
Chess S. Autism in children with congenital rubella. J Autism Child Schizophr. 1971;1(1):33–47.
Zerbo O, Traglia M, Yoshida C, et al. Maternal mid-pregnancy C-reactive protein and risk of autism spectrum disorders: the early markers for autism study. Transl Psychiatry. 2016;6(4):e783.
Shi L, Fatemi SH, Sidwell RW, Patterson PH. Maternal influenza infection causes marked behavioral and pharmacological changes in the offspring. J Neurosci. 2003;23(1):297–302.
Boulanger LM, Shatz CJ. Immune signalling in neural development, synaptic plasticity and disease. Nat Rev Neurosci. 2004;5(7):521–31.
Braunschweig D, Ashwood P, Krakowiak P, et al. Autism: maternally derived antibodies specific for fetal brain proteins. Neurotoxicology. 2008;29(2):226–31.
Pandey GK, Vadivel S, Raghavan S, Mohan V, Balasubramanyam M, Gokulakrishnan K. High molecular weight adiponectin reduces glucolipotoxicity-induced inflammation and improves lipid metabolism and insulin sensitivity via APPL1-AMPK-GLUT4 regulation in 3T3-L1 adipocytes. Atherosclerosis. 2019;288:67–75.
Hansen-Pupp I, Hellgren G, Hard AL, Smith L, Hellstrom A, Lofqvist C. Early Surge in Circulatory Adiponectin is Associated with Improved Growth at Near term in very Preterm infants. J Clin Endocrinol Metab. 2015;100(6):2380–7.
Nguyen TMD. Adiponectin: Role in Physiology and Pathophysiology. Int J Prev Med. 2020;11:136.
Vykoukal D, Davies MG. Vascular biology of metabolic syndrome. J Vasc Surg. 2011;54(3):819–31.
Ashwood P, Enstrom A, Krakowiak P, et al. Decreased transforming growth factor beta1 in autism: a potential link between immune dysregulation and impairment in clinical behavioral outcomes. J Neuroimmunol. 2008;204(1–2):149–53.
Ghaffari MA, Mousavinejad E, Riahi F, Mousavinejad M, Afsharmanesh MR. Increased Serum Levels of Tumor Necrosis Factor-Alpha, Resistin, and Visfatin in the children with Autism Spectrum disorders: a case-control study. Neurol Res Int. 2016;2016:9060751.
Shimada K, Miyazaki T, Daida H. Adiponectin and atherosclerotic disease. Clin Chim Acta. 2004;344(1–2):1–12.
Nishimura M, Morioka T, Hayashi M, et al. Plasma omentin levels are inversely associated with atherosclerosis in type 2 diabetes patients with increased plasma adiponectin levels: a cross-sectional study. Cardiovasc Diabetol. 2019;18(1):167.
Achari AE, Jain SK. Adiponectin, a therapeutic target for obesity, diabetes, and endothelial dysfunction. Int J Mol Sci 2017;18(6).
Unsal C, Hariri AG, Yanartas O, Sevinc E, Atmaca M, Bilici M. Low plasma adiponectin levels in panic disorder. J Affect Disord. 2012;139(3):302–5.
Lopez-Jaramillo P. The role of Adiponectin in Cardiometabolic diseases: effects of Nutritional interventions. J Nutr. 2016;146(2):422S–6.
Scott SR, Millwood SN, Manczak EM. Adipocytokine correlates of childhood and adolescent mental health: a systematic review. Dev Psychobiol. 2023;65(3):e22379. https://doi.org/10.1002/dev.22379.
Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45.
Norris JM, Simpson BS, Ball R, et al. A modified Newcastle-Ottawa Scale for Assessment of Study Quality in Genetic Urological Research. Eur Urol. 2021;79(3):325–6.
Fujita-Shimizu A, Suzuki K, Nakamura K, et al. Decreased serum levels of adiponectin in subjects with autism. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34(3):455–8.
Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24(5):659–85.
Blardi P, de Lalla A, Ceccatelli L, Vanessa G, Auteri A, Hayek J. Variations of plasma leptin and adiponectin levels in autistic patients. Neurosci Lett. 2010;479(1):54–7.
Essa MMA-SM, Al-Farsi YM, Ali A, Waly MI, Al-Shaffae MA, Gilles GJ. Reduced levels of adiponectin in Omani Autistic Children– a brief report. Int J Biol Med Res. 2011;2(3):793–5.
Rodrigues DH, Rocha NP, Sousa LF, Barbosa IG, Kummer A, Teixeira AL. Changes in adipokine levels in autism spectrum disorders. Neuropsychobiology. 2014;69(1):6–10.
Li C, Zhou H, Wang T, et al. Performance of the Autism Spectrum Rating Scale and Social Responsiveness Scale in identifying autism spectrum disorder among cases of intellectual disability. Neurosci Bull. 2018;34(6):972–80.
Raghavan R, Fallin MD, Hong X, et al. Cord and early childhood plasma adiponectin levels and autism risk: a prospective birth Cohort Study. J Autism Dev Disord. 2019;49(1):173–84.
Quan L, Zhao Y, Yi J, Shi XD, Zhong Y, Liu L. Serum adiponectin levels are reduced in autism spectrum disorder and association with severity of symptoms. Metab Brain Dis. 2021;36(3):491–8.
Schopler E, Reichler RJ, DeVellis RF, Daly K. Toward objective classification of childhood autism: Childhood Autism Rating Scale (CARS). J Autism Dev Disord. 1980;10(1):91–103.
Siahanidou T, Mandyla H, Papassotiriou GP, Papassotiriou I, Chrousos G. Circulating levels of adiponectin in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2007;92(4):F286–290.
Lenz AM, Diamond F. The importance of the adiponectin and leptin relationship in in utero and infant growth. Handbook of growth and growth monitoring in Health and Disease. Springer; 2012. pp. 2839–56.
Meyer DM, Brei C, Stecher L, Much D, Brunner S, Hauner H. Cord blood and child plasma adiponectin levels in relation to childhood obesity risk and fat distribution up to 5 y. Pediatr Res. 2017;81(5):745–51.
Mantzoros CS, Rifas-Shiman SL, Williams CJ, Fargnoli JL, Kelesidis T, Gillman MW. Cord blood leptin and adiponectin as predictors of adiposity in children at 3 years of age: a prospective cohort study. Pediatrics. 2009;123(2):682–9.
Constantino JN, Davis SA, Todd RD, et al. Validation of a brief quantitative measure of autistic traits: comparison of the social responsiveness scale with the autism diagnostic interview-revised. J Autism Dev Disord. 2003;33(4):427–33.
Ashwood P, Kwong C, Hansen R, et al. Brief report: plasma leptin levels are elevated in autism: association with early onset phenotype? J Autism Dev Disord. 2008;38(1):169–75.
Roemmich JN, Rogol AD. Role of leptin during childhood growth and development. Endocrinol Metab Clin North Am. 1999;28(4):749–64. viii.
Lisik MZ, Gutmajster E, Sieron AL. Plasma levels of Leptin and Adiponectin in Fragile X Syndrome. Neuroimmunomodulation. 2016;23(4):239–43.
Inami I, Okada T, Fujita H, et al. Impact of serum adiponectin concentration on birth size and early postnatal growth. Pediatr Res. 2007;61(5 Pt 1):604–6.
Blardi P, de Lalla A, D’Ambrogio T, et al. Long-term plasma levels of leptin and adiponectin in Rett syndrome. Clin Endocrinol (Oxf). 2009;70(5):706–9.
Nedvidkova J, Smitka K, Kopsky V, Hainer V. Adiponectin, an adipocyte-derived protein. Physiol Res. 2005;54(2):133–40.
Palhinha L, Liechocki S, Hottz ED, et al. Leptin induces proadipogenic and Proinflammatory Signaling in Adipocytes. Front Endocrinol (Lausanne). 2019;10:841.
Lago F, Dieguez C, Gomez-Reino J, Gualillo O. Adipokines as emerging mediators of immune response and inflammation. Nat Clin Pract Rheumatol. 2007;3(12):716–24.
Pan W, Kastin AJ. Adipokines and the blood-brain barrier. Peptides. 2007;28(6):1317–30.
Bokarewa M, Nagaev I, Dahlberg L, Smith U, Tarkowski A. Resistin, an adipokine with potent proinflammatory properties. J Immunol. 2005;174(9):5789–95.
Barbosa IG, Rocha NP, de Miranda AS, et al. Increased levels of adipokines in bipolar disorder. J Psychiatr Res. 2012;46(3):389–93.
Teixeira AL, Diniz BS, Campos AC, et al. Decreased levels of circulating adiponectin in mild cognitive impairment and Alzheimer’s disease. Neuromolecular Med. 2013;15(1):115–21.
Brochu-Gaudreau K, Rehfeldt C, Blouin R, Bordignon V, Murphy BD, Palin MF. Adiponectin action from head to toe. Endocrine. 2010;37(1):11–32.
Wei H, Alberts I, Li X. Brain IL-6 and autism. Neuroscience. 2013;252:320–5.
Mazaki-Tovi S, Romero R, Vaisbuch E, et al. Dysregulation of maternal serum adiponectin in preterm labor. J Matern Fetal Neonatal Med. 2009;22(10):887–904.
Chez MG, Dowling T, Patel PB, Khanna P, Kominsky M. Elevation of tumor necrosis factor-alpha in cerebrospinal fluid of autistic children. Pediatr Neurol. 2007;36(6):361–5.
Ashwood P, Krakowiak P, Hertz-Picciotto I, Hansen R, Pessah I, Van de Water J. Elevated plasma cytokines in autism spectrum disorders provide evidence of immune dysfunction and are associated with impaired behavioral outcome. Brain Behav Immun. 2011;25(1):40–5.
Mandic-Maravic V, Mitkovic-Voncina M, Pljesa-Ercegovac M, et al. Autism Spectrum disorders and Perinatal Complications-Is oxidative stress the connection? Front Psychiatry. 2019;10:675.
Li X, Guo H, Zhao L, et al. Adiponectin attenuates NADPH oxidase-mediated oxidative stress and neuronal damage induced by cerebral ischemia-reperfusion injury. Biochim Biophys Acta Mol Basis Dis. 2017;1863(12):3265–76.
Frye RE, James SJ. Metabolic pathology of autism in relation to redox metabolism. Biomark Med [Internet]. 2014 [cited 2023 Aug 9];8(3):321–30. Available from: https://pubmed.ncbi.nlm.nih.gov/24712422/.
Thundyil J, Pavlovski D, Sobey CG, Arumugam TV. Adiponectin receptor signalling in the brain. Br J Pharmacol. 2012;165(2):313–27.
Formolo DA, Cheng T, Yu J, Kranz GS, Yau S-Y. Central adiponectin signaling– A metabolic regulator in support of brain plasticity. Brain Plast [Internet]. 2022 [cited 2023 Aug 8];8(1):79–96. Available from: https://pubmed.ncbi.nlm.nih.gov/36448043/.
Zhang D, Wang X, Lu XY. Adiponectin exerts neurotrophic effects on dendritic arborization, Spinogenesis, and neurogenesis of the Dentate Gyrus of male mice. Endocrinology. 2016;157(7):2853–69.
Ng RC, Chan KH. Potential Neuroprotective Effects of Adiponectin in Alzheimer’s Disease. Int J Mol Sci 2017;18(3).
Ito H, Morishita R, Nagata KI. Autism spectrum disorder-associated genes and the development of dentate granule cells. Med Mol Morphol. 2017;50(3):123–9.
Nicolas S, Chabry J, Guyon A, Zarif H, Heurteaux C, Petit-Paitel A. [Adiponectin: an endogenous molecule with anti-inflammatory and antidepressant properties?]. Med Sci (Paris). 2018;34(5):417–23.
Machado-Vieira R, Gold PW, Luckenbaugh DA, et al. The role of adipokines in the rapid antidepressant effects of ketamine. Mol Psychiatry. 2017;22(1):127–33.
Lehto SM, Huotari A, Niskanen L, et al. Serum adiponectin and resistin levels in major depressive disorder. Acta Psychiatr Scand. 2010;121(3):209–15.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
MA conceived the idea, did a literature search, and write-up, MK wrote the introduction, sensitivity analysis, and discussion, MT did Sensitivity Analysis, and MUS Significantly contributed to revising the whole manuscript, proof-read, and added to the discussion.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Competing interests
No competing interests for all authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ali, M., Kamran, M., Talha, M. et al. Adiponectin blood levels and autism spectrum disorders: a systematic review. BMC Psychiatry 24, 88 (2024). https://doi.org/10.1186/s12888-024-05529-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-05529-1