Abstract
Background
Aripiprazole is a second-generation antipsychotic, efficacious in patients with schizophrenia during acute episodes. Due to its pharmacological profile, aripiprazole may be of interest in patients with specific clinical profiles who have not been studied extensively in randomised clinical trials.
Objectives
To capture experience with aripiprazole in everyday psychiatric practice using the Delphi method in order to inform decision-making on the use of aripiprazole for the treatment of patients with schizophrenia in clinical situations where robust evidence from clinical trials is lacking.
Methods
The scope of the survey was defined as the management of schizophrenia in adults. A systematic literature review was performed to identify the different clinical situations in which aripiprazole has been studied, and to describe the level of clinical evidence. Clinical profiles to include in the Delphi survey were selected if there was a clear interest in terms of medical need but uncertainty over the efficacy of aripiprazole. For each clinical profile retained, five to seven specific statements were generated and included in a questionnaire. The final 41-item questionnaire was proposed to a panel of 406 French psychiatrists with experience in the treatment of schizophrenia. Panellists rated their level of agreement using a Likert scale. A second round of voting on eleven items was organised to clarify points for which a consensus was not obtained in the first round.
Results
Five clinical profiles were identified in the literature review (persistent negative symptoms, pregnancy, cognitive dysfunction, addictive comorbidity and clozapine resistance). Sixty-two psychiatrists participated in the first round of the Delphi survey and 33 in the second round. A consensus was obtained for 11 out of 41 items in the first round and for 9/11 items in the second round. According to the panellists’ clinical experience, aripiprazole can be used as maintenance treatment for pregnant women, is relevant to preserve cognitive function and can be considered an option in patients with a comorbid addictive disorder or with persistent negative symptoms.
Conclusion
These findings may help physicians in choosing relevant ways to use aripiprazole and highlight areas where more research is needed to widen the evidence base.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Second-generation antipsychotic drugs (SGAs) were introduced over twenty years ago for the treatment of schizophrenia. These agents are now generally considered to be the preferred treatments for the management of schizophrenia due to their lower propensity to cause extrapyramidal side-effects compared to first-generation antipsychotics (FGAs), such as haloperidol [1]. Aripiprazole is an SGA that is relatively selective for the D2 dopamine receptor, at which it acts as a partial agonist [2,3,4]. It has also been suggested that aripiprazole may selectively interact with dopamine pathways involved in salience attribution and in psychotic manifestations rather than in motor function [5], which may help explain its clinical profile. This selectivity may result from the ability of partial agonists such as aripiprazole to stabilise a different molecular conformation of the D2 receptor upon binding compared to full agonists or antagonists. As a consequence, a particular subset of downstream signalling pathways is selectively activated [6, 7]. This concept has been termed ‘biased agonism’ and may be a fertile approach for future innovative drug development [8, 9].
The original pharmacological profile of aripiprazole may have consequences for its clinical profile. For instance, there is also some evidence that aripiprazole improves quality of life to a greater extent than certain SGAs [10]. Importantly, the adverse event profile of aripiprazole is different from that of some of the mixed dopamine-serotonin antagonists [11,12,13]. In addition, it has been postulated that it may be of particular use in certain specific clinical domains, such as in patients with persistent negative symptoms, comorbid substance abuse or in partial responders to other antipsychotic drugs [14, 15]. Although the utility of aripiprazole in some of these situations has been well established from randomised clinical trials [13], in others high-level evidence is missing, and existing practice guidelines provide no guidance. Moreover, the overall profile of the clinical domains in which aripiprazole is used in everyday clinical practice remains unclear [14]. Evidence-based medicine, however, integrates the most robust published evidence with individual clinical experience and patient preferences [16], and drawing on the experience of psychiatrists who use aripiprazole in their everyday clinical practice may provide useful guidance on how this medication may best be used.
The objective of this study was to capture experience with aripiprazole in psychiatric practice in order to shed light on some of these less well-documented aspects of the clinical profile of aripiprazole. To this end, we have performed a Delphi survey of practicing psychiatrists in France based on a targeted literature review.
Methods
In order to address the appropriateness of the use of aripiprazole in different clinical domains, we performed a Delphi survey of hospital-based psychiatrists in France. The implementation of the study was overseen by a scientific committee of eleven psychiatrists (the authors), who designed the Delphi questionnaire and interpreted the findings. These experts were all hospital-based, and were selected due to their experience in the field of schizophrenia and antipsychotics. The study was sponsored by Lundbeck France and Otsuka Pharmaceutical France, who performed the targeted literature review.
The study involved three consecutive and complementary approaches. In the first step, a review of the literature was performed by the study sponsors in order to identify the different clinical domains in which aripiprazole has been studied in adult patients with schizophrenia, and the strength of the clinical evidence was assessed.
In a second step, the results of the literature review were circulated to all members of the scientific committee, who met to choose the clinical domains to be presented to the Delphi panel. These domains were selected on the basis of the level of clinical evidence, their own clinical experience and the medical needs using a Metaplan® approach. This is a visualisation technique for facilitating decision-making in group discussions [17]. For the agreed domains, the scientific committee formulated specific questions relating to how aripiprazole is used in everyday clinical practice to be presented to participants in the Delphi survey.
The third step consisted of the Delphi survey itself, which was performed between October 2020 and March 2021. Participants were recruited from all sectors of the French healthcare system (public and private; general hospital or psychiatric hospital), with the exception of full-time community-based psychiatrists who were excluded as they typically do not treat patients with schizophrenia. The scope of the survey was defined as the suitability of aripiprazole treatment in a selection of specific clinical domains in the management of schizophrenia in adults.
The Delphi survey method is a procedure for building an expert consensus originally developed by the RAND Corporation in the 1950s [18, 19], widely used in medical research for building a consensus based on expert opinion and practice where high-level evidence from interventional studies is unavailable [20, 21]. A panel of experts is recruited and asked to indicate their level of agreement with a range of propositions. In the most frequent application of the method, this is done using a visual analogue, numerical or Likert scale. The process is iterative, with the propositions being adapted between rounds in order to facilitate achieving a consensus. Panellists never meet and complete the survey individually, which limits the possibility of concertation or herd effects. The development of web-based surveys over the last twenty years has facilitated the implementation and use of Delphi surveys. In the field of mental health, the Delphi method has been frequently applied to pragmatic research questions that may not be addressed specifically by randomised clinical trials [22,23,24,25].
Study participants
Potential panellists were identified from professional listings of psychiatrists in France working in public or private hospitals or clinics. Psychiatrists working full-time in the community were not eligible. Panellists did not receive remuneration for their participation. We used an iterative random selection process, adjusted by département (French administrative geographical division of the country). We initially fixed a target of 60–70 participants, in order to ensure that around thirty completed both rounds of the survey, which is considered an appropriate number to optimise the reliability of the output of the group [18]. We then selected 400 psychiatrists at random from the listing, weighted by the total number of psychiatrists in each département, who were contacted by e-mail. This process was repeated with additional batches of psychiatrists at two-weekly intervals until the target number of 60–70 participants was achieved at which time the survey was closed. A reminder e-mail was sent two weeks after the original contact. A total of four batches of invitations was required. The participant invitation lists were drawn up and managed by the study moderator and the identities of the participants were not communicated to the scientific committee or to the study sponsor.
Literature search
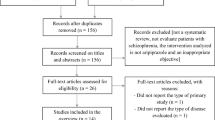
In order to identify potential items for the questionnaire, a systematic literature search was performed in the Medline database using the PRISMA methodology [26]. The goal of this search was to identify clinical situations in which the use of aripiprazole in schizophrenia in adults had been evaluated. All formulations of aripiprazole (oral tablets, intramuscular injectable and depot formulations) were considered in the literature review. The search terms used are listed in Table 1 and a PRISMA flow diagram of the selection process is provided in the Supplementary Information (Additional Fig. 1). Titles and abstracts of the identified publications were screened for relevance by two independent reviewers. Full texts of retained publications were individually reviewed to assess eligibility and the selection validated by an independent reviewer. References of retained publications were checked manually to ensure that no relevant publications had been missed. Any disagreements were discussed and, where possible, resolved by consensus. In a next step, the retained articles were classified by clinical domain and were ranked by evidence grade according to the classification system used by the French health authorities [27] (provided in the Supplementary Information: Additional Table 1). The retained publications were grouped into fourteen clinical domains.
Selection of themes and development of the questionnaire
For each of the fourteen clinical domains, the scientific committee voted on how appropriate the use of aripiprazole was, on the basis of the strength of the available evidence and their own clinical experience. For each domain, each member of the committee chose between situations in which the use of aripiprazole is clearly appropriate, those in which it is clearly not appropriate, and those in which there is a doubt. The scientific committee then prioritized the domains for which the majority of members considered that, in terms of the published evidence, there was a doubt concerning the utility of aripiprazole but where there was a clear interest in terms of medical need. Five domains were selected as being related to a significant unmet clinical need and thus the most important to include in the questionnaire (Table 2). The number and type of publications identified in the literature review which are relevant to these five themes are listed in the Supplementary Information (Additional Table 2).
Finally, for each of the five retained clinical domains, between five and seven specific questions were generated using the Metaplan® method. Each question was formulated in the following way: ‘According to your own clinical experience in the treatment of an adult patient with schizophrenia, aripiprazole is an appropriate treatment option for…’. The final questionnaire contained 28 questions, some of which had subsidiary questions (41 items in all).
Implementation of the survey
The Delphi questionnaires were administered and the data collected by an independent moderator, who was the only person who knew the identity of the panellists and had access to the individual votes. The moderator used a web-based survey software (Survey Monkey®) to invite psychiatrists to participate, to deliver the questionnaire and to collect and compile the ratings.
The study questionnaire opened with a series of screening questions to ensure that the panellist had the required experience. In order to proceed with the survey, panellists were required to confirm that they were a psychiatrist treating adult patients with schizophrenia, prescribing atypical antipsychotics, working in the hospital sector, and seeing patients in at least three of the five clinical domains of interest in the survey. The questionnaire opened with a series of questions collecting background information on the panellist (age, gender, geographical region, place and size of practice, and involvement in teaching or research activities). This was followed by the 28 questions about aripiprazole formulated as a statement for which panellists rated their level of agreement on a numerical scale from one to nine. An option of ‘no experience in this domain’ was also available, but this was never used. A free-text box was available for participants to comment on their response or on the question, if they so wished. It was not possible to skip questions. Participants could close the survey at any time and return to it when they wished.
A score of 1 – 3 was considered to indicate disagreement, a score of 7 – 9 agreement and a score of 4 – 6 undecided. Replies to the questionnaire were compiled and the proportion of panellists in agreement (or disagreement) with each statement was calculated. There is no established threshold for identifying consensus in Delphi surveys although agreement of 80% of participants is widely used [28]. However, in the present study, a low overall level of consensus was anticipated because the questions chosen were those for which the scientific committee considered that there was no clear answer; for this reason, a less stringent threshold of 65% agreement was applied. The statements reaching consensus using this criterion were identified and retained. For statements for which 50% – 65% of panellists were in agreement, the statements were rephrased for the second round.
In the second round, eleven reformulated statements were proposed to the panellists, who were asked whether they agreed or disagreed with the statement (binary choice). Replies were compiled and the proportion of panellists in agreement was calculated. Statements with which ≥ 65% of panellists agreed were considered consensual.
Results
Participants
In the first round, 406 psychiatrists who were sent the invitation opened the electronic mail, 84 of whom (20.7%) entered the Survey Monkey® interface. Of these, five refused to participate and a further seventeen either did not fulfil the eligibility criteria or did not reply to any of the questions about aripiprazole. Of the remaining 62 psychiatrists starting the questionnaire, 52 completed it (83.9%). For the second round, an invitation was sent to the 62 panellists who started the questionnaire during the first round. Of these, 49 opened the mail, 34 entered the survey interface and 33 completed the questionnaire.
The characteristics of the participants are presented in Table 3. Panellists were most frequently under 40 years old, with nine aged ≥ 60 years. The majority were men. Thirty-two had a teaching activity and sixteen were involved in research.
Persistent negative symptoms
In the first round, five questions were put to the panel corresponding to different presentations of negative symptoms (Additional Table 3). Each question had two sub-questions, concerning switching of antipsychotic medication to aripiprazole on the one hand and augmentation therapy with aripiprazole on the other. Three questions obtained a consensus with respect to switching and one with respect to augmentation (Table 4). In the second round, two questions were presented (Additional Table 3), both of which achieved consensus (Table 4). Examples of verbatim obtained for this theme are provided in Additional Table 4.
Pregnancy
In the first round, six questions were put to the panel (Additional Table 3). Two of these received a consensus (Table 4). In the second round, four questions were presented (Additional Table 3), for three of which a consensus was obtained (Table 4). Examples of verbatim obtained for this theme are provided in Additional Table 4.
Cognitive dysfunction
In the first round, seven questions, some with sub-questions, relating to cognitive symptoms were put to the panel (Additional Table 3). Two questions obtained a consensus in this round (Table 4). In the second round, a further two questions were presented (Additional Table 3), one of which achieved consensus (Table 4). Examples of verbatim obtained for this theme are provided in Additional Table 3.
Addictive comorbidity
In the first round, seven questions were put to the panel (Additional Table 3). Two of these received a consensus (Table 4). In the second round, two questions were presented (Additional Table 3), both of which achieved consensus (Table 4). Examples of verbatim obtained for this theme are provided in Additional Table 4.
Augmentation therapy for clozapine resistance
In the first round, four questions were put to the panel relating to patients resistant to clozapine therapy (Additional Table 3). Certain questions had two or three sub-questions. One question obtained a consensus (Table 4). In the second round, a single question was presented (Additional Table 3), which achieved consensus (Table 4). Examples of verbatim obtained for this theme are provided in Additional Table 4.
Discussion
The Delphi survey identified a relatively limited number of consensus statements on the themes of interest in the study. These consensus points nevertheless identify a number of clinical domains where, in spite of the limited published data available, participants feel, based on their own clinical experience, comfortable about the use of aripiprazole. These are reviewed by theme hereunder.
Persistent negative symptoms
Negative symptomatology constitutes an important dimension of schizophrenia and its adequate management remains an important unmet medical need in the treatment of schizophrenia [29,30,31,32]. Patients with pronounced negative symptoms tend to be less functional and have poorer outcomes than those in whom such symptoms are milder [11, 33,34,35,36,37]. It has been clear for several decades that negative symptoms respond less well to antipsychotic medication than acute psychotic symptoms. Over forty years ago, it was recognised that FGAs did not markedly improve negative symptoms, and could even potentially aggravate these symptoms [38, 39]. These observations contributed to the search for antipsychotics with a broader pharmacological profile and to the development of SGAs. However, the clinical benefit of these SGAs in patients with persistent negative symptoms has been a matter of debate [40,41,42,43]. Indeed, recent epidemiological findings suggest that around one-half of otherwise well-controlled patients taking an established antipsychotic treatment present with persistent residual negative symptoms [34]. As a partial agonist, aripiprazole is of interest for treating both the positive and negative dimensions of the disorder.
The Delphi panellists achieved consensus that aripiprazole is an appropriate treatment option in patients with persistent negative symptoms. For treating patients with blunted affect, a dopamine receptor partial agonist was considered a promising choice. In general, panellists thought that it would be more appropriate to treat patients presenting with persistent negative symptoms with an antipsychotic in monotherapy than in combination. Consequently, in a patient with residual negative symptoms on the current antipsychotic, a switch to aripiprazole was preferred to augmentation therapy. There is no information in the literature to support the use of augmentation with aripiprazole except in the context of clozapine resistance [44] (see below). With respect to switching to monotherapy with aripiprazole, only one comparative prospective study has been published, but this is very poorly documented; it reported improvements in the negative subscale of the Positive and Negative Syndrome Scale (PANSS) in patients treated with aripiprazole [45]. On the other hand, several case reports have been published that describe benefits on negative symptoms following a switch to aripiprazole [46,47,48]. Several panellists also stated that they would initially attempt to manage depressive or anxious symptoms by prescribing an antidepressant or anxiolytic rather than by changing antipsychotic medication. There is no information in the literature concerning the sequencing of antidepressant/anxiolytic treatment and aripiprazole in the literature (Table 5).
Pregnancy
Pregnancy and the peripartum period present a number of risks to women with schizophrenia treated with antipsychotic medication. Discontinuing treatment may result in re-emergence of psychotic episodes which may endanger the mother or baby (or both), whereas continuing treatment may expose mother and baby to drug-related adverse events. In addition, compared to the general population, women with schizophrenia more frequently present pregnancy risk factors, such as smoking during pregnancy, poor nutritional status, alcohol or recreational drug use, and high body mass index [49,50,51]. In addition, women with schizophrenia may have poor knowledge of contraceptive methods and little involvement in contraceptive decisions, and for this reason, be more likely to have unplanned or unwanted pregnancies [52,53,54]. For most stable patients, well-controlled on their medication, the discontinuation of treatment in women treated for schizophrenia, before or during pregnancy, is associated with a high risk of a new psychotic episode, notably in the case of abrupt termination of treatment [55]. The presence of maternal psychotic symptoms at birth is likely to interfere with the mother’s ability to care for the new-born child and may be detrimental to establishing a healthy bond between mother and infant [56,57,58,59]. Estimating the risks associated with use of SGAs during pregnancy is difficult, since pregnant women are excluded from randomised clinical trials and no large prospective pregnancy registries have been initiated in schizophrenia. Certain SGAs have metabolic and cardiovascular effects that may be of relevance in pregnancy, including gestational diabetes [60,61,62,63] and perinatal cardiac rhythm disturbances [64]. Given the limited amount of evidence, it is difficult to appreciate whether SGAs carry any teratogenic risk in humans, although, if it exists, this risk is likely to be low [50, 65,66,67,68,69]. An increased risk of congenital malformations has been reported in women exposed to risperidone or olanzapine [70, 71]. Whether exposure to antipsychotics in utero exposes the child to any neurodevelopmental toxicity is unknown [72], although there is no evidence for any deleterious psychiatric outcome [73].
Delphi participants reached a consensus that treatment with aripiprazole could and should be maintained during pregnancy or in a patient who finds herself pregnant, as long as psychiatric symptoms are adequately controlled. This is supported by the limited amount of published data available. Recent data from the National Pregnancy Registry for Atypical Antipsychotics in the USA found no elevated risk of major malformations in infants born to mothers exposed to aripiprazole during pregnancy [74], and this was also the conclusion of a number of smaller cohort studies [71, 75, 76]. A small number of case reports of aripiprazole exposure during pregnancy or lactation have been described, which have involved different aripiprazole doses, different lengths of treatment, and different timings of prenatal exposure [77,78,79,80,81,82,83,84,85]. Most of these have described uneventful pregnancies resulting in a healthy baby [77,78,79,80, 82, 84, 85]. Nonetheless, there have been reports of foetal tachycardia [81] and transient breathing difficulties [83] in infants exposed to aripiprazole in utero during late pregnancy. Small case series of pregnancies exposed to aripiprazole have also reported a slightly shorter gestation and lower birth weight, and a mildly elevated risk of gestational hypertension [86], as well as a possible signal of miscarriage [87]. Nonetheless, attribution of causality in these cases was not clear. There was no agreement between participants as to the utility of switching to aripiprazole in a patient well-controlled on another antipsychotic or on switching between depot and oral formulations of aripiprazole. Although a majority of panellists agreed that treatment with aripiprazole could be continued right up to delivery, some felt that it should be discontinued in the last month if the clinical state of the patient allowed. With respect to breastfeeding, transfer of aripiprazole has been demonstrated across the placenta [83, 85, 88] and also into breast milk [79, 89], so there is some potential for harmful effects on the foetus or the new-born (Table 6).
Cognitive dysfunction
Cognitive dysfunction is a fundamental aspect of schizophrenia, distinct from the positive and negative symptom domains [90, 91]. The severity of cognitive impairment is believed to be strongly associated with functional outcome and the ability to live an independent life [92, 93]. Effective management of cognitive dysfunction in schizophrenia is thus a crucial challenge for improving the long-term outcome of therapy. First-generation antipsychotics were perceived as having, at best, minimal effects on cognitive performance, and possibly even impairing performance [94, 95]. The introduction of the SGAs raised hopes that they would have a more incisive effect on cognitive function than the earlier generation of treatments [94, 96]. However, 25 years later, the real impact of SGAs on cognitive function remains a matter of debate [97,98,99]. In addition, it is probably simplistic to envisage SGAs as a homogeneous class, and there may be significant differences between drugs in terms of their response profile. In this respect, aripiprazole, which facilitates prefrontal dopaminergic neurotransmission [100], may be of interest to improve cognitive performance in schizophrenia.
The Delphi panellists supported the view that aripiprazole was a relevant treatment option for patients with schizophrenia presenting with cognitive dysfunction. In particular, they agreed that a switch to aripiprazole would be appropriate in patients with persistent cognitive dysfunction on their current antipsychotic medication. This opinion is consistent with the limited published data. The targeted literature search identified four studies that had evaluated the effects of aripiprazole on cognitive symptoms of schizophrenia and that could be graded as Evidence Level 2 [101,102,103,104]. All of these studies, which used a variety of paradigms, reported beneficial effects of aripiprazole on certain cognitive domains and some evidence of superiority with respect to risperidone or olanzapine. One of these studies reported benefits in the context of switching from an FGA to aripiprazole [103], and a second benefit following adjunctive treatment with aripiprazole in patients with persistent cognitive dysfunction on monotherapy with risperidone or olanzapine. However, patterns of improvement across cognitive domains were not consistent within or between studies, which makes it difficult to draw an unequivocal conclusion from them. In addition to these studies, a number of prospective or retrospective case series have been reported [47, 105,106,107,108,109], which all reported benefits on cognitive function of switching to aripiprazole. Panellists emphasised the importance of non-pharmacological approaches in addition to antipsychotic medication, and in particular cognitive remediation, for which the evidence base for efficacy is consistent [110]. This view is supported by findings from a prospective comparative study which evaluated the impact of combining cognitive remediation with aripiprazole or risperidone and reported a possible synergistic effect for aripiprazole [111] (Table 7).
Addictive comorbidity
The prevalence of comorbid addictive disorders in patients with schizophrenia is high compared to the general population, and many of these patients present with multiple addictions [112]. These patients are a particular challenge for the treating psychiatrist, as they may have poorer treatment persistence [113] and compliance [114], poorer symptom control [115] or more pronounced extrapyramidal symptoms [116], poorer prognosis [114, 117], higher mortality [118] and poorer social integration [115] than patients without addictive comorbidity. Treatment of patients with schizophrenia with FGAs may aggravate addictive comorbidity and compromise attempts to stop or reduce substance use [119, 120]. In contrast, there is evidence that certain SGAs may be beneficial in these patients [121] and possibly reduce craving and facilitate a reduction in substance use [122]. In this respect, aripiprazole is a particularly interesting candidate due to its partial agonist profile, which may allow a preserved hedonic response.
There was a consensus among the Delphi panellists that aripiprazole had a place in the management of patients with schizophrenia and a comorbid addictive disorder. However, they thought that it was difficult to generalise experiences and opinions across the many different types of addictive behaviour encountered in patients with schizophrenia. Certain panellists considered that the partial agonist properties of aripiprazole and its ‘pro-cognitive’ effects made it a promising candidate for the treatment of this type of patient. In everyday practice, panellists commented that, although aripiprazole treatment did reduce craving in some patients, this was not a consistent finding. Published randomised comparative clinical trials, on the other hand, have generally reported significant reductions in craving in patients treated with aripiprazole, for smokers [123], cocaine users [124] and cannabis users [125]. Similarly, uncontrolled cohort studies and case series or reports have also reported reductions in craving for various addictive substances following aripiprazole treatment [124, 126, 127]. In patients with a first psychotic episode and, as long as a diagnosis of schizophrenia could be made with confidence, panellists often prescribed aripiprazole to patients with a substance use disorder, particularly cannabis, in the hope that this medication would bring psychotic symptoms under control and help reduce substance abuse. There is very little published data on aripiprazole and cannabis addiction and the panellists’ experience is thus particularly valuable. A randomised naturalistic study comparing depot formulations of aripiprazole and paliperidone reported significantly greater reductions in craving in patients using cannabis following one years’ treatment with aripiprazole compared to paliperidone [125]. The only other published study that evaluated aripiprazole in this context was a retrospective case series in 17 cannabis users which reported no change in scores on the Severity of Dependence Scale after six months of treatment with the depot formulation [128]. There was a consensus that, in patients with an unresolved addictive disorder on their current antipsychotic, adjunctive treatment with aripiprazole in order to treat the addiction would not be an appropriate solution. If a patient’s symptoms were well-controlled on the current antipsychotic, then it may not always be appropriate to switch to aripiprazole just in the hope of having some impact on the addictive comorbidity. In contrast, if the patient was not well controlled and a switch of antipsychotic treatment was planned, then aripiprazole may be a suitable choice in this patient group. No clinical studies have yet addressed the effect of aripiprazole in different switching strategies in patients with addictive comorbidities under treatment with another antipsychotic. It was also stressed by several participants that the prescription of aripiprazole to a patient with an addictive comorbidity should not obviate the importance of providing a specific and appropriate treatment for the addictive disorder itself (Table 8).
Augmentation therapy for clozapine resistance
Perhaps up to half of patients with treatment-resistant schizophrenia (TRS) do not respond satisfactorily to clozapine [129] and these patients often have particularly severe disease [130]. Although a number of strategies have been proposed for treating patients with TRS who do not respond to clozapine, including augmentation with other antipsychotics, there is no consensus on which strategy represents the most beneficial approach [131,132,133]. Augmentation with aripiprazole may be of interest in this context.
Clozapine resistance is a complex issue and the treating physician's judgment may differ from that used in clinical studies. Resistance does not only relate to persistence of psychotic symptoms, but also to poor global functioning, persistent lack of initiative and involvement, as well as reduced social skills. These symptoms are the consequence of poor cognitive function, poor social involvement, poor reward capacities and lack of environmental stimuli. For the clinician, treatment decision-making in these cases is not limited to observation of insufficient improvement of measurable symptoms, but also to difficulty in restoring patient motivation and autonomy. In this respect, the choice of intervention in clozapine resistance may be driven by attitudes to resistance that are not easily quantified, and are based on a more pragmatic approach. This difference between outcomes used in clinical trials and physician judgement in real-world practice illustrates the interest of the Delphi method for guiding clinical practice.
Panellists considered that, if augmentation of clozapine with another SGA was being considered, then aripiprazole would be an attractive choice, since it has a complementary mechanism of action to clozapine. In addition, compared to certain other SGAs, aripiprazole carries a lower risk of metabolic side-effects [12], and is not likely to have a synergistic effect with clozapine on weight gain, dyslipidaemias and hyperglycaemia. Two systematic reviews have evaluated the interest of antipsychotic augmentation strategies in clozapine-resistant schizophrenia [129, 134], one conducted under the aegis of the Cochrane collaboration [135]. Both noted the limited number and poor quality of the available studies. The studies reviewed provided inconsistent information on the benefits of augmentation with aripiprazole. The Cochrane review identified one study demonstrating superiority of aripiprazole augmentation over quetiapine augmentation [136], and one study which reported no benefit [137]. In the second systematic review, aripiprazole and penfluridol, were the only antipsychotics included in the meta-analysis to show a significant reduction in total symptom score compared to placebo, and the effect size was highest for aripiprazole. Panellists expected benefits of augmentation therapy particularly in case of residual negative symptoms. This notion is supported by the findings of a double-blind, randomised and placebo-controlled clinical trial of aripiprazole augmentation in clozapine-resistant schizophrenia [138], which concluded that aripiprazole augmentation did not improve total symptom severity, but may provide a benefit in the negative symptom domain. Panellists thought that, in case of residual depressive symptoms, addition of an antidepressant may be more appropriate.
It was considered that there was insufficient information available to position aripiprazole with respect to ECT in this context. Panellists were sceptical that augmentation with aripiprazole would lead to a reduction in the adverse events of clozapine unless it was possible in parallel to decrease the dose of clozapine. Several participants emphasised the importance of monitoring plasma concentrations of clozapine prior to starting augmentation therapy to ensure that plasma levels are adequate, and to adjust the dose if necessary. This is particularly important in heavy smokers, since smoking strongly induces CYP1A2, the enzyme that metabolises clozapine [139]. Concerning the interest of a depot formulation of aripiprazole, panellists thought that this would principally be appropriate in patients whose observance was poor (Table 9).
Methodological issues
The aim of the recruitment process was to ensure participation of > 30 participants in both rounds of the survey. This number has been proposed by the developers of the Delphi method as being optimal for minimising the risk of an erroneous outcome and for generating a reliable consensus [18]. However, in practice, the number of participants in Delphi surveys is frequently lower: a systematic review of eighty Delphi studies in the field of healthcare published in 2011 reported that the median number of participants was seventeen [140]. We anticipated that certain potential participants may not be eligible or not prepared to complete the survey. In addition, it was expected that not all participants in the first round would be prepared to participate in the second round. In another recent Delphi survey in France which also recruited patients from professional listings, only two-thirds of first-round participants took part in the second round [141]. From these considerations, we targeted 60–70 physicians starting the survey. Once this number was reached, the survey was closed. In fact, 84 psychiatrists opened the survey, of whom seventeen did not fulfil the eligibility criteria (for example, they did not prescribe antipsychotic medication) and five declined to participate. Of the 62 psychiatrists who started the questionnaire, all but ten completed it. The relatively small number of psychiatrists who declined to participate or failed to complete the questionnaire suggests that participants who entered the survey found the content interesting and relevant. As anticipated, a proportion of participants in the first round did not take part in the second round, and this proportion was similar to that reported in the recent gastroenterology Delphi survey in France [141]. The final number of psychiatrists who completed the survey was 33, which was compliant with the initial target of at least thirty participants.
Of the 406 psychiatrists who were contacted and who opened the mail, 84 entered the survey. This response rate (20.7%) rate is thus rather low. The main reason for this is probably that participants were not co-opted by personal contact by the scientific committee, but were recruited by ‘cold call’. The co-option approach ensures that potential participants contacted are known from the outset to be interested in the subject matter and are likely a priori to be interested in participating. In contrast, using the ‘cold-call’ approach, it is not possible to target those physicians most likely to participate. It was decided to use the ‘cold-call’ rather than the co-option approach in order to capture a wide as possible cross-section of antipsychotic prescribers in France. The psychiatrists received an unsolicited e-mail from a sender address with which they were not familiar. The sender had no information on the psychiatrist other than the hospital or clinic in which they worked, and it is likely that some of the psychiatrists to whom the invitation was sent were not involved in the treatment of patients with schizophrenia. In previous surveys in the field of mental health, participation rates are generally > 80% for those in which targeted participants are co-opted [23, 142, 143] and < 20% for those using ‘cold call’ recruitment [144,145,146], although in many publications the response rate was not reported. In the light of this previous experience, the response rate observed in the present study and the low number of psychiatrists who explicitly refused to participate can be considered acceptable. No financial incentive was offered to participate and the survey was internet-based. Both of these features have been shown to be to associated with lower response rates in physician surveys [147,148,149]. It should also be noted that, to some extent, the response rate is a consequence of the recruitment target. The survey was closed once the target of 60–70 participants had been reached. It is possible that if the survey had been kept open longer or if the mailing of reminders had been more intensive, then more of the contacted psychiatrists may have responded. Finally, the survey was implemented during the pre-vaccination COVID-19 epidemic, when hospital resources and staff were under significant pressure, and this may also have discouraged certain psychiatrists from participating.
The current study has a number of more general limitations. Firstly, the literature review was carried out on one source (Medline) and may thus be not exhaustive. Secondly, members of the scientific committee and the Delphi participants were principally hospital-based. Therefore, there might be limitations on the representativeness of the clinical experience captured which may potentially lead to difficulty in generalising the results to a wider population or a different healthcare system.
Conclusion
This Delphi survey has shed light on current clinical practice with aripiprazole in clinical domains where the evidence base from published clinical trials is narrow. The ideas that emerge may be helpful for physicians in choosing the most promising ways to use this antipsychotic. They also highlight areas where more research is needed, either from formal clinical trials or pragmatic observational studies in everyday clinical practice, in order to widen the evidence base. Future research should also investigate patient perceptions of aripiprazole in these clinical domains.
Availability of data and materials
Anonymised data on the results of the survey are held by the study moderator on behalf of the authors. Reasonable requests for access to this data can be addressed to the author for correspondence.
Change history
19 June 2022
The tagging of the author’s name was incorrect in the original publication. The article has been updated to rectify the error.
References
Hasan A, Falkai P, Wobrock T, Lieberman J, Glenthoj B, Gattaz WF, et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, part 1: update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J Biol Psychiatry. 2012;13(5):318–78.
Keck PE Jr, Mcelroy SL. Aripiprazole: a partial dopamine D2 receptor agonist antipsychotic. Expert Opin Investig Drugs. 2003;12(4):655–62.
Simon N, Azorin JM. Aripiprazole as dopamine partial agonist model: Basic concepts and clinical impact. Encephale. 2018;44(6):558–64.
Wood M, Reavill C. Aripiprazole acts as a selective dopamine D2 receptor partial agonist. Expert Opin Investig Drugs. 2007;16(6):771–5.
Mailman RB, Murthy V. Third generation antipsychotic drugs: partial agonism or receptor functional selectivity? Curr Pharm Des. 2010;16(5):488–501.
Kling RC, Tschammer N, Lanig H, Clark T, Gmeiner P. Active-state model of a dopamine D2 receptor-Galphai complex stabilized by aripiprazole-type partial agonists. PLoS ONE. 2014;9(6):e100069.
Urs NM, Peterson SM, Caron MG. New Concepts in Dopamine D2 Receptor Biased Signaling and Implications for Schizophrenia Therapy. Biol Psychiatry. 2017;81(1):78–85.
Kenakin T, Christopoulos A. Signalling bias in new drug discovery: detection, quantification and therapeutic impact. Nat Rev Drug Discov. 2013;12(3):205–16.
Kenakin T, Christopoulos A. Measurements of ligand bias and functional affinity. Nat Rev Drug Discov. 2013;12(6):483.
Khanna P, Suo T, Komossa K, Ma H, Rummel-Kluge C, El-Sayeh HG, et al. Aripiprazole versus other atypical antipsychotics for schizophrenia. Cochrane Database Syst Rev. 2014;1:CD006569.
Kim DD, Barr AM, Lian L, Yuen JWY, Fredrikson D, Honer WG, et al. Efficacy and tolerability of aripiprazole versus D2 antagonists in the early course of schizophrenia: a systematic review and meta-analysis. NPJ Schizophr. 2021;7(1):29.
Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382(9896):951–62.
Stip E, Tourjman V. Aripiprazole in schizophrenia and schizoaffective disorder: A review. Clin Ther. 2010;32(Suppl 1):S3-20.
Di Sciascio G, Riva MA. Aripiprazole: from pharmacological profile to clinical use. Neuropsychiatr Dis Treat. 2015;11:2635–47.
Hernandez-Huerta D, Morillo-Gonzalez J. Dopamine D3 partial agonists in the treatment of psychosis and substance use disorder comorbidity: a pharmacological alternative to consider? CNS Spectr. 2021;26(5):444–5.
Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312(7023):71–2.
Metaplan G. Metaplan® Basic Techniques. Moderating group discussions using the Metaplan approach. 2021.
Dalkey N. The Delphi Method: an experimental study in group opinion. Santa Monica, USA: RAND Corporation; 1969.
Turoff M. The design of a policy Delphi. Technol Forecasting Soc Change. 1970;2(2):149–71.
Hasson F, Keeney S, Mckenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32(4):1008–15.
Iqbal SP-Y, L. The Delphi method. Psychologist. 2009;22:598–601.
Galderisi S, De Hert M, Del Prato S, Fagiolini A, Gorwood P, Leucht S, et al. Identification and management of cardiometabolic risk in subjects with schizophrenia spectrum disorders: A Delphi expert consensus study. Eur Psychiatry. 2021;64(1):e7.
Garriga M, Pacchiarotti I, Kasper S, Zeller SL, Allen MH, Vazquez G, et al. Assessment and management of agitation in psychiatry: Expert consensus. World J Biol Psychiatry. 2016;17(2):86–128.
Jorm AF. Using the Delphi expert consensus method in mental health research. Aust N Z J Psychiatry. 2015;49(10):887–97.
San L, Serrano M, Canas F, Romero SL, Sanchez-Cabezudo A, Villar M. Towards a pragmatic and operational definition of relapse in schizophrenia: A Delphi consensus approach. Int J Psychiatry Clin Pract. 2015;19(2):90–8.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Santé Haute Autorite De. Niveau de preuve et gradation des recommandations de bonne pratique. St Denis: HAS; 2013. p. 1–92.
Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67(4):401–9.
Buchanan RW. Persistent negative symptoms in schizophrenia: an overview. Schizophr Bull. 2007;33(4):1013–22.
Kirkpatrick B. Progress in the study of negative symptoms. Schizophrenia bulletin. 2014;40 Suppl(Suppl 2):S101-6.
Kirkpatrick B, Fenton WS, Carpenter WT Jr, Marder SR. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull. 2006;32(2):214–9.
Strauss JS, Carpenter WT Jr, Bartko JJ. The diagnosis and understanding of schizophrenia. Part III. Speculations on the processes that underlie schizophrenic symptoms and signs. Schizophrenia bulletin. 1974;11:61–9.
Aleman A, Lincoln TM, Bruggeman R, Melle I, Arends J, Arango C, et al. Treatment of negative symptoms: Where do we stand, and where do we go? Schizophr Res. 2017;186:55–62.
Bobes J, Arango C, Garcia-Garcia M, Rejas J. Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: findings from the CLAMORS study. J Clin Psychiatry. 2010;71(3):280–6.
Galderisi S, Rossi A, Rocca P, Bertolino A, Mucci A, Bucci P, et al. The influence of illness-related variables, personal resources and context-related factors on real-life functioning of people with schizophrenia. World Psychiatry. 2014;13(3):275–87.
Harvey PD, Strassnig M. Predicting the severity of everyday functional disability in people with schizophrenia: cognitive deficits, functional capacity, symptoms, and health status. World Psychiatry. 2012;11(2):73–9.
Tek C, Kirkpatrick B, Buchanan RW. A five-year followup study of deficit and nondeficit schizophrenia. Schizophr Res. 2001;49(3):253–60.
Crow TJ. Molecular pathology of schizophrenia: more than one disease process? BMJ. 1980;280(6207):66–8.
Mackay AV. Positive and negative schizophrenic symptoms and the role of dopamine. Br J Psychiatry. 1980;137:379–83.
Arango C, Garibaldi G, Marder SR. Pharmacological approaches to treating negative symptoms: a review of clinical trials. Schizophr Res. 2013;150(2–3):346–52.
Fusar-Poli P, Papanastasiou E, Stahl D, Rocchetti M, Carpenter W, Shergill S, et al. Treatments of Negative Symptoms in Schizophrenia: Meta-Analysis of 168 Randomized Placebo-Controlled Trials. Schizophr Bull. 2015;41(4):892–9.
Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet. 2009;373(9657):31–41.
Möller HJ, Czobor P. Pharmacological treatment of negative symptoms in schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2015;265(7):567–78.
Mitsonis CI, Dimopoulos NP, Mitropoulos PA, Kararizou EG, Katsa AN, Tsakiris FE, et al. Aripiprazole augmentation in the management of residual symptoms in clozapine-treated outpatients with chronic schizophrenia: An open-label pilot study. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(2):373–7.
Franza F, Fasano V, De Guglielmo S, Solomita B. Management of primary negative symptoms in schizophrenia: an one-year observational study. Psychiatr Danub. 2015;27(Suppl 1):S245–9.
Glick ID, Duggal V, Hodulik C. Aripiprazole as a dopamine partial agonist: positive and negative effects. J Clin Psychopharmacol. 2006;26(1):101–3.
Levoyer D, Drapier D, Fadier-Salicé G, Millet B. Clinical impact of aripiprazole in patients suffering from schizophrenia. Encephale. 2007;33(3 Pt 1):332–8.
Tsai CH, Chen TT, Huang WL. Combination of escitalopram and aripiprazole causes significant improvement of negative symptoms of simple schizophrenia. Psychiatry Clin Neurosci. 2014;68(7):582–3.
Galbally M, Frayne J, Watson SJ, Snellen M. Psychopharmacological prescribing practices in pregnancy for women with severe mental illness: A multicentre study. Eur Neuropsychopharmacol. 2019;29(1):57–65.
Galbally M, Snellen M, Power J. Antipsychotic drugs in pregnancy: a review of their maternal and fetal effects. Therapeutic Adv Drug Safety. 2014;5(2):100–9.
Miller LJ, Finnerty M. Family planning knowledge, attitudes and practices in women with schizophrenic spectrum disorders. J Psychosom Obstet Gynaecol. 1998;19(4):210–7.
González-Rodríguez A, Guàrdia A, ÁlvarezPedrero A, Betriu M, Cobo J, Acebillo S, et al. Women with Schizophrenia over the Life Span: Health Promotion, Treatment and Outcomes. Int J Environ Res Public Health. 2020;17(15):5594.
Posada Correa AM, Andrade Carrillo RA, Suarez Vega DC, Gómez Cano S, Agudelo Arango LG, Tabares Builes LF, et al. Sexual and Reproductive Health in Patients with Schizophrenia and Bipolar Disorder. Revista Colombiana de psiquiatria (English ed). 2020;49(1):15–22.
Sethuraman B, Rachana A, Kurian S. Knowledge, Attitude, and Practice Regarding Contraception among Women with Schizophrenia: An Observational Study from South India. Indian J Psychol Med. 2019;41(4):323–30.
Ifteni P, Moga MA, Burtea V, Correll CU. Schizophrenia relapse after stopping olanzapine treatment during pregnancy: a case report. Ther Clin Risk Manag. 2014;10:901–4.
Matevosyan NR. Pregnancy and postpartum specifics in women with schizophrenia: a meta-study. Arch Gynecol Obstet. 2011;283(2):141–7.
Snellen M, Mack K, Trauer T. Schizophrenia, mental state, and mother-infant interaction: examining the relationship. Aust N Z J Psychiatry. 1999;33(6):902–11.
Wan MW, Penketh V, Salmon MP, Abel KM. Content and style of speech from mothers with schizophrenia towards their infants. Psychiatry Res. 2008;159(1–2):109–14.
Wan MW, Warren K, Salmon MP, Abel KM. Patterns of maternal responding in postpartum mothers with schizophrenia. Infant Behav Dev. 2008;31(3):532–8.
Bodén R, Lundgren M, Brandt L, Reutfors J, Kieler H. Antipsychotics during pregnancy: relation to fetal and maternal metabolic effects. Arch Gen Psychiatry. 2012;69(7):715–21.
Galbally M, Frayne J, Watson SJ, Morgan V, Snellen M. The association between gestational diabetes mellitus, antipsychotics and severe mental illness in pregnancy: A multicentre study. Aust N Z J Obstet Gynaecol. 2020;60(1):63–9.
Gentile S. Pregnancy exposure to second-generation antipsychotics and the risk of gestational diabetes. Expert Opin Drug Saf. 2014;13(12):1583–90.
Park Y, Hernandez-Diaz S, Bateman BT, Cohen JM, Desai RJ, Patorno E, et al. Continuation of Atypical Antipsychotic Medication During Early Pregnancy and the Risk of Gestational Diabetes. Am J Psychiatry. 2018;175(6):564–74.
Gentile S. Antipsychotic therapy during early and late pregnancy. Systematic Rev Schizophrenia Bulletin. 2010;36(3):518–44.
Einarson A, Boskovic R. Use and safety of antipsychotic drugs during pregnancy. J Psychiatr Pract. 2009;15(3):183–92.
Terrana N, Koren G, Pivovarov J, Etwel F, Nulman I. Pregnancy Outcomes Following In Utero Exposure to Second-Generation Antipsychotics: A Systematic Review and Meta-Analysis. J Clin Psychopharmacol. 2015;35(5):559–65.
Cohen LS, Viguera AC, Mcinerney KA, Freeman MP, Sosinsky AZ, Moustafa D, et al. Reproductive Safety of Second-Generation Antipsychotics: Current Data From the Massachusetts General Hospital National Pregnancy Registry for Atypical Antipsychotics. Am J Psychiatry. 2016;173(3):263–70.
Damkier P, Videbech P. The Safety of Second-Generation Antipsychotics During Pregnancy: A Clinically Focused Review. CNS Drugs. 2018;32(4):351–66.
Viguera AC, Freeman MP, Góez-Mogollón L, Sosinsky AZ, Mcelheny SA, Church TR, et al. Reproductive Safety of Second-Generation Antipsychotics: Updated Data From the Massachusetts General Hospital National Pregnancy Registry for Atypical Antipsychotics. J Clin Psychiatry. 2021;82(4):20m13745.
Ellfolk M, Leinonen MK, Gissler M, Kiuru-Kuhlefelt S, Saastamoinen L, Malm H. Second-generation antipsychotic use during pregnancy and risk of congenital malformations. Eur J Clin Pharmacol. 2021;77(11):1737–45.
Huybrechts KF, Hernandez-Diaz S, Patorno E, Desai RJ, Mogun H, Dejene SZ, et al. Antipsychotic Use in Pregnancy and the Risk for Congenital Malformations. JAMA Psychiat. 2016;73(9):938–46.
Gentile S, Fusco ML. Neurodevelopmental outcomes in infants exposed in utero to antipsychotics: a systematic review of published data. CNS Spectr. 2017;22(3):273–81.
Momen NC, Robakis T, Liu X, Reichenberg A, Bergink V, Munk-Olsen T. In utero exposure to antipsychotic medication and psychiatric outcomes in the offspring. Neuropsychopharmacology. 2022;47(3):759–66.
Freeman MP, Viguera AC, Góez-Mogollón L, Young AV, Caplin PS, Mcelheny SA, et al. Reproductive safety of aripiprazole: data from the Massachusetts General Hospital National Pregnancy Registry for Atypical Antipsychotics. Arch Womens Ment Health. 2021;24(4):659–67.
Bellet F, Beyens MN, Bernard N, Beghin D, Elefant E, Vial T. Exposure to aripiprazole during embryogenesis: a prospective multicenter cohort study. Pharmacoepidemiol Drug Saf. 2015;24(4):368–80.
Habermann F, Fritzsche J, Fuhlbruck F, Wacker E, Allignol A, Weber-Schoendorfer C, et al. Atypical antipsychotic drugs and pregnancy outcome: a prospective, cohort study. J Clin Psychopharmacol. 2013;33(4):453–62.
Ballester-Gracia I, Perez-Almarcha M, Galvez-Llompart A, Hernandez-Viadel M. Use of long acting injectable aripiprazole before and through pregnancy in bipolar disorder: a case report. BMC Pharmacol Toxicol. 2019;20(1):52.
Gentile S, Tofani S, Bellantuono C. Aripiprazole and pregnancy: a case report and literature review. J Clin Psychopharmacol. 2011;31(4):531–2.
Lutz UC, Hiemke C, Wiatr G, Farger G, Arand J, Wildgruber D. Aripiprazole in pregnancy and lactation: a case report. J Clin Psychopharmacol. 2010;30(2):204–5.
Mendhekar DN, Sharma JB, Srilakshmi P. Use of aripiprazole during late pregnancy in a woman with psychotic illness. Ann Pharmacother. 2006;40(3):575.
Mendhekar DN, Sunder KR, Andrade C. Aripiprazole use in a pregnant schizoaffective woman. Bipolar Disord. 2006;8(3):299–300.
Mervak B, Collins J, Valenstein M. Case report of aripiprazole usage during pregnancy. Arch Womens Ment Health. 2008;11(3):249–50.
Watanabe N, Kasahara M, Sugibayashi R, Nakamura T, Nakajima K, Watanabe O, et al. Perinatal use of aripiprazole: a case report. J Clin Psychopharmacol. 2011;31(3):377–9.
Widschwendter CG, Hofer A. Aripiprazole use in early pregnancy: a case report. Pharmacopsychiatry. 2012;45(7):299–300.
Windhager E, Kim SW, Saria A, Zauner K, Amminger PG, Klier CM. Perinatal use of aripiprazole: plasma levels, placental transfer, and child outcome in 3 new cases. J Clin Psychopharmacol. 2014;34(5):637–41.
Galbally M, Frayne J, Watson SJ, Snellen M. Aripiprazole and pregnancy: A retrospective, multicentre study. J Affect Disord. 2018;238:593–6.
Sakai T, Ohtsu F, Mori C, Tanabe K, Goto N. Signal of Miscarriage with Aripiprazole: A Disproportionality Analysis of the Japanese Adverse Drug Event Report Database. Drug Saf. 2017;40(11):1141–6.
Nguyen T, Teoh S, Hackett LP, Ilett K. Placental transfer of aripiprazole. Aust N Z J Psychiatry. 2011;45(6):500–1.
Schlotterbeck P, Leube D, Kircher T, Hiemke C, Grunder G. Aripiprazole in human milk. Int J Neuropsychopharmacol. 2007;10(3):433.
Elvevåg BG, Goldberg TE. Cognitive impairment in schizophrenia is the core of the disorder. Crit Rev Neurobiol. 2000;14(1):1–21.
Owen MJ, Sawa A, Mortensen PB. Schizophrenia. The Lancet. 2016;388(10039):86–97.
Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. Am J Psychiatry. 2006;163(3):418–25.
Milev P, Ho BC, Arndt S, Andreasen NC. Predictive values of neurocognition and negative symptoms on functional outcome in schizophrenia: a longitudinal first-episode study with 7-year follow-up. Am J Psychiatry. 2005;162(3):495–506.
Harvey PD, Mcclure MM. Pharmacological approaches to the management of cognitive dysfunction in schizophrenia. Drugs. 2006;66(11):1465–73.
Sweeney JA, Keilp JG, Haas GL, Hill J, Weiden PJ. Relationships between medication treatments and neuropsychological test performance in schizophrenia. Psychiatry Res. 1991;37(3):297–308.
Meltzer HY, Mcgurk SR. The effects of clozapine, risperidone, and olanzapine on cognitive function in schizophrenia. Schizophr Bull. 1999;25(2):233–55.
Keefe RS, Bilder RM, Davis SM, Harvey PD, Palmer BW, Gold JM, et al. Neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE Trial. Arch Gen Psychiatry. 2007;64(6):633–47.
Nielsen RE, Levander S, Kjaersdam Telleus G, Jensen SO, Ostergaard Christensen T, Leucht S. Second-generation antipsychotic effect on cognition in patients with schizophrenia–a meta-analysis of randomized clinical trials. Acta Psychiatr Scand. 2015;131(3):185–96.
Desamericq G, Schurhoff F, Meary A, Szoke A, Macquin-Mavier I, Bachoud-Levi AC, et al. Long-term neurocognitive effects of antipsychotics in schizophrenia: a network meta-analysis. Eur J Clin Pharmacol. 2014;70(2):127–34.
Murphy A, Dursun S, Mckie S, Elliott R, Deakin JF. An investigation into aripiprazole’s partial D(2) agonist effects within the dorsolateral prefrontal cortex during working memory in healthy volunteers. Psychopharmacol. 2016;233(8):1415–26.
Kern RS, Green MF, Cornblatt BA, Owen JR, Mcquade RD, Carson WH, et al. The neurocognitive effects of aripiprazole: an open-label comparison with olanzapine. Psychopharmacol. 2006;187(3):312–20.
Maat A, Cahn W, Gijsman HJ, Hovens JE, Kahn RS, Aleman A. Open, randomized trial of the effects of aripiprazole versus risperidone on social cognition in schizophrenia. Eur Neuropsychopharmacol. 2014;24(4):575–84.
Suzuki H, Gen K, Inoue Y. An unblinded comparison of the clinical and cognitive effects of switching from first-generation antipsychotics to aripiprazole, perospirone or olanzapine in patients with chronic schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(1):161–8.
Yasui-Furukori N, Kaneda A, Sugawara N, Tomita T, Kaneko S. Effect of adjunctive treatment with aripiprazole to atypical antipsychotics on cognitive function in schizophrenia patients. J Psychopharmacol (Oxford, England). 2012;26(6):806–12.
Kim SW, Shin IS, Kim JM, Bae KY, Yang SJ, Yoon JS. Effectiveness of switching from aripiprazole to ziprasidone in patients with schizophrenia. Clin Neuropharmacol. 2010;33(3):121–5.
Pfaffenberger N, Hoertnagl C, Fleischhacker WW, Hofer A. Aripiprazole add-on treatment in a patient with schizoaffective disorder: neurocognitive outcomes. Pharmacopsychiatry. 2010;43(6):234–5.
Riedel M, Spellmann I, Schennach-Wolff R, Musil R, Dehning S, Cerovecki A, et al. Effect of aripiprazole on cognition in the treatment of patients with schizophrenia. Pharmacopsychiatry. 2010;43(2):50–7.
Suzuki H, Sekiguchi G. Influence of aripiprazole once monthly on clinical symptoms and cognitive function in two schizophrenia patients: Preliminary results. Psychiatry Clin Neurosci. 2016;70(1):71–2.
Yeh CB, Huang YS, Tang CS, Wang LJ, Chou WJ, Chou MC, et al. Neurocognitive effects of aripiprazole in adolescents and young adults with schizophrenia. Nord J Psychiatry. 2014;68(3):219–24.
Wykes T, Huddy V, Cellard C, Mcgurk SR, Czobor P. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry. 2011;168(5):472–85.
Masuda T, Misawa F, Takase M, Kane JM, Correll CU. Association With Hospitalization and All-Cause Discontinuation Among Patients With Schizophrenia on Clozapine vs Other Oral Second-Generation Antipsychotics: A Systematic Review and Meta-analysis of Cohort Studies. JAMA Psychiat. 2019;76(10):1052–62.
Hartz SM, Pato CN, Medeiros H, Cavazos-Rehg P, Sobell JL, Knowles JA, et al. Comorbidity of severe psychotic disorders with measures of substance use. JAMA Psychiat. 2014;71(3):248–54.
Swartz MS, Wagner HR, Swanson JW, Stroup TS, Mcevoy JP, Reimherr F, et al. The effectiveness of antipsychotic medications in patients who use or avoid illicit substances: results from the CATIE study. Schizophr Res. 2008;100(1–3):39–52.
Swofford CD, Scheller-Gilkey G, Miller AH, Woolwine B, Mance R. Double jeopardy: schizophrenia and substance use. Am J Drug Alcohol Abuse. 2000;26(3):343–53.
Swartz MS, Wagner HR, Swanson JW, Stroup TS, Mcevoy JP, Canive JM, et al. Substance use in persons with schizophrenia: baseline prevalence and correlates from the NIMH CATIE study. J Nerv Ment Dis. 2006;194(3):164–72.
Potvin S, Pampoulova T, Mancini-Marië A, Lipp O, Bouchard RH, Stip E. Increased extrapyramidal symptoms in patients with schizophrenia and a comorbid substance use disorder. J Neurol Neurosurg Psychiatry. 2006;77(6):796–8.
Potvin S, Stip E, Lipp O, Roy MA, Demers MF, Bouchard RH, et al. Anhedonia and social adaptation predict substance abuse evolution in dual diagnosis schizophrenia. Am J Drug Alcohol Abuse. 2008;34(1):75–82.
Lähteenvuo M, Batalla A, Luykx JJ, Mittendorfer-Rutz E, Tanskanen A, Tiihonen J, et al. Morbidity and mortality in schizophrenia with comorbid substance use disorders. Acta Psychiatr Scand. 2021;144(1):42–9.
Meszaros ZS, Dimmock JA, Ploutz-Snyder RJ, Abdul-Malak Y, Leontieva L, Canfield K, et al. Predictors of smoking severity in patients with schizophrenia and alcohol use disorders. Am J Addict. 2011;20(5):462–7.
George TP, Ziedonis DM, Feingold A, Pepper WT, Satterburg CA, Winkel J, et al. Nicotine transdermal patch and atypical antipsychotic medications for smoking cessation in schizophrenia. Am J Psychiatry. 2000;157(11):1835–42.
Azorin J-M, Simon N, Adida M, Belzeaux R. Pharmacological treatment of schizophrenia with comorbid substance use disorder. Expert Opin Pharmacother. 2016;17(2):231–53.
Green Al, Noordsy DL, Brunette MF, O’keefe C. Substance abuse and schizophrenia: pharmacotherapeutic intervention. J Substance Abuse Treatment. 2008;34(1):61–71.
Kim SH, Han DH, Joo SY, Min KJ. The effect of dopamine partial agonists on the nicotine dependency in patients with schizophrenia. Hum Psychopharmacol. 2010;25(2):187–90.
Beresford TP, Clapp L, Martin B, Wiberg JL, Alfers J, Beresford HF. Aripiprazole in schizophrenia with cocaine dependence: a pilot study. J Clin Psychopharmacol. 2005;25(4):363–6.
Cuomo I, Kotzalidis GD, De Persis S, Piacentino D, Perrini F, Amici E, et al. Head-to-head comparison of 1-year aripiprazole long-acting injectable (LAI) versus paliperidone LAI in comorbid psychosis and substance use disorder: impact on clinical status, substance craving, and quality of life. Neuropsychiatr Dis Treat. 2018;14:1645–56.
Chen SF, Shen YC. Long-Acting Injectable Aripiprazole for a Schizophrenic Patient Concomitant With Stimulant Use Disorder. J Clin Psychopharmacol. 2019;39(5):508–9.
Wu BJ, Chen HK, Lee SM. Do atypical antipsychotics really enhance smoking reduction more than typical ones?: the effects of antipsychotics on smoking reduction in patients with schizophrenia. J Clin Psychopharmacol. 2013;33(3):319–28.
Szerman N, Basurte-Villamor I, Vega P, Martinez-Raga J, Parro-Torres C, Cambra Almerge J, et al. Once-Monthly Long-Acting Injectable Aripiprazole for the Treatment of Patients with Schizophrenia and Co-occurring Substance Use Disorders: A Multicentre, Observational Study. Drugs - real world outcomes. 2020;7(1):75–83.
Siskind D, Siskind V, Kisely S. Clozapine Response Rates among People with Treatment-Resistant Schizophrenia: Data from a Systematic Review and Meta-Analysis. Canadian J Psychiatry Revue Canadienne De Psychiatrie. 2017;62(11):772–7.
Henna Neto J, Elkis H. Clinical aspects of super-refractory schizophrenia: a 6-month cohort observational study. Revista brasileira de psiquiatria. 2007;29(3):228–32.
Chakrabarti S. Clozapine resistant schizophrenia: Newer avenues of management. World J Psychiatry. 2021;11(8):429–48.
Mouaffak F, Tranulis C, Gourevitch R, Poirier MF, Douki S, Olié JP, et al. Augmentation strategies of clozapine with antipsychotics in the treatment of ultraresistant schizophrenia. Clin Neuropharmacol. 2006;29(1):28–33.
Porcelli S, Balzarro B, Serretti A. Clozapine resistance: augmentation strategies. Eur Neuropsychopharmacol. 2012;22(3):165–82.
Siskind DJ, Lee M, Ravindran A, Zhang Q, Ma E, Motamarri B, et al. Augmentation strategies for clozapine refractory schizophrenia: A systematic review and meta-analysis. Aust N Z J Psychiatry. 2018;52(8):751–67.
Barber S, Olotu U, Corsi M, Cipriani A. Clozapine combined with different antipsychotic drugs for treatment-resistant schizophrenia. Cochrane Database Syst Rev. 2017;3(3):Cd006324.
Genç Y, Taner E, Candansayar S. Comparison of clozapine-amisulpride and clozapine-quetiapine combinations for patients with schizophrenia who are partially responsive to clozapine: a single-blind randomized study. Adv Ther. 2007;24(1):1–13.
Cipriani A, Accordini S, Nosè M, Purgato M, Girlanda F, Tansella M, et al. Aripiprazole versus haloperidol in combination with clozapine for treatment-resistant schizophrenia: a 12-month, randomized, naturalistic trial. J Clin Psychopharmacol. 2013;33(4):533–7.
Chang JS, Ahn YM, Park HJ, Lee KY, Kim SH, Kang UG, et al. Aripiprazole augmentation in clozapine-treated patients with refractory schizophrenia: an 8-week, randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2008;69(5):720–31.
Wagner E, Mcmahon L, Falkai P, Hasan A, Siskind D. Impact of smoking behavior on clozapine blood levels - a systematic review and meta-analysis. Acta Psychiatr Scand. 2020;142(6):456–66.
Boulkedid R, Abdoul H, Loustau M, Sibony O, Alberti C. Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS ONE. 2011;6(6):e20476.
Hébuterne X, Peyrin-Biroulet L, Hausfater P. The management of emergency hospital visits for inflammatory bowel diseases: A French national expert consensus report. Dig Liver Dis. 2020;52(4):420–6.
Castro-Calvo J, King DL, Stein DJ, Brand M, Carmi L, Chamberlain SR, et al. Expert appraisal of criteria for assessing gaming disorder: an international Delphi study. Addiction (Abingdon, England). 2021;116(9):2463–75.
Rybak YE, Lai KSP, Ramasubbu R, Vila-Rodriguez F, Blumberger DM, Chan P, et al. Treatment-resistant major depressive disorder: Canadian expert consensus on definition and assessment. Depress Anxiety. 2021;38(4):456–67.
Newcomer JW, Nasrallah HA, Loebel AD. The Atypical Antipsychotic Therapy and Metabolic Issues National Survey: practice patterns and knowledge of psychiatrists. J Clin Psychopharmacol. 2004;24(5 Suppl 1):S1-6.
Perlis RH. Use of treatment guidelines in clinical decision making in bipolar disorder: a pilot survey of clinicians. Curr Med Res Opin. 2007;23(3):467–75.
Wahid SS, Ottman K, Hudhud R, Gautam K, Fisher HL, Kieling C, et al. Identifying risk factors and detection strategies for adolescent depression in diverse global settings: A Delphi consensus study. J Affect Disord. 2021;279:66–74.
Leece P, Bhandari M, Sprague S, Swiontkowski MF, Schemitsch EH, Tornetta P, et al. Internet versus mailed questionnaires: a randomized comparison (2). J Med Internet Res. 2004;6(3):e30.
Pit SW, Vo T, Pyakurel S. The effectiveness of recruitment strategies on general practitioner’s survey response rates - a systematic review. BMC Med Res Methodol. 2014;14:76.
Vangeest JB, Johnson TP, Welch VL. Methodologies for improving response rates in surveys of physicians: a systematic review. Eval Health Prof. 2007;30(4):303–21.
Acknowledgements
The authors would like to thank warmly all the psychiatrists who participated in this study for their time and insight, as well as Isabelle Tonelli of Otsuka Pharmaceutical France for her valuable contributions to the discussions.
Funding
This study was funded by Lundbeck France and Otsuka Pharmaceutical France.
Author information
Authors and Affiliations
Contributions
All authors participated in the design of the study, the choice and wording of the items in the questionnaire, the interpretation of the findings and the preparation of the present manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Since no individual patient data was collected in the course of this study, and physician participation was voluntary, ethical committee approval was not necessary. The survey was conducted in the accordance with the code for data privacy of the French data protection agency (Commission Nationale de l'Informatique et des Libertés). The online survey interface provided information on the goals and procedures of the study and required participants to provide explicit consent to participate in the survey, on the basis of the information provided, before proceeding to the study questionnaire.
Consent for publication
Not applicable.
Competing interests
MR is an employee of Lundbeck France, who market treatments for schizophrenia, including an injectable depot formulation of aripiprazole. PML received financial support from Otsuka and Lundbeck for the organization of meetings of the scientific committee, for the implementation of the survey and for editorial support, personal fee from Janssen, Eisai, Neuraxpharm, and Ethypharm, support for meeting from Eisai, Lundbeck and Ethypharm, and fee for advisory boards from Janssen, Eisai and Lundbeck. PN received honoraria from Otsuka and Lundbeck. EF received consulting fees from Bristol Myers Squibb, Janssen-Cilag, Lilly, Lundbeck, Otsuka, Recordatti, Sanofi and honoraria as speaker from Abbvie, AstraZeneca, Bristol Myers Squibb, Janssen-Cilag, Lundbeck, Otsuka, MSD, and Sanofi. IA was occasionally expert on reports and for consulting activities for Otsuka, Janssen, BMS, Astrazeneca and Lundbeck and was invited as speaker and auditor for conferences by Otsuka, Janssen, BMS and Astrazeneca. DD received honoraria as speaker from Janssen Cilag and Eisai, and for advisory boards from Lundbeck, Ethyfarm, Janssen and Eisai. WEH received grants from le Conseil Régional du Centre-Val de Loire, la Fondation de France and le Ministère de la Santé, consulting fees from Air Liquide, Janssen, Lundbeck and Otsuka, honoraria from Eisai, Chugai and UCB, payments from Mapreg SAS, and supports for attending meetings and participating on advisory boards from Janssen and Lundbeck. RJ received support from Lundbeck and Otsuka for the manuscript, grants from FIOP national grant and Institut Universitaire de France, supports for attending meeting from Lundbeck and for participating on advisory boards from Otsuka and Lundbeck. SM received honoraria as consultant and lecturer from Lundbeck, Otsuka, Janssen, Eisai, GSK and Pfizer. MR is an employee of Lundbeck France, who market treatments for schizophrenia, including an injectable depot formulation of aripiprazole. NS received support from Lundbeck and Otsuka for the manuscript, consulting fees from Tempero Bio and Aelis Farma, support for attending meetings from Camarus, and for participation on advisory boards from Bioproject. MNV has no conflict of interest to declare. JMA received honoraria or research or educational conference grants from Lundbeck and Otsuka.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Place of the partial dopamine receptor agonist aripiprazole in themanagement of schizophrenia in adults: a Delphi consensus study. Additional Table 1. Evidence level classification of the Frenchhealth authorities. Additional Table 2. Studies identified in the literature review. Additional Table 3. Questions asked in the Delphisurvey. Additional Table 4. Examples of verbatim from theDelphi survey. Additional Figure 1. PRISMAflow diagram for the literature search.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Llorca, PM., Nuss, P., Fakra, É. et al. Place of the partial dopamine receptor agonist aripiprazole in the management of schizophrenia in adults: a Delphi consensus study. BMC Psychiatry 22, 364 (2022). https://doi.org/10.1186/s12888-022-04008-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-022-04008-9