Abstract
Background
Pulmonary stenosis (PS) is a congenital heart diseases (CHDs) with a spectrum of stenosis. Monochorionic (MC) twins are at increased risk of CHDs, especially acquired CHDs in twin-twin transfusion syndrome (TTTS). PS/Pulmonary atresia (PA) is a rare coincidence with TTTS. MC twin pregnancies have increased in last decades due to increasing in maternal age and extensive use of assisted reproductive technologies. Therefore, attention to this group is important for heart abnormalities, especially in twins with TTTS. Multiple cardiac abnormalities in MC twins with TTTS are to be expected due to cardiac hemodynamic changes and may be eliminated by Fetoscopic laser photocoagulation treatment. Prenatal diagnosis of PS is necessary given the importance of treatment after birth.
Case presentation
We here present a case of coexistence of TTTS with PS in a growth restricted recipient twin who successfully treated with balloon pulmonary valvuloplasty in neonatal period. Also, we detected infundibular PS after valvuloplasty that treated with medical therapy (propranolol).
Conclusions
It is important to detect acquired cardiac abnormalities in MC twins with TTTS, and follow them up after birth to determine the need of intervention in neonatal period.
Similar content being viewed by others
Background
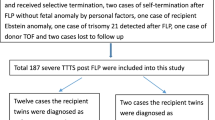
Twin-to-twin transfusion syndrome (TTTS) is a severe complication in monochorionic (MC) twin pregnancies. It is associated with fetal and neonatal cardiac dysfunction, especially in recipient twin. Acquired heart dysfunction is seen in recipient twins who complicated with ventricular hypertrophy, cardiomegaly and atrio-ventricular valves regurgitation [1]. In MC pregnancies with TTTS, the risk of at least one of the infants with CHD is threefold, as compared with uncomplicated MC twin pregnancies [2]. The development of acquired CHDs in MC twins is associated with TTTS, indicating an influence of hemodynamic alterations on cardiac development. MC twins with TTTS are associated with increased risk of ventricular septal defect (VSD), right ventricular outflow tract obstruction (RVOTO), atrial septal defect (ASD), coarctation of aorta (CoA), and aortic stenosis (AS) [3]. RVOTO may occur in the recipient twin of at least 9% of MC twin pregnancies that complicated with TTTS [4]. The likely etiology of RVOTO in recipient twins in TTTS is altered fetal circulation and right ventricular hypertrophy [5, 6]. Fetoscopic laser therapy has significant effect on heart function of donor and recipient twins of TTTS. Some of these cardiac disorders that are due to hemodynamic changes in TTTS improve after laser treatment, but some remain. Therefore, The diagnosis and follow up of PS/PA after laser treatment of TTTS is important because despite intervention, 35/7% of recipient twins die, 32.1% shows in utero regression and 32.1% has persistence of PS/PA [7]. Infundibular pulmonary stenosis (IPS) is a pathologic feature of the right tract from the right ventricular outflow tract to the peripheral pulmonary arteries at the infundibular level [8]. It can cause right ventricular hypertrophy and early treatment can lead to reduction of right ventricular pressure. Propranolol reduces the infundibular obstruction, but some cases need surgery [9].
Case presentation
A 27-year-old pregnant woman, primigravida, MC twin pregnancy, with a gestational age of 21 weeks was referred to our center due to TTTS stage 3. Her pregnancy was a product of in vitro fertilization (IVF). She had no history of medical disease or drug usage. Fetal echocardiography showed biventricular hypertrophy, cardiomegaly (Fig. 1) and severe pulmonary valve stenosis (PS) (Figs. 2 and 3) in recipient twin. No other major anomalies were detected in the both fetuses. Fetoscopic laser photocoagulation (FLP) was done at our center due to TTTS stage 3. After that, the course of the TTTS stopped, but PS persisted (Fig. 4) with presence of severe tricuspid valve regurgitation (Fig. 5) and at 32 weeks of gestation, the pregnancy was terminated by cesarean section due to fetal growth restriction (FGR) and absent Doppler wave in umbilical artery of recipient twin. Both babies were born with good APGAR score. After birth, in transthoracic echocardiography of recipient twin, Doppler spectral showed severe PS with peak pressure gradient more than 100 mmHg (Fig. 6). Contrast injection in lateral view of angiocardiography detected severe valvular and sub valvular pulmonary stenosis (Fig. 7). After birth, due to the persistence of stenosis, After initiation of prostaglandin infusion, the recipient twin underwent balloon pulmonary valvuloplasty at the age of one month, when the weight of baby was 1300 g with heart rate:155–160/min, respiratory rate:70/min, O2 saturation > 75–80, lactic acid(in ABG):12. The baby was under mechanical ventilation with SIMV PC mode and the preoperative trans thoracic echocardiography showed right ventricular hypertrophy (decreased end diastolic diameter), significant TR, small pulmonary annulus, small PDA (diameter = 2 mm with left to right shunt) and PFO with dominant right to left shunt. Balloon inflation of stenotic pulmonary valve in stenotic location showed a full dilation of stenosis (Fig. 8). Post procedure transthoracic echocardiography showed significant reduction in transpulmonary valve gradient (Fig. 9). Due to dynamic infundibular (subvalvular) stenosis and persistence of high transpulmonary valve gradient (about 100 mmHg), propranolol with maximum dose of 2 mg/kg was started and after 4 weeks, the gradient reduced from 100 to 30 mmHg. The baby had a good growth after treatment, with 3700 g weigh after three months.
Discussion and conclusions
PS/pulmonary atresia (PA) is a serious complications of MC twin pregnancies with TTTS, in recipient twin. The common abnormal cardiac presentation in recipient twins are ventricular hypertrophy and cardiomegaly, but PS/PA is rare. Recipient twins can develop progressive ventricular hypertrophy, diastolic dysfunction, and finally RVOTO and PS/PA [10, 11]. Postnatally, some need percutaneous balloon pulmonary valvuloplasty or surgical valvotomy. Critical PS causes cyanosis and can be lethal in infants. After initiation of prostaglandin infusion, percutaneous balloon valvuloplasty is the treatment of choice [12]. This procedure was done in our case successfully and IPS had a good response to propranolol. Murakoshi T. [13] reported 3 cases of pulmonary stenosis in the recipient twin in twin-twin transfusion syndrome. Two cases underwent postnatal balloon valvuloplasty to release the pulmonary valvular stenosis in neonatal period. The third one died soon after delivery and autopsy showed a slightly thickened pulmonary valve. Ortiz JU. [7] carried out a prospective study including 260 cases of TTTS, in which PS was observed in 16 out of 260 of recipient twins (6.2%). In above-mentioned study, Postnatally, seven recipients underwent percutaneous balloon pulmonary valvuloplasty just like the case we presented and one required surgical valvotomy.
It is important to detect acquired cardiac abnormalities in MC twins with TTTS, and follow up even if they are treated with fetoscopic laser photocoagulation during pregnancy and after birth to determine the need of intervention in neonatal period.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- PS:
-
Pulmonary stenosis
- CHDs:
-
Congenital heart diseases
- MC:
-
Monochorionic
- TTTS:
-
Twin-twin transfusion syndrome
- PA:
-
Pulmonary atresia
- FLP:
-
Fetoscopic laser photocoagulation
- VSD:
-
Ventricular septal defect
- RVOTO:
-
Right ventricular outflow tract obstruction
- ASD:
-
Atrial septal defect
- CoA:
-
Coarctation of aorta
- AS:
-
Aortic stenosis
- IVF:
-
In vitro fertilization
- FGR:
-
Fetal growth restriction
- IPS:
-
Infundibular pulmonary stenosis
References
Zosmer N, Bajoria R, Weiner E, Riby M, Vaughan J, Fisk NM. Clinical and echographic features of in utero cardiac dysfunction in the recipient twin in twin-twin transfusion syndrome. Br Heart J. 1994;72:74–9.
Pettit K, Merchant M, Machin G, Tacy T, Norton M. Congenital heart defects in a large, unselected cohort of monochorionic twins. J Perinatol. 2013;33:457–61.
Michelfelder E, Tan X, Cnota J, Divanovic A, Statile C, Lim FY, Crombleholme T. Prevalence, spectrum, and outcome of right ventricular outflow tract abnormalities in twin-twin transfusion syndrome: a large, single-center experience. Congenit Heart Dis. 2015;10:209–18.
Lougheed J, Sinclair BG, Fung K, Fung K, Bigras JL, Ryan G, Smallhorn MBBSJF, Hornberger LK. Acquired right ventricular outflow tract obstruction in the recipient twin in twin-twin transfusion syndrome. J Am Coll Cardiol. 2001;38(5):1533–8.
Fesslova V, Villa L, Nava S, Mosca F, Nicolini U. Fetal and neonatal echocardiographic findings in twin-twin transfusion syndrome. Am J Obstet Gynecol. 1998;179:1056–62.
Simpson LL, Marx GR, Elkadry EA, D’Alton ME. Cardiac dysfunction in twin-twin transfusion syndrome: a prospective longitudinal study. Obstet Gynecol. 1998;92:557–62.
Ortiz JU, Masoller N, Gomez O, Bennasar M, Eixarch E, Lobmaier SM, Crispi F, Gratacos E, Martinez JM. Rate andoutcomes of pulmonary stenosis and functional pulmonary atresia in recipient twins with twin-twin transfusion syndrome. Fetal Diagn Ther. 2017;41:191–6.
El ouahabi K, Erraboun N, Bouzerda A, Raissouni M, Asfalou I, Benyass A, Lakhal Z, Moutakillah Y, AitHoussa M, Zbir E. Isolated infundibular pulmonary stenosis. A case report. J Cardiovasc Med Cardiol. 2020;7(2):196–202.
Thapar MK, Rao PS. Use of propranolol for severe dynamic infundibular obstruction prior to balloon pulmonary vulvuloplasty (a brief communication). Cathet Cardiovas Diagn. 1990;19(4):240–1.
Karatza A, Wolfenden J, Taylor M, Wee L, Fisk N, Gardiner H. Influence of twin-twin transfusion syndrome on fetal cardiovascular structure and function: prospective case-control study of 136 monochorionic twin pregnancies. Heart. 2002;88:271–7.
Bahtiyar M, Dulay A, Weeks B, Friedman A, Copel J. Prevalence of congenital heart defects in monochorionic/diamniotic twin gestations: a systematic literature review. J Ultrasound Med. 2007;26:1491–8.
Binh HA, Chau NNM, Xuan NT, Tuan TV, Son NH. Balloon valvuloplasty for critical pulmonary valve stenosis in a newborn. J Pediatr Surg Case Rep. 2020;61:101591.
Murakoshi T, Yamamori K, Tojo Y, et al. Pulmonary stenosis in recipient twins in twin-to-twin transfusion syndrome: report on 3 cases and review of literature. Croat Med J. 2000;41(3):252–6.
Acknowledgements
None
Funding
Not received.
Author information
Authors and Affiliations
Contributions
AG, FJ, KH, MS and ASA conducted the initial database search. AG and FJ evaluated and screened the data. ASA, MN and AR conceptualized and supervised the study and wrote the manuscript. AG and FJ critically revised the manuscript for important intellectual content. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was in accordance with the ethical issues for human subject's research. The requirement for informed consent was obtained from the patient and parents gave their written consent for their child’s personal or clinical details along with any identifying images to be published in this study and approved by the Ethics Committee of (Tehran University of Medical Sciences). All methods were performed in accordance with the relevant guidelines and regulations of the relevant institution.
Consent for publication
The requirement for written consent to publish information was obtained from the study participant and approved by the Ethics Committee of (Tehran University of Medical Sciences).
Competing interests
No competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Golbabaei, A., Jafari, F., Hessami, K. et al. Pulmonary valve stenosis in a recipient twin in twin-to-twin transfusion syndrome with successful balloon valvuloplasty after birth: a case report. BMC Pediatr 23, 337 (2023). https://doi.org/10.1186/s12887-023-04159-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04159-y