Abstract
Background
Sub-Saharan African countries are a high-burden region of neonatal mortality and showed slow progress in its reduction. In developing countries, as long as the current trend of mortality persists, achieving a sustainable development target for neonatal mortality would be challenging. The aim of this study was to detect significant geographic areas and identify community and individual-level predictors of neonatal mortality in Ethiopia to draw attention to a policy.
Methods
A weighted total sample of 24,136 mothers from the 2019 mini-Ethiopian demographic and health survey data were included in the analysis. Global Moran’s I statistics was run to check the clustering of neonatal mortality and then kriging interpolation was done to predict the magnitude of neonatal mortality in Ethiopia. In addition, SaTScan analysis was also executed to identify hot spot clusters of neonatal mortality. Finally, a multilevel mixed-effect logistic regression model was used to identify community and individual-level predictors of early neonatal and neonatal mortality.
Results
The lifetime early neonatal and neonatal mortality among mothers in Ethiopia was 5.08 (95% CI: 4.13–6.03) and 6.54 (5.55, 7.52) per 1000 births respectively. Neonatal mortality was spatially clustered in the country and the SaTScan analysis identified significant hotspot areas of neonatal mortality in the Amhara and Afar regions and some areas of the Somali and Oromia regions. Its predicted magnitude was > 8 per 1000 births in wide areas of the Amhara and Benishangul regions. A multilevel mixed-effect logistics regression analysis identified that a lower level of maternal education, being a twin neonate, and being a male neonate were predictors of both early neonatal and neonatal mortality. Whereas, the younger age of mothers predicted neonatal mortality.
Conclusions
Neonatal mortality in Ethiopia is geographically clustered and sociodemographic and obstetric factors played a significant role. Policy direction should focus on evidence-based practices like midwives-led community and facility-based continuum of care from preconception to postnatal periods to possibly reduce neonatal mortality.
Similar content being viewed by others
Background
Neonatal mortality is a global public health concern [1] and the problem is strikingly high in developing countries. Low-and-middle income countries, particularly, sub-Saharan African countries are suffering from a high burden of neonatal mortality and showed slow progress in neonatal mortality reduction [2]. Neonatal mortality is also unequally distributed and almost 80% of newborn deaths in 2016 were from the two regions; southern Asia accounted for 39%, and similarly, sub-Saharan Africa 38% of all such deaths [3]. In Ethiopia, according to the 2016 demographic and health survey report, neonatal mortality was 29 per 1000 live births. It was only about a 24% decrease over 5 years [4]. Amhara is the leading region in the country that suffered from a huge burden of neonatal mortality. Most of the deaths during the neonatal period also unevenly occur in the first week of life [3].
Neonatal mortality, particularly early neonatal death is mainly attributed to complications of preterm birth, infection, low birth weight, and intrapartum-related events [3, 5,6,7]. Some large-scale studies [6, 8,9,10] also identified sociodemographic factors such as lack of education, obstetric factors like perinatal care none/low utilization, maternal morbidity, neonatal factors like sex, multiple gestations, gestational age at birth, and morbidity were significantly associated with neonatal mortality. At large, neonatal mortality is associated with the quality of maternal and fetal care predominantly around the time of childbirth and the death is preventable as well as treatable with well-known and cost-effective interventions [3].
Studies revealed that several interventions were found to decrease neonatal mortality. Maternal care before and during pregnancy namely, preconception care, antenatal care, prenatal nutrition counseling, and iron and multi-micro-nutrient supplementation are proven interventions. Likewise, helping babies breathe and basic resuscitation, cord care, kangaroo mother care, and exclusive breastfeeding are significant interventions to reduce neonatal mortality [11,12,13,14]. Similarly, community-level interventions [13, 15, 16] like participatory women’s groups and community health education intervention as well as improving access to high-quality antenatal and postnatal care found to decline neonatal mortality. Moreover, facility-level interventions [15, 17, 18] such as the availability of comprehensive emergency obstetrics, quality-improving interventions, and availability of maternity waiting homes are among significant factors to reduce neonatal mortality.
However, based on the current trends, 30 million deaths of newborn infants would occur between 2017 and 2030. About 80% would occur in south Asia and sub-Saharan Africa [3]. In the past 5 years in Ethiopia, no significant change in neonatal mortality was reported between 2016 and 2019 [19]. Yet studies done in the country are mainly devoted to neonates admitted in hospitals [20,21,22] and a small-scale communities [23]. These studies potentially lack national representativeness. In addition, other studies which analyzed the 2016 Ethiopian demographic and health survey data [8, 24, 25], didn’t consider the spatial analysis and are not timely for future planning. Thus, investigating geographic locations of a high burden of neonatal death and identifying contributing factors based on current data could be supportive of interventions to achieve the Sustainable Development Goal (SDG).
Methods
Study area
The mini-Ethiopian demographic and health survey (EDHS) was done in Ethiopia, a country in the Horn of East Africa. The country is of diverse geography and population. Since May 1991, the country is arranged into nine regional administrative states and two city administrations. The regions are further subdivided into 68 zones, 817 districts, and 16,253 kebeles administrative structures [4]. In the country, health service is structured into a three-tier system: primary, secondary, and tertiary levels of care [26].
Data source and sampling procedure
This, secondary data analysis, is done by using the 2019 mini–Ethiopian Demographic and Health Survey (EDHS) data set. The sampling frame used in the survey was the census enumeration areas (EAs) created for the upcoming Ethiopian Population and Housing Census (PHC).
The EDHS is a nationally representative two-stage cluster cross-sectional survey. As described in detail in the EDHS 2019 report [19], in the first stage, 305 EAs (93 urban and 212 rural) were selected with probability proportional to EAs size and with independent selection for each sampling stratum (urban and rural). Then, in the second stage, 30 fixed households per cluster were selected with an equal probability of systematic selection. In the current study, as shown in the figure (Fig. 1), a weighted total of 24,136 mothers in the reproductive age (15–49 year) group and a weighted neonatal and early neonatal deaths, as well as the total number of children even born from each mother were included.
Study variables
The definition of the outcome variables of this study was made according to the World Health Organization (WHO) classification that can be accessed from https://www.who.int/data/gho/indicator-metadata-registry/imr-details/67. Accordingly, Early Neonatal Death (END) in this analysis was defined as the death of a newborn baby between zero and 7 days after birth. Whereas, Neonatal Death (ND) was defined as the death of a newborn baby between zero and 28 days after birth.
Early neonatal and neonatal deaths were measured and coded as “Yes = 1" whether the mothers ever experienced it in their lifetime and “No = 0" when they never had. In the data set the death and its corresponding date since birth was reported. From this information, END and ND were computed by dividing them by the total live births ever given by mothers and multiplying the result by 1000.
The independent variables used in this analysis were both individual and community-level variables. Maternal age, maternal education attainment, wealth index, number of babies at birth, sex of the child, and birth order were among individual-level variables. Whereas, region, place of residence, altitude of the residence, and community-level poverty were among community-level variables.
Community-level poverty was generated by aggregating individual-level variables at the community (cluster) level. The poorest and poorer family income categories were re-categorized as ‘poor’. Then, the prevalence of the new variable was divided by the cluster size, and the generated value was further categorized as ‘low’ and ‘high’ based on the median value.
Data analysis
Statistical analysis
The sociodemographic and reproductive characteristics of the study participants, and the outcome variable were described in frequency and percentage. Both descriptive and regression analyses were done by Stata 14.0 statistical software.
A multilevel (cluster/enumeration areas and individual level) mixed-effect binary logistic regression model was used to analyze the association between the outcome and independent variables. Four models were used in this analysis. The first, namely, the null model (Model I) was used to check the variability of neonatal mortality in the cluster/community/enumeration areas. Model I provided evidence to calculate random effect by using an interclass correlation (ICC) whereas, the other three models, multilevel mixed-effect models, were used to identify factors associated with outcome variables. The three models were, Model II, a model comprised of individual-level independent variables, Model III, of the community-level variables, and Model IV, the final multivariable model that included both individual and community-level variables. In the last three models, independent variables that had an association with early neonatal and neonatal mortality at a p-value of < 0.2 during bivariate analysis were considered. In the final model, an odds ratio, its 95% confidence interval, and a p-value of < 0.05 were used to declare statistical significance.
Measures of variation (random effect) were estimated by using intraclass correlation (ICC) of ≥0.05, median odds ratio (MOR), and proportional change in the variance (PCV). The details of these estimations were discussed elsewhere in scientific articles [27,28,29,30]. Finally, models were compared based on deviance and the final which had the lowest deviance was considered the best-fitted model.
Spatial analysis
In the EDHS dataset, 305 clusters or EAs with their corresponding latitude and longitude coordinates were included. The Global Moran’s I statistics was done by using ArcMap 10.8 to evaluate whether the pattern of neonatal death is clustered, random, or dispersed across the study clusters. For the clustered outcome variable (based on Moran’s index p-value), spatial interpolation by using ArcMap 10.8 was computed to predict the burden of mortality in the country. Also, scan statistics by using a Bernoulli probability model of SaTScan V.9.6 were carried out to detect clusters and a scanning window with low or high rates of mortality. Relative risk, log-likelihood ratio, and p-value were reported and the statistical significance of the hot spot cluster/scanning window was declared by a p-value of < 0.05.
Results
Sociodemographic, reproductive, and neonatal mortality-related characteristics of study participants
A total of 24,136 weighted samples of mothers were included in the analysis. The age of mothers ranges from 15 to 49 years with a median age of 35 (IQR = 39–40) years. Nearly two-thirds (67.64%) of mothers had not attended formal education and only about a fiftieth (1.97%) of mothers attended secondary and above level of education. Concerning reproductive characteristics, almost two-thirds (66.05%) of mothers gave birth to five and more children (Table 1).
The weighted lifetime early neonatal mortality amongst mothers in Ethiopia was 5.08 (95% CI: 4.13–6.03) per 1000 births. Similarly, the weighted neonatal mortality was 6.54 (5.55, 7.52) per 1000 births. The mortality was higher among mothers younger than 30 years of age with a twice higher rate among teenage mothers. Also, among mothers who gave twin births and those whose birth order was one, both early neonatal and neonatal mortality were found to be high (Table 1).
Spatial distribution of neonatal mortality
The global spatial autocorrelation revealed a clustering pattern of neonatal mortality across the EAs (Moran’s index = 0.100460, z-score = 2.324555, p-value = 0.020096) (Fig. 2). In addition, kriging interpolation analysis predicted that neonatal mortality was relatively higher in northwestern, central, and southeast Amhara. Similarly, most areas of Benshangul Gumz, southern Gambela, and northwest SNNP regions had a mortality rate of > 8 per 1000 births. The neonatal mortality rate in most of the remaining parts of the country was between 4.3–8.3 per1000 births (Fig. 3).
Also, a SaTScan analysis detected a total of three statistically significant cluster areas with high neonatal mortality. The most likely primary cluster area with the highest neonatal mortality was detected in the Amhara region of south Gondar, Gojjam, Wollo, Oromo, Wag Himra, north Shewa zones, and Argoba woreda. In addition, the Oromia region of west and north Shewa, Afar region of zones 1, 3, 4, and 5, and Addis Ababa City were among the primary clusters with a relative risk of (RR) = 1.67, p-value = < 0.001). Another most likely secondary cluster area with high neonatal mortality was spotted in the Oromia region of east Welega of Diga. The remaining secondary cluster areas were detected in the Harari region, Oromia region of east Hararge and east Bale, and the Somali region of Nogab, Jarar, Fafan, and Shabelle zones (Fig. 4, Table 2).
Random effect and model comparison
Random effect or community variation was assessed by ICC, MOR, and PCV. The ICC in the null model of early neonatal and neonatal mortality was 0.081 and 0.072 respectively. As indicated in the ICC result, about 8% of the variation of early neonatal mortality and 7% of neonatal mortality was attributable to the differences at the cluster level factors. The higher value of MOR (1.8) in the null model also indicated that neonatal mortality was different between clusters. In addition, the PCV value in the final model indicated that 35.75% of early neonatal mortality and 28.23% of neonatal mortality were attributable to both individual and community-level factors. Moreover, the four models were compared to select the fit model so that the final model which had the lowest deviance was considered the best-fitted model (Table 3).
Factors associated with early neonatal and neonatal mortality
Demographic and reproductive variables were analyzed in the bivariate multilevel logistic regression model. The variables which were associated with early neonatal and neonatal mortality at a p-value of 0.2 were further analyzed in multivariable multilevel mixed effect models (Model II and III). In the final model (Model IV), both individual-level and community-level variables were fitted to control confounders and to identify statistically significant factors of early neonatal and neonatal mortality (Tables 4 and 5).
Accordingly, the final model revealed that mothers whose current age was 15–19 years were about twofold [Adjusted odds ratio (AOR) = 2.16, 95% CI: 1.04, 4.51] more likely to have neonatal mortality than elder-aged mothers. Also, mothers who didn’t complete primary education were likely to experience both early neonatal and neonatal mortality. Not completing primary education among mothers resulted in above two and three times more likely mortality of early neonates (AOR = 2.61, 95% CI: 1.03, 6.59) and neonates (AOR = 3.12, 95% CI: 1.22, 7.94) than educated mothers respectively. Likewise, mothers who didn’t attend formal education were nearly three times more likely to have neonatal mortality than educated mothers (AOR = 3.12, 95% CI: 1.24, 7.87) (Tables 4 and 5).
Early neonatal and neonatal mortality was also attributed to neonatal factors. Mothers who gave birth to twin babies had a higher than a threefold chance of early neonatal mortality (AOR = 3.79, 95% CI: 2.48, 5.79), while about five times more likely mortality of neonates (AOR = 5.01, 95% CI: 3.32, 7.56). Similarly, mothers who gave birth to male neonates had a higher chance of both early neonatal and neonatal mortality than female neonates (Tables 4 and 5).
Community-level variables didn’t show a statistically significant association for both neonatal and early neonatal mortality in the final model, Model IV. However, mothers who live in a specific altitude area were more likely to have both early neonatal and neonatal mortality in Model III. As compared to middle or temperate altitudes, mothers who live in an area of lowland altitude had a greater likelihood of early neonatal (AOR = 1.54, 95% CI: 1.05, 2.26) and neonatal (AOR = 1.41, 95% CI: 1.01, 1.98) mortality (Tables 4 and 5).
Discussion
Neonatal mortality is a worldwide public health issue and one of the leading health concerns in low-and-middle-income countries [1, 3, 31]. This study detected significant hotspot areas and identified community and individual-level factors that contributed to neonatal and early neonatal mortality in Ethiopia.
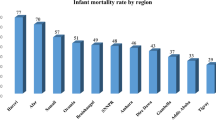
Neonatal mortality in Ethiopia is geographically clustered in wide areas of the Amhara and Afar regions and some areas of the Somali region and eastern zones of the Oromia region. Similarly, a higher geographic variation of neonatal mortality in the 2016 EDHS was reported and it was revealed that the rate was high in Oromia and Afar regions next to Amhara and Somali regions [4]. Neonatal mortality was found to be predicted by maternal education attainment, less antenatal attendance [32, 33], adolescent pregnancy [33], and home births [5]. This attribution could be informative for the aforementioned regions and areas of high neonatal mortality in Ethiopia. As indicated in reports, in the clusters of high neonatal death, more than 70% of mothers were not accessing any form of media (> 80% in the Amhara region), more than 80% of mothers didn’t complete elementary education, > 65% didn’t attend at least four visits of antenatal care, > 70% gave birth at home, and only < 30% of births were assisted by skilled attendants [4]. Also, in the Amhara region, most neonates die in the perinatal period due to prolonged labor and its complication, ruptured uterus [34]. Though neonatal mortality in Ethiopia showed a 41% reduction from 49/1000 livebirths in 2000 to 29/1000 livebirths in 2016, the regional distribution has remained higher in Afar, Amhara, Oromia, and Somali regions with the persistently highest rate (47/1000 live births) in the Amhara region [4].
In addition, low birth weight, neonatal morbidity, and maternal morbidity were found to be predictors of neonatal mortality in Ethiopia [35, 36]. Maternal nutrition and morbidities are also directly associated with low birth weight among newborn babies [37,38,39,40] and nutritional intervention is recommended to avert low birth weight thereby neonatal mortality [41,42,43]. In Ethiopia, studies revealed that pregnant mothers are suffering from malnutrition due to inadequate food diversity and household food insecurity [44, 45], and these further result in low birth weight and preterm birth [40, 46, 47] as well as directly in neonatal mortality [48]. Food insecurity is common in Ethiopia as revealed by studies [49,50,51] and significant food insecurity was observed in lowland and highland areas than in midland areas [51].
Neonatal death is statistically significant among teenage mothers in Ethiopia. Mothers whose age ranges between 15 and 19 years were about four times and those between 25 and 29 years were nearly two times more likely to have neonatal death than elderly mothers. Studies [52,53,54,55,56,57,58] also revealed an association between maternal age and neonatal death. There is evidence that teenagers during pregnancy face many obstetric complications like anemia, urinary tract infection, pregnancy-induced hypertension, and preterm births [59]. Among the common obstetric complications that teenagers experience, preterm birth alone increases the risk of neonatal mortality in this age group of mothers [58]. Higher neonatal mortality among younger-age mothers in this study could reflect that developing countries are still having higher neonatal mortality in the late Millenium Development Goals (MDG) and Sustainable Development Goals (SDG) era and might continue to have it in the future [3].
Mothers who didn’t attend formal education and those who didn’t complete primary education had close to three times more likely risk of early neonatal and neonatal mortality in Ethiopia. Maternal level of educational attainment was also found a predictor of neonatal death in other studies [56, 60]. In Ethiopia, female education could be affected by the deep-rooted practice of early marriage, which in turn is associated with lower education and economic dependence [61, 62]. Educated and employed mothers are more empowered to decide using maternal and childcare services [63]. It is suggested that educating girls and accessing maternal health services are among the key interventions to reduce neonatal mortality [64, 65].
Neonatal and early neonatal mortality is higher among mothers who gave male birth than female birth. Death among males was found to be one and half times higher in Ethiopia. Several studies conducted so far in Ethiopia similarly identified higher mortality among male neonates [23, 66, 67]. Similarly, as supported by other studies [67,68,69] done in sub-Saharan Africa, mothers who gave twin birth had about four and more times higher likelihood of death than singleton births in this study. Higher death amongst twin births could be related to significantly higher preterm birth and anomaly, and lower Apgar and birth weight [70]. Whereas, though the sex variation of mortality is inconclusive, some studies explored more susceptibility to infection, prematurity, and poor perinatal conditions in male neonates than in females [71,72,73,74].
Although the government of Ethiopia executed different health-related goals of the Millennium Development Goal (MDG) and still implementing the Sustainable Development Goal (SDG), neonatal mortality in the country remained high [19]. In the health sector transformation plan [75], Ethiopia was proposed to achieve over 90% coverage of 4+ antenatal care, deliveries attended by skilled health professionals, antiretroviral therapy for HIV-positive pregnant mothers, and postnatal care to reduce neonatal mortality to the level of 10/1000 live births in 2020. The proposed time to reduce neonatal mortality was passed, yet the Ethiopian neonatal mortality estimate for 2019 showed 27/1000 live births [76]. As revealed by some studies, among the individual interventions believed to improve neonatal health, such as health facility construction campaigns [77] and institutional delivery [78] contributed a little. Countries like Ethiopia should adapt an integrated evidence-based continuum of care approaches than a fragmented individual intervention. Therefore, as revealed and suggested by a recent Live Saved Tools Modeling study to estimate the number of deaths that would be prevented by 2035, countries that account for the vast majority of the world’s maternal and neonatal deaths and stillbirths can potentially avert the problem substantially by installing midwife-led sexual, reproductive, maternal, newborn, and adolescent interventions [79].
In this analysis, large data was used and statistically significant clusters of neonatal mortality in Ethiopia were identified. However, this analysis is mainly focused on determining the lifetime experience of neonatal mortality among mothers in Ethiopia. To understand the current magnitude and determinates of neonatal mortality, analyzing the data from a recent 5 years period would be helpful.
Conclusion
Neonatal mortality in Ethiopia is common and actionable socio-demographic and obstetric factors were found to predict it. Also, it is geographically clustered and Amhara and Afar regions are widely affected areas in the country. Policymakers should focus on evidence-based recommendations such as; midwives-led community and facility-based continuum of care from preconception through prenatal, intranatal, postnatal, and neonatal periods to possibly reduce neonatal mortality.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the DHS program repository, [https://dhsprogram.com/] upon registration with no requirement of accession number.
Abbreviations
- DHS:
-
Demographic and Health Survey
- EAs:
-
Enumeration Areas
- EDHS:
-
Ethiopian Demographic and Health Survey
- END:
-
Early Neonatal Death
- ICC:
-
Intraclass Correlation Coefficients
- LL:
-
Log Likely
- MMR:
-
Maternal Mortality Ratio
- ND:
-
Neonatal Death
- NGO:
-
Non-Governmental Organizations
- PHC:
-
Population and Housing Census
References
WHO, UNICEF. Reaching the every newborn national 2020 milestones: country progress, plans and moving forward: World Health Organization; 2017. Cited 2021 May 26.
Hug L, Alexander M, You D, Alkema L, for Child UI-aG. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. The lancet. Glob Health. 2019;7(6):e710–e20.
UNICEF, WHO, World Bank Group, United Nations. Levels and trends in child mortality report 2017: UNICEF; 2017. Cited 2021 May 26.
Central Statistical Agency (CSA) [Ethiopia], ICF. Ethiopia Demographic and health survey 2016. Addis Ababa and Rockville: CSA and ICF; 2016.
Gudayu TW, Zeleke EG, Lakew AM. Time to death and its predictors among neonates admitted in the intensive care unit of the University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia. Res Rep Neonatol. 2020;10:1–10.
Warren JB, Lambert WE, Fu R, Anderson JM, Edelman AB. Global neonatal and perinatal mortality: a review and case study for the Loreto Province of Peru. Res Rep Neonatol. 2012;2:103–13.
Roro EM, Tumtu MI, Gebre DS. Predictors, causes, and trends of neonatal mortality at Nekemte referral hospital, east Wollega zone, western Ethiopia (2010–2014). Retrospective cohort study. PLoS One. 2019;14(10):e0221513.
Wolde HF, Gonete KA, Akalu TY, Baraki AG, Lakew AM. Factors affecting neonatal mortality in the general population: evidence from the 2016 Ethiopian demographic and health survey (EDHS)—multilevel analysis. BMC Res Notes. 2019;12(1):1–6.
Aminu M, Unkels R, Mdegela M, Utz B, Adaji S, Van Den Broek N. Causes of and factors associated with stillbirth in low-and middle-income countries: a systematic literature review. BJOG Int J Obstet Gynaecol. 2014;121:141–53.
Amare D, Mela M, Dessie G. Unfinished agenda of the neonates in developing countries: magnitude of neonatal sepsis: systematic review and meta-analysis. Heliyon. 2019;5(9):e02519.
Atrash H, Jack B. Preconception care to improve pregnancy outcomes: the science. J Human Growth Dev. 2020;30(3):355–62.
Lassi ZS, Kedzior SG, Tariq W, Jadoon Y, Das JK, Bhutta ZA. Effects of preconception care and periconception interventions on maternal nutritional status and birth outcomes in low-and middle-income countries: a systematic review. Nutrients. 2020;12(3):606.
Shukla VV, Carlo WA. Review of the evidence for interventions to reduce perinatal mortality in low-and middle-income countries. Int J Pediatr Adolesc Med. 2020;7(1):4–10.
Innerdal M, Simaga I, Diall H, Eielsen M, Niermeyer S, Eielsen O, et al. Reduction in perinatal mortality after implementation of HBB training at a district hospital in Mali. J Trop Pediatr. 2020;66(3):315–21.
Colbourn T, Nambiar B, Bondo A, Makwenda C, Tsetekani E, Makonda-Ridley A, et al. Effects of quality improvement in health facilities and community mobilization through women's groups on maternal, neonatal and perinatal mortality in three districts of Malawi: MaiKhanda, a cluster randomized controlled effectiveness trial. Int Health. 2013;5(3):180–95.
Akombi BJ, Renzaho AM. Perinatal mortality in sub-Saharan Africa: a meta-analysis of demographic and health surveys. Ann Glob Health. 2019;85(1):106.
Gabrysch S, Nesbitt RC, Schoeps A, Hurt L, Soremekun S, Edmond K, et al. Does facility birth reduce maternal and perinatal mortality in Brong Ahafo, Ghana? A secondary analysis using data on 119 244 pregnancies from two cluster-randomised controlled trials. Lancet Glob Health. 2019;7(8):e1074–e87.
Tiruneh GT, Getu YN, Abdukie MA, Eba GG, Keyes E, Bailey PE. Distribution of maternity waiting homes and their correlation with perinatal mortality and direct obstetric complication rates in Ethiopia. BMC Pregnancy Childbirth. 2019;19(1):1–11.
Ethiopian Public Health Institute (EPHI) [Ethiopia], ICF. Ethiopia Mini demographic and health survey 2019: key indicators. Rockville: EPHI and ICF; 2019.
Seid SS, Ibro SA, Ahmed AA, Akuma AO, Reta EY, Haso TK, et al. Causes and factors associated with neonatal mortality in neonatal intensive care unit (NICU) of Jimma University medical center, Jimma, south West Ethiopia. Pediatric Health Med Ther. 2019;10:39.
Elmi Farah A, Abbas AH, Tahir AA. Trends of admission and predictors of neonatal mortality: a hospital based retrospective cohort study in Somali region of Ethiopia. PLoS One. 2018;13(9):e0203314.
Orsido TT, Asseffa NA, Berheto TM. Predictors of neonatal mortality in neonatal intensive care unit at referral Hospital in Southern Ethiopia: a retrospective cohort study. BMC Pregnancy Childbirth. 2019;19(1):1–9.
Kolola T, Ekubay M, Tesfa E, Morka W. Determinants of neonatal mortality in north Shoa zone, Amhara regional state, Ethiopia. PLoS One. 2016;11(10):e0164472.
Basha GW, Woya AA, Tekile AK. Determinants of neonatal mortality in Ethiopia: an analysis of the 2016 Ethiopia demographic and health survey. Afr Health Sci. 2020;20(2):715–23.
Tesema GA, Worku MG. Individual-and community-level determinants of neonatal mortality in the emerging regions of Ethiopia: a multilevel mixed-effect analysis. BMC Pregnancy Childbirth. 2021;21(1):1–11.
Federal Democratic Republic of Ethiopia Minstry of Health. Health sector development programme IV (2010/11–2014/15). 2010.
Goldstein H, Browne W, Rasbash J. Partitioning variation in multilevel models. Understanding statistics. 2002;1(4):223–31.
Merlo J, Chaix B, Yang M, Lynch J, Råstam L. A brief conceptual tutorial of multilevel analysis in social epidemiology: linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Community Health. 2005;59(6):443–9.
Merlo J, Chaix B, Yang M, Lynch J, Råstam L. A brief conceptual tutorial on multilevel analysis in social epidemiology: interpreting neighbourhood differences and the effect of neighbourhood characteristics on individual health. J Epidemiol Community Health. 2005;59(12):1022–9.
Huang FL. Alternatives to multilevel modeling for the analysis of clustered data. J Exp Educ. 2016;84(1):175–96.
Blencowe H, Cousens S, Jassir FB, Say L, Chou D, Mathers C, et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health. 2016;4(2):e98–e108.
Belachew A, Tewabe T, Dessie G. Neonatal mortality and its association with antenatal care visits among live births in Ethiopia: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2022;35(2):348–55.
McKinnon B, Harper S, Kaufman JS. Do socioeconomic inequalities in neonatal mortality reflect inequalities in coverage of maternal health services? Evidence from 48 low-and middle-income countries. Matern Child Health J. 2016;20(2):434–46.
Desta M, Kassa GM, Getaneh T, Sharew Y, Alemu AA, Birhanu MY, et al. Maternal and perinatal mortality and morbidity of uterine rupture and its association with prolonged duration of operation in Ethiopia: a systematic review and meta-analysis. PLoS One. 2021;16(4):e0245977.
Alemu AY, Belay GM, Berhanu M, Minuye B. Determinants of neonatal mortality at neonatal intensive care unit in Northeast Ethiopia: unmatched case-control study. Trop Med Health. 2020;48:1–10.
Kebede B, Gebeyehu A, Sharma HR, Yifru S. Prevalence and associated factors of neonatal mortality in North Gondar zone, Northwest Ethiopia. Ethiop J Health Dev. 2012;26(2):66–71.
Walsh JM, McAuliffe FM. Impact of maternal nutrition on pregnancy outcome–does it matter what pregnant women eat? Best Pract Res Clin Obstet Gynaecol. 2015;29(1):63–78.
Mahumud RA, Sultana M, Sarker AR. Distribution and determinants of low birth weight in developing countries. J Prev Med Public Health. 2017;50(1):18.
He Z, Bishwajit G, Yaya S, Cheng Z, Zou D, Zhou Y. Prevalence of low birth weight and its association with maternal body weight status in selected countries in Africa: a cross-sectional study. BMJ Open. 2018;8(8):e020410.
Desalegn M, Terefe B, Bikila H. Effect of food insecurity and other possible factors associated with low birth weight among mothers who gave birth to live newborns in West Ethiopia: a facility-based unmatched case–control study. Nutr Diet Suppl. 2021;13:133.
Nnam N. Improving maternal nutrition for better pregnancy outcomes. Proc Nutr Soc. 2015;74(4):454–9.
Zerfu TA, Umeta M, Baye K. Dietary diversity during pregnancy is associated with reduced risk of maternal anemia, preterm delivery, and low birth weight in a prospective cohort study in rural Ethiopia. Am J Clin Nutr. 2016;103(6):1482–8.
Hanson MA, Bardsley A, De-Regil LM, Moore SE, Oken E, Poston L, et al. The International Federation of Gynecology and Obstetrics (FIGO) recommendations on adolescent, preconception, and maternal nutrition:“think nutrition first”#. Int J Gynecol Obstet. 2015;131:S213–S53.
Nigatu M, Gebrehiwot TT, Gemeda DH. Household food insecurity, low dietary diversity, and early marriage were predictors for undernutrition among pregnant women residing in Gambella, Ethiopia. Adv Public Health. 2018;2018.
Hidru HD, Berwo Mengesha M, Hailesilassie Y, Tekulu WF. Burden and determinant of inadequate dietary diversity among pregnant women in Ethiopia: a systematic review and Meta-analysis. J Nutr Metab. 2020;2020:1272393.
Sahlu D, Deyessa N, Firdu N, Asfaw S. Food insecurity and other possible factors contributing to low birth weight: a case control study in Addis Ababa, Ethiopia. Asian Pac J Reprod. 2020;9(4):174.
Richterman A, Raymonville M, Hossain A, Millien C, Joseph JP, Jerome G, et al. Food insecurity as a risk factor for preterm birth: a prospective facility-based cohort study in rural Haiti. BMJ Glob Health. 2020;5(7):e002341.
Augusto ALP, de Abreu Rodrigues AV, Domingos TB, Salles-Costa R. Household food insecurity associated with gestacional and neonatal outcomes: a systematic review. BMC Pregnancy Childbirth. 2020;20(1):1–11.
Motbainor A, Worku A, Kumie A. Level and determinants of food insecurity in east and west Gojjam zones of Amhara region, Ethiopia: a community based comparative cross-sectional study. BMC Public Health. 2016;16(1):1–13.
Abdu J, Kahssay M, Gebremedhin M. Household food insecurity, underweight status, and associated characteristics among women of reproductive age group in Assayita District, Afar regional state, Ethiopia. J Environ Public Health. 2018;2018:7659204.
Alemu ZA, Ahmed AA, Yalew AW, Simanie B. Spatial variations of household food insecurity in east Gojjam zone, Amhara region, Ethiopia: implications for agroecosystem-based interventions. Agric Food Secur. 2017;6(1):1–9.
Kozuki N, Lee AC, Silveira MF, Sania A, Vogel JP, Adair L, et al. The associations of parity and maternal age with small-for-gestational-age, preterm, and neonatal and infant mortality: a meta-analysis. BMC Public Health. 2013;13(3):1–10.
Kamal SM. What is the association between maternal age and neonatal mortality? An analysis of the 2007 Bangladesh demographic and health survey. Asia Pacific. J Public Health. 2015;27(2):NP1106–NP17.
Kang G, Lim JY, Kale AS, Lee LY. Adverse effects of young maternal age on neonatal outcomes. Singap Med J. 2015;56(3):157.
Kim Y-N, Choi D-W, Kim DS, Park E-C, Kwon J-Y. Maternal age and risk of early neonatal mortality: a national cohort study. Sci Rep. 2021;11(1):814.
Fonseca SC, Flores PVG, Camargo KR Jr, Pinheiro RS, Coeli CM. Maternal education and age: inequalities in neonatal death. Rev Saude Publica. 2017;51:94.
Wu H, Zhao M, Liang Y, Liu F, Xi B. Maternal age at birth and neonatal mortality: associations from 67 low-income and middle-income countries. Paediatr Perinat Epidemiol. 2021;35(3):318–27.
Dhaded SM, Somannavar MS, Vernekar SS, Goudar SS, Mwenche M, Derman R, et al. Neonatal mortality and coverage of essential newborn interventions 2010-2013: a prospective, population-based study from low-middle income countries. Reprod Health. 2015;12(2):1–8.
Leppälahti S, Gissler M, Mentula M, Heikinheimo O. Is teenage pregnancy an obstetric risk in a welfare society? A population-based study in Finland, from 2006 to 2011. BMJ Open. 2013;3(8):e003225.
Grady SC, Frake AN, Zhang Q, Bene M, Jordan DR, Vertalka J, et al. Neonatal mortality in East Africa and West Africa: a geographic analysis of district-level demographic and health survey data. Geospat Health. 2017;12(1).
Malé C, Wodon Q. Basic profile of Child marriage in Ethiopia; 2016.
Raj A, Salazar M, Jackson EC, Wyss N, McClendon KA, Khanna A, et al. Students and brides: a qualitative analysis of the relationship between girls’ education and early marriage in Ethiopia and India. BMC Public Health. 2019;19(1):1–20.
Woldemicael G. Do women with higher autonomy seek more maternal and child health-care? Evidence from Ethiopia and Eritrea: Sociologiska institutionen; 2007.
Saugstad OD. Reducing global neonatal mortality is possible. Neonatology. 2011;99(4):250–7.
Moyer CA, Dako-Gyeke P, Adanu RM. Facility-based delivery and maternal and early neonatal mortality in sub-Saharan Africa: a regional review of the literature. Afr J Reprod Health. 2013;17(3):30–43.
Limaso AA, Dangisso MH, Hibstu DT. Neonatal survival and determinants of mortality in Aroresa district, southern Ethiopia: a prospective cohort study. BMC Pediatr. 2020;20(1):33.
Mitiku HD. Neonatal mortality and associated factors in Ethiopia: a cross-sectional population-based study. BMC Womens Health. 2021;21(1):1–9.
Debelew GT, Afework MF, Yalew AW. Determinants and causes of neonatal mortality in Jimma zone, Southwest Ethiopia: a multilevel analysis of prospective follow up study. PLoS One. 2014;9(9):e107184.
Monden CW, Smits J. Mortality among twins and singletons in sub-Saharan Africa between 1995 and 2014: a pooled analysis of data from 90 demographic and health surveys in 30 countries. Lancet Glob Health. 2017;5(7):e673–e9.
Rezavand N, Veisi F, Malek-Khosravi S, Zangeneh M, Kohzadi M. Assessment of frequency of twin pregnancy and neonatal outcome in deliveries of Mo’tazedi hospital, Kermanshah in 2004–2007. J Obstet Gynecol India. 2014;64(1):19–22.
Lawn JE, Cousens S, Zupan J, Team LNSS. 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365(9462):891–900.
Drevenstedt GL, Crimmins EM, Vasunilashorn S, Finch CE. The rise and fall of excess male infant mortality. Proc Natl Acad Sci. 2008;105(13):5016–21.
Green MS. The male predominance in the incidence of infectious diseases in children: a postulated explanation for disparities in the literature. Int J Epidemiol. 1992;21(2):381–6.
Bouman A, Heineman MJ, Faas MM. Sex hormones and the immune response in humans. Hum Reprod Update. 2005;11(4):411–23.
The Federal Democratic Republic of Ethiopia Ministry of Health. Health sector transformation plan (2015/16–2019/20). 2015.
Tefera YG, Ayele AA. Newborns and Under-5 mortality in Ethiopia: the necessity to revitalize Partnership in Post-COVID-19 era to meet the SDG targets. J Prim Care Community Health. 2021;12:2150132721996889.
Croke K, Mengistu AT, O'Connell SD, Tafere K. The impact of a health facility construction campaign on health service utilisation and outcomes: analysis of spatially linked survey and facility location data in Ethiopia. BMJ Glob Health. 2020;5(8):e002430.
Lohela TJ, Nesbitt RC, Pekkanen J, Gabrysch S. Comparing socioeconomic inequalities between early neonatal mortality and facility delivery: cross-sectional data from 72 low-and middle-income countries. Sci Rep. 2019;9(1):1–11.
Nove A, Friberg IK, de Bernis L, McConville F, Moran AC, Najjemba M, et al. Potential impact of midwives in preventing and reducing maternal and neonatal mortality and stillbirths: a lives saved tool modelling study. Lancet Glob Health. 2021;9(1):e24–32.
Acknowledgments
I greatly acknowledge the DHS program for approving the request and granting access to use the mini-Ethiopian demographic and health survey data set.
Funding
The author declares that he has no source of funding involved in this secondary data analysis.
Author information
Authors and Affiliations
Contributions
TWG obtained permission to use the dataset, identified research question, reviewed available works of literature, analyzed and interpreted results, wrote up the manuscript, and reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The survey was implemented by the Ethiopian Public Health Institute in partnership with Central Statistical Agency and the Federal Ministry of Health. It followed formal ethical approval and consent; therefore, further ethical approval was not required in this secondary data analysis. The DHS program was communicated for the data set used in this analysis and permission was granted to download and use the data from https://dhsprogram.com/Data/terms-of-use.cfm. The geographic identifiers were limited at the regional and EAs level that was a large geographical area. And individual-level variables and the aggregated community variables were not included any personal identifiers like names, house numbers, and phone numbers.
Consent for publication
Not applicable.
Competing interests
The author declares that he has no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gudayu, T.W. Epidemiology of neonatal mortality: a spatial and multilevel analysis of the 2019 mini-Ethiopian demographic and health survey data. BMC Pediatr 23, 26 (2023). https://doi.org/10.1186/s12887-023-03838-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-03838-0