Abstract
Background
Neurally adjusted ventilatory assist is an emerging mode of respiratory support that uses the electrical activity of the diaphragm (Edi) to provide synchronised inspiratory pressure support, proportional to an infant’s changing inspiratory effort. Data on Edi reference values for neonates are limited. The objective of this study was to establish reference Edi values for preterm and term neonates who are not receiving respiratory support.
Methods
This was a prospective observational study of newborn infants breathing spontaneously in room air. The Edi waveform was monitored by a specialised naso/orogastric feeding tube with embedded electrodes positioned at the level of the diaphragm. Edi minimums and peaks were recorded continuously for 4 h without changes to routine clinical handling.
Results
Twenty-four newborn infants (16 preterm [< 37 weeks’ gestation]; 8 term) were studied. All infants were breathing comfortably in room air at the time of study. Edi data were successfully captured in all infants. The mean (±SD) Edi minimum was 3.02 (±0.94) μV and the mean Edi peak was 10.13 (±3.50) μV. In preterm infants the mean (±SD) Edi minimum was 3.05 (±0.91) μV and the mean Edi peak was 9.36 (±2.13) μV. In term infants the mean (±SD) Edi minimum was 2.97 (±1.05) μV and the mean Edi peak was 11.66 (±5.14) μV.
Conclusion
Reference Edi values were established for both preterm and term neonates. These values can be used as a guide when monitoring breathing support and when using diaphragm-triggered modes of respiratory support in newborn infants
Similar content being viewed by others
Background
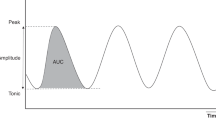
The initiation of a spontaneous breath by the respiratory centre of the brain results in the electrical excitation of the diaphragm via the phrenic nerve and subsequent diaphragmatic contraction to facilitate an inflow of air. Recently, new technology has become available that can measure diaphragmatic excitation and associated electrical activity of the diaphragm (Edi) [1]. This is achieved using an Edi catheter, which is a specialised naso/orogastric tube that has electrodes embedded at the level of the gastro-oesophageal junction. The catheter assesses neural respiratory control by measuring the total action potentials of the motor units in the diaphragmatic crura [1], representative of phrenic nerve activity and global diaphragm activation [2]. The Edi is presented as a waveform with a cyclic pattern that has distinctive peak and minimum values. There are two key measures from this Edi waveform: (1) Edi minimum (the end expiratory Edi value [just prior to the subsequent inspiration]); and (2) Edi peak (the amplitude of electrical activity associated with inspiratory effort) [3].
These Edi waveforms can be filtered, processed and relayed to a ventilator, which can then provide synchronised inspiratory pressure support. The ventilator provides support that is proportional to inspiratory effort, based on the difference between the Edi peak and Edi minimum. This modality, referred to as neurally adjusted ventilatory assist (NAVA), is an emerging mode of respiratory support that can be utilised either non-invasively via nasal prongs or mask, or invasively [4]. Over 100 clinical and experimental studies have demonstrated the benefit of neural monitoring and ventilator assist control compared to conventional modes of ventilation, during both non-invasive and invasive ventilation. These studies have shown that NAVA improves patient-ventilator interaction, offering equivalent or improved physiological outcomes and favourable ventilator parameters (lower peak inspiratory pressures and down-regulation of Edi to limit over-assist) [5, 6].
Although several studies have evaluated the clinical use of NAVA in newborn infants, reference Edi data in healthy neonates have previously only been collected in two studies, involving 20 infants [3, 7]. However, data pertaining to healthy preterm and term infants not requiring respiratory support is limited. Establishing reference values for this population is important for the clinical utility of this technology. Excessive respiratory support can suppress an infant’s natural respiratory drive while under supporting breathing is also detrimental [8]. The potential morbidity and mortality associated with incorrect support is well established [9].
This observational study of preterm and term newborn infants aimed to establish reference Edi values. We also sought to determine how these values vary according to sleeping states, feeding and skin-to-skin care.
Methods
Patient selection
Newborn infants born at 29–42 weeks’ gestation who were admitted to the Neonatal Intensive Care Unit (NICU) at the Royal Hospital for Women were opportunistically recruited for this prospective observational study. Inclusion criteria required that neonates were on room air with no current respiratory issues and with a naso/orogastric feeding tube in situ. Exclusion criteria included infants that had been on respiratory support within the last week, congenital lung anomalies, major neurological conditions and brain anomalies, neuromuscular diseases and conditions affecting innervation of the diaphragm.
Study procedure
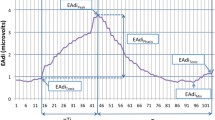
An Edi catheter (6 Fr) was inserted when the infant’s conventional naso/orogastric feeding tube was due to be changed as per unit policy. The Edi catheter was positioned at the level of the diaphragm (starting with a measurement of the direct distance from nose to earlobe to xiphisternum [NEX]) and the correct position confirmed by analysis using Servo-n software (Getinge AB Gothenburg, Sweden). The Edi waveform was recorded continuously for the duration of the study. It was adjusted so that in the “catheter positioning screen”, the Edi waveform, superimposed as a pink waveform, was noted to occur on the middle 2 out of 4 retro-cardiac ECG tracing. Data output from the Servo-n included Edi peak, Edi min and respiratory rate. The Servo-n stored the data in 1 min (averaged) increments, which were then extracted and analysed. It is important to note that infants may have had sighs (high Edi peak) or apneoas (no Edi waveform), which would not be represented due to this 1 min averaging.
Infants were observed for a continuous four-hour period, resulting in 240 data points for each variable observed (see example Additional file 1). Heart rate and oxygen saturation (SpO2) were also recorded from telemetry monitors every 15 minutes throughout the study. An observer subjectively recorded sleep, awake and feeding states by direct observation, as well as timing skin-to-skin care (defined as continuous skin-to-skin contact in a vertical position on the parent’s chest). Feeding states for comparison were defined as 1 h pre- and post-prandial. During the study period, normal clinical activity was not interrupted. On completion of the observation period, the Edi catheter was left in situ for use as a regular nasogastric tube. All infants were studied for a single 4 h period only.
Statistical analyses
Basic descriptive statistics were performed to calculate population means and standard deviations. Paired sample t-tests were used to compare means between sleep states, feeding and skin-to-skin care. Statistical significance was defined as p < 0.05.
Results
Patient inclusion
A total of 24 infants (16 preterm; 8 term) were enrolled in the study (Table 1). Birth weights ranged from 1270 g to 3490 g, and postnatal age ranged from day 2 to 34. All infants were breathing comfortably in room air at the time of enrolment. Infants were studied for 240 minutes, and all infants completed the study (individual Edi data available Additional file 2). For feeding state comparisons, at least 45 minutes of data was analysed per subject both pre- and post-prandially. Feeding state comparisons could not be conducted for one infant (not feeding at the time of the study).
Average Edi peak, Edi min, respiratory rate, heart rate and oxygen saturation across all 24 infants are presented in Table 2. Heart rate, respiratory rate and oxygen saturations were all within the normal range for gestational age. The mean (±SD) Edi minimum was 3.02 (±0.94) μV and the mean (±SD) Edi peak was 10.13 (±3.50) μV. Averaged data for the preterm and term infants are also presented. There was no significant difference in Edi minimum (p = 0.844) or Edi peak (p = 0.259) between preterm and term infants. Based on data from the entire cohort, the reference ranges (defined as mean ± 2 SD) for Edi minimum and Edi peak would be 1–5 μV and 3–17 μV, respectively.
Edi minimum and Edi peak were compared during various states (Table 3). There were no differences observed with feeding (pre- vs post-prandial). Edi minimum was significantly higher when infants were awake (4.07 [±1.45] μV vs 2.69 [±0.82] μV; p < 0.001). Similarly, Edi peak was significantly higher when infants were awake (13.43 [±4.49] μV vs 9.11 [±2.92] μV; p < 0.001]. During skin-to-skin care, Edi peaks were significantly lower (7.01 [±0.50] μV vs 10.14 [±3.53] μV; p = 0.013) and less variable (p = 0.04).
Differences between Edi minimums did not reach statistical significance. There were no significant differences between male and female infants.
Discussion
The observational data in this study represent Edi waveforms from a large cohort of healthy preterm and term newborn infants, which we have used to define reference values for Edi minimum (1–5 μV) and Edi peak (3–17 μV). These values can be used as a reference in clinical practice to define a goal for electrical activity in infants requiring respiratory support. This is particularly relevant in infants being supported with NAVA as breathing support is always proportional to the infant’s Edi activity (specifically, proportional to the difference between the Edi peak and Edi minimum). There was no significant difference found between the preterm and term population in the study suggesting that diaphragm electrical activity is similar in infants that are spontaneously breathing without support. This supports the use of these reference values in both preterm and term infants.
We noted that diaphragm electrical activity was significantly higher when infants were awake. This is an expected finding as the sleep stage is characterised by slower, more regular respiration rates [10]. It is also consistent with previous studies, which demonstrated that peak Edi activity was 60% higher in the awake state [3]. Peak Edi was also significantly lower during skin-to-skin care, which has previously been reported and is not surprising given the known positive effects of skin-skin care on cardiorespiratory stability and sleep quality [11,12,13]. It should be noted, however, that only three infants had skin-to-skin care during their respective observation periods.
We found no significant difference in Edi waveforms when comparing waveforms before and after feeds. This is consistent with previous studies investigating changes in Edi with naso/orogastric feeds [14]. There are other studies that have shown a post-prandial decrease in peak Edi, however, this was in a small population of term infants who were suck feeding [3]. The majority of infants in this study were predominantly fed with a naso/orogastric tube, which is likely to explain the discrepancy.
It is important to recognise that the Edi waveform is variable in individual infants. Infants often have irregular, periodic breathing patterns that can fluctuate with time. The effects of clinical variables such as sigh breaths, apnoeas, use of accessory muscles and changing respiratory rate are not reflected when the Edi waveform is averaged. When using reference ranges, the trend in an individual infant’s Edi waveform is more important than any single value. There is also variability between infants, which explains why there is an overlap between the reference ranges for Edi minimum and Edi peak (it is not possible for the Edi minimum to be greater than the Edi peak at any one point in time).
There were some important limitations to acknowledge with respect to this study. Although these data represent the largest reported cohort of spontaneously breathing preterm and term infants, the sample size does not allow for a true reference range based on gestation. We found that the electrical diaphragm activity is similar in preterm infants and term infants, but these were all infants who did not require respiratory support. This reflects an increasingly small percentage of the population as gestation decreases. Consequently, we were not able to recruit infants less than 29 weeks gestation where differences in diaphragm activity may be more apparent. We also acknowledge that the inclusion of infants admitted to a special care nursery may not represent a true healthy newborn population. Although infants were subjectively breathing comfortably at the time of enrolment, some residual subclinical respiratory disease cannot be ruled out. We are reassured that our findings are similar to previous published data [3, 5, 6]. Finally, it is important to note that Edi signals may be affected by equipment and software factors, such as electrode configuration or signal amplification. This again highlights the value of trend monitoring when interpreting Edi data in an individual infant.
Conclusions
In summary, reference Edi minimum and peak values were established for both preterm and term neonates. These values can be used as a guide for clinicians when using diaphragm-triggered modes on respiratory support in newborn infants to ensure an optimal level of respiratory support.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- Edi:
-
Electrical activity of the diaphragm
- SD:
-
Standard deviation
- NAVA:
-
Neurally adjusted ventilatory assist
- NICU:
-
Neonatal Intensive Care Unit
References
Stein H, Beck J, Dunn M. Non-invasive ventilation with neurally adjusted ventilatory assist in newborns. Semin Fetal Neonatal Med. 2016;21(3):154–61.
Beck J, Gottfried SB, Navalesi P, Skrobik Y, Comtois N, Rossini M, et al. Electrical activity of the diaphragm during pressure support ventilation in acute respiratory failure. Am J Respir Crit Care Med. 2001;164(3):419–24.
Stein HM, Wilmoth J, Burton J. Electrical activity of the diaphragm in a small cohort of term neonates. Respir Care. 2012;57(9):1483–7.
Beck J, Brander L, Slutsky AS, Reilly MC, Dunn MS, Sinderby C. Non-invasive neurally adjusted ventilatory assist in rabbits with acute lung injury. Intensive Care Med. 2008;34(2):316–23.
Sinderby C, Beck J. Neurally adjusted ventilatory assist: first indications of clinical outcomes. J Crit Care. 2014;29(4):666–7.
Beck J, Sinderby C. Neurally adjusted Ventilatory assist in newborns. Clin Perinatol. 2021;48(4):783–811.
Stein H, Hall R, Davis K, White D. Electrical activity of the diaphragm (Edi) values and Edi catheter placement in non-ventilated preterm neonates. J Perinatol. 2013;33(9):707.
Brander L, Leong-Poi H, Beck J, Brunet F, Hutchison SJ, Slutsky AS, et al. Titration and implementation of neurally adjusted ventilatory assist in critically ill patients. Chest. 2009;135(3):695–703.
Duyndam A, Bol BS, Kroon A, Tibboel D, Ista E. Neurally adjusted ventilatory assist: assessing the comfort and feasibility of use in neonates and children. Nurs Crit Care. 2013;18(2):86–92.
Tarullo AR, Balsam PD, Fifer WP. Sleep and infant learning. Infant Child Dev. 2011;20(1):35–46.
Baley J. Skin-to-skin care for term and preterm infants in the neonatal ICU. Pediatrics. 2015;136(3):596–9.
Ludington-Hoe SM, Swinth JY. Developmental aspects of kangaroo care. J Obstet Gynecol Neonatal Nurs. 1996;25(8):691–703.
Soukka H, Grönroos L, Leppäsalo J, Lehtonen L. The effects of skin-to-skin care on the diaphragmatic electrical activity in preterm infants. Early Hum Dev. 2014;90(9):531–4.
Ng E, Schurr P, Reilly M, Dunn M, Beck J. Impact of feeding method on diaphragm electrical activity and central apnea in preterm infants (FEAdi study). Early Hum Dev. 2016;101:33–7.
Acknowledgements
The authors thank the babies and families who participated in the study. The authors also thank all the nursing staff who supported data collection and cared for the infants during the study.
Funding
Internally funded.
Author information
Authors and Affiliations
Contributions
SB conceived the study. SB, VG, TS, JS and KL designed the study. VG coordinated the implementation of the study and was responsible for data acquisition and subsequent analysis. ST drafted the manuscript. All authors (SB, VG, TS, JS, KL and ST) reviewed and revised the manuscript, providing important intellectual content, and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed following the Declaration of Helsinki and approved by the Human Research Ethics Committee of South Eastern Sydney Local Health District (Reference Number: 17/083). All parents or legal guardians provided written informed consent for infants to participate in the study.
Consent for publication
Not applicable.
Competing interests
The specialised nasogastric feeding tubes required for this study were provided at no cost by the manufacturer (Getinge AB, Gothenburg, Sweden). The manufacturer had no involvement in study concept, design, conduct, analyses or manuscript preparation.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gurumahan, V., Thavalingam, S., Schindler, T. et al. Reference values for diaphragm electrical activity (Edi) in newborn infants. BMC Pediatr 22, 559 (2022). https://doi.org/10.1186/s12887-022-03619-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03619-1