Abstract
Background
Myelodysplastic syndrome (MDS) is a rare disease in children and the treatment option before the allogeneic hematopoietic stem cell transplantation (allo-HSCT) is rarely reported. Our main objective was to report our single-center experience with the DNA-hypomethylating agent, decitabine-combined minimally myelosuppressive regimen (DAC + MMR) bridged allo-HSCT in children with MDS.
Methods
Twenty-eight children with de novo MDS who underwent allo-HSCT between 2011 and 2020 were enrolled. Patients were divided into subgroups (refractory cytopenia of childhood [RCC] and advanced MDS [aMDS]) and treated by HSCT alone or pre-transplant combination treatment based on risk stratification. The patients’ clinical characteristics, treatment strategies and outcomes were retrospectively evaluated.
Results
Twenty patients with aMDS had received pre-transplant treatment (three were treated with decitabine alone, thirteen with DAC + MMR, and four with acute myeloid leukemia type [AML-type] induction therapy). DAC + MMR was well tolerated and the most common adverse events were myelosuppression and gastrointestinal reaction. DAC + MMR had shown an improved marrow complete remission (mCR) compared with AML-type chemotherapy (13/13, 100% versus 2/4, 50%, P = 0.044). The median follow-up for total cohort was 53.0 months (range, 2.3-127.0 months) and the 4-year overall survival (OS) was 71.4 ± 8.5%. In the subgroup of aMDS, pretreatment of DAC + MMR resulted in a much better survival rate than AML-type chemotherapy (84.6 ± 10.0% versus 0.0 ± 0.0%, P < 0.001).
Conclusions
The DAC + MMR bridged allo-HSCT may be recommended as a novel and effective approach.
Similar content being viewed by others
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) might be the only curative approach for many children with myelodysplastic syndrome (MDS). It is routinely implemented to patients with advanced MDS (aMDS) (including refractory anemia with excessive blasts [RAEB] and RAEB in transformation [RAEB-t]) or patients with refractory cytopenia of childhood (RCC) accompanied with monosomy 7, complex karyotype, severe neutropenia or transfusion dependenc e[1, 2]. Watch-and-wait strategy or immunosuppression therapy (IST) may be a choice for RCC patients with hypocellular bone marrow (BM) and absence of monosomy 7 and complex karyotype. However, a relevant proportion of those patients still need allo-HSCT subsequently for non-response or relaps e[3]. The recent update of the European Working Group of MDS in childhood (EWOG-MDS) data showed that the survival outcomes of patients transplanted from either a human leukocyte antigen identical (HLA-identical) sibling or an unrelated donor (UD) matched for 9/10 or 10/10 HLA-loci might be almost comparabl e[4]. However, cord blood transplantation (CBT) resulted in survival rates below 30-60 %[5,6,7]. As for haploidentical transplantation, data is far more limited, remaining identified. Interestingly, the 5-year overall survival rate (OS) of HSCT from haploidentical family donors for pediatric patients with MDS was as high as 86% in a recent Korean cohor t[8]. Generally, there is still a paucity of data to inform the best transplant type for pediatric MDS.
As for the pre-transplant period for aMDS, a diversity of therapy strategies like intensive chemotherapy, AML-type induction chemotherapy, minimally myelosuppressive regimen (MMR) and DNA methyltransferase (DNMT) inhibitors has been investigate d[9, 10]. Intensive chemotherapy is not generally recommended due to showing no survival benefi t[11]. The acute myeloid leukemia type (AML-type) induction chemotherapy is controversial because of its somewhat severe toxicity and considerable mortalit y[10, 11]. The debut of low-dose induced remission treatment (low dose of cytarabine and anthracycline in conjunction with granulocyte colony stimulating factor [G-CSF]) was reported in 1995, being applied among aged patients with myeloid tumor and yielding certain efficac y[12]. Then, it has been continuously improved and demonstrated to be efficacious during the past decades mainly among adult MDS/AML population s[13, 14]. Intriguingly, pediatric AML patients receiving MMR (one-tenth of standard dose of cytarabine, one-half dose of anthracycline in conjunction with G-CSF) showed similar outcomes and mutation clearance levels, but significantly lower toxicity compared with those receiving standard chemotherapy in our cente r[15, 16].
Hypermethylation of critical genes was revealed in adult and childhood MDS, considered one of the disease’s driving alteration s[9, 17, 18]. In addition, hypermethylation of the promoters of various genes was associated with unfavorable prognosis in MDS, and the strategy of adopting DNA-hypomethylating agents including azacitidine (AZA) and decitabine (DAC) combination therapy is appealing for MD S[19, 20]. It has been widely recognized that low-dose DNA-hypomethylating agents could improve the quality of life and prolong survival to a significant extent for old people, especially for those unfit for allo-HSCT or intensive chemotherap y[21]. However, the role of DNA-hypomethylating agents in the treatment of childhood MDS is scarc e[22, 23].
Considering the possible advantages of disease control with good tolerability during HSCT preparation, improved antitumoral alloimmunity, reduced risk of relapse, and so on,[24,25,26] we have upheld a scientific hypothesis that decitabine-combined MMR strategy (DAC + MMR) bridged allo-HSCT may be a feasible way for pediatric aMDS patients with low toxicity and high efficiency. Here, we present retrospective data on the 28 children with de novo MDS who underwent allo-HSCT during the past decade in our single center. The clinical features, chemotherapy regimens, transplant characteristics, outcomes, adverse events and complications were investigated and analyzed.
Patients and methods
Patient population
A total of 28 pediatric MDS patients hospitalized and receiving allo-HSCT from January 2011 to December 2020 at our single center were finally enrolled in this study. Both experienced hematologists and pathologists reviewed the diagnosis of all patients. They were newly diagnosed as de novo MDS according to pediatric modification of the World Health Organization (WHO) classification. According to the current recommendations, they were categorized as RCC, RAEB and RAEB-t [27, 28]. Following the proposed categorization by Hasle et al., patients with RCC were termed as low-grade MDS while those with RAEB or with RAEB-t were termed as advanced MDS (aMDS) [29].
The inclusion criteria were as follows: (1) younger than 14 years of age at disease onset; (2) newly diagnosed as de novo MDS; (3) not Down syndrome (DS)-related MDS; (4) receiving allo-HSCT after diagnosis. Patients who developed AML at any time before transplantation were excluded. Cytogenetic analysis of BM cells was performed for all of the patients.
The indications for allo-HSCT among MDS patients were: (1) RCC patients with monosomy 7, 7q deletion or complex karyotype; (2) RCC patients with severe neutropenia or transfusion dependence; (3) aMDS patients.
Ethical statement
This retrospective study was authorized by the local ethical committee of Children’s Hospital of Soochow University. The written informed consents were obtained from the patients’ parents or legal guardians. The study is carried out in accordance with the Declaration of Helsinki.
Chemotherapy
The AML-type induction chemotherapy was similar to the protocol of AML induction remission therapy used in our cente r[15, 16]. The decitabine-combined minimally myelosuppressive regimen (DAC + MMR) included three subtypes of regimens. One subtype was “DAC + MAG”, which contained decitabine (20 mg/m2 once a day intravenously from the first day to the 5th day), cytarabine (10 mg/m2 every 12 hours subcutaneously from the 6th to 15th day), mitoxantrone (5 mg/m2 once a day intravenously for the 6th, 8th and 10th day) and G-CSF (5 μg/m2 once a day subcutaneously from the 6th to 15th day). One was aliased as “DAC + HAG”, which contained decitabine, cytarabine and G-CSF with the same usage as above and homoharringtonine (1 mg/m2 once a day intravenously from the 6th to 12th day). And the third one contained decitabine, cytarabine, and G-CSF with the same usage as above, and idarubicin (5 mg/m2 once a day intravenously from the 6th to 8th day) was abbreviated as “DAC + IDAG”. Additionally, sole decitabine treatment prior to transplantation performed as decitabine at 20 mg/m2 once a day intravenously for five consecutive days was applied for some aMDS patients with BM blasts slightly higher than 5%.
Transplantation
The conditioning regimens included myeloablative conditioning (MAC) and reduced-intensity conditioning (RIC). All the regimens were busulfan and cyclophosphamide based (Bu + Cy) or fludarabine and busulfan based (Flu+Bu). The types of transplantation included HLA-identical transplantation (containing sibling donor allo-HSCT [sib-HSCT] and unrelated matched HSCT), haploidentical transplantation, and cord blood transplantation (CBT). The graft-versus-host disease (GVHD) prophylaxis contained calcineurin inhibitors (cyclosporine A or tacrolimus), mycophenolate mofetil, as well as short-term methotrexate.
Evaluation and criterion
The neutropenia was defined as absolute neutrophil count (ANC) < 1.5*109 /L and severe neutropenia was ANC < 0.5*109 /L. The thrombocytopenia was defined as platelet count (Plt) < 100*109 /L, and severe thrombocytopenia was Plt < 20*109 /L and/or clinical need for platelet transfusion. The response to treatment was assessed by reference to the International Working Group (IWG) response criteria in myelodysplasia [30]. Marrow complete remission (mCR) referred to the achievement of marrow blasts ≤5% with or without improved cytopenias. Adverse events of administered treatments were graded by using the common terminology criteria of adverse events score (CTCAE) (version 4.0). Graft failure (the primary) was defined as ANC that did not maintain sustained engraftment (> 0.5*109 /L) within 28 days post-transplantation. The granulocyte engraftment was defined as ANC ≥0.5*109/L for three consecutive days. The platelet engraftment was defined as Plt ≥20*109/L for seven consecutive days without platelet transfusion support. The acute and chronic graft-versus-host disease (GVHD) were graded based on traditional criteria [31, 32].
Follow-up
All the patients were followed up every month and the follow-up endpoint was August 31, 2021. The overall survival time (OS) was calculated from the date of first diagnosis to the date of death or last follow-up. The events included death, relapse, graft failure, severe complications (acute renal failure, for instance) and secondary tumor (progression to AML, for instance) and the event-free survival time (EFS) was defined as survival without those events. Relapse was defined as morphological evidence of disease in BM or recurrence and sustained pre-transplant chromosomal abnormalities. The relapse-free survival (RFS) time was calculated.
Statistical analysis
The continuous variables with normal distribution were expressed as mean and standard deviation, while variables with skewed distribution were expressed as median and range. The categorical variables were described as number and percentage. The independent-samples T test was used to assess normal distributional variables. The Mann-Whitney U test and Kruskal-Wallis H test were used to assess skewed distributional variables, as appropriate. The categorical variables were analyzed using Chi square or Fisher’s Exact Test, as appropriate. The Kaplan-Meier methods were used to describe survival functions and the log-rank test was used to compare the survival curves. A Cox’s proportional hazards regression model was used to determine the significance of risk factors for the outcomes. Factors with at least P-value< 0.10 in the univariate analysis were included in the model. Hazard ratios (HR) and 95% confidence intervals (CI) were calculated. SPSS 26.0 software was employed for data processing. GraphPad Prism 8.0.2 software was served as the tool for results visualization. Two-tailed P-values< 0.05 were considered statistically significant.
Results
Patients’ general features
From 2011 to 2020, 28 children with de novo MDS receiving HSCT met inclusion criteria. The general features of the 28 patients were shown in Table 1. The median age at diagnosis was 79.5 months (range, 19-138 months). Diagnosis were low-grade MDS (RCC, n = 7) and aMDS (RAEB, n = 15 and RAEB-t, n = 6). At diagnosis, 89.3% (25/28) of patients had cytopenia involving at least two lineages and 32.1% (9/28) had severe neutropenia (Table 2). The chromosome abnormalities accounted for 35.7% (10/28), and mainly were monosomy 7 (n = 6), trisomy 8 (n = 2), complex karyotype (n = 1), and + 1, der (1;12)(q10;q10) (n = 1) (Table 2). Of the 21 aMDS patients, 20 patients were treated pre-HSCT, while only one patient went directly to HSCT (patient 11, Table 2). Among treated patients, 65.0% (13/20) received DAC + MMR, 15.0% (3/20) had sole decitabine, and 20.0% (4/20) accepted AML-type chemotherapy. The median age at HSCT was 81.5 months (range, 21-152 months). The majority of patients underwent myeloablative conditioning (23/28, 82.1%). Transplantation was performed between 2011 and 2015 in 11 (11/28, 39.3%) patients and between 2016 and 2020 in 17 (17/28, 60.7%) patients. Transplant types were HLA-identical HSCT in 7 cases, haploidentical HSCT in 18 cases and CBT in 3 cases. Until August 31, 2021, none of the patients lost follow-up and none of the survivals relapsed.
Response to chemotherapy
The pre-transplant treatments and responses of each patient were summarized in Table 2. During the pre-transplant period, different strategies were applied to the patients according to the attending’s decision and patient’s agreement.
Three aMDS patients with BM blasts slightly higher than 5% were treated with sole decitabine prior to transplantation. One patient received two cycles of decitabine and achieved mCR. One patient achieved mCR after one cycle of decitabine. The rest one patient was a 3-years old girl at diagnosis, and traditional Chinese medicine was taken without medical advice since December 2011 (patient 20, Table 2). One cycle of decitabine and subsequent allo-HSCT were performed in 2015, and she had achieved mCR before transplantation. Thirteen aMDS patients (seven were RAEB and six were RAEB-t) received DAC + MMR and a total of 23 cycles of DAC + MMR were administered. All of them achieved mCR before transplantation. Two of the four patients who received AML-type induction therapy achieved mCR, while the other two gained 6.0 and 8.5% of BM blasts before transplantation (Table 2). Eight patients (including seven RCC patients and one aMDS patient [patient 11, Table 2]) proceed to transplantation directly.
Adverse events on decitabine concomitant chemotherapy
A total of 27 cycles of decitabine were administered among the 16 patients, of which, 4 cycles were sole decitabine therapy for three patients and 23 cycles were decitabine-combined MMR for 13 patients.
The most common hematologic toxicity was myelosuppression. At the beginning of decitabine-concomitant treatment, 12 of 16 patients (75.0%) had neutropenia, and 5 of the 16 patients (31.3%) had severe neutropenia. During the decitabine-concomitant therapy, four patients with previously normal ANC developed neutropenia (n = 2) or severe neutropenia (n = 2), and five patients with initial neutropenia worsen to severe neutropenia. 14 of the 27 cycles (51.9%) involved neutropenia, and 13 of the 27 cycles (48.1%) involved severe neutropenia. Twelve patients had severe thrombocytopenia during the treatment, involving 13 of the 27 cycles (48.1%). The non-hematologic toxicities were mainly mild and the most common complications were gastrointestinal problems and infection. Nine episodes of infection were observed in eight patients and eight of the nine episodes occurred in severe neutropenia. There was no delay or reduction during the sole decitabine therapy for the three patients. As for decitabine-combined MMR therapy, treatment was delayed in two cycles. Vomiting (CTCAE grade 3) and gastritis led to prolonged treatment after one cycle of “DAC + IDAG” in one patient (patient 14, Table 2). Acute pancreatitis led to treatment discontinuation after two cycles of “DAC + MAG” in one patient (patient 1, Table 2).
Allogeneic hematopoietic stem cell transplantation
All the 28 MDS patients enrolled in the present study proceeded to allo-HSCT, and depending on the transplant types, they were divided into three groups (HLA-identical HSCT treated group [n = 7], haploidentical HSCT treated group [n = 18] and CBT treated group [n = 3]). There were no statistical differences in the age at transplantation, time interval from diagnosis to transplantation, gender distribution, gender and blood type of donor and recipient compatibility, conditioning regimen among the three groups (Table 3). Compared with patients with haploidentical HSCT, patients with HLA-identical HSCT accessed younger donors (P < 0.001) (Table 3). Patients with CBT were transfused significantly fewer mononuclear cells and CD34+ cells when compared with patients in other two groups (both P = 0.023) (Table 3). There were 7 (7/7, 100%), 18 (18/18, 100%) and 1 (1/3, 33.3%) patients who were successfully engrafted in granulocyte among HLA-identical HSCT group, haploidentical HSCT group and CBT group, respectively. The median time for granulocytic engraftment were 13.0 (11.0-20.0), 14.0 (10.0-18.0), and 19.0 (19.0-19.0) days, respectively. There were 7 (7/7, 100%), 17 (17/18, 94.4%) and 1 (1/3, 33.3%) patients reached platelet engraftment among the three groups and the median time were 14.0 (11.0-40.0), 15.0 (9.0-66.0) and 22.0 (22.0-22.0) days, respectively. There were no statistical differences in the incidence of the main complications (aGVHD, cGVHD, cytomegalovirus infection, Epstein-Barr virus infection, other infections, bronchiolitis obliterans, and so on) (Table 3).
Survival and main complications
The median follow-up within the whole cohort was 53.0 months (range, 2.3-127.0 months), while the median follow-up of the survivors (n = 20) was 63.7 months (range, 23.1-127.0 months). By August 31, 2021, 20 patients (20/28, 71.4%) were alive without evidence of MDS (Table 2). The causes of death of 8 patients were reviewed and listed in Table 2. Four patients died of severe aGVHD. Two patients died of severe lung infection. One patient with CBT presented with graft failure and died 2 months after transplantation due to disease progression. One with CBT suffered sudden cardiac death on day one after transplantation.
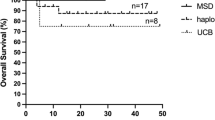
The 4-year OS rate for the total cohort was 71.4 ± 8.5%, while that for patients with RCC and those with aMDS was 85.7 ± 13.2% and 66.7 ± 10.3%, respectively (Fig. 1a). Patients with abnormal karyotypes at diagnosis had significantly low survival rate when comparing with patients whose karyotypes at diagnosis were normal (50.0 ± 15.8% versus 83.3 ± 8.8%, P = 0.048) (Fig. 1b). Compared with transplantation from HLA-identical (matched sibling or unrelated) donors for 9/10 or 10/10 HLA-loci (4-year OS, 100.0 ± 0.0%), the outcomes of haploidentical HSCT were also satisfactory with an estimated 4-year OS of 72.2 ± 10.6%, while the three patients with CBT showed a dismal survival (0.0 ± 0.0%) (Fig. 1c).
The overall survival of the whole 28 de novo MDS patients with allo-HSCT. a The overall survival of RCC patients (n = 7) compared with aMDS patients (n = 21). b The overall survival of patients with normal karyotype (n = 18) compared with those with abnormal karyotypes (n = 10). c The overall survival of patients with different transplant types. MDS: myelodysplastic syndrome; allo-HSCT: allogeneic hematopoietic stem cell transplantation; RCC: refractory cytopenia of childhood; aMDS: advanced myelodysplastic syndrome
Based on the different bridging treatment strategies, the 21 aMDS patients were further analyzed (Fig. 2). One aMDS patient with 6% BM blasts underwent HSCT directly and has been alive without MDS. With respect to the 20 aMDS patients with pretreatment, the rate of the subgroup of the 13 patients treated with DAC + MMR was as high as 84.6 ± 10.0%. The three patients with DAC alone came out an estimate 4-year OS of 66.7 ± 27.2%. At the same time, all of the four patients treated with AML-type induction therapy followed by HSCT died soon after transplantation (Fig. 2a). Among the 13 aMDS patients with haploidentical HSCT, five patients died, and four of the five ones died of severe aGVHD, and it finally showed a 4-year OS of 61.5 ± 13.5% (Fig. 2b).
The overall survival of the subgroup of the 21 aMDS patients with allo-HSCT. a The overall survival of aMDS patients with different bridging treatment strategies. b The overall survival of aMDS patients with different transplant types. aMDS: advanced myelodysplastic syndrome; allo-HSCT: allogeneic hematopoietic stem cell transplantation
In addition, potential risk factors including gender, age at diagnosis, cytogenetics at diagnosis, age at transplantation, time interval from diagnosis to transplantation, percentage of BM blasts at diagnosis or before transplantation, conditioning regimen, transplant type, transplantation period and acute/chronic GVHD were analyzed. The factors with P < 0.10 (the factors included cytogenetics at diagnosis [P = 0.066], percentage of BM blasts at transplantation [P = 0.024], transplant type [P = 0.001] and acute GVHD [P = 0.001] for the whole MDS cohort, while the factors were percentage of BM blasts at transplantation [P = 0.028], transplant type [P = 0.013] and acute GVHD [P = 0.005] for the aMDS patients) in univariate analysis were further taken into the multivariate analysis (Tables 4 and 5). Finally, CBT (HR = 49.272, 95% CI 2.868-846.433, P = 0.007 for the whole cohort, HR = 7.973, 95% CI 1.180-53.882, P = 0.033 for the subgroup of aMDS patients) and grade III-IV of aGVHD (HR = 64.283, 95% CI 4.605-897.352, P = 0.002 for the whole cohort, HR = 14.757, 95% CI 1.556-139.928, P = 0.019 for the subgroup of aMDS patients) were demonstrated to be the independent prognostic factors for OS (Table 5).
Discussion
Here, we reported a cohort of children with MDS who underwent allo-HSCT over the past decade at our single center. To the best of our knowledge, this may be the latest research in China for systematically reviewing a certain size of cohort regarding pediatric MDS with transplantation and is also the first domestic study in China that reported the experience of decitabine-combined minimally myelosuppressive regimen prior to allo-HSCT for pediatric aMDS.
Pediatric MDS is a heterogeneous group of clonal disorder accounting for less than 5% of childhood hematological malignancies. The morphology, cytogenetics and therapy approaches would profoundly influence the survival outcome s[33]. It is recognized that patients with abnormal karyotype such as monosomy 7 or complex karyotype are more likely to progress to advanced disease and have poor outcome s[34, 35]. In the present study, ten patients with abnormal karyotypes had a significant low survival rate compared to 18 patients whose karyotypes were normal. However, the cytogenetic data is far more limited with great heterogeneity which should be carefully interpreted. Recently, with the increased access to gene mutation landscape, genetic counseling for both patients and their families would affect pediatric MDS’s clinical diagnosis and therapeutic decision s[36,37,38]. The gene mutation assay was performed among the 16 patients of this cohort and 14 of them were verified to carry different gene mutations (Supplementary Table 1). It will be a great challenge for pediatric hematologists further to explore the underlying conditions and their hematopoietic impacts.
As for treatment strategy, it is widely accepted that allogeneic HSCT is the only curative treatment for pediatric MD S[5, 39]. Especially, high-risk subtype of MDS is recommended to receive an early transplantation. Allo-HSCT for pediatric MDS has been adeptly mastered during the past decade in our center. The 4-year OS as high as 71.4 ± 8.5% for the total cohort, 85.7 ± 13.2% and 66.7 ± 10.3% for low-grade and advanced MDS respectively are revealed in our study, consistent with that of recent reports ranging from 30 to 80 %[1, 5, 40, 41]. It is reported that allo-HSCT from a matched related or unrelated donor offers a superior survival probability for pediatric MD S[4]. The data of the seven patients with HLA-identical transplantation in our center confirmed this conclusion again. Our preliminary data showed that the 4-year OS of haploidentical HSCT was 72.2 ± 10.6%, which indicated that haploidentical HSCT would be a feasible alternative among childhood MDS for an urgent need of transplantation. Consistently, a Korean group reviewed 36 pediatric patients with MDS who proceeded to haploidentical HSCT (n = 9) or HLA-identical HSCT (n = 24) or CBT (n = 3 )[8]. Intriguingly, the OS of HSCT from haploidentical family donors was comparable with that from HLA-identical donors (86% versus 79%, P = 0.625 )[8]. With the theoretic advantages, including low incidence of acute and chronic GVHD, despite multiple HLA mismatching and so on, cord blood has been considered as an attractive source for transplantatio n[42, 43]. However, in our center, all the three patients with CBT in the cohort died soon after transplantation, leading to no obvious benefit regarding overall survival. In the future, more data of CBT will be needed to draw certain conclusions. The cumulative incidence of transplantation-related mortality (TRM) for the total cohort was 28.6 ± 8.5%. Acute GVHD is a serious transplant complication that contributes TRM after allo-HSC T[43]. In the risk factor analysis for OS, grade III-IV aGVHD was associated with higher risk of mortality and should be prevented.
It is challenging and time-consuming for donor searching and HSCT preparation. Therefore, the disease should be controlled through a bridging treatment based on risk stratification. What has been reached as a common consensus is that conventional chemotherapy is dubious, especially for high-risk MDS. The advent of epigenetic treatment options for myeloid disorders has led to the combination concepts, and their integration with transplantation already shows a reliably improved outcome in adult MD S[24, 44]. However, the experience among pediatric MDS is far more limited with anecdotal report s[22, 45]. In our study, an excellent response rate of 100% (100.0% achieved mCR) was observed using decitabine-combined MMR with a median of two cycles (range, 1-3) for pediatric advanced MDS. At the same time, three patients with RAEB achieved mCR after one or two cycles of sole decitabine. More encouragingly, the strategy of low-dose decitabine-combined-MMR use proved to be very tolerable with mild non-hematologic toxicity in the pediatric population. Considering the heterogeneity of MDS and unevenly distributed subgroups, patients with advanced MDS were further extracted and analyzed to better illustrate the effect of decitabine-combined therapy bridged allo-HSCT. As a result, 13 patients with DAC + MMR treatment showed a quite inspiring survival (84.6 ± 10.0%), and none of the 11 survivals relapsed at last follow-up. DAC + MMR appears to be a promising bridge to HSCT with its high efficiency of eliminating the excess BM blasts with low toxicity. These exciting results provided a valuable clinical experience for the use of decitabine in the pediatric population.
Preemptive treatment for the minimal residual disease (MRD) is essential for preventing or substantially delaying hematological relapse after HSCT in pediatric MDS, especially in high-risk subgroups. The discovery of genome-wide DNA hypermethylation in pediatric MDS provides a rationale for DNMT inhibitors applicatio n[9, 17]. Low-dose decitabine could directly and irreversibly inhibit the DNA methyltransferases. More intriguing potential of decitabine among antitumoral alloimmunity and pro-apoptotic effect of tumor cells has emerged in recent year s[24,25,26, 45]. The MMR is originated from the low-dose chemotherapy consisting of low-dose cytarabine and aclarubicin combined with G-CSF, abbreviated as “CAG”, proposed in 1995. The CAG regimen achieved certain efficacy in refractory/relapse adult MDS and AM L[12]. Even in low/intermediate risk adult MDS and AML, the CR rates of low-dose induction therapy were significantly higher than intensive chemotherap y[46]. However, the cardiac toxicity associated with aclarubicin mainly limited to a certain extent of the application of CAG regimen. Then, alternatives with similar therapeutic effect and mild cardiac toxicity were developed, forming different regimens of MMR. The advantages of MMR may be due to the synergy of G-CSF and low-dose chemotherapy drugs. G-CSF priming could preferentially potentiate Ara-C and anthracycline-mediated cytotoxicity on myeloid tumor cells, presumably by enhancing G0 resting tumor cells into the cell cycl e[47]. In addition, the G-CSF combination may inhibit the self-renewal capacity of myeloid tumor cells and leukemia stem cell s[48, 49]. It will be of great interest to investigate the underline specific mechanisms in the future. Hence, the combinatorial approach of decitabine, low dose chemotherapy drugs and G-CSF is reasonable and might be an effective strategy for pediatric MDS before transplantation.
Several limitations about our study should be considered. Firstly, the fundamental limitation is that this analysis did not include patients who received chemotherapy and/or DNA-hypomethylating therapy and did not progress to transplantation. The excellent overall responses to decitabine-concomitant treatment may not be accurately attainable for each individual among the heterogeneous MDS population. Secondly, details including chemotherapy regimens, donor types and conditioning regimens vary widely, and the robustness of the results may be impaired. Thirdly, this cohort included 28 patients with a median follow-up of 53.0 months, which is not adequate enough and may lead to a considerable bias. Finally, our analysis has the intrinsic limitation related to the retrospective nature and comparison with limited historical controls. In 2018, we had registered a multicenter study of DAC + MMR for children with MDS or AML (ChiCTR1800015872) and we are struggling for large confirmatory and prospective studies to help us to clarify whether this approach can alter the natural history of the disease. Therefore, the results in the present study must be interpreted with caution and further evidence from future prospective studies is required.
In summary, our cohort shows that probably, about 71% of the children with MDS would achieve prolonged survival with allo-HSCT. Abnormal karyotype at diagnosis, high BM blast cell percentage before transplantation and severe aGVHD may indicate undesirable outcomes. CBT is not preferred, while haploidentical HSCT might be a feasible alternative when HLA-identical HSCT is unavailable. The bridging therapy of DAC + MMR was safe and well tolerated. It appears to be more effective than AML-type chemotherapy with higher mCR rate and better survival rate in childhood MDS. Our study may provide a novel and practical bridging approach for pediatric MDS with subsequent allo-HSCT. Due to the lack of randomized controlled trials, further prospective randomized study to explicitly determine the safety and efficacy of this approach in comparison with no decitabine (AML-type chemotherapy-combined HSCT or HSCT only) are required.
Availability of data and materials
The datasets used and analyzed during the current study available from the corresponding author on reasonable request.
References
Locatelli F, Strahm B. How I treat myelodysplastic syndromes of childhood. Blood. 2018;131(13):1406–14.
Galaverna F, Ruggeri A, Locatelli F. Myelodysplastic syndromes in children. Curr Opin Oncol. 2018;30(6):402–8.
Hasegawa D. The current perspective of low-grade myelodysplastic syndrome in children. Int J Hematol. 2016;103(4):360–4.
Strahm B, Nöllke P, Zecca M, et al. Hematopoietic stem cell transplantation for advanced myelodysplastic syndrome in children: results of the EWOG-MDS 98 study. Leukemia. 2011;25(3):455–62.
Basquiera AL, Pizzi S, Correas AG, et al. Allogeneic hematopoietic stem cell transplantation in pediatric myelodysplastic syndromes: a multicenter experience from Argentina. Pediatr Blood Cancer. 2015;62(1):153–7.
Parikh SH, Mendizabal A, Martin PL, et al. Unrelated donor umbilical cord blood transplantation in pediatric myelodysplastic syndrome: a single-center experience. Biol Blood Marrow Transplant. 2009;15(8):948–55.
Tavares R, Bonfim CS, Seber A, et al. Hematopoietic cell transplantation in pediatric patients with acute leukemias or myelodysplastic syndrome using unrelated adult or umbilical cord blood donors in Brazil. Pediatr Transplant. 2020;24(7):e13789.
Yoo JW, Im HJ, Kim H, et al. Improved outcomes of allogeneic hematopoietic stem cell transplantation including haploidentical transplantation for childhood myelodysplastic syndrome. Bone Marrow Transplant. 2020;55(8):1595–603.
Lamim Lovatel V, de Souza FC, Ferreira Rodrigues E, et al. Expression profiles of DNA methylation and demethylation machinery components in pediatric myelodysplastic syndrome: clinical implications. Cancer Manag Res. 2020;12:543–56.
Duarte FB, Moura A, Funke V, et al. Impact of treatment prior to allogeneic transplantation of hematopoietic stem cells in patients with myelodysplastic syndrome: results of the Latin American bone marrow transplant registry. Biol Blood Marrow Transplant. 2020;26(5):1021–4.
Hasle H, Niemeyer CM. Advances in the prognostication and management of advanced MDS in children. Br J Haematol. 2011;154(2):185–95.
Yamada K, Furusawa S, Saito K, et al. Concurrent use of granulocyte colony-stimulating factor with low-dose cytosine arabinoside and aclarubicin for previously treated acute myelogenous leukemia: a pilot study. Leukemia. 1995;9(1):10–4.
Xiu C, Li X, Wu L, et al. The efficacy and toxicity of the CHG priming regimen (low-dose cytarabine, homoharringtonine, and G-CSF) in higher risk MDS patients relapsed or refractory to decitabine. J Cancer Res Clin Oncol. 2019;145(12):3089–97.
Saito K, Nakamura Y, Aoyagi M, et al. Low-dose cytarabine and aclarubicin in combination with granulocyte colony-stimulating factor (CAG regimen) for previously treated patients with relapsed or primary resistant acute myelogenous leukemia (AML) and previously untreated elderly patients with AML, secondary AML, and refractory anemia with excess blasts in transformation. Int J Hematol. 2000;71(3):238–44.
Hu Y, Chen A, Zheng X, et al. Ecological principle meets cancer treatment: treating children with acute myeloid leukemia with low-dose chemotherapy. Natl Sci Rev. 2019;6(3):469–79.
Hu Y, Chen A, Gao L, et al. Minimally myelosuppressive regimen for remission induction in pediatric AML: long-term results of an observational study. Blood Adv. 2021;5(7):1837–47.
Hasegawa D, Manabe A, Kubota T, et al. Methylation status of the p15 and p16 genes in paediatric myelodysplastic syndrome and juvenile myelomonocytic leukaemia. Br J Haematol. 2005;128(6):805–12.
Vidal DO, Paixão VA, Brait M, et al. Aberrant methylation in pediatric myelodysplastic syndrome. Leuk Res. 2007;31(2):175–81.
Flotho C, Sommer S, Lübbert M. DNA-hypomethylating agents as epigenetic therapy before and after allogeneic hematopoietic stem cell transplantation in myelodysplastic syndromes and juvenile myelomonocytic leukemia. Semin Cancer Biol. 2018;51:68–79.
Du M, Zhou F, Jin R, Hu Y, Mei H. Mutations in the DNA methylation pathway predict clinical efficacy to hypomethylating agents in myelodysplastic syndromes: a meta-analysis. Leuk Res. 2019;80:11–8.
Jabbour E, Short NJ, Montalban-Bravo G, et al. Randomized phase 2 study of low-dose decitabine vs low-dose azacitidine in lower-risk MDS and MDS/MPN. Blood. 2017;130(13):1514–22.
Waespe N, Van Den Akker M, Klaassen RJ, et al. Response to treatment with azacitidine in children with advanced myelodysplastic syndrome prior to hematopoietic stem cell transplantation. Haematologica. 2016;101(12):1508–15.
Cseh AM, Niemeyer CM, Yoshimi A, et al. Therapy with low-dose azacitidine for MDS in children and young adults: a retrospective analysis of the EWOG-MDS study group. Br J Haematol. 2016;172(6):930–6.
Qin T, Youssef EM, Jelinek J, et al. Effect of cytarabine and decitabine in combination in human leukemic cell lines. Clin Cancer Res. 2007;13(14):4225–32.
Qiu YY, Mirkin BL, Dwivedi RS. Inhibition of DNA methyltransferase reverses cisplatin induced drug resistance in murine neuroblastoma cells. Cancer Detect Prev. 2005;29(5):456–63.
Roolf C, Richter A, Konkolefski C, et al. Decitabine demonstrates antileukemic activity in B cell precursor acute lymphoblastic leukemia with MLL rearrangements. J Hematol Oncol. 2018;11(1):62.
Hasle H, Niemeyer CM, Chessells JM, et al. A pediatric approach to the WHO classification of myelodysplastic and myeloproliferative diseases. Leukemia. 2003;17(2):277–82.
Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405.
Hasle H. Myelodysplastic and myeloproliferative disorders of childhood. Hematology Am Soc Hematol Educ Program. 2016;2016(1):598–604.
Cheson BD, Greenberg PL, Bennett JM, et al. Clinical application and proposal for modification of the international working group (IWG) response criteria in myelodysplasia. Blood. 2006;108(2):419–25.
Schoemans HM, Lee SJ, Ferrara JL, et al. EBMT-NIH-CIBMTR task force position statement on standardized terminology & guidance for graft-versus-host disease assessment. Bone Marrow Transplant. 2018;53(11):1401–15.
Shulman HM, Cardona DM, Greenson JK, et al. NIH Consensus development project on criteria for clinical trials in chronic graft-versus-host disease: II. The 2014 Pathology working group report. Biol Blood Marrow Transplant. 2015;21(4):589–603.
Hamilton BK, Rybicki L, Hirsch C, et al. Mutation clonal burden and allogeneic hematopoietic cell transplantation outcomes in acute myeloid leukemia and myelodysplastic syndromes. Bone Marrow Transplant. 2019;54(8):1281–6.
Kardos G, Baumann I, Passmore SJ, et al. Refractory anemia in childhood: a retrospective analysis of 67 patients with particular reference to monosomy 7. Blood. 2003;102(6):1997–2003.
Moriwaki K, Manabe A, Taketani T, Kikuchi A, Nakahata T, Hayashi Y. Cytogenetics and clinical features of pediatric myelodysplastic syndrome in Japan. Int J Hematol. 2014;100(5):478–84.
Schratz KE, DeZern AE. Genetic predisposition to myelodysplastic syndrome in clinical practice. Hematol Oncol Clin North Am. 2020;34(2):333–56.
Drusbosky LM, Singh NK, Hawkins KE, et al. A genomics-informed computational biology platform prospectively predicts treatment responses in AML and MDS patients. Blood Adv. 2019;3(12):1837–47.
Ahmed IA, Farooqi MS, Vander Lugt MT, et al. Outcomes of hematopoietic cell transplantation in patients with germline SAMD9/SAMD9L mutations. Biol Blood Marrow Transplant. 2019;25(11):2186–96.
Andolina JR, Kletzel M, Tse WT, et al. Allogeneic hematopoetic stem cell transplantation in pediatric myelodysplastic syndromes: improved outcomes for de novo disease. Pediatr Transplant. 2011;15(3):334–43.
Strahm B, Locatelli F, Bader P, et al. Reduced intensity conditioning in unrelated donor transplantation for refractory cytopenia in childhood. Bone Marrow Transplant. 2007;40(4):329–33.
Inagaki J, Fukano R, Kurauchi K, Noguchi M, Tanioka S, Okamura J. Hematopoietic stem cell transplantation in children with refractory cytopenia of childhood: single-center experience using high-dose cytarabine containing myeloablative and aplastic anemia oriented reduced-intensity conditioning regimens. Biol Blood Marrow Transplant. 2015;21(3):565–9.
Benadiba J, Ansari M, Krajinovic M, et al. Pharmacokinetics-adapted Busulfan-based myeloablative conditioning before unrelated umbilical cord blood transplantation for myeloid malignancies in children. Plos One. 2018;13(4):e0193862.
Kanda J, Umeda K, Kato K, et al. Effect of graft-versus-host disease on outcomes after pediatric single cord blood transplantation. Bone Marrow Transplant. 2020;55(7):1430–7.
Gore SD, Fenaux P, Santini V, et al. A multivariate analysis of the relationship between response and survival among patients with higher-risk myelodysplastic syndromes treated within azacitidine or conventional care regimens in the randomized AZA-001 trial. Haematologica. 2013;98(7):1067–72.
Glasser CL, Lee A, Eslin D, Marks L, Modak S, Glade Bender JL. Epigenetic combination therapy for children with secondary myelodysplastic syndrome (MDS)/acute myeloid leukemia (AML) and concurrent solid tumor relapse. J Pediatr Hematol Oncol. 2017;39(7):560–4.
Wei G, Ni W, Chiao JW, Cai Z, Huang H, Liu D. A meta-analysis of CAG (cytarabine, aclarubicin, G-CSF) regimen for the treatment of 1029 patients with acute myeloid leukemia and myelodysplastic syndrome. J Hematol Oncol. 2011;4:46.
Anzai H, Frost P, Abbruzzese JL. Synergistic cytotoxicity with 2′-deoxy-5-azacytidine and topotecan in vitro and in vivo. Cancer Res. 1992;52(8):2180–5.
Beekman R, Touw IP. G-CSF and its receptor in myeloid malignancy. Blood. 2010;115(25):5131–6.
Chen J, Yang N, Liu H, et al. Immunological effects of a low-dose cytarabine, aclarubicin and granulocyte-colony stimulating factor priming regimen on a mouse leukemia model. Oncol Lett. 2018;16(3):3022–8.
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (NSFC) (No. 81770193, 81970163, 81800185), Jiangsu project (CXTDA2017014, BE2019672), Suzhou project (SS201809, GSWS2020039), and National Clinical Research Center for Hematological Disorders (2020ZKPB02).
Funding
This work was supported by grants from the National Natural Science Foundation of China (NSFC) (No. 81770193, 81970163, 81800185), Jiangsu project (CXTDA2017014, BE2019672), Suzhou project (SS201809, GSWS2020039), and National Clinical Research Center for Hematological Disorders (2020ZKPB02).
Author information
Authors and Affiliations
Contributions
H.S.Y. designed the study; G.J.Y. H.Y.X and G.L. collected clinical data and analyzed the data; X.P.F. and L.J. provided advice on data collection and analysis; G.J.Y. wrote the manuscript. All authors reviewed and approved the submited manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study was authorized by the local ethical committee of Children’s Hospital of Soochow University. The written informed consents were obtained from the patients’ parents or legal guardians. The study is carried out in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
Junyan Gao, Yixin Hu, Li Gao, Peifang Xiao, Jun Lu and Shaoyan Hu declare no financial ties and no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
The gene mutation data for the 28 children with de novo MDS.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gao, J., Hu, Y., Gao, L. et al. The effect of decitabine-combined minimally myelosuppressive regimen bridged allo-HSCT on the outcomes of pediatric MDS from 10 years’ experience of a single center. BMC Pediatr 22, 312 (2022). https://doi.org/10.1186/s12887-022-03376-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03376-1