Abstract
Background
Hirschsprung disease (HSCR) is a complex genetic disorder characterized by the lack of ganglion cells in the intestines. A current study showed that the NRG1 rare variant frequency in Indonesian patients with HSCR is only 0.9%. Here, we investigated the impact of NRG1 expressions and methylation patterns on the pathogenesis of HSCR.
Methods
This cross-sectional study determined NRG1 type I (HRGα, HRGβ1, HRGβ2, HRGβ3, HRGγ, and NDF43 isoforms), type II and type III expressions in both ganglionic and aganglionic colons of 20 patients with HSCR and 10 control colons by real-time polymerase chain reaction (qPCR). For methylation studies, we treated the extracted gDNA from 16 HSCR patients’ and 17 control colons with sodium bisulfate and analyzed the methylation pattern of NRG1 exon 1 with methylation-specific PCR. The samples were collected and analyzed at our institution from December 2018 to December 2020.
Results
NRG1 types I, II and III expressions were upregulated (17.2-, 3.2-, and 7.2-fold, respectively) in the ganglionic colons compared with control colons (type I: 13.32 ± 1.65 vs. 17.42 ± 1.51, p < 0.01; type II: 13.73 ± 2.02 vs. 16.29 ± 2.19, p < 0.01; type III: 13.47 ± 3.01 vs. 16.32 ± 2.58, p = 0.03; respectively); while only type I (7.7-fold) and HRGβ1/HRGβ2 (3.3-fold) isoforms were significantly upregulated in the aganglionic colons compared to the controls (type I: 14.47 ± 1.66 vs. 17.42 ± 1.51, p < 0.01; HRGβ1/HRGβ2: 13.62 ± 3.42 vs 14.75 ± 1.26, p = 0.01). Moreover, the frequency of partially methylated NRG1 was higher in the ganglionic (81%) and aganglionic (75%) colons than in the controls (59%).
Conclusions
Our study provides further insights into the aberrant NRG1 expression in the colons of patients with HSCR, both ganglionic and aganglionic bowel, which might contribute to the development of HSCR, particularly in Indonesia. Furthermore, these aberrant NRG1 expressions might be associated with its methylation pattern.
Similar content being viewed by others
Background
Hirschsprung disease (HSCR) is a heterogeneous genetic disorder characterized by the absence of ganglion cells in the gastrointestinal tract, causing a functional obstruction. The most common classifications are short-segment HSCR, long-segment HSCR, and total colon aganglionosis [1, 2]. The incidence of HSCR in Indonesia is higher (3.1 cases per 10,000 live births) [3] than other populations (vs. 1.5, 2.1, and 2.8 cases per 10,000 live births in European, African, and Asian ancestry cases, respectively) [1, 2]. This difference might be caused by the genetic background of Indonesians, particularly the RET rs2435357 and rs2506030 risk alleles [4].
NRG1 has been successfully established as a gene candidate for HSCR disease [5]. This genome-wide association study result can be confirmed with the NRG1 variants in patients with HSCR from European and Chinese populations [6, 7], where those mutations downregulate the protein level of NRG1 and cause HSCR disease. However, a current study showed that NRG1 rare variant frequency in Indonesian patients with HSCR is only 0.9% [8].
Moreover, expressions of genes involved in HSCR are influenced by epigenetic mechanisms, including methylation patterns [9,10,11]. NRG1 hypermethylation has been associated with the downregulated NRG1 expressions [12]. In contrast, one study showed that NRG1 expression was not affected by the methylation status [13]. Moreover, while one study showed the aberrant NRG1 expression in patients with HSCR compared to controls [13], Tang et al. [14] revealed no differences in overall NRG1 expressions between patients with HSCR and controls. These conflicting results concerning the role of NRG1 expressions and methylation level on HSCR pathogenesis emphasize the need for confirmation in other populations, mainly Indonesian.
Methods
Patients
This cross-sectional study involved all patients diagnosed with HSCR with the age of < 18 years old, except those who had low quality of DNA or RNA. The samples of ganglionic and aganglionic colons of patients with HSCR were collected at definitive surgery, while the control colon samples were obtained at stoma closure from patients with anorectal malformation. The samples were collected and analyzed at our institution from December 2018 to December 2020.
The HSCR patients' and controls' parents signed a written informed consent form to be included in this study. The Medical and Health Research Ethics Committee of Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada/Dr. Sardjito Hospital gave approval for this study (KE/FK/0111/EC/2020 and KE/FK/0880/2018).
Total RNA isolation and quantitative real-time polymerase chain reaction (qPCR)
We extracted the total RNA from colons of 20 patients with HSCR and 10 controls according to our previous study [15], followed by a qPCR to determine the NRG1 expressions using all of the isoform’s primer sets from a previous study [6].
DNA isolation, bisulfite conversion, and methylation-specific PCR
The QIAamp DNA Mini Kit (QIAGEN, Valencia, CA) was used to extract the total DNA from 16 HSCR patients and 17 control colons. Subsequently, the total DNA was determined using a NanoDrop 2000 Spectrophotometer (Thermo Scientific, Wilmington, DE, USA). Only high-quality DNAs with the OD260/280 ratios of 1.8 to 2.0 were utilized for the subsequent experiment.
DNA genomic (500 ng) was treated with sodium bisulfite using EZ DNA Gold Methylation Kit (ZYMO, USA), then continued with PCR. NRG1 exon 1 methylation was analyzed using the following primers as follows: methylated forward: 5’-GTTTTAGCGCGGTCGTTC-3’, methylated reverse: 5’-CGAACTCCGACTTCTTACCG-3’; unmethylated forward 5’-GTAGTGTGAGTGTTTTAGTGTGGTTG-3, unmethylated reverse: 5’CAAACTCCAACTTCTTACCA-3’. PCR products were then run on gel agarose 2% using fluorosafe. Positive methylation DNA controls used methylated samples with SssI methyltransferase (New England Biolabs, MA, USA) for the methylation-specific PCR (MS-PCR) [13].
Statistics
The Livak (2−ΔΔCT) method was used to compare the NRG1 expressions between both the ganglionic and aganglionic colons from patients with HSCR and control colons [15]. NRG1 expression data were provided as mean values ± standard deviation (SD). The normality of the NRG1 expression was determined by the Kolmogorov–Smirnov test. Independent t-tests were used to analyze the significant differences of NRG1 expression between the groups. A p-value of < 0.05 was considered significant. The IBM Statistical Package for the Social Sciences (SPSS) version 23 (Chicago, USA) was used for all statistical analyses.
Results
Comparison of NRG1 expressions in HSCR and control colons
We determined NRG1 type I (HRGβ1, HRGβ2, HRGβ3, HRGγ, and NDF43 isoforms), type II and type III expressions in both ganglionic and aganglionic colons of 20 patients with HSCR and 10 control colons. qPCR showed that expressions of all NRG1 isoforms, except HRGα/NDF43, were upregulated in ganglionic colons compared with control colons, including type I, type II, and type III (p < 0.01, < 0.01, 0.03, respectively) (Table 1).
Interestingly, in the aganglionic colons of patients with HSCR, only type I and HRGβ1/ HRGβ2 isoforms were significantly upregulated in the HSCR samples compared to the controls (p < 0.01 and 0.01) (Table 2).
Comparison of NRG1 methylation level in patients with HSCR and control
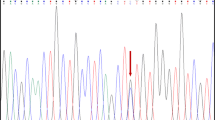
Next, we determined the NRG1 methylation level in colons of 16 patients with HSCR and 17 controls. The frequency of partially methylated NRG1 in the ganglionic (81%) and aganglionic (75%) colons were higher than the control (59%) colons, whereas none of the samples showed a full methylated pattern (Table 3 and Fig. 1).
Representative electrophoresis result of NRG1 methylation. G: ganglionic colon of HSCR patient; A: aganglionic colon of HSCR patient; C: control colon; K: positive control; W: negative control. Full-length gels are presented in Supplementary Figure 1. Positive control: positive methylation controls using DNA samples treated with SssI methyltransferase for the methylation-specific PCR (MS-PCR); negative control: without DNA
Discussion
NRG1 variants have been associated with the development of HSCR across populations [5,6,7]. However, the frequency of rare variants in our HSCR patients’ series is very low [8]. Therefore, we looked for other factors that might have a role in the HSCR pathogenesis, including NRG1 expressions and methylation patterns.
Here, we are able to show the aberrant NRG1 expressions in patients with HSCR, both in the ganglionic and aganglionic colons. Our study demonstrates significantly upregulated NRG1 expressions in patients with HSCR compared with control colons, indicating that the aberrant NRG1 expression might impact HSCR pathogenesis. This finding further confirmed a previous study [13]. However, our study has several novelties: 1) we tested the expressions of all isoforms of NRG1, including types I, II, and III (vs. only NRG1 type I [13]); 2) we quantitatively compared the NRG1 expressions between patients with HSCR and control colons (vs. only determined whether the NRG1 was expressed in patients with HSCR and control colons [6]), and 3) in the Indonesian population (vs. Chinese population [6, 13]). Interestingly, although from the same Chinese population, two studies revealed different findings: one study had the aberrant NRG1 expression in patients with HSCR [13], while another report [14] showed no differences in NRG1 expressions between patients with HSCR and controls. These findings together with our results highlight the differences in the epigenetic profile in HSCR patients among population.
In addition, a previous study showed the downregulated NRG1 expressions in breast cancer cell lines compared to normal ones [12]. In contrast, our results showed that NRG1 expressions in Indonesian patients with HSCR are upregulated compared to controls. These differences might be due to 1) different diseases may have different impacts on NRG1 expressions (developmental anomalies vs. cancer), 2) variations in genetic backgrounds between populations (Indonesia vs. Caucasian), and 3) different genetic resources (colon tissue vs. cell lines).
It has been shown that some gene expressions involved in the HSCR pathogenesis or enteric nervous system development are affected by the methylation pattern, including RET, GFRA4, EDNRB, and SHH [9]. Moreover, it has been hypothesized that NRG1 expression was affected by its hypermethylation [13]. However, they failed to prove the hypothesis and suggested a further study on different ethnic groups. Here, we successfully showed that the partially methylated NRG1 was higher in patients with HSCR than controls. Hypermethylation has been shown to suppress gene expressions [16]. Therefore, we suggest that the aberrant NRG1 expressions in our patients might be due to the methylation status. The differences between our findings and a previous report [13] might be due to the differences in genetic characteristics among populations within Asian people [17].
Notably, limitations due to small sample size and single center study should be considered during interpretation of our findings. Moreover, it suggests a further multicenter studies with a larger sample size are necessary to identify other epigenetic factors that influence the NRG1 expression in patients with HSCR.
Conclusions
Our study provides further insights into the aberrant NRG1 expression in the colons of patients with HSCR, both ganglionic and aganglionic bowel, which might contribute to the development of HSCR, particularly in Indonesia. Furthermore, these aberrant NRG1 expressions might be associated with its methylation status.
Availability of data and materials
All data generated or analyzed during this study are included in the submission. The raw data are available from the corresponding author on reasonable request.
Abbreviations
- GAPDH :
-
Glyceraldehyde-3-phosphate dehydrogenase
- HSCR:
-
Hirschsprung disease
- NRG1 :
-
Neuregulin 1
- qPCR:
-
Quantitative real-time polymerase chain reaction
References
Tam PK. Hirschsprung’s disease: a bridge for science and surgery. J Pediatr Surg. 2016;51:18–22.
Amiel J, Sproat-Emison E, Garcia-Barcelo M, et al. Hirschsprung disease, associated syndromes and genetics: a review. J Med Genet. 2008;45:1–14.
Gunadi, Karina SM, Dwihantoro A. Outcomes in patients with Hirschsprung disease following definitive surgery. BMC Res Notes. 2018;11:644.
Gunadi, Iskandar K, Makhmudi A, Kapoor A. Combined genetic effects of RET and NRG1 susceptibility variants on multifactorial Hirschsprung disease in Indonesia. J Surg Res. 2019;233:96–9.
Garcia-Barcelo MM, Tang CS, Ngan ES, Lui VC, Chen Y, So MT, et al. Genome-wide association study identifies NRG1 as a susceptibility locus for Hirschsprung’s disease. Proc Natl Acad Sci USA. 2009;106:2694–9.
Tang CS, Ngan ES, Tang WK, So MT, Cheng G, Miao XP, et al. Mutations in the NRG1 gene are associated with Hirschsprung disease. Hum Genet. 2012;131:67–76.
Luzón-Toro B, Torroglosa A, Núñez-Torres R, Enguix-Riego MV, Fernández RM, de Agustín JC, et al. Comprehensive analysis of NRG1 common and rare variants in Hirschsprung patients. PLoS ONE. 2012;7:e36524.
Gunadi, Budi NYP, Sethi R, et al. NRG1 variant effects in patients with Hirschsprung disease. BMC Pediatr. 2018;18:292.
Torroglosa A, Villalba-Benito L, Luzón-Toro B, Fernández RM, Antiñolo G, Borrego S. Epigenetic mechanisms in Hirschsprung disease. Int J Mol Sci. 2019;20:3123.
Angrisano T, Sacchetti S, Natale F, et al. Chromatin and DNA methylation dynamics during retinoic acid-induced RET gene transcriptional activation in neuroblastoma cells. Nucleic Acids Res. 2011;39:1993–2006.
Tang W, Li B, Tang J, Liu K, et al. Methylation analysis of EDNRB in human colon tissues of Hirschsprung’s disease. Pediatr Surg Int. 2013;29:683–8.
Chua YL, Ito Y, Pole JCM, et al. The nrg1 gene is frequently silenced by methylation in breast cancers and is a strong candidate for the 8p tumour suppressor gene. Oncogene. 2009;2009(28):4041–52.
Tang W, Li B, Xu X, et al. Aberrant high expression of NRG1 gene in Hirschsprung disease. J Pediatr Surg. 2012;47(9):1694–8.
Tang CS, Tang WK, So MT, Miao XP, Leung BM, Yip BH, et al. Fine mapping of the NRG1 Hirschsprung’s disease locus. PLoS ONE. 2011;20(6):e16181.
Gunadi, Kalim AS, Budi NYP, Hafiq HM, Maharani A, Febrianti M, et al. Aberrant expressions and variant screening of SEMA3D in Indonesian Hirschsprung Patients. Front Pediatr. 2020;8:60.
Biermann K, Steger K. Epigenetics in male germ cells. J Androl. 2007;28:466–80.
Tajima A, Pan IH, Fucharoen G, Fucharoen S, Matsuo M, Tokunaga K, et al. Three major lineages of Asian Y chromosomes: implications for the peopling of east and southeast Asia. Hum Genet. 2002;110:80–8.
Acknowledgements
We are thankful to a native speaker at the English Services Center, Faculty of Medicine, Public Health and Nursing, UGM, for proofreading our manuscript. We are also grateful to those who provided excellent technical support and assistance during the study.
Funding
This work was supported by a grant from the Indonesian Ministry of Research, Technology, and Higher Education (1700/UN1/DITLIT/DIT-LIT/LT/2018 and 2817/UN1.DITLIT/DIT-LIT.LT/2019 to G) and the Faculty of Medicine, Public Health, and Nursing, Universitas Gadjah Mada, Indonesia (UPPM/363/M/05/04/05.18 to G. and KI). The funder had no role in the design of the study, preparation of the manuscript, and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
G and KI conceived the study. G and ASK drafted the manuscript, and KI critically revised the manuscript for important intellectual content. ASK, M, and NYPB facilitated all project-related tasks. All authors have read and approved the manuscript and agreed to be accountable for all aspects of the work to ensure that questions related to accuracy or integrity of any part of work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Medical and Health Research Ethics Committee of Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada/Dr. Sardjito Hospital gave approval for this study (KE/FK/0111/EC/2020 and KE/FK/0880/2018). The patients with HSCR and controls were ascertained for this study after their parents signed a written informed consent form. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gunadi, Kalim, A.S., Marcellus et al. The impact of NRG1 expressions and methylation on multifactorial Hirschsprung disease. BMC Pediatr 22, 216 (2022). https://doi.org/10.1186/s12887-022-03287-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03287-1