Abstract
Background
Hemophagocytic lymphohistiocytosis (HLH) is a rare, life-threatening disorder characterized by prolonged fever, cytopenia, hepatosplenomegaly, rash, icterus, and other neurological symptoms. Successful treatment of HLH by etoposide has improved outcomes for children with HLH. However, the development of treatment-related acute myeloid leukemia (t-AML) after the usage of this drug is a concern.
Case presentation
We report a case of acquired EBV-triggered HLH with progression to t-AML following etoposide therapy with cytogenetic abnormality for t (11; 19) (q23; p13) resulting in MLL gene fusion. The development of t-AML was detected 23 months after HLH diagnosis.
Conclusions
Although the successful treatment of HLH by etoposide has improved outcomes for children with HLH, t-AML is a serious complication of topoisomerase II inhibitor therapy and is characterized by the presence of gene rearrangement. This study suggests that HLH patients undergoing therapy with HLH-2004 protocol need monitoring for future malignancy, especially in the initial 2 to 3 years.
Similar content being viewed by others
Background
Hemophagocytic lymphohistiocytosis (HLH) is a life-threatening disease of the immune system. HLH can be related into inherited gene defects or be triggered by severe infections, particularly with Epstein-Barr virus (EBV), rheumatoid disorders, or various malignant neoplasms. Familial hemophagocytic lymphohistiocytosis (FHL) is an immune disorder of autosomal recessive inheritance and is usually diagnosed within the first two years of life. Disease-causing mutations in gene PRF1, UNC13D, STX11, RAB27A, and STXBP2 (Munc18-2) have been found in FHL [1]. Hematopoietic stem cell transplantation (HSCT) is currently the only available curative method for FHL patients. Secondary HLH may occur anytime in life. EBV-associated hemophagocytic lymphohistiocytosis (EBV-HLH) syndrome is the most common trigger in the pediatric population. The mortality rate is 50 % if only supportive care is given for EBV-HLH patients [2]. HLH patients can die because of overwhelming infections or uncontrolled systemic inflammation and multi-organ failure. Therefore, HLH needs prompt diagnosis and immediate institution of therapy to improve the outcome in affected children. The control of the primary triggering factor and suppression of the overactive inflammation should be simultaneously pursued in treatment of HLH.
The successful treatment of HLH by etoposide has improved outcomes in children with HLH. However, development of t-AML related to the usage of this drug is a concern. In the present study, a case of EBV-HLH is reported with progression to t-AML following etoposide therapy with cytogenetic abnormality for t (11; 19) (q23; p13) resulting in MLL gene fusion.
Case presentation
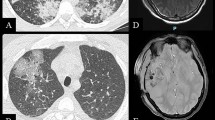
The patient was a 10-month-old Chinese female who was first diagnosed with HLH when she showed various symptoms, such as persistent high fever of unknown origin, seizures, jaundice, pancytopenia, coagulopathy, and hepatosplenomegaly. Physical examination also revealed lethargy, pallor, cervical lymph node swelling, and hepatosplenomegaly. Laboratory evaluations showed Hg b at 9.7 g/dl, H ct at 19.7 %, platelet at 60 K/μL, WBC at 2.67 K/μL, ferritin at 622 ng/mL, triglyceride at 532 mg/dl, ALT at 4068 U/L, AST at 9162 U/L, ALP at 1016 U/L, lactate dehydrogenase (LDH) at 12,108 U/L, total bilirubin at 100.9 umol/L, direct bilirubin at 51.5 umol/L, fibrinogen at 390 mg/dl, PT/PTT at 20.5/65.4 s, thrombin time of 46.7 s, and D-dimers at 851 ng/L. In summary, the patient fulfilled 5 out of 8 HLH-2004 criteria [3]. The cerebrospinal fluid examination showed protein at 3.5 g/L and pleocytosis at 20 × 109/L. A magnetic resonance imaging (MRI) of the brain revealed no abnormality. Polymerase chain reaction (PCR) analysis for the EBV EBNA-1 was positive in peripheral blood. The EBV-DNA in blood was 6.25 × 104 IU/mL. Bone marrow examination showed increased hemophagocytic histiocytes (HS) (Fig. 1a), which is consistent with HLH. Cytogenetic analysis was normal. A hereditary defect predisposing to HLH was not excluded. However, the long recurrence-free period argues against an hereditary background.
The patient received chemotherapy according to the HLH-2004 protocol, which includes etoposide, steroids, intrathecal methotrexate, and cyclosporin. The patient achieved complete remission of the disease at the end of the initial treatment period of 16 weeks. The patient did not achieved full remission of the disease until the end of the initial treatment period of 8 weeks. Treatment was thus continued until week 16 and was then stopped asl the parents declined further therapy. In total, the patient’s cumulative dose of etoposide was 2100 mg/m2 during the 16-week period.
After 23 months, the patient was readmitted with fever, leukocytosis, anemia, diffuse lymphadenopathy, and hepato-splenomegaly of 5 and 4 cm, which is palpable below the costal margins. LDH was elevated at 1788 U/L. Bone marrow examination revealed 89 % monoblasts, without evidence of HS (Fig. 1b). Flow cytometry studies indicated that 86.4 % of leukocytes were positive for CD33, CD7, CD11b, CD13, CD15, CD34, CD38, CD64, CD117, myeloperoxidase (MPO), and cytoplasmic CD68. Chromosome analysis of 48 h culture from bone marrow aspiration revealed complex karyotype aberrations. The karyotype was interpreted as 46, XX, d e r (11) t (11; 19) (q23; p13) inv (11) (q23 p15), and d e r (19) t (11; 19). The fusion gene was MLL/ELL. The diagnosis of AML (M5b) was made,. Induction chemotherapy with idarubicin and Ara-C (DA) was given, and the patient achieved complete remission in bone marrow morphology after two courses.
The patient is currently on chemotherapy for AML, and her bone marrow revealed no residual or recurrent leukemia cell after the initial complete remission.
Discussion
We report a case of a 10-month-old Chinese female with EBV-associated HLH, who showed a progression to t-AML following etoposide therapy with cytogenetic abnormality for t (11; 19) (q23; p13) and MLL gene fusion, 23 months after the onset of HLH.
The t-AML following the etoposide therapy is not infrequent in malignant neoplasms such as leukemia and has first been reported in lung cancer in the 1980s [3]. About 2–12 % of patients treated with topoisomerase II inhibitors develop t-AML, frequently associated with translocations at 11q23 [4]. A review of related literature revealed 13 (11 secondary HLH and 2 FHL) cases of t-AML in HLH patients treated with etoposide (Table 1) [5–16].
The aim of this paper is to fully describe the patient with an adverse effect of etoposide in the therapy of HLH and to characterize the risks and prognosis of t-AML.
HLH is a life-threatening hyperinflammatory disease caused by an uncontrolled and dysfunctional immune response of inherited or acquired immune deficiencies. All forms of HLH are characterized by an impaired function of natural killer (NK) cells and cytotoxic T-cells (CTL) [2]. EBV-associated HLH patients had mortality rates 14 times higher than when etoposide therapy was not initiated within the first four weeks [6]. The international protocol (HLH -94/2004), which consists of etoposide, dexamethasone, and cyclosporine, has been shown to induce remission of the disease. Etoposide is considered the most effective therapy for HLH, which acts through the inhibition of topoisomerase II and shows a high activity in monocytic and histiocytic disorders. The cumulative dose of etoposide of the HLH-2004 protocol 8 weeks induction is 1500 mg/m2. Imashuku et al. [17] reported that the chance of survival was significantly better for EBV-HLH patients receiving a cumulative dose of etoposide of 1000 to 3000 mg/m2 (P = .0001), compared with that of <1000 mg/m2 and without etoposide.
However, development of t-AML related to the usage of this drug is a concern. Most translocations of leukemia associated with epipodophyllotoxin disrupt an 8.3 kb breakpoint cluster region (b c r) between exons 5 and 11 of the MLL gene at chromosome band 11q23 [18]. Molecular characterization of breakpoints at 11q23 led to the identification of the MLL gene, which plays an important role in gene regulation during embryonic development and regulation of HOX genes during normal haematopoiesis [18]. MLL translocations are related to the occurrence of leukemia by gene fusion and resistance to stress-induced cell death and specific drugs. Four out of thirteen t-AML cases had MLL gene translocations at chromosome band 11q23.
Additional chromosome aberrations, such as t (15; 17), t (8; 21), inv (16), t (8; 16), t (11; 20), or t (11; 16), were also reported in younger patients and showed a shorter latency period between the primary tumor and t-AML [19]. Four of the 13 reported t-AML cases following etoposide in HLH therapy protocol were diagnosed with treatment-related APL with t (15; 17), as shown in Table 1.
Cases of t-AML following epipodophyllotoxin treatment generally occur within a relatively short latency period (ranging from 6 to 36 months), with 11 out of 13 cases developing t-AML within 36 months, as shown in these findings (Table 1). In the present study, the time interval between the occurrence of the hemophagocytic syndrome and the diagnosis of t-AML is 23 months.
One study demonstrates how early translocations first occur during the administration of topoisomerase II therapy. The MLL-GAS7 translocation was PCR-detectable by 1.5 months after starting treatment at low cumulative doses of the DNA topoisomerase II inhibitor doxorubicin [20]. Ng et al. [12] conservatively estimated that a 6.7 kb MLL cleavage fragment was detected in the bone marrow 3 months after a low dose of etoposide and 3 months prior to the diagnosis of overt t-AML. These studies may offer new leads for early detection and diagnosis as well as an understanding of the mechanism behind these translocations.
Different factors play a role for the risk of etoposide-related AML, which include the cumulative dose, schedule, other chemotherapeutic agents, and host factors. Imashuku et al. [17] investigated that the dosage of etoposide in the range of 1000–3000 mg/m2 was appropriate. However, three patients (shown in Table 1) who received less than 1000 mg/m2 cumulative dose of etoposide developed t-AML. The National Cancer Therapy Evalution Program (CTEP) showed that the calculated cumulative 6-year risks for the occurrence of t-AML for the low (<1.5 g/m2), moderate (1.5–2.99 g/m2), and high dose (≥3.0 g/m2) groups were 3.2, 0.7, and 2.2 %, respectively, and concluded that the incidence of t-AML after treatment with epipodophyllotoxins is not purely dose-dependent [21]. Winick [22] investigated the epipodophyllotoxin administration associated with the highest incidence (12 %) of t-AML in weekly or twice-weekly schedules in primary ALL. The administration of L-asparaginase, methotrexate, 6-mercaptopurine, cisplatin, and anthracyclines associated with epipodophyllotoxins is considered to increase the risk of t-AML [23]. Genetic polymorphisms in CYP3A5, CYP3A4, NQO1, and glutathione S-transferase genotypes have been demonstrated to play an important role in secondary malignancies [24, 25].
The outcome of t-AML is generally considered to be poorer than that of de novo AML. Remission is 80–90 % in t-AML, but long-term survival rates were 10–20 % [26]. Children with t-AML have a 5-year survival rate (23.7 %), which is significantly lower than that of children with AML as a first primary cancer (53.2 %) [26, 27]. Cytogenetics are important prognostic parameters in t-AML. Patients with t-AML who have favorable karyotypes, such as t (8; 21), inv (16), or t (15; 17), have good prognosis and can be given chemotherapyonly [27]. Su et al. [5] noted that all four t-APL patients receiving a combined application of all-trans retinoic acid and darubicin/Ara C had good diagnoses. Elliott et al. [28] observed that t-APL is sensitive to standard therapy. All four t-APL patients in Table 1 were alive after receiving chemotherapyonly. Schoch et al. [29] observed no statistically significant differences in overall survival (OS) of t-AML patientsin the group of the unfavorable and intermediate cytogenetics, whereas only the favorable subgroup showed a significantly shorter OS as compared with de novo AML. Outcomes were better among t-AML patients randomly assigned to receive intensively timed induction therapy than among those who received standard-timed induction [23]. Allogenic bone marrow transplantation was most effective for t-AML in remission at the time of transplant. Half (3/6) of the transplantation recipients for t-AML were alive, as shown in Table 1.
Conclusions
In conclusion, therapy-related AML is the most serious complication of VP-16/etoposide-related chemotherapy for HLH.
Abbreviations
CTEP, the national cancer therapy evalution program; CTL, cytotoxic t-cells; EBNA-1, Epstein-Barr virus nuclear antigen-1; HLH, hemophagocytic lymphohistiocytosis; HS, hemophagocytic histiocytes; HSCT, hematopoietic stem cell transplantation; MLL, mixed-lineage leukemia; MTX, methotrexate; NK, natural killer cells; OS, overall survival; PCR, polymerase chain reaction; T-AML, treatment-related acute myeloid leukemia
References
Bode SF, Lehmberg K, Maul-Pavicic A, Vraetz T, Janka G, Stadt U, Ehl S. Recent advances in the diagnosis and treatment of hemophagocytic lymphohistiocytosis. Arthritis Res Ther. 2012;14:213.
Janka EG. Familial and acquired hemophagocytic lymphohistiocytosis. Annu Rev Med. 2012;63:233–46.
Rajaqopala S, Singh N. Diagnosing and treating hemophagocytic lymphohistiocytosis in the tropics: systematic review from the Indian subcontinent. Acta Med Acad. 2012;41:161–74.
Smith MA, Rubinstein L, Ungerleider RS. Therapy-related acute myeloid leukemia following treatment with epipodophyllotoxins: estimating the risks. Med Pediatr Oncol. 1994;23:86–98.
Su Y, Zhou X, Zhang L, Zhang L, Zhang R. Report of a case with secondary acute promyelocytic leukemia after therapy for hemophagocytic lymphohistiocytosis and review of literature. Chin J Pediatr. 2013;51:938–42.
Sathiyamoorthy S, Shad A, Ozdemirli M. Acute promyelocytic leukemia following chemotherapy for EBV-associated hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2011;56:850–2.
Rama Chandran S, Ariffin H. Secondary acute myeloid leukemia after etoposide therapy for haemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2009;53:488–90.
Shamsian BS, Gharib A, Rezaei N, Esfahani SA, Alavi S, Goudarzipour K, Arzanian MT. Development of secondary T-cell acute lymphoblastic leukemia in a child with hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2010;55:725–6.
Seo YI, Park R, Choi TY, Shin JW, Won JH, Park HS, Lee NS, Cho D. A case of therapy-related acute monocytic leukemia following low-dose of etoposide treatment for hemophagocytic lymphohistocytosis. Korean J Lab Med. 2007;27:244–7.
Kitazawa J, Ito E, Arai K, Yokoyama M, Fukayama M, Imashuku S. Secondary acute myelocytic leukemia after successful chemotherapy with etoposide for Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis. Med Pediatr Oncol. 2001;37:153–4.
Takahashi T, Yagasaki F, Endo K, Takahashi M, Itoh Y, Kawai N, Kusumoto S, Murohashi I, Bessho M, Hirashima K. Therapy-related AML after successful chemotherapy with low dose etoposide for virus-associated hemophagocytic syndrome. Int J Hematol. 1998;68:333–6.
Ng A, Ravetto PF, Taylor GM, Wynn RF, Eden OB. Coexistence of treatment-related MLL cleavage and rearrangement in a child with haemophagocytic lymphohistiocytosis. Br J Cancer. 2004;91:1990–2.
Stine KC, Saylors RL, Sawyer JR, Becton DL. Secondary acute myelogenous leukemia following safe exposure to etoposide. J Clin Oncol. 1997;15:1583–6.
Ohtake M, Suzuki R, Kondo S. Etoposide-related t-AML in a case of EBV-HLH. Presented at the 16th Annual Meeting of EBV infection-related diseases. Tokyo (in Japanese); 2006.
Henter JI, Elinder G, Lubeck PO, Ost A. Myelodysplastic syndrome following epipodophyllotoxin therapy in familial hemophagocytic lymphohistiocytosis. Pediatr Hematol Oncol. 1993;10:163–8.
Rudd E, Göransdotter Ericson K, Zheng C, Uysal Z, özkan A, Gurgey A, Fadeel B, Nordenskjöld M, Henter JI. Spectrum and clinical implications of syntaxin 11 gene mutations in familial haemophagocytic lymphohistiocytosis: Association with disease-free remissions and haematopoietic malignancies. J Med Genet. 2006;43:e14.
Imashuku S, Teramura T, Kuriyama K, Kitazawa J, Ito E, Morimoto A, Hibi S. Risk of etoposide-related acute myeloid leukemia in the treatment of Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis. Int J Hematol. 2002;75:174–7.
Rubnitz JE, Behm FG, Downing JR. 11 q23 Rearrangements in acute leukemia. Leukemia. 1996;10:74–82.
Quensel B, Kantarjian H, Bjergaard JP, Brault P, Lai JL, Estey E, Tilly H, Stoppa AM, Archimbaud E, Harousseau JL. Therapy-related acute myeloid leukemia with t (8; 21), inv (16), t (8; 16):A report on 25 cases and review of the literature. J Clin Oncol. 1993;11:2370–9.
Megonigal MD, Cheung NK, Rappaport EF, Nowell PC, Wilson RB, Jones DH, Addya K, Leonard DB, Kushner BH, Williams TM, Lange BJ, Felix CA. Detection of leukemia-associated MLL-GAS7 translocation early during chemotherapy with DNA topoisomerase II inhibitors. Proc Natl Acad Sci U S A. 2000;97:2814–9.
Hijiya N, Hudson MM, Lensing S, Zacher M, Onciu M, Behm FG, Razzouk BI, Ribeiro RC, Rubnitz JE, Sandlund JT, Rivera GK, Evans WE, Relling MV, Pui CH. Cumulative incidence of secondary neoplasms as a first event after childhood acute lymphoblastic leukemia. JAMA. 2007;297:1207–15.
Winick NJ, McKenna RW, Shuster JJ, Schneider NR, Borowitz MJ, Bowman WP, Jacaruso D, Kamen BA, Buchanan GR. Secondary acute myeloid leukemia in children with acute lymphoblastic leukemia treated with etoposide. J Clin Oncol. 1993;11:209–17.
Barnard DR, Lange B, Alonzo TA, Buckley J, Kobrinsky JN, Gold S, Sanders J, Burden L, Woods WG. Acute myeloid leukemia and myelodysplastic syndrome in children treated for cancer: comparison with primary presentation. Blood. 2002;100:427–34.
Blanco JG, Edick MJ, Hancock ML, Winick NJ, Dervieux T, Amylon MD, Bash RO, Behm FG, Camitta BM, Pui CH, Raimondi SC, Relling MV. Genetic polymorphisms in CYP3A5, CYP3A4 and NQO1 in children who developed therapy-related myeloid malignancies. Pharmacogenetics. 2002;12:605–11.
Woo MH, Shuster JJ, Chen C, Bash RO, Behm FG, Camitta B, Felix CA, Kamen BA, Pui CH, Raimondi SC, Winick NJ, Amylon MD, Relling MV. Glutathione S-transferase genotypes in children who develop treatment-related acute myeloid malignancies. Leukemia. 2000;14:232–7.
Sandler ES, Friedman DJ, Mustafa MM, Winick NJ, Bowman WP, Buchanan GR. Treatment of children with epipodophyllotoxin-induced secondary acute myeloid leukemia. Cancer. 1997;79:1049–54.
National Cancer Institute. Overall period survival 2003-ALL and AML Children < 20 years Allowing multiple primaries. Survellance Research Program, National Cancer Institute SEER*Stat software. 2006. (www.seer.cancer.gov/seerstat) version 6.3.6: Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER 17 Regs Limited-Use, Nov 2006 Sub (1973–2004 varying) - Linked to County Attibutes - Total U.S, 1969–2004 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch, released April 2007, based on the November 2006 submission.
Elliott MA, Letendre L, Tefferi A, Hogan WJ, Hook C, Kaufmann SH, Pruthi RK, Pardanani A, Begna KH, Ashrani AA, Wolanskyj AP, Al-Kali A, Litzow MR. Therapy-related acute promyelocytic leukemia: observations relating to APL pathogenesis and therapy. Eur J Haematol. 2012;88:237–43.
Schoch C, Kern W, Schnittger S, Hiddemann W, Haferlach T. Karyotype is an independent prognostic parameter in therapy-related acute myeloid leukemia (t-AML): an analysis of 93 patients with t-AML in comparison to 1091 patients with de novo AML. Leukemia. 2004;18:120–5.
Acknowledgements
The authors thank Professor Ke Lei for providing the image of the bone marrow smear for the patient.
Authors’ contributions
All authors contributed to the conception and design and gave the final approval for the version to be published. HP drafted the manuscript; DF, LS, and LS participated on the design and coordination and helped in drafting the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent was obtained from the patient’s parents for publication of this case report. A copy of the written consent is available for review by the editor of this journal. The report has been performed with the approval of the ethics committee of the Department of Pediatric Hematology.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Pan, H., Feng, Dn., Song, L. et al. Acute myeloid leukemia following etoposide therapy for EBV-associated hemophagocytic lymphohistiocytosis: a case report and a brief review of the literature. BMC Pediatr 16, 116 (2016). https://doi.org/10.1186/s12887-016-0649-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-016-0649-z