Abstract
Background
Persistent placoid maculopathy (PPM) is a rare idiopathic chorioretinopathy characterized by choriocapillaris (CC) hypoperfusion. In a case of PPM, we quantified CC flow deficits (FDs) over time and observed an increase in CC perfusion as the visual acuity and outer photoreceptor anatomy improved.
Case presentation
A 58-year-old man was diagnosed with PPM in both eyes based on the patient’s clinical presentation and imaging. He presented with sudden-onset central scotomas in both eyes for about two months. On referral, the best corrected visual acuity (BCVA) was 20/20 in the right eye and 20/100 in the left eye. Plaque-like yellowish macular lesions were observed bilaterally and autofluorescence imaging showed bilateral hyperautofluorescent lesions. Fluorescein angiography (FA) revealed early-phase hyper-fluorescent staining that intensified in the late phases, while indocyanine green angiography (ICGA) displayed persistent hypofluorescence in both eyes. Foveal centered swept source optical coherence tomography (SS-OCT) B-scans showed bilateral focal deposits on the level of retinal pigment epithelium (RPE) and disruption of outer photoreceptor bands. The CC FDs were quantified on SS-OCT angiography (SS-OCTA) images using a previously published algorithm that was validated. The CC FD% was 12.52% in the right eye and 14.64% in the left eye within a 5 mm circle centered on the fovea. After 5 months of steroid treatment, BCVA remained 20/20 in the right eye and improved to 20/25 in the left eye. On OCT imaging, the outer photoreceptor bands fully recovered in both eyes, while some focal deposits remained along the RPE in the left eye. The CC perfusion in both eyes improved, with CC FD% decreasing from 12.52% to 9.16% in the right eye and from 14.64% to 9.34% in the left eye.
Conclusions
Significant impairment of macular CC perfusion was detected after the onset of PPM. Improvement in central macular CC perfusion corresponded with improvements in BCVA and outer retinal anatomy. Our findings suggest that imaging and quantification of CC FDs could serve as a valuable imaging strategy for diagnosing PPM and for following disease progression.
Similar content being viewed by others
Background
Persistent placoid maculopathy (PPM) is an idiopathic, bilateral chorioretinopathy that was first described in 2006 [1]. Its pathophysiology has not been clearly established [2]. Previous studies have reported hypoperfusion of the choriocapillaris (CC) in PPM; [3,4,5] however, CC flow deficits (FDs) have not been quantified previously.
Optical coherence tomography angiography (OCTA) can detect blood flow within the CC by repeating multiple B-scans at a specific position and then comparing differences in the intensity and phase signals from these repeated B scans [6]. These changes in the signals from repeated B-scans are due to the movement of erythrocytes within the capillaries, and result in an angiographic image of blood flow [7,8,9,10,11]. Swept-source optical coherence tomography angiography (SS-OCTA) provides a more detailed visualization of the CC than spectral domain OCT angiography (SD-OCTA) due to its longer wavelength of 1050 nm band compared with the SD-OCTA wavelength of 840 nm band [12, 13]. Due to its longer wavelength band and faster imaging speed, SS-OCTA imaging also allows for better penetration of light through the retinal pigment epithelium (RPE) and denser scan patterns, which results in better detection of blood flow in the CC and improved image quality. Validated algorithms have been developed to quantify the CC flow deficits (FDs) [14].
In this report, we describe a case of PPM with macular CC hypoperfusion at baseline, and as the best-corrected visual acuity (BCVA) improves, the percentage of CC FDs decreases, and the outer photoreceptor anatomy improves.
Case presentation
A 58-year-old man was referred with a history of sudden-onset central scotomas in both eyes that had persisted for two months. He initially complained of headaches, fevers, chills, and muscle aches for the first five days, and tested negative for COVID-19 twice. His electrocardiogram, chest x-ray, and head computed tomography were normal when performed in the emergency room. There was no remarkable medical or family history. He was referred by an outside retina specialist with a diagnosis of an uncertain maculopathy.
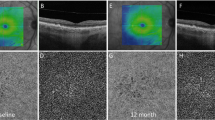
On examination, his best corrected visual acuity (BCVA) measurements were 20/20 in the right eye and 20/100 in the left eye. The anterior segment examination was unremarkable in both eyes. Plaque-like yellowish macular lesions were observed bilaterally (Fig. 1A and C). Autofluorescence imaging showed bilateral focal hyperautofluorescent lesions (Fig. 1B and D). Fluorescein angiography (FA) revealed early-phase macular hyperfluorescent staining (Fig. 1E and G) that intensified in the late phases (Fig. 1F and H), while indocyanine green angiography (ICGA) showed persistent macular hypofluorescence in both eyes (Fig. 1I-L). The foveal centered SS-OCT B-scans showed bilateral focal deposits on the retinal pigment epithelium (RPE) and disruption of the outer photoreceptor bands (Fig. 2A and C). The CC FDs were imaged using SS-OCTA and quantified using our previously published method [14]. The CC structural images displayed some focal defects (Fig. 2E and G) while the CC flow images (Fig. 2I-K) showed more obvious foci with loss of perfusion. After binarization, the density of CC FDs within a 5 mm circle centered on the fovea were 12.52% in the right eye and 14.64% in the left eye (Fig. 2M and O). Laboratory tests, which included a complete blood count, angiotensin-converting enzyme levels, a comprehensive metabolic panel, a treponemal syphilis test and a QuantiFERON test, were all found to be unremarkable.
Bilateral fundus appearance at the first visit. A, C Optos fundus images show plaque-like yellowish lesions in the central maculae of the right (A) and left (C) eyes at presentation. B, D Autofluorescence of the right (B) and left (D) eyes at presentation show focal hyperautofluorescent lesions. E, F, G, H, Early phase E, G and late phase F, H fluorescein angiography images of the right E, F and left G. H eyes show persistent hyperfluorescence staining that increases in intensity with time. I, J, K, L Early phase (I, K) and late phase (J, K) indocyanine green angiography images show persistent hypo-fluorescence in both eyes
Longitudinal changes in the outer retinal bands and choriocapillaris in both eyes. A, C The foveal centered SS-OCT B-scans show focal deposits on retinal pigment epithelium (RPE) and disruption of the outer photoreceptor bands in both the right (A) and left (C) eyes at presentation. B, D 5 months later, the right eye shows restoration of the outer photoreceptors bands (B), while some focal deposits remain along the RPE in the left eye (D). The blue boxes show the magnification of the fovea region in both eyes. The yellow lines in A-D were the boundaries of the CC slab. E, G At the first visit, choriocapillaris (CC) structural images from the algorithm display some focal signal intensity defects in the right (E) and left eyes (G). (F, H) At the 5-month follow-up, CC structural images appeared to have little signal variability throughout the scan area. (I, K) CC flow deficit (FD) images of the right (I) and left eyes (K) show focal areas of CC hypoperfusion at the first visit. (J, L) 5 months later, CC flow images are greatly improved. (M, N, O, P) Binarized CC FDs images with the white denote the area of CC FD. The CC FD% were 12.52% (M) in the right eye and 14.64% (O) in the left eye within a 5 mm circle centered on the fovea at the first visit. At five months of follow-up, the CC FD% were 9.16% (N) in the right eye and 9.34% (P) in the left eyes
Based on the patient’s clinical presentation and imaging, he was diagnosed with PPM and treated with oral prednisone which started at 60 mg daily and tapered to 10 mg daily over 7 weeks, then subsequently tapered off over 15 weeks. Two months after the onset of treatment, his BCVA remained stable in the right eye at 20/20 and improved to 20/25 in the left eye. At his five-month follow-up visit, the right eye outer photoreceptor bands had fully recovered, while some focal deposits remained along the RPE in the left eye (Fig. 2B and D). Improvements in both the CC structural and flow images were observed (Fig. 2F, H, J and L) with the CC FDs in the right eye decreasing to 9.16%, and in the left eye, the CC FDs decreased to 9.34% (Fig. 2N and P).
Discussion and conclusions
In this case, significant impairment of macular CC perfusion was detected on the onset of PPM. A previous study argued the choroidal hypoperfusion was due to a masking effect caused by cellular infiltrate, [15] and another research speculated it was an artifact of optical blockage by the placoid lesions [16]. However, our observation that the CC structural images (Fig. 2E-H) had few signal abnormalities while the central CC flow images (Fig. 2I-L) were markedly abnormal suggests that the CC hypoperfusion was real.
In previous reports, CC flow impairment has been suggested based on FA, ICGA and OCTA imaging [1, 3,4,5, 15, 16]. In this current report, we were able to both document and quantitate CC FDs longitudinally using SS-OCTA. Moreover, CC perfusion improved over time as the visual acuity and the outer retina anatomy improved. At presentation, CC FDs were measured at 12.52% and 14.64% in the right and left eyes respectively, with the better CC perfusion corresponding to better BCVA and outer retinal OCT anatomy in the right eye. After 5 months of treatment, the CC FDs improved bilaterally to about 9%. The photoreceptor and RPE anatomy on OCT imaging returned nearly to normal except for some remaining focal deposits along the RPE in the left eye.
The patient was treated with oral prednisone for 5 months resulting in improved vision and no evidence of macular neovascularization, which had been reported previously [3]. Although oral steroids are generally used as first-line agents, [2] it remains controversial whether steroids are needed or if gradual improvement is the normal course of disease progression.
This report demonstrates the value of SS-OCTA imaging for both the structural integrity of the outer retina and RPE as well as the quantitation of central macular CC FDs. We then correlated these findings with disease symptoms and were able to show that CC perfusion improved as BCVA improved and the outer retinal OCT anatomy was restored. These results suggest that imaging and quantitation of CC FDs should be a valuable parameter to monitor when following disease progression in PPM.
Availability of data and materials
All data supporting our findings are provided in the manuscript.
Abbreviations
- PPM:
-
persistent placoid maculopathy
- CC:
-
choriocapillaris
- CC FDs:
-
choriocapillaris flow deficits
- BCVA:
-
best corrected visual acuity
- FA:
-
fluorescein angiography
- ICGA:
-
indocyanine green angiography
- OCT:
-
optical coherence tomography
- SS-OCT:
-
swept source optical coherence tomography
- OCTA:
-
optical coherence tomography angiography
- SS-OCTA:
-
swept source optical coherence tomography angiography
- SD-OCTA:
-
spectral domain optical coherence tomography angiography
- RPE:
-
retinal pigment epithelium
References
Golchet PR, Jampol LM, Wilson D, Yannuzzi LA, Ober M, Stroh E. Persistent placoid maculopathy: a new clinical entity. Trans Am Ophthalmol Soc. 2006;104:108–20.
Kolomeyer AM, Brucker AJ. Persistent placoid maculopathy: a systematic review. Retina. 2018;38(10):1881–95.
Fogel Levin M, Wong A, Sarraf D. Choroidal ischemia drives macular neovascularization in persistent placoid maculopathy. Am J Ophthalmol Case Rep. 2022;26:101563.
Klufas MA, Phasukkijwatana N, Iafe NA, et al. Optical coherence tomography angiography reveals Choriocapillaris Flow reduction in Placoid Chorioretinitis. Ophthalmol Retina. 2017;1(1):77–91.
Sassalos TM, Saraf SS, Ober MD. Chorioretinal Perfusion in Persistent Placoid Maculopathy. Ophthalmic Surg Lasers Imaging Retina. 2017;48(12):1026–31.
Chen CL, Wang RK. Optical coherence tomography based angiography [Invited]. Biomed Opt Express. 2017;8(2):1056–82.
An L, Wang RK. In vivo volumetric imaging of vascular perfusion within human retina and choroids with optical micro-angiography. Opt Express. 2008;16(15):11438–52.
Fingler J, Schwartz D, Yang C, Fraser SE. Mobility and transverse flow visualization using phase variance contrast with spectral domain optical coherence tomography. Opt Express. 2007;15(20):12636–53.
Kurokawa K, Sasaki K, Makita S, Hong YJ, Yasuno Y. Three-dimensional retinal and choroidal capillary imaging by power Doppler optical coherence angiography with adaptive optics. Opt Express. 2012;20(20):22796–812.
Makita S, Jaillon F, Yamanari M, Miura M, Yasuno Y. Comprehensive in vivo micro-vascular imaging of the human eye by dual-beam-scan Doppler optical coherence angiography. Opt Express. 2011;19(2):1271–83.
Yu L, Chen Z. Doppler variance imaging for three-dimensional retina and choroid angiography. J Biomed Opt. 2010;15(1):016029.
Lane M, Moult EM, Novais EA, et al. Visualizing the Choriocapillaris under Drusen: comparing 1050-nm swept-source Versus 840-nm spectral-domain Optical Coherence Tomography Angiography. Invest Ophthalmol Vis Sci. 2016;57(9):OCT585–590.
Miller AR, Roisman L, Zhang Q, et al. Comparison between spectral-domain and swept-source Optical Coherence Tomography Angiographic Imaging of Choroidal Neovascularization. Invest Ophthalmol Vis Sci. 2017;58(3):1499–505.
Shi Y, Chu Z, Wang L, et al. Validation of a compensation strategy used to Detect Choriocapillaris Flow deficits under Drusen with swept source OCT angiography. Am J Ophthalmol. 2020;220:115–27.
Nika M, Kalyani PS, Jayasundera KT, Comer GM. Pathogenesis of persistent placoid maculopathy: a multidol imaging analysis. Retina. 2015;35(8):1531–9.
Gendy MG, Fawzi AA, Wendel RT, Pieramici DJ, Miller JA, Jampol LM. Multimodal imaging in persistent placoid maculopathy. JAMA Ophthalmol. 2014;132(1):38–49.
Acknowledgements
We thank the patient for granting permission to publish this information. We appreciate Linda O’Koren and Mark Lazcano, Department of Ophthalmology, Bascom Palmer Eye Institute, University of Miami Miller School of Medicine, in obtaining the SS-OCTA scans.
Funding
This research was supported by grants from the National Eye Institute (R01EY028753), Carl Zeiss Meditec, an unrestricted grant from the Research to Prevent Blindness, Inc., New York, NY, and the National Eye Institute Center Core Grant (P30EY014801) to the Department of Ophthalmology, University of Miami Miller School of Medicine.
Author information
Authors and Affiliations
Contributions
JL and PJR designed the study; JL, CYW, MS, LB, JN, AS, TA and PJR participated in the acquisition of data. JL, YC, RKW, GG and PJR analyzed and interpreted the data. JL and PJR wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was performed in accordance with the tenets of the Declaration of Helsinki and complied with the Health Insurance Portability and Accountability Act of 1996 and was approved by the institutional review board of the University of Miami Miller School of Medicine. The patient provided written informed consent for participation in the study. A copy of the written consent is available for review by the editor of this journal.
Consent for publication
Written informed consent was obtained for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor of this journal.
Competing interests
Philip Rosenfeld and Giovanni Gregori receive research support from Carl Zeiss Meditec, Inc. and the University of Miami co-own a patent that is licensed to Carl Zeiss Meditec, Inc.
Philip Rosenfeld also received research funding from Gyroscope Therapeutics, Stealth BioTherapeutics, and Alexion Pharmaceuticals. He is also a consultant for Annexon, Apellis, Boehringer-Ingelheim, Carl Zeiss Meditec, Chengdu Kanghong Biotech, Ocunexus (InflammX) Therapeutics, Ocudyne, Regeneron Pharmaceuticals, and Unity Biotechnology. He also has equity interest in Apellis, Valitor, Verana Health, and Ocudyne.
Ruikang K. Wang discloses intellectual property owned by the Oregon Health and Science University and the University of Washington. He also receives research support from Colgate Palmolive Company and Estee Lauder Inc. He is a consultant to Insight Photonic Solutions, and Carl Zeiss Meditec.
The other authors have no disclosures.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, J., Wu, C.Y., Shen, M. et al. Longitudinal quantification of choriocapillaris flow deficits in persistent placoid maculopathy: a case report. BMC Ophthalmol 23, 161 (2023). https://doi.org/10.1186/s12886-023-02894-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-023-02894-5