Abstract
Purpose
To determine the impact of the loco-regional treatment modality, on the loco-regional recurrence (LRR) rates and overall survival (OS) in breast cancer patients younger than 40 years.
Methods
Data of 623 breast cancer patients younger than 40 years of age were retrospectively reviewed. Patients were stratified according to the locoregional treatment approach into three groups: the mastectomy group (M), the mastectomy followed by radiation therapy group (MRX) and the breast conservative therapy group (BCT).
Results
Median follow-up was 72 months (range, 6-180). Two hundred and nine patients were treated with BCT, 86 with MRM and 328 with MRX. The 10-year rate LRR rates according to treatment modality were: 13.4% for BCT, 15.1% for MRM and 8.5% for MRX (p 0.106). On univariate analysis, T stage (p 0.009), AJCC stage (p 0.047) and Her 2 status (p 0.001) were associated with LRR. Ten-year overall survival (OS) was 72.7% (78.5% in the BCT group, 69.8% in the MRM group and 69.8% in the MRX group, p 0.072).
On Univariate analysis, age < 35 (p 0.032), grade III (p 0.001), N3 stage (p 0.001), AJCC stage III (p 0.005), ER negative status (0.04), Her 2-status positive (0.006) and lack of chemotherapy administration (p 0.02) were all predictors of increased mortality.
Conclusion
For patients younger than 40 years of age, similar LRR and overall survival outcomes were achieved using BCT, M or MRX. Young age at diagnosis should not be used alone in recommending one loco-regional treatment approach over the others.
Similar content being viewed by others
Introduction
Breast cancer is the most common female cancer with about 11% of the cases occurring in women younger than 35 years of age (http://seer.cancer.gov/statfacts/html/breast.html). In 2020, breast cancer was the leading cause of cancer related deaths in women aged 20–39 years [1].
Young age at diagnosis is usually associated with higher incidence of nodal positivity, lymphatic vascular invasion, hormone receptor negativity, Her-2 over expression and high grade tumors [2,3,4].
Historically, several investigators reported higher locoregional failure (LRF) rates and inferior survival in young women diagnosed with breast cancer despite intensive treatments. Fowble and colleagues found an increased rates of LRF in women younger than 35 years when compared to women 35–50 and above 50 years (24% vs. 14% vs. 12%) [5]. In a pooled analysis of 10,709 patients enrolled in to 5 NSABP studies, the 12-year incidences of IBTR for women aged 49 years or younger, 50 to 59 years, and 60 years or older were 9.6%, 5.8%, and 5.6%, respectively [6].
Recommending one treatment modality over the others was never an easy decision in such patients. Breast Conserving Therapy (BCT) is associated with better quality of life and is favored by many patients in this age group; however, concerns arise with some reports demonstrating higher LRF rates in this age group with BCT when compared with mastectomy [7].
The problem becomes more evident in the developing countries where more women are diagnosed at young age [8, 9].
The aim of the current study is to evaluate the effect of different loco-regional treatment approaches on the loco-regional recurrence rates and overall survival in breast cancer patients younger than or equal to forty years of age.
Materials and methods
After obtaining IRB approval of National Cancer Institute, Cairo University and deeming informed consents unnecessary given the retrospective nature of the study, we retrospectively reviewed the medical records of 870 female patients, 40 years or younger, diagnosed with invasive breast cancer and treated between January 1st, 2005, and December 31st, 2013, at the National Cancer institute, Cairo University, Cairo, Egypt. Patients with DCIS, breast non-epithelial tumors, inflammatory breast cancer, metastatic disease at initial presentation or those who received neoadjuvant chemotherapy were excluded from this study. Only, 623 patients were included in the current analysis.
Patients were treated with either modified radical mastectomy (MRM), mastectomy followed by post mastectomy radiation therapy (MRX) or breast conserving therapy (BCT).
Treatment modality was chosen based on clinical stage, physician discretion and patient preferences.
Post mastectomy radiation was given using two tangential fields to the chest wall delivering 50 Gy/25 fractions /5 weeks; a direct supraclavicular field was added for patients who had positive nodes.
Patients who were treated with breast conserving surgery were treated with post-operative radiation therapy to the whole breast using two tangential fields delivering a dose of 50 Gy/25 fractions /5 weeks. A boost of 10 Gray/5 fractions was given to all patients with negative margins. Patients with margins ≤ 2 mm or with positive margins received a boost dose of 16 Gray/8 fractions.
Regional nodal irradiation was given to 69 (33%) patients in the BCT group and 210 (64%) patients in the MRX group.
Radiation therapy was administered to stage I patients after mastectomy in case of close surgical margins (< 2 mm), presence of N1mic disease or at physician’s discretion in patients with multiple adverse pathological features (triple negative histology, lymphovascular space invasion and metaplastic differentiation).
Statistical analysis
Continuous variables were expressed as the mean ± SD and categorical variables were expressed as a number (percentage). Percent of categorical variables were compared using Pearson’s Chi-square test or Fisher’s exact test when was appropriate. Trend of change in distribution of relative frequencies between ordinal data were compared using Chi-square test for trend. Loco-regional recurrence was defined as any ipsilateral local (in-breast, chest wall or skin) or regional (supraclavicular, infraclavicular, axillary or internal mammary nodes) recurrence. Locoregional Recurrence Free Survival (LRRFS) was calculated as the time from end of treatment to date at which Locoregional Recurrence (LRR) was detected or most recent follow-up in which Locoregional recurrence was not detected (censored). Binary logistic regression analysis was done to find independent predictors for LRR, LRRFS. A p-value < 0.05 was considered significant. All statistics were performed using SPSS 22.0 for windows (SPSS Inc., Chicago, IL, USA) and MedCalc windows (MedCalc Software bvba 13, Ostend, Belgium).
Results
Patient, treatment and tumor characteristics
The median follow up for the entire cohort was 72 months (range, 6-180). Median age at diagnosis was 37 years (range, 19–40). Eighty six (14%) patients were treated with modified radical mastectomy (MRM), 328 (53%) patients were treated with mastectomy followed by radiation therapy (MRX) and 209 (33%) patients were treated with breast conserving surgery followed by radiation therapy (BCT). Patients, tumor and treatment characteristics stratified according to the loco-regional treatment modality are summarized in Table 1.
Patients with adverse features (T4 tumors, N3 disease, AJCC stage III, GIII and hormone receptor negative tumors) were more likely to be treated with MRX (Table 1).
Regional nodal irradiation was given to 96 (33%) patients in BCT group and 210 (64%) patients in the MRX group.
Three hundred and twelve (95%) patients in the MRX group received adjuvant chemotherapy compared to 74 (86%) and 192 (92%) in the MRM and BCT groups, respectively (p 0.013).
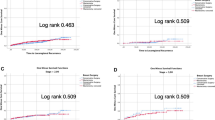
Locoregional recurrence for the entire population
Seventy (11%) patients experienced loco-regional recurrence in the entire cohort. The 10-year rate of LRR was 15.1%, 8.8% and 13.4% in the MRM MRX and BCT groups, respectively (p 0.106).
On univariate analysis, T stage (p 0.009), AJCC stage (p 0.047) and Her 2 status (p 0.001) were shown to have statistically significant association with LRR. Other factors included in the univariate analysis are shown in Table 2.
On multivariate analysis, T3 disease (HR 0.334, CI 0.143–0.784, p 0.012) was the only factor that had independent association with lowered loco-regional recurrence free survival Table 3.
Distant metastases for the entire population
One hundred and sixty-eight patients (27%) developed distant metastases in the entire group. The 10-year rate of distant metastasis was 32.6%, 29.6% and 20.6% for patients treated with MRM, MRX and BCT, respectively (p = 0.057).
On univariate analysis, loco-regional treatment strategy (p 0.033), age group (p 0.021), tumor grade (p 0.001), T stage (p 0.019), N stage (p 0.004), AJCC stage (p 0.005) and Her 2 status (p 0.006) all had statistically significant impact on DM rate. All factors included in the univariate analysis are presented in Table 2.
On multivariate analysis, N3 disease (HR 1.827, CI 1.168–2.858, p 0.008) and MRM (HR 1.434, CI 1.005–2.047, p 0.047) were associated with increased hazard of distant metastases Table 3.
Overall survival
Actuarial 10-year overall survival was 72.7% for the entire population. The difference in the 10-year OS among the three treatment groups was not statistically significant (69.8% for MRM, 69.8% for MRX and 78.5% for BCT, p 0.072).
On univariate analysis (Table 2), factors that had statistically significant correlation with OS were age group (p 0.032), grade (p 0.001), N stage (p 0.001), AJCC stage (p 0.005), ER status (0.04), Her 2 status (0.006) and chemotherapy administration (p 0.02).
On Multivariate analysis chemotherapy administration (HR 0.478, CI 0.293–0.780, p 0.003) and age above 35 years were associated with lowered mortality Table 3.
Patients with stage I disease
Patients with stage I disease (n = 46) were treated with BCT (n = 20), MRM (n = 12) or MRX (n = 14). On univariate analysis, the loco-regional treatment modality did not have a statistically significant effect on the 10-year LRR rate, DM rate or OS. Loco-regional recurrence rate was 41.7% in the MRM group, 7.1% in the MRX group and 20% in the BCT group (p 0.101). The 10-year rate of distant metastases was 33.3% in the MRM group, 35.7% in the MRX group and 15% in the BCT group (p 0.321). The 10-year OS rate was 66.7% in the MRM, 64.3% in the MRX group and 85%% in the BCT group (p 0.321). Other factors included in the univariate analysis are presented in Table 4.
Patients with stage II disease
Patients with stage II disease (n = 260) were treated with MRM (n = 51), MRX (n = 111) and BCT (n = 98). On univariate analysis, no statistically significant difference was found in the LRR rate when patients were stratified according to the locoregional treatment modality. The 10-year LRR rate was 9.8% in the MRM group, 11.7% in the MRX group and 12.2% in the BCT group (p 0.201). Other factors found to have statistically significant correlation with LRR were Her-2 status (p 0.035) and chemotherapy administration (p 0.014).
Fifty three patients (20.3%) developed distant metastases at 10 years. No statistically significant difference in the rate of distant metastases (DM) was found when patients were stratified according to the locoregional treatment modality (27.5% in the MRM group, 22.5% in the MRX group and 14.3% in the BCT group, p 0.127).
The 10-year OS rate was 79.2%. Factors affecting OS on univariate analysis were grade (p 0.001), N stage (p 0.030), Her 2 status (p 0.001) and chemotherapy administration (p 0.006). All factors examined in the univariate analysis are presented in Table 5.
Patient with stage III disease
In patients with stage III disease (n = 317), twenty three patients were treated with MRM, 203 patients with MRX and 91 patients with BCT. The locoregional treatment strategy did not affect the rate of LRR (8.7% for MRM, 10.3% for MRX and 7.7% for BCT, p 0.766). On univariate analysis, Her-2 status was the only factor that had a marginally significant effect on the 10-year rate of LRR (p 0.058).
The 10-year rate of distant metastases was 32.5%. The Locoregional treatment modality did not have a significant impact on the rate of distant metastases (43.5% in the MRM group, 33% in the MRX group and 28.6% in the BCT group, p 0.381). The rate of distant metastases was significantly affected by tumor grade (p 0.037), Her-2 status (p 0.002) and chemotherapy administration (p 0.005).
The 10-year OS rate was 76.2% for patients with stage III disease. A non-significant difference in the OS was observed based on the Locoregional treatment approach (52.2% for MRM, 66.5% for MRX and 72.5% for BCT, p 0.168). Factors that were found to significantly affect OS on univariate analysis were grade (p 0.001), N stage (p 0.30), Her 2 status (p 0.001) and chemotherapy administration (p 0.006). All factors included in the univariate analysis are presented in Table 6.
Discussion
In the present study, 623 patients younger than or equal to 40 years of age with breast cancer were retrospectively studied to detect the impact of different treatment modalities on the rate of LRR, DM and OS. Unlike previous reports, this study identified three groups of patients based on the loco-regional treatment approach; the breast conserving surgery followed by radiation group (BCT), the modified radical mastectomy group (MRM) and the mastectomy followed by post mastectomy radiation group (MRX).
In our study the incidence of 10-year LRR among all patients was 11.2%. This incidence is slightly higher than what has been published in the POSH observational cohort study which reported a LRR incidence of 4.8% among 2882 women of 18 to 40 years with breast cancer treated in the UK between 2000 and 2008 [10]. Another study from the Department of Radiation Oncology, The University of Texas M. D. Anderson cancer center, reported an LRR rate of 19.8% among 652 young patients with breast cancer treated between years 1973 and 2006 [11]. The lower rates of LRR in the current study and the POSH analysis as compared to the M.D. Anderson results might be explained by the more contemporary patient population and treatment strategies adopted in both studies.
In the current report, the rate of mastectomy was 66% vs. 34% for breast conservation. This could be explained by the higher percentage of patients with T2-3 tumors (58%) and also reflecting both patient and physician preference while treating this young age group. However, similar LRR rates were found for the three treatment groups implying no clinical advantage in choosing mastectomy over breast conservation for this group of patients. This is consistent with data published by other investigators. Plichta, et al. studied 584 women aged ≤ 40 years with breast cancer. Median age was 37 years, and median follow-up was 124 months. When stratified by lumpectomy versus mastectomy, there was no statistically significant difference in the LRF rates. Lumpectomy LRF rates were 1% at 5 years and 4% at 10 years. Mastectomy LRF rates were 3.5% at 5 years and 8.7% at 10 years. Unfortunately, there were no clear data about the percentage of patients who received post-mastectomy radiatiotherapy [12].
Kheirelseid et al. [13] prospectively analyzed data of patients with breast cancer younger than 40 years of age, treated at Galway University hospital, Department of Surgery from 1989 to 2009. They compared the LRF rates in their patients based on the surgical treatment they received. No statistically significant difference in LRF was determined comparing those who underwent mastectomy to those who had BCT.
In our study, higher incidence of LRF was detected in the patients who had hormone receptor negative tumors (10% vs. 5.6% for patients with positive hormone receptors). Among patients with negative hormone receptors, there was a statistically significant difference in the rates of LRF when stratified according to the locoregional treatment modality (17.8% for MRM vs. 7.3% for MRX and 11.6% for BCT, p 0.04). The clinical implication could be an essential role for radiation therapy in this subset of patients.
We were not able to demonstrate any significant association between the locoregional treatment strategy and overall survival either on univariate or multivariate analysis in the current analysis. Five year OS was 81.4% in the BCT group vs. 72.8% in the MRM group vs. 74.8% in the MRX group (p 0.1).
In the recently published POSH analysis, mastectomy patients had a significantly worse OS compared with BCS (HR, 0.53; 95% CI 0.45–0.62; P < 0.001), however, on multivariate analysis the difference was no longer significant (HR, 0.79; 95% CI 0.61–1.03; P 0.081) [14].
The inherent nature of this retrospective analysis carries the risk of selection bias. Furthermore, we were not able to perform further subset analysis due to the relatively small number of recurrences.
Conclusion
For patients younger than 40 years of age, similar LRR and overall survival outcomes were achieved using BCT, M or MRX. Young age at diagnosis should not be used alone in recommending one loco-regional treatment approach over the others.
Availability of data and materials
Data set used by authors to generate the results is available upon reasonable request.
Abbreviations
- AJCC:
-
American Joint Committee on Cancer
- BCT:
-
Breast Conservative Therapy
- CI:
-
Confidence Interval
- DCIS:
-
Ductal Carcinoma Insitu
- DM:
-
Distant Metastasis
- ER:
-
Estrogen Receptor
- HER2:
-
Human Epdiermal Growth Factor Receptor 2
- HR:
-
Hazard Ratio
- IBTR:
-
Ipsilateral Breast Tumor Recurrence
- IRB:
-
Institutional Review Board
- LRF:
-
Loco-regional Failure
- LRR:
-
Loco-regional Recurrence
- LRRFS:
-
Loco-regional Recurrence Free Survival
- M:
-
Mastectomy
- MRM:
-
Modified Radical Mastectomy
- MRX:
-
Mastectomy + Radiotherapy
- N:
-
Node
- NSABP:
-
National Surgical Adjuvant Breast and Bowel Project
- OS:
-
Overall survival
- SD:
-
Standard Deviation
- T:
-
Tumor
- UK:
-
United Kingdom
References
Siegel R, Miller K, Wagel N, et al. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17–48.
Bonnier P, Romain S, Charpin C, et al. Age as a prognostic factor in breast cancer: relationship to pathologic and biologic features. Int J Cancer. 1995;62(2):138–44.
Colleoni M, Rotmensz N, Robertson C, et al. Very young women (< 35 years) with operable breast cancer: features of disease at presentation. Ann Oncol. 2002;13(2):273–9.
Gonzalez-Angulo AM, Broglio K, Kau SW, et al. Women age < or = 35 years with primary breast carcinoma: disease features at presentation. Cancer. 2005;103(12):2466–72.
Fowble BL, Schultz DJ, Overmoyer B, et al. The influence of young age on outcome in early stage breast cancer. Int J Radiat Oncol Biol Phys. 1994;30(1):23–33.
Anderson SJ, Wapnir I, Dignam JJ, et al. Prognosis after ipsilateral breast tumor recurrence and locoregional recurrences in patients treated by breast-conserving therapy in five national surgical adjuvant breast and bowel project protocols of nodenegative breast cancer. J Clin Oncol. 2009;27(15):2466–73.
Goldhirsch A, Winer EP, Coates AS, et al. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the primary therapy of early breast Cancer 2013. Ann Oncol. 2015;24:2206–23.
Villarreal-Garza C, Aguila C, Magallanes-Hoyos MC, et al. Breast cancer in young women in Latin America: an unmet, growing burden. Oncologist. 2013;18:1298–306.
Wang K, Ren Y, Li H, et al. Comparison of clinicopathological features and treatments between young (40 years) and older (> 40 years) female breast cancer patients in West China: a retrospective, epidemiological, multicenter, case only study. PLoS ONE. 2016;11:e0152312.
Maishman T, Cutress RI, Hernandez A, et al. Local recurrence and breast oncological surgery in Young Women with breast Cancer: the POSH observational cohort study. Ann Surg. 2017;266(1):165–72.
Beadle BM, Woodward WA, Tucker SL, et al. Ten-year recurrence rates in young women with breast cancer by locoregional treatment approach. Int J Radiat Oncol Biol Phys. 2009;73(3):734–44.
Plichta JK, Rai U, Tang R, et al. Factors Associated with Recurrence Rates and Long-Term Survival in Women diagnosed with breast Cancer ages 40 and younger. Ann Surg Oncol. 2016;23(10):3212–20.
Kheirelseid EH, Boggs JM, Curran C, et al. Younger age as a prognostic indicator in breast cancer: a cohort study. BMC Cancer. 2011;11:383.
Copson E, Eccles B, Maishman T, et al. Prospective observational study of breast cancer treatment outcomes for UK women aged 18–40 years at diagnosis: the POSH study. J Natl Cancer Inst. 2013;105(13):978–88.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
RB, YA, TM, MI & AH: data collection and material preparation. MB: data analysis. RB, YA & ME: writing the first draft of the manuscript. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. All authors contributed to the study conception and design.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board of the National Cancer Institute, Cairo University approved this study. Consent to participate was not required given the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Boutrus, R.R., Abdelazim, Y.A., Mohammed, T. et al. The impact of loco-regional treatment modality on the outcomes in breast cancer patients younger than forty years of age. BMC Cancer 24, 599 (2024). https://doi.org/10.1186/s12885-024-12325-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12325-3