Abstract
Background
Papillary thyroid carcinoma (PTC) is the most frequent malignant tumor in thyroid carcinoma. The aim of this study was to explore the risk factors associated with central lymph node metastasis in papillary thyroid microcarcinoma (PTMC) and establish a nomogram model that can assess the probability of central lymph node metastasis (CLNM).
Methods
The clinicopathological data of 377 patients with cN0 PTMC were collected and analyzed from The Second Affiliated Hospital of Fujian Medical University from July 1st, 2019 to December 30th, 2021. All patients were examined by underwent ultrasound (US), found without metastasis to central lymph nodes, and diagnosed with PTMC through pathologic examination. All patients received thyroid lobectomy or total thyroidectomy with therapeutic or prophylactic central lymph node dissection (CLND). R software (Version 4.1.0) was employed to conduct a series of statistical analyses and establish the nomogram.
Results
A total of 119 patients with PTMC had central lymph node metastases (31.56%). After that, age (P < 0.05), gender (P < 0.05), tumor size (P < 0.05), tumor multifocality (P < 0.05), and ultrasound imaging-suggested tumor boundaries (P < 0.05) were identified as the risk factors associated with CLNM. Subsequently, multivariate logistic regression analysis indicated that the area under the receiver operating characteristic (ROC) curve (AUC) of the training cohort was 0.703 and that of the validation cohort was 0.656, demonstrating that the prediction ability of this model is relatively good compared to existing models. The calibration curves indicated a good fit for the nomogram model. Finally, the decision curve analysis (DCA) showed that a probability threshold of 0.15–0.50 could benefit patients clinically. The probability threshold used in DCA captures the relative value the patient places on receiving treatment for the disease, if present, compared to the value of avoiding treatment if the disease is not present.
Conclusion
CLNM is associated with many risk factors, including age, gender, tumor size, tumor multifocality, and ultrasound imaging-suggested tumor boundaries. The nomogram established in our study has moderate predictive ability for CLNM and can be applied to the clinical management of patients with PTMC. Our findings will provide a better preoperative assessment and treatment strategies for patients with PTMC whether to undergo central lymph node dissection.
Similar content being viewed by others
Introduction
Papillary thyroid carcinoma is the most frequent malignant tumor in thyroid carcinoma. The clinic-biological behavior of PTC is relatively inert, with a 10-year survival of over 90% after standard management [1, 2]. According to the definition by World Health Organization (WHO), PTMC is defined as a papillary thyroid carcinoma less than 10 mm [3]. Increasing awareness of health examinations has prompted more people to take regular medical checkups, which has enabled PTMC to be detected at an early stage rather than by the time symptoms emerge. At the same time, the high-resolution ultrasound makes it possible to detect microscopic tumors that would otherwise be difficult to observe and makes the morphology of tumors clearer, reducing the probability of misdiagnosis and underdiagnosis. Thanks to the popularity of health examinations and the application of examination devices such as high-resolution ultrasound, more and more patients with asymptomatic thyroid carcinoma are detected in the early stage. In recent years, the incidence rate of PTC is obviously increasing worldwide. It is reported that the incidence of thyroid cancer in China also continues to grow, with an annual growth rate of about 20% [4]. Not only in China, but also in other countries the incidence of thyroid cancer is increasing year by year. A report from 2015 American Thyroid Association (ATA) Management Guidelines suggested that the incidence of thyroid cancer has increased threefold in the past 30 years [5]. In South Korea, the incidence of thyroid cancer increased by an average of 24.2% per year from 1999 to 2010 [6]. Although PTMC exhibits a slow progression with a relatively better prognosis, the lymph node metastasis occurs frequently in the early stages, especially the CLNM, which has been considered to be a risk for distant metastasis and recurrence [7].
The TNM classification of malignant tumors is a globally accepted standard for classifying the anatomical extent of the spread of malignant tumors. Most common tumors have their own TNM classification, and papillary thyroid cancer is no exception. According to the TNM system, patients with PTMC are labeled as cN1 or cN0 for lymph node positive or negative, respectively, based on the results of physical examination or imaging. Thyroidectomy combined with therapeutic lymph node dissection, including CLND, has now become a frequent initial surgical strategy for patients with clinical lymph node-positive (cN1) PTMC [8]. Despite this, for patients with no preoperatively detected cervical lymph node metastases, some experts advocate prophylactic central lymph node dissection (pCLND), while other clinicians believe it is unnecessary. Therefore, it remains a hot topic of debate whether to perform pCLND in PTMC patients without clinical lymph node-positive (cN0). According to ATA guidelines (version: 2015) and National Comprehensive Cancer Network (NCCN) guidelines (version: 2022), pCLND is not recommended as a routine surgical procedure in cN0 PTMC patients without high risk factors [5, 9]. Nevertheless, the necessity of pCLND for PTMC patients with cN0 has been positively highlighted in multiple guidelines from some different countries [10, 11]. Given that PTMC patients is frequently found central region lymph nodes involvement and pCLND is considered helpful to the risk reduction of recurrence and second operation, the Chinese Society of Clinical Oncology (CSCO) guidelines (version: 2018) recommended performing pCLND after a comprehensive assessment of the patient's surgical risks and benefits [12]. Although various studies committed to find the risk factors for CLNM, it is still lack of consensus and standard criterion to instruct clinicians on the indications for CLND. Therefore, it is significant to construct a prediction model to assess the lymph node involvement preoperatively to further realize the personalized precision treatment.
In this study, we aimed to establish a prediction model to assess the conditions of PTMC patients preoperatively and instruct clinicians to provide optimal surgical strategies for PTMC patients with cN0. Since existing guidelines and treatment protocols do not explicitly mention the necessity of CLND for PTMC patients with cN0 and there is no quantitative criterion to guide clinicians on the circumstances under which CLND is necessary, the decision-making resulting from such pros and cons judgments is subjective, which may lead to irregularities in treatment. Our study aims to develop a nomogram-based CLNM risk model for PTMC to help with the decision on the surgery choice, utilizing clinical data from our medical center and focusing on five independent factors: age, gender, multifocality, tumor boundary, and tumor size.
Methods
Ethics approval and informed consent
This research protocol was approved by the Ethics Committee of Second Affiliated Hospital of Fujian Medical University (2022 Ethical Review No. 481) and was conducted in accordance with the Declaration of Helsinki, and informed consent was obtained from all subjects or their legal guardians.
General data
A total of 377 patients with PTMC enrolled in the Thyroid and Breast Surgery of Second Affiliated Hospital of Fujian Medical University from July 2019 to December 2021 were recruited in the current study. All data were extracted from the electronic medical record system, and no personally identifiable information was displayed in accordance with the principles of patient privacy protection. The completed information was provided in Supplemental Table 1. The PTMC diagnosis of all samples was confirmed through postoperative pathology.
Inclusion criteria were as follows:
-
Patients with completed clinical and pathologic information records.
-
Patients who underwent ultrasound examination before operation in our hospital without clinical abnormal findings in central lymph nodes by physical and ultrasound examination.
-
Initial thyroidectomy, intraoperative frozen section and postoperative paraffin pathological diagnosis of PTMC, and surgical range including total CLND.
-
Patients who were operated by the same medical team.
The exclusion criteria were as follows:
-
Other types of thyroid carcinoma (thyroid follicular carcinoma, thyroid medullary carcinoma, and undifferentiated thyroid carcinoma et al.).
-
Missing information of medical record and US reports of our hospital.
-
History of head/neck surgery or radiology, history of other malignancy and metastatic thyroid cancer.
-
PTMC patients with distant metastasis.
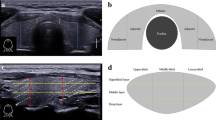
Moreover, the US reports were issued by more than two US physicians, and the ultrasonic characteristic records included position, boundary situation, microcalcification situation, the length/width ratio, and the peripheral blood supply of tumor. In addition, all specimens were examined by two or more pathologic physicians from Second Affiliated Hospital of Fujian Medical University. Pathological characteristics analysis included pathological type of tumor, size, multifocality (more than one lesion in unilateral thyroid lobe), and central lymph node metastasis.
Surgical strategy
Surgeries were conducted by specialists from the same medical team and who perform at least 100 surgeries annually. All patients received thyroid lobectomy or total thyroidectomy with therapeutic or prophylactic CLND. The upper, lower, and external boundaries of CLND were lower edge of hyoid bone, upper edge level of the brachiocephalic artery and internal carotid artery sheath. The posterior boundary was anterior fascia, including all paratracheal, pretracheal and prelaryngeal lymph nodes and adipose tissues [12].
Statistical analysis
We conducted this study to identify the relationship between clinical features and central lymph nodes (CLN) involvement in PTMC patients. A series of continuous statistical calculations were performed by using R software (Version 4.1.0; http://www.r-project.org). The chi-square test and Mann–Whitney U test was adopted for univariate analysis. Subsequently, the all data from our medical center was randomly divided into two cohorts for cross-validation: 70% for a training cohort and 30% for an internal testing cohort. The least absolute shrinkage and selection operator (LASSO) regression analysis is a regression analysis method that executes both variable selection and regularization to improve the accuracy of forecasting and the explainability of the statistical model. In order to reduce redundant factors and obviate model overfitting, LASSO regression analysis was employed to screen out the optimal variables as potential risk factors for this prediction model [13]. Variables of which the p-value < 0.05 from the LASSO regression were applied to multivariate logistic regression and a subsequent nomogram was constructed. The prediction efficiency of the novel predictive model was evaluated through the receiver operating characteristic (ROC) curve, the calibration curve, and the area under the ROC curve (AUC) which is also known as concordance index (C-index). Notably, C-index is specifically used for the quantification of the ability to discriminate between outcomes. After that, the net benefit at disparate threshold probabilities were quantified to further identify the clinic value of the model by use of the method of DCA. P < 0.05 was considered as statistically significant.
Results
Clinicopathological characteristics of PTMC patients
A total of 377 cases diagnosed with non-distance-metastatic histologically confirmed PTMC in Second Affiliated Hospital of Fujian Medical University from 2019 to 2021 were recruited in the current study. The ratio of male to female was approximately 1:3.60, which is similar to other studies on PTMC. Approximately 81% of the PTMC patients were < 55 years old. The majority of the specimens were solitary tumor. Approximately 68.44% of the patients were lymph node negative. The clinicopathological characteristics of the samples involved in are summarized in Table 1.
Selection of potential predictors
The univariate analysis was used to identify the relationship between the central lymph node metastasis and 9 risk factors, involving age, gender, multifocality, tumor location, tumor boundary, tumor aspect ratio, microcalcification, tumor size, and peripheral blood supply of tumors. According to the results of univariate analysis, five variables were identified to be significantly related to CLNM, including age, gender, multifocality, tumor boundary and tumor size (Table 2). Subsequently, to avoid the affection of confounding factors, the LASSO regression analysis was performed to confirm the final variables. The LASSO coefficient overview of the selected factors was showed in Fig. 1a and 5-fold cross-validation results were produced to identify the preferred value of the penalty parameter λ (λ = 0.002157022) (Fig. 1b). As a result, the finally selected potential predictors were age, gender, multifocality, tumor boundary and tumor size.
Establishment and validation of the prediction model
All data were randomly divided into two cohorts for cross-validation purposes to ensure the model's generalizability, which consisted of the training cohort (n = 269, 70% of all cases from our center) and the validation cohort (n = 108, 30% of all cases from our center). The features of 5 variables between training and validation cohorts were summarized in Table 3. To gain a more complete understanding of the relationship between the CLNM and these predictors, the multivariable logistic regression analysis was further performed and a prediction model was subsequently established. The results were visualized in the form of a nomogram, which is easier to apply in the clinical practice (Fig. 2). After that, the ROC curve and the calibration curve were performed to evaluate the prediction efficiency of the nomogram model. As shown in Fig. 3, the AUC was 0.703 for the training cohort and it was 0.656 for the validation cohort. The C-index of this model in the training cohort was 0.703 (95%CI: 0.640–0.731), and the one in validation cohort was 0.656 (95%CI: 0.672–0.707). The calibration curve of CLNM risk nomogram in PTMC indicated a good consistency in both training and validation cohorts, and all the mean absolute error < 0.05, which suggested the good fit of the predictor model (Fig. 4). The probability threshold used in DCA captures the relative value the patient places on receiving treatment for the disease, if present, compared to the value of avoiding treatment if the disease is not present. Consequently, the DCA was conducted to showed that applying this prediction model has benefited patients when the threshold probability is in the range of 0.15–0.50 (Fig. 5).
According to our study, CLNM may be related to several factors, including age, gender, tumor size, tumor multifocality, and ultrasound imaging-suggested tumor boundaries. The nomogram established in our study has moderate predictive ability for CLNM and can be applied to the clinical management of patients with PTMC.
Discussion
Thanks to the development of high-resolution ultrasound, fine-needle aspiration biopsy (FNAB) as well as cytological and molecular diagnosis, more and more asymptomatic PTMC is being diagnosed at early stage [14]. Although the incidence of PTMC continues to rise, mortality rates have remained largely stable, with a 10-year survival rate of 94.6% [1, 15]. As a result, there is a growing debate about whether PTMC is over-diagnosed and over-treated. Some academics proposed that active surveillance (AS) was an effective management for PTMC, which meant surgery could be performed after the tumor progression was found during the monitoring process [16]. Based on active surveillance in low-risk PTMC, Ito et al. found that after 10 years of follow-up, only 8% of patients had a tumor size increase of more than 3 mm and only 3.8% had clinically confirmed lymph node metastases, and these patients still had a good prognosis with delayed surgery [2]. Thus, AS was suggested as an alternative option for the treatment of low-risk PTMC patients. A lot of academics from the United States, Italy and other countries have come to the same conclusion, believing that AS is a viable and safe alternative to immediate surgery for patients with cN0 PTMC [17,18,19]. Although many studies support this idea, there is still disagreement on the need to individualize patient care based on risk factors and patient preferences.
Currently, most academics believe that CLND is necessary for PTMC patients with cN1, but pCLND remains controversial for PTMC patients with cN0. On the one hand, ATA guidelines (version: 2015) and NCCN guidelines (version: 2022) suggest that pCLND is not recommended as a routine surgical procedure in cN0 PTMC patients without high risk factors [5, 9]. Some studies have shown that pCLND not only failed to improve the prognosis of patients, but also increased the risk of laryngeal return nerve injury and permanent hypoparathyroidism [5, 20]. On the other hand, some guidelines from different countries in Asia emphasized actively the significance of the routine pCLND for PTMC patients with cN0 [21]. It is helpful to reduce the rate of local recurrence and at the same time confirm the stage of thyroid cancer to provide guidance for subsequent treatments in terms of thyroid-stimulating hormone (TSH) suppression and radioactive iodine (RAI) therapy. PTMC patients were prone to develop CLNM at early stage [22]. In addition, it has been found that a second surgery in patients with post-operative recurrence is more difficult and has an increased probability of complications due to adhesions and altered natural anatomy [23]. Therefore, pCLND is significant to reduce the risk of reoperation for PTMC patients. Furthermore, ultrasound is the main way to evaluate the central lymph node involvement in PTMC patients preoperatively, but it has some limitations in clinical practice. The study conducted by YU et al. indicated that ultrasound has poor sensitivity in evaluating preoperative CLNM in patients with PTMC, ranging from 21.6%-38% [24]. Additionally, Kim and colleagues found that the false negative rate was 30% for preoperative ultrasound assessment of CLNM [25]. Consistent with this observation, in our study, all patients enrolled were cN0 PTMC patients, but 31.56% of them still had CLNM confirmed by the postoperative pathological results. While ultrasound has limitations, it remains a valuable non-invasive tool, and improving its accuracy through technological advancements or combined modalities could be an area for future research.
In current study, a total of 377 cN0 PTMC patients admitted to Thyroid and Breast Surgery of Second Affiliated Hospital of Fujian Medical University were enrolled to explore the risk factors associated with CLNM, resulting that gender, age, multifocality, tumor boundary and tumor size were the risk factors for CLNM in cN0 PTMC patients. Similarly, Pisanu A et al. identified gender, age, maximum tumor diameter, multifocality of the tumor, and vascular invasion as risk factors for the development of CLNM in patients with PTMC [26]. Additionally, the study conducted by YU X and colleagues indicated that male patients, age less than 45 years, multifocality of tumor, and tumor size larger than 5 mm in diameter were risk elements for CLNM [24]. In addition, Wei X et al. found that tumor location, aspect ratio and microcalcifications on ultrasound were associated with CLNM of PTMC patients [27]. The study by Gao Y et al. revealed that microcalcifications and poorly defined tumor boundaries were risk factors relevant to the development of CLNM in patients with PTMC [28]. In conclusion, some of the risk factors associated with CLNM in PTMC patients mentioned in other studies were not confirmed in this study such as tumor location, aspect ratio and microcalcifications, which may be related to the clinical experience of the ultra-sonographers and different ultrasound equipment.
The nomogram can make the prediction model simple and visualize the results in a graphical formal, which is widely used clinically in a variety of tumorigenesis and prognosis prediction, including breast cancer [29], gastric cancer [30], prostate cancer [31] and so on. However, most of the current nomograms of CLNM prediction in PTMC patients were established on the basis of postoperative pathological characteristics, and few models were proposed to make predictions about the CLNM preoperatively or intraoperatively [8, 32]. In current study, the nomogram was finally established based on clinical information, preoperative ultrasound examination and intraoperative frozen pathological characteristics, which is of great significance in the decision of surgical strategy for PTMC patients preoperatively. According to the nomogram risk model, the AUC value was 0.703 for the training set and 0.663 for the validation set, indicating that the model has moderate predictive efficacy. The calibration curves showed that the mean error between the actual probability of CLNM in PTMC patients and the predicted probability of this nomogram was less than 0.05, suggesting a good fit of the model. Ultimately, we evaluated the impact of the model on clinical decision making through clinical decision curves, meaning whether or not the patient would actually receive a clinical benefit. It was revealed that the model was able to contribute to improved clinical decisions and benefit patients within a certain threshold probability range (0.15–0.50). Although the nomogram shows promise, its effectiveness in clinical practice may need to be validated in a variety of settings and populations to ensure its robustness and generalizability. In summary, a prediction model for the development of CLNM in patients with cN0 PTMC was established based on clinical, ultrasound and intraoperative frozen pathological features. An aggressive pCLND was recommended to reduce the risk of tumor recurrence when the total score of a PTMC patients is higher than 120 based on the nomogram. Conversely, pCLND is not recommended when the total score of a PTMC patient is less than 120, which can reduce surgical complications. It is worth mentioning that for whether or not to perform pCLND, a balance needs to be struck between the benefits of pCLND and the possible reduction in quality of life due to surgical complications. In addition, the preference for AS and pCLND should be a shared decision between the patient and the surgeon. Therefore, adequate preoperative education and shared decision-making also play an important role in the management of pCLND.
However, there are still several limitations to this study. Firstly, as this study is a retrospective analysis, there is inevitably selective bias. Indeed, a number of other potential confounders, such as genetic mutations, environmental factors, and patients' lifestyles, which were not included in the study, may have influenced the results. Additionally, the pathological features and genotypes of FNA sample preoperatively should be further added into the future prediction model. Secondly, our model was only applied to cN0 PTMC, not for other subtypes of thyroid cancer. It is also important to incorporate the nomogram into a wider clinical framework, including endocrinologists, surgeons, pathologists, and even patient navigators, to ensure comprehensive care. Thirdly, this study was only conducted with single-center data from our medical center and lack of the external validation. Hence, subsequent evaluation with follow-up data from multicenter is indicated. Furthermore, it is suggested that future research may include prospective studies, the integration of genetic profiling, and the development of personalized medicine approaches for a more comprehensive investigation to guide clinical decision-making choices.
In conclusion, an effective nomogram for evaluating cervical central lymph node metastasis of cN0 PTMC was established based on the clinicopathological data from our medical center. Five variables were identified to be significantly related to CLNM, including age, gender, multifocality, tumor boundary and tumor size. For cN0 PTMC patients with a score higher than 120 according to the nomogram, clinicians can consider performing pCLND and making strict postoperative assessments.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
Yu X, Wan Y, Sippel R, Chen H. Should all papillary thyroid microcarcinomas be aggressively treated? An analysis of 18,445 cases. Ann Surg. 2011;254(4):653–60.
Ito Y, Miyauchi A, Oda H. Low-risk papillary microcarcinoma of the thyroid: a review of active surveillance trials. Eur J Surg Oncol. 2018;44(3):307–15.
Sobin L. Histological typing of thyroid tumours. Histopathology. 1990;16(5):513.
Health Commission Of The People’s Republic Of China N. National guidelines for diagnosis and treatment of thyroid cancer 2022 in China (English version). Chin J Cancer Res. 2022;34(3):131–50.
Haugen B, Alexander E, Bible K, Doherty G, Mandel S, Nikiforov Y, Pacini F, Randolph G, Sawka A, Schlumberger M, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1–133.
Peinado H, Alečković M, Lavotshkin S, Matei I, Costa-Silva B, Moreno-Bueno G, Hergueta-Redondo M, Williams C, García-Santos G, Ghajar C, et al. Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through MET. Nat Med. 2012;18(6):883–91.
Liu L, Liang J, Li J, Liu X, Jiang L, Long J, Jiang Y, Wei Z. The incidence and risk factors for central lymph node metastasis in cN0 papillary thyroid microcarcinoma: a meta-analysis. Eur Arch Otorhinolaryngol. 2017;274(3):1327–38.
Lu S, Zhao R, Ni Y, Ding J, Qiu F, Peng Y, Pan G, Wu F, Zhang Y, Shi J, et al. Development and validation of a nomogram for preoperative prediction of cervical lymph node involvement in thyroid microcarcinoma. Aging (Milano). 2020;12(6):4896–906.
Haddad R, Bischoff L, Ball D, Bernet V, Blomain E, Busaidy N, Campbell M, Dickson P, Duh Q, Ehya H, et al. Thyroid Carcinoma, Version 2.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Cancer Netw. 2022;20(8):925–51.
Hyun S, Song H, Kim S, Nam S, Roh J, Han M, Choi S. Impact of combined prophylactic unilateral central neck dissection and hemithyroidectomy in patients with papillary thyroid microcarcinoma. Ann Surg Oncol. 2012;19(2):591–6.
Kim S, Woo J, Lee J, Park I, Choe J, Kim J, Kim J. Prophylactic central neck dissection might not be necessary in papillary thyroid carcinoma: analysis of 11,569 Cases from a Single Institution. J Am Coll Surg. 2016;222(5):853–64.
Lin Y, Huang H, Guo Y, Jentzen W, Rosenbaum S, Kühl H. Chinese Society of Clinical Oncology (CSCO) diagnosis and treatment guidelines for persistent/recurrent and metastatic differentiated thyroid cancer 2018. Chin J Cancer Res. 2019;31(1):99-116.
Friedman JH, Hastie T, Tibshirani R. Regularization paths for generalized linear models via coordinate descent. J Stat Softw. 2010;33(1):1–22.
Chéreau N, Buffet C, Trésallet C, Tissier F, Leenhardt L, Menegaux F. Recurrence of papillary thyroid carcinoma with lateral cervical node metastases: Predictive factors and operative management. Surgery. 2016;159(3):755–62.
Cao Y, Zhang T, Li B, Qu N, Zhu Y. Prognostic evaluation model for papillary thyroid cancer: a retrospective study of 660 cases. Gland Surg. 2021;10(7):2170–9.
Shaha A, Tuttle R. Editorial: Risk of disease progression during active surveillance of papillary thyroid cancer. Surgery. 2018;163(1):53–4.
Tuttle R, Fagin J, Minkowitz G, Wong R, Roman B, Patel S, Untch B, Ganly I, Shaha A, Shah J, et al. Natural history and tumor volume kinetics of papillary thyroid cancers during active surveillance. JAMA otolaryngol Head Neck Surg. 2017;143(10):1015–20.
Haugen B. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: what is new and what has changed? Cancer. 2017;123(3):372–81.
Molinaro E, Campopiano M, Pieruzzi L, Matrone A, Agate L, Bottici V, Viola D, Cappagli V, Valerio L, Giani C, et al. Active Surveillance in Papillary Thyroid Microcarcinomas is Feasible and Safe: Experience at a Single Italian Center. J Clin Endocrinol Metab. 2020;105(3):e172–80.
Chen L, Wu Y, Lee C, Chen H, Loh E, Tam K. Prophylactic Central Neck Dissection for Papillary Thyroid Carcinoma with Clinically Uninvolved Central Neck Lymph Nodes: a systematic review and meta-analysis. World J Surg. 2018;42(9):2846–57.
Takami H, Ito Y, Okamoto T, Yoshida A. Therapeutic strategy for differentiated thyroid carcinoma in Japan based on a newly established guideline managed by Japanese Society of Thyroid Surgeons and Japanese Association of Endocrine Surgeons. World J Surg. 2011;35(1):111–21.
Zhang L, Wei W, Ji Q, Zhu Y, Wang Z, Wang Y, Huang C, Shen Q, Li D, Wu Y. Risk factors for neck nodal metastasis in papillary thyroid microcarcinoma: a study of 1066 patients. J Clin Endocrinol Metab. 2012;97(4):1250–7.
Vasica G, O’Neill C, Sidhu S, Sywak M, Reeve T, Delbridge L. Reoperative surgery for bilateral multinodular goitre in the era of total thyroidectomy. Br J Surg. 2012;99(5):688–92.
Yu X, Song X, Sun W, Zhao S, Zhao J, Wang Y. Independent Risk factors predicting central lymph node metastasis in papillary thyroid Microcarcinoma. Horm Metab Res. 2017;49(3):201–7.
Kim E, Park J, Son K, Kim J, Jeon S, Na D. Preoperative diagnosis of cervical metastatic lymph nodes in papillary thyroid carcinoma: comparison of ultrasound, computed tomography, and combined ultrasound with computed tomography. Thyroid. 2008;18(4):411–8.
Pisanu A, Reccia I, Nardello O, Uccheddu A. Risk factors for nodal metastasis and recurrence among patients with papillary thyroid microcarcinoma: differences in clinical relevance between nonincidental and incidental tumors. World J Surg. 2009;33(3):460–8.
Wei X, Wang M, Wang X, Zheng X, Li Y, Pan Y, Li Y, Mu J, Yu Y, Li D, et al. Prediction of cervical lymph node metastases in papillary thyroid microcarcinoma by sonographic features of the primary site. Cancer Biol Med. 2019;16(3):587–94.
Gao Y, Qu N, Zhang L, Chen J, Ji Q. Preoperative ultrasonography and serum thyroid-stimulating hormone on predicting central lymph node metastasis in thyroid nodules as or suspicious for papillary thyroid microcarcinoma. Tumour Biol. 2016;37(6):7453–9.
Deng J, Zhang D, Zhang W, Li J. Construction and validation of new nomograms to predict risk and prognostic factors of breast cancer bone metastasis in Asian females: a population-based retrospective study. Int J Gen Med. 2021;14:8881–902.
Zhang M, Ding C, Xu L, Feng S, Ling Y, Guo J, Liang Y, Zhou Z, Chen Y, Qiu H. A nomogram to predict risk of lymph node metastasis in early gastric cancer. Sci Rep. 2021;11(1):22873.
Venclovas Z, Muilwijk T, Matjosaitis A, Jievaltas M, Joniau S, Milonas D. Head-to-Head Comparison of Two Nomograms Predicting Probability of Lymph Node Invasion in Prostate Cancer and the Therapeutic Impact of Higher Nomogram Threshold. J Clin Med. 2021;10(5):99.
Yang Y, Chen C, Chen Z, Jiang J, Chen Y, Jin L, Guo G, Zhang X, Ye T. Prediction of central compartment lymph node metastasis in papillary thyroid microcarcinoma. Clin Endocrinol (Oxf). 2014;81(2):282–8.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
PQ conceptualized, draft and reviewed and edited the manuscript. PQ, QG and KP managed the project and secured the necessary acquisition funding. JL contributed to guide data analysis, and interpretation and manuscript writing. QG foresee the research, managed the project, reviewed, and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research protocol was approved by the Ethics Committee of Second Affiliated Hospital of Fujian Medical University (2022 Ethical Review No. 481) and was conducted in accordance with the Declaration of Helsinki, and informed consent was obtained from all subjects or their legal guardians.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qiu, P., Guo, Q., Pan, K. et al. Development of a nomogram for prediction of central lymph node metastasis of papillary thyroid microcarcinoma. BMC Cancer 24, 235 (2024). https://doi.org/10.1186/s12885-024-12004-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12004-3