Abstract
Background
Papillary microcarcinoma (PMC) is a subgroup of papillary thyroid carcinoma (PTC) measuring 1.0 cm or less in diameter. Herein we focused on the search for risk factors predicting nodal metastasis and recurrence in PMCs, analyzing differences in presentation, treatment, and prognosis between nonincidental and incidental tumors.
Methods
From January 1998 to May 2007, 149 patients had a diagnosis of PMC in our department. A cross-sectional study of 76 patients with nonincidental and 73 patients with incidental PMC was carried out. Demographic data, diagnostic results, tumor characteristics, risk assessment, surgical treatment, and postoperative and follow up results were evaluated.
Results
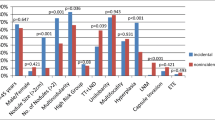
Cytology detected thyroid cancer and nodal involvement in nonincidental PMC. Mean tumor size was significantly larger in nonincidental PMC (7.5 vs. 4.2 mm), which was commonly found within a normal thyroid gland or Hashimoto’s thyroiditis, while incidental PMC was associated with a multinodular goiter. TNM staging system showed a higher cancer stage (IVA) in nonincidental. At multivariate analysis, capsular invasion and a nonincidental diagnosis were the two independent factors significantly affecting nodal metastasis. All patients with nonincidental PMC underwent iodine-131 ablation therapy after surgery compared with 49 patients with incidental. Nodal metastasis at diagnosis was the only factor influencing recurrence which was found in three nonincidental cases: two in the lateral and one in the central neck compartments.
Conclusions
Several PMCs presented with risk-free clinical courses. Some nonincidental tumors had a more aggressive behavior and a tendency to recurrence. In these cases, early detection and aggressive treatment are mandatory as for conventional PTC according to risk stratification and cancer stage.
Similar content being viewed by others
References
Hedinger C, Williams ED, Sobin LH (1988) Histologic typing of thyroid tumors. In: World Health Organization’s international histological classification of tumors, vol 11, 2nd edn. Springer-Verlag, New York, pp 9–10
Bondeson L, Ljungberg O (1981) Occult thyroid carcinoma at autopsy in Malmö, Sweden. Cancer 47:319–323
Franssila KO, Harach HR (1986) Occult papillary carcinoma of the thyroid in children and young adults. A systematic autopsy study in Finland. Cancer 58:715–719
Carlini M, Giovannini C, Castaldi F et al (2005) High risk for microcarcinoma in thyroid benign diseases Incidence in a one-year period of total thyroidectomies. J Exp Clin Cancer Res 24:231–235
Yang GCH, LiVolsi VA, Baloch ZW (2002) Thyroid microcarcinoma: fine-needle aspiration diagnosis and histologic follow up. Int J Surg Pathol 10:133–139
Leenhardt L, Grosclaude P, Chérié-Challine L, Thyroid Cancer Committee (2004) Increased incidence of thyroid carcinoma in France: a true epidemic or thyroid nodule management effects? Report from the French Cancer Committee. Thyroid 14:1056–1060
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 10:2164–2167
Cady B, Rossi R, Silverman M et al (1985) Further evidence of the validity of risk group definition in differentiated thyroid carcinoma. Surgery 98:1171–1178
Hay ID, Bergstralh EJ, Goelner JR et al (1993) Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery 114:1050–1058
Mazzaferri EL, Jhiang SM (1994) Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 97:418–428
Baudin E, Travagli JP, Ropers J et al (1998) Microcarcinoma of the thyroid gland: the Gustave-Roussy Institute experience. Cancer 83:553–559
Topliss D (2004) Thyroid incidentaloma: the ignorant in pursuit of the impalpable. Clin Endocrinol 60:18–20
Barbaro D, Simi U, Meucci G et al (2005) Thyroid papillary cancers: microcarcinoma and carcinoma, incidental cancers and non-incidental cancers. Are they different diseases? Clin Endocrinol 63:577–581
Ito Y, Uruno T, Nakano K et al (2003) An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid 13:381–3387
Roti E, Rossi R, Trasforini G et al (2006) Clinical and histological characteristics of papillary thyroid microcarcinoma: results of a retrospective study in 243 patients. J Clin Endocrinol Metab 91:2171–2178
Chow SM, Law SCK, Chan JKC et al (2003) Papillary microcarcinoma of the thyroid. Prognostic significance of lymph node metastasis and multifocality. Cancer 98:31–40
Noguchi S, Yamashita H, Uchino S et al (2008) Papillary microcarcinoma. World J Surg 32:747–753
Wada N, Duh QY, Sugino K et al (2003) Lymph node metastasis from 259 papillary thyroid microcarcinomas. Frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 237:399–407
Lin KD, Lin JD, Huang MJ et al (1997) Clinical presentations and predictive variables of thyroid microcarcinoma with distant metastasis. Int Surg 82:378–381
Rosai J, LiVolsi VA, Sobrinho-Simoes M et al (2003) Renaming microcarcinoma of the thyroid gland: the Porto proposal. Int J Surg Pathol 11:249–251
DeLellis RA, Lloyd RV, Heitz PU et al (eds) (2004) World Health Organization classification of tumors: pathology and genetics of tumors of endocrine organs. IARC Press, Lyon, pp 64–66
Shah JP, Kian K, Forastiere A et al (2002) Thyroid gland. In: American Joint Committee on cancer: cancer staging manual, 6th edn. Springer-Verlag, New York, pp 77–87
Pellegriti G, Scollo C, Lumera G et al (2004) Clinical behavior and outcome of papillary thyroid cancers smaller than 1.5 cm in diameter: study of 299 cases. J Clin Endocrinol Metab 89:3713–3720
Hay ID, Grant CS, Van Heerden JA et al (1992) Papillary thyroid microcarcinoma: a study of 535 cases observed in a 50-year period. Surgery 112:1139–1147
Fleming ID, Cooper JS, Henson DE (1997) Thyroid gland. In: American Joint Committee on cancer: cancer staging manual, 5th edn. Lippincott-Raven, Philadelphia, pp 59–64
Pattou F, Combemale F, Fabre S et al (1998) Hypocalcemia following total thyroidectomy: incidence and prediction of outcome. World J Surg 22:718–724
QBGroup spa, DRG online 1999–2008. http://www.drg.it. Accessed 29 July 2008
Schonberger J, Marienhagen J, Agha A et al (2007) Papillary microcarcinoma and papillary cancer of the thyroid ≤1 cm. Modified definition of the WHO and the therapeutic dilemma. Nuklearmedizin 46:115–120
Piersanti M, Ezzat S, Asa SL (2003) Controversies in papillary microcarcinoma of the thyroid. Endocr Pathol 14:183–191
Yasuhiro I, Takashi U, Yuuki T et al (2005) Papillary microcarcinomas of the thyroid with preoperative detectable lymph node metastasis show significantly higher aggressive characteristics on immunohistochemical examination. Oncology 68:87–96
Pelizzo MR, Boschin IM, Toniato A et al (2004) Natural history, diagnosis, treatment and outcome of papillary thyroid microcarcinoma (PTMC): a mono-institutional 12-year experience. Nucl Med Commun 25:547–552
Lo CY, Chan WF, Lang BHH et al (2006) Papillary microcarcinoma: is there any difference between clinically overt and occult tumors? World J Surg 30:759–766
Sugitani I, Fujimoto Y (1999) Symptomatic versus asymptomatic papillary thyroid microcarcinoma: a retrospective analysis of surgical outcome and prognostic factors. Endocr J 46:209–216
Bramley MD, Harrison BJ (1996) Papillary microcarcinoma of the thyroid gland. Br J Surg 83:1674–1683
Voutilainen PE, Siironen P, Franssila KO et al (2003) AMES, MACIS and TNM prognostic classifications in papillary thyroid carcinoma. Anticancer Res 23:4283–4288
Khoo ML, Freeman JL, Witterick IJ et al (2002) Underexpression of p27/Kip in thyroid papillary microcarcinomas with gross metastatic disease. Arch Otolaryngol Head Neck Surg 128:253–257
Sawka AM, Kullathorn T, Brouwers M et al (2004) A systematic review and metaanalysis of the effectiveness of radioactive iodine remnant ablation for well differentiated thyroid cancer. J Clin Endocrinol Metab 89:3668–3676
Cooper DS, Doherty GM, Haugen BR et al (2006) Management guidelines for patient with thyroid nodules and differentiated thyroid cancer. Thyroid 16:109–141
Pacini F, Schlumberger M, Dralle H et al (2006) European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur J Endocrinol 154:787–803
Leenhardt L, Hejblum G, Franc B et al (1999) Indications and limits of ultrasound-guided cytology in the management of nonpalpable thyroid nodules. J Clin Endocrinol Metab 84:24–28
Mazzaferri E, Sipos J (2008) Should all patients with subcentimeter thyroid nodules undergo fine-needle aspiration biopsy and preoperative neck ultrasonography to define the extent of tumor invasion? Thyroid 18:597–602
Berker D, Aydyn Y, Ustun Y et al (2008) The value of fine needle aspiration biopsy in the sub-centimeter thyroid nodules. Thyroid 18:603–608
Acknowledgment
This study was supported by a grant from the University of Cagliari, Italy.
Author information
Authors and Affiliations
Corresponding author
Additional information
Part of this study was presented at the 10th AFCE Congress (Association Francophone de Chirurgie Endocrinienne), Reims, France, June 2007.
Rights and permissions
About this article
Cite this article
Pisanu, A., Reccia, I., Nardello, O. et al. Risk Factors for Nodal Metastasis and Recurrence Among Patients with Papillary Thyroid Microcarcinoma: Differences in Clinical Relevance Between Nonincidental and Incidental Tumors. World J Surg 33, 460–468 (2009). https://doi.org/10.1007/s00268-008-9870-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9870-8