Abstract
Multidisciplinary team meetings are a current international practice in cancer care, but to date, few data exist on the specificity of its practice in hematology.
In this manuscript, we present the result of the first national study, realized with quantitative and qualitative methods in France, which brings new insights in order to improve the collegial decision-making process.
To improve the effectiveness of MDTMs, the needs to focus on complex cases, to enhance patient centeredness and teamwork are relevant aspects, and a specific focus on hematological particularities is warranted to truly improve process.
Background Understanding the Multidisciplinary team meetings (MDTMs) process in different medical specialties facilitates the identification of core factors supporting effective MDTM work. Our mixed-methods study explores the participants’ perceptions of hematology MDTMs.
Design Online questionnaires collected data concerning the decision-making process, benefits and inconveniences of MDTMs for both patients and professionals. Semi-directive phone interviews were conducted and analyzed, thereby supplying qualitative data.
Results A total of 205 professionals responded to the questionnaire and 22 participated in the qualitative interviews. The data indicate the unique characteristics of hematology, including a specific definition of collegiality, the frequent solicitation of expert advice and the anticipation of treatment even prior to the occurrence of MDTMs. Additional information concerning patients’ wishes and psychosocial conditions are also needed. Participants emphasize the subjective aspects and the impact of the climate of MDTMs on medical decisions.
Conclusion Although MDTMs are recognized to be a valuable tool, organizational and relational issues may interfere with their efficiency.
To improve the effectiveness of MDTMs, the needs to focus on complex cases, to enhance patient centeredness and teamwork are relevant aspects. A specific focus on hematological particularities might be warranted to truly improve the collegial decision-making process in the context of hematology.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Multidisciplinary team meetings (MDTMs) are a current international practice to facilitate the care of cancer patients. They bring together health professionals from different disciplines whose skills are essential to establish the diagnosis and to make a decision offering patients the best management according to the state of the medical science. They promote the coordination of communication and treatment, thereby improving the decision-making process and the quality of care [1,2,3,4,5].
In France, the first Cancer Plan (2003–2007) [6] defines MDTMs’ requirements (membership, standards, quorum, procedures and formal reporting criteria for records) and objectives: to standardize the management of cancer patients, analyze medical files and evaluate treatment risks and benefits with the aim of proposing an appropriate decision in accordance with evidence-based medicine (EBM).
According to professionals involved in cancer care in France, MDTMs can improve physicians’ adherence to reference guidelines, inclusions to clinical trials, elaboration of personalized plans of care and the transparency of therapeutic choices. In addition, these meetings play a pivotal role in medical training and the process of updating the relevant knowledge [7,8,9].
MDTMs are particularly useful in complex cases (e.g., allogeneic hematopoietic cells transplantation – allo-HCT, transition from curative to palliative care decisions), the frequency of which has been estimated to range between 25 and 40% of examined cases [10, 11]. Nevertheless, the time allocated to the discussion of these complex situations during MDTMs may be insufficient due to the significant number of files that must be treated [12,13,14]. Other impediments of MDTMS, such as poor attendance, insufficient data, lack of administrative support and inadequate leadership, can negatively impact decision-making and the potential effect of MDTMs on the organization of treatment [15].
Research has reported contradictory results concerning the impact of MDTMs on the quality of decision-making and patient outcomes [16,17,18,19] and the reported data also show variability in terms of the implementation of the recommendations made during these meetings [3, 20]. Understanding the MDTM process in the context of different medical specialties may contribute to the task of identifying core factors related to effective MDTM work.
To date, little evidence has been collected concerning MDTMs in hematology field [21,22,23,24]. In the most extensive data set, including all types of MDTMs, hematology was an outlier in relation to several statements regarding the process of clinical decision-making in MDTMs and its impact on the timeliness of care, as well as on patient choices, involvement, staging and survival rates [25].
Hematological malignancies account for approximately 10% of new cancer diagnoses in Western countries and are the sixth most prevalent form of cancer overall. Intensive and innovative treatments, often potentially lifesaving, are core practices in hematology; however, their toxicities often lead to potentially life-threatening or distressing side effects. Thus, the implementation of MDTMs in the context of hematology may require adjustments to ensure that the modalities of such meetings are able to produce benefits for patients and health care professionals.
Our nationwide, mixed-methods study explores the perceptions of participants in French hematology MDTMs concerning these meetings.
Methods
Study design and data collection
We conceived an exploratory study to investigate the representations of health professionals working in Hematology field about the MDTM. A mixed-method approach was chosen to better identify specificities of this specialty: a questionnaire was conceived in the basis of previous research and a qualitative approach was employed to explore relevant points of the survey’s answers.
Our mixed-method study has been performed in accordance with the relevant guidelines [26, 27].
Informed consent was obtained from participants after information about the study’s objectives and methods.
Quantitative approach and survey
Based on previous research, we developed a 46-item Survey Monkey questionnaire. This online survey software facilitates the collection and analysis of a targeted population’s perception about a subject. Three categories of questions – close-ended, open-ended, and descriptive—may be proposed and the questionnaire may be sent by e-mail and/or web links.
Our questionnaire pertained to the following themes: socio-demographic data, professional profile and a description of MDTMs in terms of respondents’ participation (frequency and kind of MDTM attended), duration, relevant information, quorum, participant professionals, clinical trials inclusions, implementation of MDTMs’ decisions, discussion dynamics, decisional process, patient representation, benefits and inconveniences of MDTMs for patients and professionals. It was composed of different kinds of questions: yes/no questions (e.g. « do you regularly participate in MDTM therapeutic decisions ?»), multiple choice questions (e.g. frequency of MDTMs: weekly/every two weeks/monthly/other); Likert scale questions (e.g. fully agree↔strongly disagree); ranking questions (e.g. from 1 to 5 the importance of data).
Our survey was tested before it was distributed to members of the French Society of Hematology (about 1000 members) and the French Association of Residents in Hematology (about 250 members).
Qualitative approach and interviews
A qualitative approach was employed to explore certain significant points in the survey, notably respondents’ opinions concerning their participation, the discussion dynamics and the benefits and inconveniences of MDTMs.
The qualitative part of the study has been realized according to COREQ recommendations [27].
We referred to the framework approach [28], according to which relevant themes referred to existing knowledge concerning the topic area, are organized into a pre-established grid. The interview guide was based on the data provided by the Survey Monkey questionnaire. Consenting respondents were contacted to conduct a telephone interview lasting thirty minutes.
A professional with a dual master’s degree in psychology and sociology who also had twenty years of experience in clinical and research work in the field of hematology conducted all the interviews, which were recorded and transcribed in their entirety.
Data analysis
Quantitative data were processed only by descriptive statistics, reported by raw numbers and percentages for simple and multiple-choice questions, weighted average was added to Likert scale and ranking questions. No comparisons were made among different subgroups. As all respondents did not answer to all the questions, we reported the number of respondents for each question, so to avoid wrong interpretations of data.
NVIVO 8 computer-assisted qualitative data analysis software was used to assist in the handling, storage and management of the data. Two investigators coded the transcripts independently: each investigator used tree nodes to organize codes into a hierarchical structure and subsequently established relationships among different themes and subthemes. A third investigator reviewed the coding process and participated in the thematic analysis. The interpretations provided by the three investigators were than validated by other collaborators (consensual validity).
Results
Quantitative data
Of the 205 respondents, ranging from 26 to 68 years old, 58% were women. They mostly work in France (93%): 67% in clinical hematology services, and 74% in university hospital centers. Most of respondents were clinical hematologists (67%) and biological hematologists (22%). See Table 1 for more details regarding the survey’s population.
One hundred fifty-four complete responses were ultimately obtained, but all answers are reported: number of responses and percentage are indicated for each item. For significant quantitative data please see Additional file 1.
Among the respondents, 93% participated in one or more MDTMs, mostly local (80%) or inter-hospital meetings (43%) in generalist hematology (64%), lymphoid pathologies (57%), myeloid pathologies (54%) and transplantation (39%). The mean length of the MDTMs was 120 min, and about 20 files were reviewed in average during each meeting.
Opinions were divided concerning the specialties that should represent a minimum quorum for a hematology MDTM: for 32% of respondents, 3 physicians with different specialties (clinician, biologist or radiologist) including at least a clinical hematologist were necessary; whereas for 24% of respondents, 3 clinical hematologists were required. The participants’ specialties most frequently cited were clinical hematologists, biological hematologists, cytogeneticists/molecularists.
Regarding patient centeredness, 92% of respondents (61% always and 31% frequently) informed the patient that his/her file was to be discussed among colleagues, but only 14.6% and 13.4% considered patient preferences and psychosocial data to be essential elements involved in producing an optimal therapeutic proposal, respectively. It is important to note that if the treatment implemented is different from that proposed by the MDTM, only 54% of the respondents systematically notified patients about this decision.
Most of respondents believed that MDTMs contribute to enhance decisions in line with the relevant guidelines (95%), to increase inclusion in clinical trials (91%), to improve decision-making (100%), care coordination (89%), quality of care (92%) and feeling of safety for patients (92%). Regarding the MDTMs’ role in improving patient prognosis, timeliness of exams or treatments and patient involvement in medical decision-making, respondents’ opinions were more divided.
About the benefits of MDTMs for professionals, respondents are unanimous about the advantages related to information/knowledge sharing (100%), interactions with colleagues (100%), reviewing the patient file (99%) and helping with decision-making (98%). Other benefits, such as reducing decision uncertainty, sharing legal responsibility and increasing work satisfaction are mentioned.
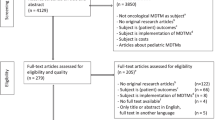
The clinical situations most frequently discussed in hematology MDTMs are: hematological malignancies (95%), difficult diagnoses (83%), benign complex cases (54%), and malignant cases without therapeutic indication (e.g., stage A CLL) (41%). MDTMs discussions appears to be particularly useful with respect to the situations outlined in Fig. 1, ranked from most to least useful: relapse with several therapeutic possibilities that have not yet been prioritized by recommendations; therapeutic decisions related to an uncertain diagnosis; allogeneic hematopoietic cell transplantation (allo-HCT) indication for advanced hematological malignancy; first-line treatment; compassionate treatment for advanced malignancy; and palliative situations lacking therapeutic alternatives.
Respondents were asked to rank suggestions in order of usefulness of discussions; averages were assigned to each answer choice (1 = least useful, 6 = more useful).
Weighted average of clinical situations discussed in hematology MDTM provided by respondents (N = 105).
For more than 98% of respondents, the treatment can be initiated prior to MDTM discussion. This situation can happen in up to 21% of the cases, corresponding to therapeutic emergencies.
Eighty-seven percent of the respondents often sought advice from external experts, as frequently as 10 times per month. The reasons why MDTMs may not be adequate to produce a therapeutic proposal are (ranked from most frequently cited to least frequently cited): the need to consult references or seek expert advice (71%), a lack of information regarding the pathology (70%) or the patient (57%), the complexity of the case (48%), a disagreement among MDTM participants (14%).
The disadvantages of MDTMs are reported less often but the following are quoted: technical issues (55%), interrupts/delays (51%), exacerbation of problems within teams (36%), time losses (27%), peer judgments (15%), and the fact that such meetings are likely to lead to insufficient consideration of patient preferences (25%). Only 6% of respondents considered MDTM to be inappropriate in the context of hematology.
Qualitative data
Twenty-two of the survey respondents agreed to participate in the qualitative study. They were mostly hematologists (99%) and men (59%) between the ages of 28 and 65. They worked mainly in adult clinical hematology departments (77%) or oncology-hematology units (23%) as public hospital practitioners. They participate weekly at least to a local MDTM; they may also take part in specific pathology and/or regional MDTM.
For more details about qualitative study’s respondents see Table 2.
Qualitative data were organized in accordance with the following themes: MDTM implementation, the dynamics of the MDTM (organizational aspects and subjective issues), the discussion of complex cases, the failure to implement the MDTMs’ decisions, the benefits and inconveniences of MDTMs and suggestions for improving MDTMs.
MDTM implementation
Most respondents mentioned the preliminary existence of weekly “staff” meetings prior to the implementation of MDTMs as encouraged by the French Cancer Plan. In their opinion, the current regulatory status of the MDTMs, which required the presence of various specialists to ensure the collective character of decisions made during these meetings, served as a guarantee against unilateral decisions.
The dynamics of the MDTM
Most interviewees highlighted the issue of MDTM dynamics, which depend on both organizational and “subjective” aspects (see Table 3 for significant quotations).
Organizational aspects
The number of MDTMs’ participants ranged from 5 to 20. The interviewees highlighted their interest in the presence of various specialists, but they also wondered whether too many participants could influence the decision-making process negatively.
In addition to the medical data, the presence of the referent hematologist is essential: he or she is supposed to be aware of patients’ conditions, preferences and psychosocial data, which are rarely recorded in medical files. This information is particularly useful when the efficacy of different therapeutic options is equivalent. It is worth noting that some interviewees questioned the influence of these “subjective data”, which may be affected by the referent hematologist’s perceptions, on decisions made during MDTMs.
The time allocated to the task of examining files influences the quality of the discussions, which also depends on whether the cases are examined at the beginning or the end of the meeting.
Most interviewees considered the “compulsory recording” of all files to be “a waste of time” and believed that "difficult cases" should be prioritized. Other interviewees highlighted the risk of neglecting “simple files”, which could nevertheless raise important decisions, such therapeutic abstention. Some respondents also emphasized the importance of reminding all MDTM participants of current recommendations. Regarding this issue, other interviewees mentioned time pressure and drew attention to the discrepancy between the purpose of MDTMs, i.e., to make decisions, and the pedagogical value of such meetings.
Subjective issues
Several interviewees described an MDTM as a “mini-concentration of the team’s life”. Participating in MDTM discussions is correlated to the participant’s expertise and to the ambience of the meeting. A “kind ambience” facilitates the expression of opinions by all participants. In contrast, "interpersonal conflicts" may emerge during these meetings, thereby hindering these discussions and leading to "peremptory" positions. Some interviewees noted that two groups participate in an MDTM: “professionals who express an opinion that exudes authority and those who listen…”.
The ambience of an MDTM is associated with the team’s interpersonal relationships and the role of the department head, who is typically the moderator of these meetings. Two "figures" are described: a moderator who facilitates speaking and stimulates exchanges by adopting a position of equality with regard to each participant and a leader who imposes his or her recommendations, returning to decisions made in his or her absence and discouraging the participation of the team members.
Discussing complex files
The interviewees mentioned “complex files”, which could lead to a demanding decision-making process or even occasionally to the absence of a unanimous therapeutic proposal. Aspects of the situations discussed included the following:
-
- Doubts regarding diagnosis
-
- Therapeutic abstentions
-
- Multi-treated patients
-
- Comorbidities jeopardizing the feasibility of standard treatments
-
- Inclusion in new clinical trials
-
- Prescription of new, expensive treatments
-
- Indications supporting Hematopoietic Cell Transplantation (HCT)
-
- Palliative care (PC) decisions.
Indications suggesting HCT and PC decisions were quoted most frequently as “complex situations”, which involved a significant risk of "unreasonable stubbornness". Participants noted that information regarding patients’ psychosocial situations and wishes was rarely presented.
Several interviewees questioned the overestimation of the benefits of curative treatments in the context of these medical situations and observed that the advice given during MDTMs frequently lacked the power to alter the initial convictions of the referent hematologist.
When a consensus was not reached, two or three therapeutic alternatives could be proposed to the referent hematologist. Some interviewees noted that "subjective" bias could interfere with the referent hematologist’s decision. These interviewees evoked the possibility of resorting to asking experts on specific pathologies, reference centers focusing on rare diseases or even national-/expert-level MDTMs. Other interviewees affirmed that the “final word” should be given to the department head due to his or her wealth of scientific knowledge and clinical experience. Some respondents also remarked that, in all cases, “the decision should be shared with the patient”.
The failure to implement MDTMs’ decisions
The reasons for the failure to implement decisions made at the MDTM were as follows: a lack of medical elements, the absence of the referent hematologist and/or the pathology specialist, the patient’s refusal and the evolution of the patient’s clinical situation. In these latter situations, either the file was presented at the next meeting (occasionally a regional and more expert MDTM) or the referent hematologist made a decision based on EBM recommendations.
A “really exceptional situation” occurred when the referent hematologist disagreed with the conclusion of the MDTM, instead opting for another therapeutic choice. These situations were associated with tense interpersonal relationships and MDTM dynamics involving conflict.
Benefits of MDTMs
Most interviewees were rather enthusiastic regarding the benefits of the MDTMs and mentioned the following aspects: the benefits for training and updating one’s knowledge, homogenization of practices, legitimization of decisions and shared responsibility (see Table 4 for significant quotations in this context).
MDTMs are a mean of regulating individual practices and, in the event of litigations or legal actions, may be used as a “safeguard” for physicians. Other benefits of MDTMs include the positive consequences for the organization of clinical activities and team cohesion.
In the opinions of respondents, the most important benefit to patients was the discussion of their files by a panel of experts, thus increasing the medical relevance of the resulting therapeutic choice. In addition, MDTMs can increase patients’ chances of benefiting from the latest therapies, of being included in clinical trials and of accessing scientific advances in various specialties. A few respondents also emphasized ethical arguments relating to equality of opportunity due to the homogenization of medical practices.
Challenges to the effectiveness of MDTMs
Significant quotations concerning this point are provided in Table 3. The most frequently quoted inconvenience was the fact that MDTM is “very time-consuming” and that institutions do not allocate specific time to engage in this activity.
Several interviewees regret the influence of interpersonal conflicts on the decision-making. Others criticize the "mechanical character” of decisions based only on scientific knowledge, notably neglecting the psychosocial aspects of clinical situations.
The MDTM’s interference in the doctor–patient relationship is particularly noticeable when the collective decision conflicts with the perspective of the referent hematologist. Some interviewees informed patients that their initial therapeutic suggestion would be examined in MDTMs prior to a definitive decision being made.
The majority of interviewees did not report any inconveniences of MDTMs for patients. Some interviewees noted that therapeutic decisions concerning "very advanced" diseases are not always suitable for the patient’s situation due to a lack of psychosocial data (see Table 5 for significant quotations in this context).
Improving MDTMs
Respondents emphasized the fact that institutional recognition of MDTMs as a medical activity is essential to the improvement of these meetings.
Most interviewees’ suggestions concerned logistics: adequate support (appropriate for the specific situation of hematology) and human resources, particularly with respect to secretaries.
Other suggestions concerned organizational matters, notably time regulation: some respondents proposed a preliminary "sorting" of priority files to limit the cases to be discussed during the meetings so that all these cases could be treated equitably.
In addition to the need for the regular participation of pathologists, cytologists, radiologists, and pharmacists, some respondents also suggested the inclusion of other medical specialists (geriatricians and/or PC physicians) or paramedical professionals (nurses, social workers, or psychologists). Other respondents recommended the inclusion of multidisciplinary staff for discussions regarding difficult files, in particular cases in which PC was indicated.
The role of the moderator in limiting interference (e.g., outside requests or phone calls) and encouraging discussion was emphasized. Two interviewees suggested that MDTM moderators should have training in group-leading techniques.
Discussion
Our study is the first nationwide, mixed-methods study to explore the perceptions of participants in hematology MDTMs.
Some results seem to be specific to the decision-making process associated with hematology.
The frequent solicitation of external experts reflects the complexity of hematologic practice, given the existence of hundreds of different hematologic malignancies and the need for accurate and specific expertise to ensure the best possible therapeutic proposal.
In fact, our respondents seem to value the benefit of collegiality more in the contexts of complex cases and difficult situations, even with respect to the management of benign diseases or difficult diagnoses, than in the context of the systematic discussion of every new cancer case, which is actually the regulatory requirement in most countries [29].
With respect to other kinds of tumors, core participants in the MDTMs usually include medical oncologists, radiotherapists and surgeons. In hematology, the therapeutic aspect relies exclusively on clinical hematologists, and while others in attendance are considered to provide substantial help regarding accurate diagnosis and staging, they are frequently less involved in the choice of treatment itself. This situation leads to a particular definition of the MDTM composition required for hematology, which, moreover, can vary depending on the more specific type of disease (e.g., generalist, lymphoid, myeloid) or treatment (auto or allo-HCT, car-T-cells therapy).
Moreover, the frequent anticipation of treatment even prior to discussion at an MDTM in the context of rapidly progressive diseases (such as acute leukemia or aggressive lymphoma) seems to be a particular aspect of hematological practice.
Besides hematology specificities, our study highlights relevant points regarding MDTMs’ decisional process and ethical issues, which may also concern other medical specialties.
As noted in the literature, essentially in the contexts of boards pertaining to solid tumors, our results show that the decision-making process associated with MDTMs is affected by organizational and interpersonal factors [4, 11, 15, 19].
The most frequently quoted organizational factor is the insufficient time allocated to the tasks of preparing for the meeting and to examining all files accurately. Variations in terms of the quality of file discussion and insufficient time for in-depth discussion of complex files are relevant issues that have been described previously [3, 8, 13]. Regarding this issue, a French retrospective analysis of MDTM data highlighted the conflict between the need to respond to the completeness required by the Cancer Plan and the importance of prioritizing multidisciplinary [9]. As other studies have shown [2], the absence of institutional acknowledgment is also considered to be an obstacle to MDTM efficiency: organizational factors impact participants’ attendance negatively, which is a primary reason for the failure to implement MDTM decisions. Among the reasons for the failure to implement MDTM recommendations, our results indicate patient refusal, which may be attributed to poor consideration of patients’ choices and their psychological and social conditions throughout the decision-making process [13, 30,31,32,33,34].
Our data highlight the relevant issue of the usefulness of psychosocial information.
Participants seem to be ambivalent regarding this subject: quantitative data show that a quarter of the respondents consider that patient preferences are insufficiently took into consideration, but less than 15% think that neither these preferences nor psychosocial data are essential to make therapeutic choices. Qualitative data contribute to understand this point: psychosocial data seem to be considered relevant in clinical situations that entail a significant risk of "unreasonable stubbornness" (e.g., allo-HCT indications) or in cases in which a PC decision could be discussed.
Due to the paucity of psychosocial data in medical files, the issue of the subjective perception of the patients' conditions and preferences by the referent hematologist has been raised. To address this issue, the participation of nurses and other health care professionals and PC teams in MDTMs is suggested [10], and such participation has already been implemented in some countries [19]. Nevertheless, some evidence shows that the inclusion of nursing personnel is viewed as less important [14, 35,36,37]. Indeed, several authors have shown that the biomedical approach tends to take precedence over other points of view [15, 35, 38, 39].
The decision-making process is influenced by MDTM dynamics, which are themselves affected by the number of participants involved in the meetings, team relationships and the performance of the MDTM coordinator.
The group’s size is related to its diversity and range of abilities, but it may negatively affect the equality of participation and the effectiveness of the decision-making process [11]. Regarding the number of participants, our data highlight the issue of a possible discrepancy between two main tasks of an MDTM: the decision-making process and the goal of training and knowledge updating.
Team relationships and the coordinator role influence the involvement of the participants, the decisions made at the MDTM and, indirectly, the implementation of those decisions. Indeed, the internal elements of these groups (cultures, beliefs, attitudes, and the interactions among group members), interpersonal factors (lack of trust or respect between team members) and hierarchical stances can impede the decision-making process. It has been shown that team dynamics, ranging from interactive debates to exchanges dominated by single individuals, may impact interactivity and MDTM discussions [14, 37].
Our qualitative data highlight the participants’ concerns about the influence of subjective factors on clinical decisions. A recent French study, based on an ethnographic observation of MDTMs related to breast and ovarian cancer and referred to Longino’s theory of scientific deliberation [40] showed that MDTMs do not always respond to the conditions required to ensure objectivity and rationality. Nevertheless, the author noted that the lateral control among peers and the collective evaluation of the most recently available data contribute to limiting the influence of subjective preferences in the MDTM setting [41].
The meeting climate and quality of the decision-making process both impact the participants’ opinions regarding recommendations made at the MDTM. Some evidence shows that approximately one-third of MDTM participants disagree regarding the decisions ultimately made at such meetings [42]. This unexpressed dissent influences the participants’ feelings concerning the way in which the MDTM can interfere with doctor–patient interactions, although other research has shown that MDTMs do not affect this relationship [43].
These issues regarding MDTM dynamics and the pivotal role of the MDTM coordinator have been acknowledged [43,44,45,46,47]. The role of personal qualities and nontechnical skills in managing MDTMs has been emphasized, and specific leadership training for MDTM chairs has been recommended [3, 48, 49].
In spite of organizational and interpersonal issues, hematologists – as professionals of other medical specialties, seem to highly appreciate MDTMs and largely recognize its value as part of the decision-making process.
Limitations
Our study faces certain limitations, notably with respect to the sampling process. Regarding quantitative data, online survey monkey don’t allow researchers to know if concerned population (SFH and AIH members) received e-mails asking their participation. Besides, a quarter of the respondents didn’t answer to all the questions, negatively impacting the analysis of the data.
Concerning the qualitative study, we consider that voluntary participation may induce a bias connected to the particular views of the respondents with respect to the subject in question.
Moreover, even if the similarities are noted between the population of the survey and the qualitative study regarding the medium age (40 years old) and the frequency of participation in MDTM (weekly), the interviewed professionals are not representative of the survey’s population. The sex ratio is inverted: 58% of the survey’s participants are female, whereas in the qualitative study, most of the respondents (59%) are male. It is difficult to know if gender differences may impact the professionals’ perception of the approached themes.
As for the survey’s respondents, the majority of qualitative study’s respondents work in university hospitals (respectively 74% and 55%), but the percentages of respondents working in local and regional hospitals were higher in the qualitative study. We may make the assumption of the influence of the work conditions in these different institutional settings on the respondents’ appreciations of MDTM issues, but we didn’t explore this point.
Further research could explore the means to improve the quality of MDTM and the decision-making process in hematology. Taking into account the need for frequent referral, a particular definition of multidisciplinarity and consideration of frequent emergencies might be warranted to truly improve the collegial discussion proceeding in this medical specialty.
Public policies considering the unmet needs of MDTMs could be envisaged, such as better recognition of the time dedicated to this activity and its preparation, technical issues and specific leadership training for MDTM chairs.
Conclusion
Our study is the first nationwide, mixed-methods study to explore the perceptions of participants in hematology MDTMs. It highlights certain aspects of the decision-making process in this medical specialty, such as the frequent need for referral, the particular definition of the participants’ specialties and the recurrent clinical emergencies. But it also points out organizational and interpersonal issues, which may interfere with MDTMs’ performance.
Organizational obstacles are mainly related to a lack of institutional recognition of this medical activity (in terms of time pressure and workload) and to the compulsory registration of all files. Poor team ambience negatively influences MDTM discussions and the implementation of its recommendations. A main result of our qualitative study underscores the influence of subjective factors on clinical decisions, which are expected to adhere to scientific data and EBM. These findings raise important ethical issues, which should be explored by larger research – not only in the Hematology, but also in the context of other medical specialties.
Availability of data and materials
The quantitative data used to support the findings of this study are available at Sandra Malak, Alice Polomeni, 2022, French Multidisciplinary meetings in hematology, Synapse storage, DOI: https://doi.org/10.7303/syn35106206. The qualitative data used to support the findings of this study are restricted by the Ethics Commission of the French Society of Hematology in order to protect participants’ privacy. Data are available from Alice Polomeni, alice.polomeni@aphp.fr for researchers who meet the criteria for access to confidential data.
References
Engelhardt M, Ihorst G, Schumacher M, Rassner M, Gengenbach L, Moller M, Shoumariyeh K, Neubauer J, Farthmann J, Herget G, Wasch R. Multidisciplinary tumor boards and their analyses: the yin and yang of outcome measures. BMC Cancer. 2021;21(1):173. https://doi.org/10.1186/s12885-021-07878-6. Epub 2021/02/19. PubMed PMID: 33596881; PMCID: PMC7891134.
Jalil R, Ahmed M, Green JS, Sevdalis N. Factors that can make an impact on decision-making and decision implementation in cancer multidisciplinary teams: an interview study of the provider perspective. Int J Surg. 2013;11(5):389–94. https://doi.org/10.1016/j.ijsu.2013.02.026. Epub 2013/03/19. PubMed PMID: 23500030.
Lamb BW, Brown KF, Nagpal K, Vincent C, Green JS, Sevdalis N. Quality of care management decisions by multidisciplinary cancer teams: a systematic review. Ann Surg Oncol. 2011;18(8):2116–25. https://doi.org/10.1245/s10434-011-1675-6. Epub 2011/03/29. PubMed PMID: 21442345.
Selby P, Popescu R, Lawler M, Butcher H, Costa A. The value and future developments of multidisciplinary team cancer care. Am Soc Clin Oncol Educ Book. 2019;39:332–40. https://doi.org/10.1200/EDBK_236857. Epub 2019/05/18. PubMed PMID: 31099640.
Walraven JEW, van der Hel OL, van der Hoeven JJM, Lemmens V, Verhoeven RHA, Desar IME. Factors influencing the quality and functioning of oncological multidisciplinary team meetings: results of a systematic review. BMC Health Serv Res. 2022;22(1):829. https://doi.org/10.1186/s12913-022-08112-0. Epub 2022/06/28. PubMed PMID: 35761282; PMCID: PMC9238082.
Cannell E. The French Cancer Plan: an update. Lancet Oncol. 2005;6(10):738. https://doi.org/10.1016/s1470-2045(05)70369-7. Epub 2005/10/19. PubMed PMID: 16229093.
Bas Theron F, Gresy B, Guillermo V, Chambaud L. Évaluation des mesures du plan cancer 2003–2007 relatives au dépistage et à l’organisation des soins. Inspection générale des affaires sociales; 2009.
Descotes JL, Guillem P, Bondil P, Colombel M, Chabloz C. Assessment of cancer RCP meetings in Rhone-Alpes: a survey on the ground. Prog Urol. 2010;20(9):651–6. https://doi.org/10.1016/j.purol.2010.03.012. Epub 2010/10/19. PubMed PMID: 20951934.
Guillem P, Bolla M, Courby S, Descotes JL, Laramas M, Moro-Sibilot D. Multidisciplinary team meetings in cancerology: setting priorities for improvement. Bull Cancer. 2011;98(9):989–98. https://doi.org/10.1684/bdc.2011.1428. Epub 2011/09/13. PubMed PMID: 21908262.
Orgerie MB, Duchange N, Pelicier N, Chapet S, Dorval E, Rosset P, Lemarie E, Herve C, Moutel G. Decision process in oncology: the importance of multidisciplinary meeting. Bull Cancer. 2010;97(2):255–64. https://doi.org/10.1684/bdc.2009.0957. Epub 2009/10/15. PubMed PMID: 19825531.
Soukup T, Petrides KV, Lamb BW, Sarkar S, Arora S, Shah S, Darzi A, Green JSA, Sevdalis N. The anatomy of clinical decision-making in multidisciplinary cancer meetings: a cross-sectional observational study of teams in a natural context. Medicine (Baltimore). 2016;95(24):e3885.
Hong NJ, Wright FC, Gagliardi AR, Paszat LF. Examining the potential relationship between multidisciplinary cancer care and patient survival: an international literature review. J Surg Oncol. 2010;102(2):125–34. https://doi.org/10.1002/jso.21589. Epub 2010/07/22. PubMed PMID: 20648582.
Lamb BW, Wong HW, Vincent C, Green JS, Sevdalis N. Teamwork and team performance in multidisciplinary cancer teams: development and evaluation of an observational assessment tool. BMJ Qual Saf. 2011;20(10):849–56. https://doi.org/10.1136/bmjqs.2010.048660. Epub 2011/05/26. PubMed PMID: 21610266.
Soukup T, Lamb BW, Arora S, Darzi A, Sevdalis N, Green JS. Successful strategies in implementing a multidisciplinary team working in the care of patients with cancer: an overview and synthesis of the available literature. J Multidiscip Healthc. 2018;11:49–61. https://doi.org/10.2147/JMDH.S117945. Epub 2018/02/07. PubMed PMID: 29403284; PMCID: PMC5783021.
Lamprell K, Arnolda G, Delaney GP, Liauw W, Braithwaite J. The challenge of putting principles into practice: Resource tensions and real-world constraints in multidisciplinary oncology team meetings. Asia Pac J Clin Oncol. 2019;15(4):199–207. https://doi.org/10.1111/ajco.13166. Epub 2019/05/23. PubMed PMID: 31115170.
Croke JM, El-Sayed S. Multidisciplinary management of cancer patients: chasing a shadow or real value? An overview of the literature. Curr Oncol. 2012;19(4):e232-8. https://doi.org/10.3747/co.19.944. Epub 2012/08/10. PubMed PMID: 22876151; PMCID: PMC3410834.
Lamb BW, Taylor C, Lamb JN, Strickland SL, Vincent C, Green JS, Sevdalis N. Facilitators and barriers to teamworking and patient centeredness in multidisciplinary cancer teams: findings of a national study. Ann Surg Oncol. 2013;20(5):1408–16. https://doi.org/10.1245/s10434-012-2676-9. Epub 2012/10/23. PubMed PMID: 23086306.
Pillay B, Wootten AC, Crowe H, Corcoran N, Tran B, Bowden P, Crowe J, Costello AJ. The impact of multidisciplinary team meetings on patient assessment, management and outcomes in oncology settings: A systematic review of the literature. Cancer Treat Rev. 2016;42:56–72. https://doi.org/10.1016/j.ctrv.2015.11.007. Epub 2015/12/09. PubMed PMID: 26643552.
Berardi R, Morgese F, Rinaldi S, Torniai M, Mentrasti G, Scortichini L, Giampieri R. Benefits and limitations of a multidisciplinary approach in cancer patient management. Cancer Manag Res. 2020;12:9363–74. https://doi.org/10.2147/CMAR.S220976. Epub 2020/10/17. PubMed PMID: 33061625; PMCID: PMC7533227.
Look Hong NJ, Gagliardi AR, Bronskill SE, Paszat LF, Wright FC. Multidisciplinary cancer conferences: exploring obstacles and facilitators to their implementation. J Oncol Pract. 2010;6(2):61–8. https://doi.org/10.1200/JOP.091085. Epub 2010/07/02. PubMed PMID: 20592777; PMCID: PMC2835483.
Habermann TM, Khurana A, Lentz R, Schmitz JJ, von Bormann AG, Young JR, Hunt CH, Christofferson SN, Nowakowski GS, McCullough KB, Horna P, Wood AJ, Macon WR, Kurtin PJ, Lester SC, Stafford SL, Chamarthy U, Khan F, Ansell SM, King RL. Analysis and impact of a multidisciplinary lymphoma virtual tumor board. Leuk Lymphoma. 2020;61(14):3351–9. https://doi.org/10.1080/10428194.2020.1817432. Epub 2020/09/25. PubMed PMID: 32967496; PMCID: PMC8682150.
Lamb BW, Sevdalis N, Benn J, Vincent C, Green JS. Multidisciplinary cancer team meeting structure and treatment decisions: a prospective correlational study. Ann Surg Oncol. 2013;20(3):715–22. https://doi.org/10.1245/s10434-012-2691-x. Epub 2012/10/16. PubMed PMID: 23064794.
Le Divenah A, David S, Bertrand D, Chatel T, Viallards ML. Multidisciplinary consultation meetings: decision-making in palliative chemotherapy. Sante Publique. 2013;25(2):129–35 Epub 2013/08/24 PubMed PMID: 23964537.
Atwell D, Vignarajah DD, Chan BA, Buddle N, Manders PM, West K, Knesl M, Long J, Min M. Referral rates to multidisciplinary team meetings: is there disparity between tumour streams? J Med Imaging Radiat Oncol. 2019;63(3):378–82. https://doi.org/10.1111/1754-9485.12851. Epub 2019/01/10. PubMed PMID: 30623607.
Lamb BW, Sevdalis N, Taylor C, Vincent C, Green JS. Multidisciplinary team working across different tumour types: analysis of a national survey. Ann Oncol. 2012;23(5):1293–300. https://doi.org/10.1093/annonc/mdr453. Epub 2011/10/22. PubMed PMID: 22015450.
Ponto J. Understanding and evaluating survey research. J Adv Pract Oncol. 2015;6(2):168–71 Epub 2015 Mar 1. PMID: 26649250; PMCID: PMC4601897.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. https://doi.org/10.1093/intqhc/mzm042. (Epub 2007 Sep 14 PMID: 17872937).
Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. Second Edition ed: SAGE Publications Ltd; 2013.
Winters DA, Soukup T, Sevdalis N, Green JSA, Lamb BW. The cancer multidisciplinary team meeting: in need of change? history, challenges and future perspectives. BJU Int. 2021;128(3):271–9. https://doi.org/10.1111/bju.15495. Epub 2021/05/25. PubMed PMID: 34028162.
Geerts PAF, van der Weijden T, Savelberg W, Altan M, Chisari G, Launert DR, Mesters H, Pisters Y, van Heumen M, Hermanns R, Bos GMJ, Moser A. The next step toward patient-centeredness in multidisciplinary cancer team meetings: an interview study with professionals. J Multidiscip Healthc. 2021;14:1311–24.
Lamb BW, Green JS, Benn J, Brown KF, Vincent CA, Sevdalis N. Improving decision making in multidisciplinary tumor boards: prospective longitudinal evaluation of a multicomponent intervention for 1,421 patients. J Am Coll Surg. 2013;217(3):412–20.
Restivo L, Apostolidis T, Bouhnik AD, Garciaz S, Aurran T, Julian-Reynier C. Patients’ non-medical characteristics contribute to collective medical decision-making at multidisciplinary oncological team meetings. PLoS One. 2016;11(5):e0154969.
Rosell L, Wihl J, Nilbert M, Malmstrom M. Health professionals’ views on key enabling factors and barriers of national multidisciplinary team meetings in cancer care: a qualitative study. J Multidiscip Healthc. 2020;13:179–86. https://doi.org/10.2147/JMDH.S240140. Epub 2020/02/28. PubMed PMID: 32103978; PMCID: PMC7029585.
Stairmand J, Signal L, Sarfati D, Jackson C, Batten L, Holdaway M, Cunningham C. Consideration of comorbidity in treatment decision making in multidisciplinary cancer team meetings: a systematic review. Ann Oncol. 2015;26(7):1325–32. https://doi.org/10.1093/annonc/mdv025. Epub 2015/01/22. PubMed PMID: 25605751.
Devitt B, Philip J, McLachlan SA. Team dynamics, decision making, and attitudes toward multidisciplinary cancer meetings: health professionals’ perspectives. J Oncol Pract. 2010;6(6):e17-20. https://doi.org/10.1200/JOP.2010.000023. Epub 2011/03/02. PubMed PMID: 21358945; PMCID: PMC2988673.
Gray R, Gordon B, Meredith M. Patients’ Needs: Improving the Effectiveness of Multidisciplinary Team Meetings in Cancer Services2017.
Walsh J, Harrison JD, Young JM, Butow PN, Solomon MJ, Masya L. What are the current barriers to effective cancer care coordination? a qualitative study. BMC Health Serv Res. 2010;10:132.
Hahlweg P, Didi S, Kriston L, Harter M, Nestoriuc Y, Scholl I. Process quality of decision-making in multidisciplinary cancer team meetings: a structured observational study. BMC Cancer. 2017;17(1):772.
Horlait M, De Regge M, Baes S, Eeckloo K, Leys M. Exploring non-physician care professionals’ roles in cancer multidisciplinary team meetings: A qualitative study. PLoS One. 2022;17(2):e0263611.
Longino H. Science as social knowledge: Values and objectivity in scientific inquiry. Princeton University Press. 1990.
Yvonnet S. An analysis of medical decision making: the case of multidisciplinary team meetings. Bull Cancer. 2022;109(3):346–57.
Sidhom MA, Poulsen M. Group decisions in oncology: doctors’ perceptions of the legal responsibilities arising from multidisciplinary meetings. J Med Imaging Radiat Oncol. 2008;52(3):287–92. https://doi.org/10.1111/j.1440-1673.2007.01916.x. Epub 2008/05/15. PubMed PMID: 18477124.
Orgerie MB, Duchange N, Pelicier N, Rosset P, Lemarie E, Dorval E, Chapet S, Herve C, Moutel G. Multidisciplinary meetings in oncology do not impact the physician-patient relationship. Presse Med. 2012;41(3 Pt 1):e87-94. https://doi.org/10.1016/j.lpm.2011.07.026. Epub 2011/11/15. PubMed PMID: 22079306.
Taplin SH, Rodgers AB. Toward improving the quality of cancer care: addressing the interfaces of primary and oncology-related subspecialty care. J Natl Cancer Inst Monogr. 2010;2010(40):3–10.
Taplin SH, Weaver S, Salas E, Chollette V, Edwards HM, Bruinooge SS, Kosty MP. Reviewing cancer care team effectiveness. J Oncol Pract. 2015;11(3):239–46. https://doi.org/10.1200/JOP.2014.003350. Epub 2015/04/16. PubMed PMID: 25873056; PMCID: PMC4438110.
Weaver SJ, Dy SM, Rosen MA. Team-training in healthcare: a narrative synthesis of the literature. BMJ Qual Saf. 2014;23(5):359–72. https://doi.org/10.1136/bmjqs-2013-001848. Epub 2014/02/07. PubMed PMID: 24501181; PMCID: PMC3995248.
Rosell L, Wihl J, Hagberg O, Ohlsson B, Nilbert M. Function, information, and contributions: an evaluation of national multidisciplinary team meetings for rare cancers. Rare Tumors. 2019;11:2036361319841696. https://doi.org/10.1177/2036361319841696. Epub 2019/05/21. PubMed PMID: 31105919; PMCID: PMC6506921.
Wihl J, Rosell L, Bendahl PO, De Mattos CBR, Kinhult S, Lindell G, von Steyern FV, Nilbert M. Leadership perspectives in multidisciplinary team meetings; observational assessment based on the ATLAS instrument in cancer care. Cancer Treat Res Commun. 2020;25:100231.
Walraven JEW, van der Meulen R, van der Hoeven JJM, Lemmens V, Verhoeven RHA, Hesselink G, Desar IME. Preparing tomorrow’s medical specialists for participating in oncological multidisciplinary team meetings: perceived barriers, facilitators and training needs. BMC Med Educ. 2022;22(1):502. https://doi.org/10.1186/s12909-022-03570-w. Epub 2022/06/28. PubMed PMID: 35761247; PMCID: PMC9238222.
Acknowledgements
We thank all the participants who have made it possible to obtain these results and to do this work. Our thanks to the French Society of Hematology and to the French Association of Residents in Hematology.
Funding
This study was supported by the Assistance Publique-Hôpitaux de Paris for English language review.
Author information
Authors and Affiliations
Contributions
All authors have participated in all the stages of this research, from the conception to the manuscript review. A. POLOMENI: research's design conception, material analysis, manuscript writing, review. D. BORDESSOULE: research's design conception, material analysis, manuscript writing, review. S. MALAK: research's design conception, material analysis, manuscript writing, review. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Commission of the French Society of Hematology approved the research. In accordance with local legal requirements, it was not necessary to present the study to another review committee, as it does not involve intervention on subjects, but relies only on questionnaires and interviews with professionals. They all gave their informed consent and the anonymity of the responses was assured. Our mixed-method study has been performed in accordance with the relevant guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Polomeni, A., Bordessoule, D. & Malak, S. Multidisciplinary team meetings in Hematology: a national mixed-methods study. BMC Cancer 23, 950 (2023). https://doi.org/10.1186/s12885-023-11431-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11431-y