Abstract
Background
Cervical cancer is the fourth most frequently diagnosed and found to be the leading cause of cancer death in women, especially in low and middle-income countries. Even though cervical cancer is a preventable disease, its preventive measures have not been equitably implemented across and within different countries; especially in low and middle-income countries, due to different contributing factors.
Objective
This study aimed to assess cervical cancer screening utilization and its’ predictors among Women in Bench Sheko Zone, Southwest Ethiopia.
Method
A community-based cross-sectional study design was employed in Bench Sheko Zone from February 2021 to April 2021. Using a multi-stage stratified sampling method, a total of 690 women in the age range of 30–49 years were included in the study. The logistic regression analysis was used considering a 95% confidence interval and a P-value of < 0.05.
Results
Ninety-six (14.2%) of the participants have utilized cervical cancer screening. Predictors like; age between 40–49 years (AOR = 5.35, 95% CI = [2.89, 9.90]), partner educational status of certificate and above (AOR = 4.36, 95% CI = [1.65, 11.51]), first sexual intercourse before eighteen years (AOR = 4.85, 95% CI = [2.29, 10.26]), ever used of alcohol (AOR = 3.99, 95% CI = [1.23, 12.89]), good knowledge (AOR = 8.98, 95% CI = [4.06, 19.89]), favorable attitude (AOR = 3.56, 95% CI = [1.78, 7.09]), and high perceived benefit (AOR = 2.94, 95% CI = [1.48, 5.84]) were strongly associated with cervical cancer screening utilization.
Conclusion
In this study, cervical cancer screening utilization was relatively low. Therefore, promotion of the perception of women towards cervical cancer screening, and provision of health-related information towards different behavioral-related factors should have to be addressed at each level of health care.
Similar content being viewed by others
Background
Cervical cancer is the fourth most frequently diagnosed cancer and leading cause of cancer death in women, with an estimation of 604,000 new cases and 342,000 deaths worldwide in 2020 [1]. Of estimated new cases and deaths, 117,316 (10.6%) new cases and 76,745(10.8%) death of cervical cancer occur in Africa every year. Yet, because of poor access to screening and treatment services, the vast majority of deaths occur in women living in low- and middle-income countries (LMICs) [2]. In Ethiopia, 7,445 (9.6%) new cases and 5,338 (10.3%) death of cervical cancer occur every year [3].
Cervical cancer is contributed by different factors including; human papillomavirus (HPV) [4], some sexually transmittable infections (human immunodeficiency virus (HIV) [5], herpes simplex virus type-2 [6], chlamydia [7], and gonorrhea [8], smoking [9], a higher number of childbirths [10], multiple sexual partners [11], poor socio-economical status [12], and long-term use of oral contraceptives [13], and corticosteroid drugs [14].
Cervical cancer is a preventable disease. As a result, it can be prevented using comprehensive cervical cancer control methods which include primary prevention (vaccination against HPV), secondary prevention (screening and treatment of pre-cancerous lesions), tertiary prevention (diagnosis and treatment of invasive cervical cancer), and palliative care [4, 15]. However, these preventive measures have not equally implemented across and within countries. In low and middle-income countries (LMICs), only 44% of women have screened for cervical cancer, with the lowest prevalence among women in Sub-Saharan Africa, compared with > 60% of women who have screened in high-income countries [15]. In 2015, the cervical cancer screening rate in Ethiopia is extremely low 2.9% [16].
High-quality screening programs are also important to prevent cervical cancer among unvaccinated women. The world health organization (WHO) recommends the screening of women aged 30 to 49 years either through visual inspection with acetic acid (VIA) in low-resource settings or a papanicolaou test (cervical cytology) every 3 to 5 years or HPV testing every 5 years, coupled with timely and efficacious treatment of precancerous lesions [17, 18].
In Ethiopia, the first cancer prevention and control plan was published in 2015 [19], and a “screen-and-treat” approach has been implemented using visual inspection with acetic acid (VIA) and cryotherapy which were found to be feasible and appropriate screening and treating methods [20]. Despite the implementation of this approach, the cervical cancer screening utilization remains low [21,22,23,24,25] due to different factors like; low knowledge [26], poor attitude [27], inadequate diagnostic facilities [28], poorly structured referral system [29], financial constraints [30], poor infrastructure [31], young women [32], and low parity [32]. Due to these reasons, the incidence and mortality of women associated with cervical cancer remain increasing [3]. However, the incidence and mortality related to cervical cancer have declined markedly in developed countries like; United States and England due to a widespread screening practice [33, 34].
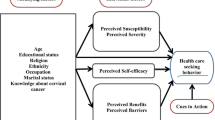
Thus, to increase the cervical cancer screening utilization among eligible women, it is necessary to identify factors using a health belief model (HBM) which helps to predict the health behaviors of women [35, 36]. However, there is paucity of studies related to the perception of women towards cervical cancer and its screening in Ethiopia. Therefore, this study aimed to assess cervical cancer screening utilization and associated factors among women in Bench Sheko Zone, Ethiopia.
Method and materials
Study design and period
A community based cross-sectional study design was employed from February 2021 to April 2021.
Study setting
The study was conducted in Bench Sheko Zone, which is found in the Southern Nation Nationality and Peoples’ Region (SNNPR) State, Ethiopia. Bench Sheko is bordered on the west by South Sudan, on the north by Sheka Zone, on the northwest by Keffa Zone, and on the east by west Omo Zone. The administrative center of Bench Sheko Zone is Mizan Teferi, which is located 561 km far from Addis Ababa. The zone has a total of two administrative towns and six districts namely; Debub Bench, Guraferda, Semen Bench, Shey Bench, Gide Bench, Sheko, Cize town administration, and Mizan Aman town administration with a total population of 609,588 (2011 Zonal Report). In Bench Sheko Zone, there are 1 teaching hospital, 1 primary hospital, 25 health centers, and 130 health posts with different health services. Currently, only the Mizan Tepi University Teaching hospital and Mizan health center give cervical cancer screening service.
Study participants
According to Ethiopian cervical cancer prevention and control guideline [37], all women aged between 30–49 years in Bench Sheko Zone were source population. Hence, women aged between 30–49 years and who lived in selected kebeles during the study period were the study population. Furthermore, women in the age range of 30–49 years and who lived for at least 6 months in the study area were included in the study, whereas, those who were critically ill during the data collection period were excluded.
Sample size determination
The sample size was calculated using a single population proportion formula of \(n=({z\frac{a}{2})}^{2}\frac{p(1-p)}{{d}^{2}}\), where n = the sample size, d = degree of precision = 0.04, Z α/2 = 1.96 by assuming 95% confidence interval and the population proportion of 0.155 (15.5%), as it was used for the study conducted in Jimma town, Southwest Ethiopia [22]. Then, by adding a 10% non-response rate and design effect of 2, the final sample size was 690.
Sampling procedure
For this particular study, a multi-stage stratified sampling technique was used to select the study participants. The primary sampling units, the 3 districts; Shey Bench, Gidi Bench, and Debub Bench, and 1 administrative town, Mizan Aman were selected by simple random sampling from the total of 6 districts and two administrative towns in Bench Sheko Zone, respectively.
The secondary sampling units, the 21 kebeles (the smallest administrative unit within the district) were randomly selected from each stratum (urban and rural). Then, the sample size was distributed to each selected kebeles by population proportion to size (PPS) formula. Then, the tertiary sampling units, the households were selected by using systematic random sampling. The sampling interval (kth interval) of six was used to select the eligible participants using the household lists which were determined after the survey. Then, the next household was selected systematically with a random starting point which was selected from the first 6 households, and the next eligible woman in the household was interviewed every 6th household. For households with more than one eligible woman, only one study participant was selected using the lottery method. Revisit of three times was made when the eligible respondent was not available at the time of the data collection [Fig. 1].
Operational definitions
Cervical cancer screening utilization
Was defined as a woman who ever utilize cervical cancer screening within the past 5 years [25, 38].
Multiple sexual partners
Those women who have ever had more than one sexual partner in their life serially or at the same time [39].
Knowledgeable
Women who were responded to the knowledge-related questions and a score of the mean value or above were considered as knowledgeable [25, 40].
Favorable attitude
Women who were responded to the attitude-related questions and a score of the mean value or above were considered to have a favorable attitude [25, 40].
Perceived susceptibility for cervical cancer
Perception of women about the chances of experiencing a risk or acquiring cervical cancer [22, 41, 42].
Perceived severity of cervical cancer
Perceptions of women on the seriousness of contracting cervical cancer [22, 42, 43].
The perceived benefit of undergoing cervical cancer screening
Refers to the perception of the positive consequences that are caused by the utilization of cervical cancer screening [22, 42, 44].
Perceived barriers for undergoing cervical cancer screening
Refers to the perceptions of women on the obstacles or factors to undergoing cervical cancer screening [22, 42, 45].
Perceived susceptibility, severity, benefit, and barriers were assessed using the 5 points Likert Scale (1: strongly disagree, 2: Disagree, 3: Neutral, 4: Agree, 5: strongly agree). The total scores were computed and dichotomized into high/positive and low/negative using the mean score [22].
Data collection tools and procedure
A structured interviewer administered questionnaire was used to collect the data which was adapted from different reviewed literature [22, 24, 25, 38, 46,47,48]. The questionnaire was translated from English to the national language Amharic and to assure its consistency, it was translated back to English by another linguistic professional. The data were collected by eight trained BSc nurses and supervised by four public health professionals. Before doing the actual data collection, three days of training was given regarding the objective of the study on the data collection tool, interviewing approach, and privacy and confidentiality. The questionnaire was also pretested among 5% of the total study participants in Sheka Zone.
Data quality assurance
The quality of the data was assured by providing three days training for data collectors and using of pretested questionnaire. Moreover, close supervision of the data collection process was done and the questionnaire was checked for consistency, clarity, and completeness.
Data processing and analysis
After data collection was completed, the data was entered into Epi-data manager version 4.0.2.101 and exported to Statistical Package for the Social Sciences (SPSS) version 22.0 for analysis. Descriptive statistics like frequency, percentage, and mean with standard deviation were used. Bivariate logistic regression analysis was performed to select variables for multivariate analysis with a 95% confidence interval and a p-value less than 0.05. Finally, multivariate logistic regression analysis was performed and a p-value of less than 0.05 was considered as strong predictor variables for cervical cancer screening utilization.
Results
Socio-demographic characteristics of the respondents
From the total of 690 eligible women, 678 women have participated in the study yielding a response rate of 98.2%. The mean ± SD age of the participants was 36.01 (SD ± 5.11) years. More than half, 415 (61.2%) of the participants were urban residents, and 297 (43.8%) were protestant religion followers. From the total participants, more than three-fourth, 527(77.7%) of them were currently married. Concerning the respondents’ educational status, 188 (27.7%) of them were unable to read and write. Of all participants, 265(39.1%) were housewives, 194(28.6%) had partners who able to read and write, and 195(28.8%) had partners whose occupations were merchants [Table 1].
Reproductive health and behavioral related characteristics of the respondents
From the total participants, more than two-third, 470(69.3%) of them had the first sexual intercourse before the age of eighteen, whereas, majority or 635(93.7%) of them gave their first child after the age of eighteen with the mean ± SD of 21.8(SD ± 2.6) years. Of all the study participants, about 155(22.9%), 98(14.5%), and 81(11.9) had a history of HIV test, and a history of sexual transmitted diseases (STD), and smoking history, respectively. Concerning contraceptive history, about 427(63.0) of the participants were used modern contraceptives [Table 2].
Cervical cancer screening utilization
Ninety-six (14.2%) (95% CI: 11.5, 16.8) of the participants have ever utilized cervical cancer screening at least once in the last five years. Among the total participants who screened for cervical cancer, about 56 (8.3%), 25 (3.7%), and 15(2.2%) of them were screened due to the offer by the health professionals, self-initiated, and know someone screened, respectively. The most common reason for the participants not to utilize cervical cancer screening was feeling healthy, 269 (39.7%) [Fig. 2].
Predictors of cervical cancer screening utilization
Using bivariate logistic regression, different factors like; the age of participants, partner educational status, age at first sex, ever use of alcohol, smoking history, overall knowledge, overall attitude, perceived susceptibility, perceived severity, and perceived benefit were found to be significantly associated with cervical cancer screening utilization.
After adjusting for possible confounding factors using multivariate logistic regression model; the age of participants, partner educational status, age at first sex, ever use of alcohol, overall knowledge, overall attitude, and perceived benefit were found to be strong predictors of cervical cancer screening utilization.
Participants with the age range of 40–49 years were five times more likely to use cervical cancer screening than those whose ages were 30–39 years (AOR = 5.35, 95% CI = [2.89, 9.90]). Participants with partner educational status of the certificate and above were four times more likely to use cervical cancer screening than those with partner educational status of unable to read and write (AOR = 4.36, 95% CI = [1.65, 11.51]). Those who had first sexual intercourse before eighteen years were almost five times more likely to use cervical cancer screening than those who had first sexual intercourse after eighteen (AOR = 4.85, 95% CI = [2.29, 10.26]). Participants who had ever used alcohol were almost four times more likely to use cervical cancer screening than their counterparts (AOR = 3.99, 95% CI = [1.23, 12.89]). Knowledgeable participants were almost nine times more likely to use cervical cancer screening than their counterparts (AOR = 8.98, 95% CI = [4.06, 19.89]). Those who had a favorable attitude were almost four times more likely to use cervical cancer screening than their counterparts (AOR = 3.56, 95% CI = [1.78, 7.09]). Having perceived benefit of cervical cancer screening utilization were almost four times more likely to use cervical cancer screening than their counterparts (AOR = 2.94, 95% CI = [1.48, 5.84]) [Table 3].
Discussion
Cervical cancer is a public health problem worldwide, and it is one of the leading causes of death in women [18]. The WHO and Ethiopian Federal Ministry of Health (FMOH) recommends cervical cancer screening for age-eligible women every three to five years [19, 49]. This approach enables for the decrement of the incidence and mortality of women associated with cervical cancer [33]. Therefore, this community-based study was conducted to assess the cervical screening utilization among women in Bench Sheko Zone, Ethiopia.
Hence, in this study, the cervical cancer screening utilization was 14.2%. This result was found to be low as compared with the studies conducted in Uganda, 30.3% [50], Nigeria, 20.6% [51], Tanzania, 22% [52] and in other parts of Ethiopia like; Wolatita, 22.9% [53], Addis Ababa, 25% [54], and Gondar, 23.5% [55]. The possible reasons could be due to limited access to screening services, the difference in socio-demographic characteristics and the difference in study subjects. For instance, the study subjects in the study conducted in Uganda and Gondar, Ethiopia were all HIV-infected women.
n contrast to the other studies, this study was found to be higher in the cervical cancer screening utilization compared with the studies conducted in different areas where, 0.2% in Ghana [56], 5.4% in Debre Markos, Northwest Ethiopia [25], and 5.9% in Arbaminch town, Southern Ethiopia [57]. This difference might be attributed to the difference in the study population, the difference in the study period and area, and the difference in the status of knowledge and attitude of the study population.
In this study, women with advanced age were more likely to use cervical cancer screening than young age women. This finding was supported by the other studies conducted in Malawi [58], and in other parts of Ethiopia like; Mekelle [59], Dire Dawa [26], and Arbaminch [57]. The plausible explanation for this might be due to the fact that the advanced age of women is believed to be a risk factor for cervical cancer where this might lead the woman for the repeated visit of health care services. Moreover, women with advanced age might increase the chance of accessing health-related information related to cervical cancer and its screening services which in turn leads them to utilize cervical cancer screening services. In women with advanced age, high parity is also common which is known to be a risk factor for cervical cancer [60] and this might also contribute for cervical cancer screening.
Participants with high partner educational status were more likely to use cervical cancer screening than those with partner educational status of unable to read and write. This finding was found to be consistent with the studies conducted in Ghana [61], Kenya [62] and in different parts of Ethiopia like; Jimma [22], Debre Markos [25], and Shabadino [21]. This could be due to the fact that educated women have access to different health-related information including the severity of cervical cancer and the benefit of cervical cancer screening utilization.
In this study, the first sexual intercourse before eighteen years was also found to be a strong predictor variable for cervical cancer screening utilization. This finding is consistent with the study conducted in Debre Markos [25]. The possible explanation for this might be women who started sexual intercourse at an early age, may have increased lifetime sexual partners which in turn increase the chance of being infected with sexually transmitted infection (STI) with its signs and symptoms which lead to visit health facilities.
Ever use of alcohol was found to be associated with cervical cancer screening. This finding is in line with the study conducted in USA [63]. These findings give evidence to the idea that alcoholic women are at higher risk for the progression from human papillomavirus infection to the in situ cervical cancer and invasive cervical cancer [64]. This health constraint of women will probably enable them to visit health institutions for cervical cancer screen utilization.
The good knowledge status of the participants was more likely to use cervical cancer screening than their counterparts. This result was congruent with different studies conducted in Kenya [65], Jamaica [32], Tanzania [39], Japan [66], China [67], Dire Dawa [26] and, Finote Selam, Ethiopia [68]. This may be due to the fact that women with good knowledge about cervical cancer will have a better understanding of risk factors, clinical manifestations, complications, and prevention and treatment options, for instance; cervical cancer screening procedure and cryotherapy. Therefore, knowledge on cervical cancer will contribute for the good practice of cervical cancer screening utilization.
Participants with favorable attitudes were found to be associated with cervical cancer screening utilization. Similarly, other studies conducted in Ethiopia, like in Hosanna [69], Mekelle [59], Gondar [55], and Finote Selam [68] also support our finding. This could be explained by that the women with favorable attitudes will have good perceptions (perceived benefit, perceived susceptibility, perceived severity, and perceived barrier) towards the cervical cancer prevention and control mechanisms which imposes the women to engage in cervical cancer screening utilization [70].
Furthermore, in this study, women with high perceived benefits were more likely to use the screening service. Similarly, this is supported by the study conducted in Arsi, Southeastern Ethiopia [71]. A possible explanation for this might be the perception towards the positive consequences secondary to the utilization of cervical cancer screening will help the women to be aware of the procedure properly, and it will also direct them to be engaged in cervical cancer screening utilization.
This study has its own limitations. First, since cross-sectional study design was implemented, it can’t establish a cause-effect relationship between the independent variables and dependent variables (cervical cancer screening utilization). Second, behavioral characteristics like alcohol utilization were not measured for its concentration of different types of alcohol. Despite these limitations, the result of this study may provide important insight for the policymakers and concerned bodies at different health sectors.
Conclusion
In this study, the cervical cancer screening utilization was relatively low. Different predictors like; the age of participants, partner educational status, age at first sex, ever use of alcohol, overall knowledge, overall attitude, and perceived benefit were found to be strong predictors of cervical cancer screening utilization. Therefore, promotion of the perception of women towards cervical cancer screening, and provision of health-related information towards different behavioral-related factors should have to be addressed at each level of health care.
Availability of data and materials
All relevant data are included within the manuscript, but any additional data required are available from the primary author, [Alemayehu Sayih Belay], upon request. Email: Alex.sayihalem2018@gmail.com.
Abbreviations
- AOR:
-
Adjusted Odd Ratio
- CI:
-
Confidence Interval
- COR:
-
Crude Odd Ratio
- ETB:
-
Ethiopian Birr
- FMOH:
-
Federal Ministry of Health
- HIV:
-
Human Immunodeficiency Virus
- HPV:
-
Human Papillomavirus
- IQR:
-
Inter Quartile Range
- LMICs:
-
Low- and Middle-Income Countries
- PPS:
-
Population Proportion to Size
- SD:
-
Standard Deviation
- SPSS:
-
Statistical Package for The Social Sciences
- STD:
-
Sexual Transmitted Disease
- VIA:
-
Visual Inspection with Acetic Acid
- WHO:
-
World Health Organization
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
WHO. Africa - Global Cancer Observatory (GLOBOCAN 2020). 2020.
WHO. Ethiopia - Global Cancer Observatory (GLOBOCAN 2020) 2020 [Available from: https://gco.iarc.fr/today/data/factsheets/populations/231-ethiopia-fact-sheets.pdf.
WHO. Human papillomavirus (HPV) and cervical cancer 11 November 2020 [Available from: https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer.
Castle PE, Einstein MH, Sahasrabuddhe VV. Cervical cancer prevention and control in women living with human immunodeficiency virus. CA: a cancer journal for clinicians. 2021;71(6):505–26.
Chattopadhyay K, Williamson A-L, Hazra A, Dandara C. The combined risks of reduced or increased function variants in cell death pathway genes differentially influence cervical cancer risk and herpes simplex virus type 2 infection among black Africans and the Mixed Ancestry population of South Africa. BMC Cancer. 2015;15:1–7.
Zhu H, Shen Z, Luo H, Zhang W, Zhu X. Chlamydia trachomatis infection-associated risk of cervical cancer: a meta-analysis. Medicine. 2016;95(13).
Klein C, Kahesa C, Mwaiselage J, West JT, Wood C, Angeletti PC. How the cervical microbiota contributes to cervical cancer risk in sub-Saharan Africa. Front Cell Infect Microbiol. 2020;10:23.
Muntyanu A, Nechaev V, Pastukhova E, Logan J, Rahme E, Netchiporouk E, et al. Risk factors and communities disproportionately affected by cervical cancer in the Russian Federation: A national population-based study. The Lancet Regional Health-Europe. 2022;20: 100454.
Zibako P, Tsikai N, Manyame S, Ginindza TG. Cervical cancer management in Zimbabwe (2019–2020). PLoS ONE. 2022;17(9): e0274884.
Liu Z-C, Liu W-D, Liu Y-H, Ye X-H, Chen S-D. Multiple sexual partners as a potential independent risk factor for cervical cancer: a meta-analysis of epidemiological studies. Asian Pac J Cancer Prev. 2015;16(9):3893–900.
Kashyap N, Krishnan N, Kaur S, Ghai S. Risk factors of cervical cancer: a case-control study. Asia Pac J Oncol Nurs. 2019;6(3):308–14.
Rahmawati DL, Rahayu DE, Hardjito K. Correlation between Oral Contraceptive Use and the Incidence of Cervical Cancer. Poltekita: Jurnal Ilmu Kesehatan. 2023;16(4):497–504.
Feldman CH, Liu J, Feldman S, Solomon DH, Kim SC. Risk of high-grade cervical dysplasia and cervical cancer in women with systemic lupus erythematosus receiving immunosuppressive drugs. Lupus. 2017;26(7):682–9.
Lemp JM, De Neve J-W, Bussmann H, Chen S, Manne-Goehler J, Theilmann M, et al. Lifetime Prevalence of Cervical Cancer Screening in 55 Low-and Middle-Income Countries. JAMA. 2020;324(15):1532–42.
Gelibo T, Roets L, Getachew T, Bekele A. Coverage and factors associated with cervical cancer screening: results from a population-based WHO steps study in Ethiopia. Adv Oncol Res Treat. 2017;1(115):2.
NCDs WT. best buys’ and other recommended interventions for the prevention and control of noncommunicable diseases. Geneva: World Health Organization. 2017.
Organization WH. WHO guidelines for the use of thermal ablation for cervical pre-cancer lesions. 2019.
Federal Ministry of Health E. National Cancer Control Plan of Ethiopia 2016–2020 October 2015 [Available from: https://www.iccp-portal.org/sites/default/files/plans/NCCP%20Ethiopia%20Final%20261015.pdf.
Shiferaw N, Salvador-Davila G, Kassahun K, Brooks MI, Weldegebreal T, Tilahun Y, et al. The single-visit approach as a cervical cancer prevention strategy among women with HIV in Ethiopia: successes and lessons learned. Global Health: Science and Practice. 2016;4(1):87–98.
Kasim J, Kalu A, Kamara B, Alema HB. Cervical Cancer screening service utilization and associated factors among women in the Shabadino District, Southern Ethiopia. Journal of Cancer Epidemiology. 2020;2020.
Nigussie T, Admassu B, Nigussie A. Cervical cancer screening service utilization and associated factors among age-eligible women in Jimma town using health belief model. South West Ethiopia BMC women’s health. 2019;19(1):1–10.
Muluneh BA, Atnafu DD, Wassie B. Predictors of cervical cancer screening service utilization among commercial sex workers in Northwest Ethiopia: a case-control study. BMC Womens Health. 2019;19(1):1–9.
Teame H, Gebremariam L, Kahsay T, Berhe K, Gebreheat G, Gebremariam G. Factors affecting utilization of cervical cancer screening services among women attending public hospitals in Tigray region, Ethiopia, 2018; case control study. PLoS ONE. 2019;14(3): e0213546.
Aynalem BY, Anteneh KT, Enyew MM. Utilization of cervical cancer screening and associated factors among women in Debremarkos town, Amhara region, Northwest Ethiopia: Community based cross-sectional study. PLoS ONE. 2020;15(4): e0231307.
Belay Y, Dheresa M, Sema A, Desalew A, Assefa N. Cervical Cancer Screening Utilization and Associated Factors Among Women Aged 30 to 49 Years in Dire Dawa, Eastern Ethiopia. Cancer Control. 2020;27(1):1073274820958701.
Idowu A, Olowookere SA, Fagbemi AT, Ogunlaja OA. Determinants of cervical cancer screening uptake among women in Ilorin, North Central Nigeria: a community-based study. Journal of cancer epidemiology. 2016;2016.
Mugassa AM, Frumence G. Factors influencing the uptake of cervical cancer screening services in Tanzania: A health system perspective from national and district levels. Nurs Open. 2020;7(1):345–54.
Tigeneh W, Molla A, Abreha A, Assefa M. Pattern of cancer in Tikur Anbessa specialized hospital oncology center in Ethiopia from 1998 to 2010. Int J Cancer Res Mol Mech. 2015;1(1):1.
Binka C, Nyarko SH, Awusabo-Asare K, Doku DT. Barriers to the uptake of cervical cancer screening and treatment among rural women in Ghana. Biomed Res Int. 2019;2019:1–8.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians. 2018;68(6):394–424.
Ncube B, Bey A, Knight J, Bessler P, Jolly PE. Factors associated with the uptake of cervical cancer screening among women in Portland, Jamaica. N Am J Med Sci. 2015;7(3):104.
Fontham ET, Wolf AM, Church TR, Etzioni R, Flowers CR, Herzig A, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA: A Cancer Journal for Clinicians. 2020;70(5):321–46.
Mendes D, Mesher D, Pista A, Baguelin M, Jit M. Understanding differences in cervical cancer incidence in Western Europe: comparing Portugal and England. The European Journal of Public Health. 2018;28(2):343–7.
Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice: Wiley; 2008.
Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2(4):328–35.
Federal Democratic Republic of Ethiopia Ministry of Health. Guideline for Cervical Cancer Prevention and Control in Ethiopia. 2015.
Gebreegziabher M, Asefa NG, Berhe S, Factors affecting the practices of cervical cancer screening among female nurses at public health institutions in Mekelle town, Northern Ethiopia,. a cross-sectional study. J Cancer Res. 2014;2016:2016.
Kileo NM, Michael D, Neke NM, Moshiro C. Utilization of cervical cancer screening services and its associated factors among primary school teachers in Ilala Municipality, Dar es Salaam. Tanzania BMC Health Serv Res. 2015;15(1):1–9.
Segni MT, Demissie HF, Tadesse DM, Amdemichael R, Mamo YT, Worku A. Level of knowledge and associated factor toward cervical cancer among women age (21–64) years visiting health facilities in Gulele sub-city Addis Ababa Ethiopia. J Pancreas. 2017;18(1):44–8.
Ibekwe CM, Hoque ME, Ntuli-Ngcobo B. Perceived susceptibility of cervical cancer screening among women attending Mahalapye district hospital. Botswana Southern African J Epidemiol Infect. 2010;25(2):16–21.
LaMorte WW. The Health Belief Model: Behavioral Change Models September 9, 2019 [Available from: https://sphweb.bumc.bu.edu/otlt/mph-modules/sb/behavioralchangetheories/behavioralchangetheories2.html.
Hoque M, Ibekwe C, Ntuli-Ngcobo B. Screening and perceived severity of cervical cancer among women attending Mahalapye District Hospital. Botswana Asian Pacific J Cancer Prev. 2009;10(6):1095–100.
Ibekwe C, Hoque M, Ntuli-Ngcobo B. Perceived benefits of cervical cancer screening among women attending Mahalapye District Hospital. Botswana Asian Pac J Cancer Prev. 2010;11(4):1021–7.
Ibekwe C, Hoque M, Ntuli-Ngcobo B, Hoque M. Perceived barriers of cervical cancer screening among women attending Mahalapye district hospital, Botswana. Arch Clin Microbiol. 2011;2(1):4.
Kibicho JW. Factors influencing utilization of cervical cancer screening services in Embu hospital, Embu county. Kenya: University of Nairobi; 2014.
Bekela E. Assessment of knowledge and attitude of cervical cancer and screening among primary health care workers of West Wollega Zone, Ethiopia, 2016: Addis Ababa University; 2016.
Tadesse A. CKnowledge, attitude and practice (KAP) towards screening for cervical cancer among Adama University female students, Adama, Ethiopia, 2014, 1–58. Recuperado de: http://etd.aau.edu.et/bitstream/123456789/6303/1/Almaz. 2015;20.
Organization WH. WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention: World Health Organization; 2013.
Wanyenze RK, Bwanika JB, Beyeza-Kashesya J, Mugerwa S, Arinaitwe J, Matovu JK, et al. Uptake and correlates of cervical cancer screening among HIV-infected women attending HIV care in Uganda. Glob Health Action. 2017;10(1):1380361.
Ifemelumma C, Anikwe C, Okorochukwu B, Onu F, Obuna J, Ejikeme B, et al. Cervical cancer screening: assessment of perception and utilization of services among health workers in low resource setting. International J Reprod Med. 2019;2019.
Lyimo FS, Beran TN. Demographic, knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania: three public policy implications. BMC Public Health. 2012;12(1):1–8.
Tekle T, Wolka E, Nega B, Kumma WP, Koyira MM. Knowledge, attitude and practice towards cervical cancer screening among women and associated factors in Hospitals of Wolaita Zone. Southern Ethiopia Cancer Manag Res. 2020;12:993.
Getachew S, Getachew E, Gizaw M, Ayele W, Addissie A, Kantelhardt EJ. Cervical cancer screening knowledge and barriers among women in Addis Ababa, Ethiopia. PLoS ONE. 2019;14(5): e0216522.
Erku DA, Netere AK, Mersha AG, Abebe SA, Mekuria AB, Belachew SA. Comprehensive knowledge and uptake of cervical cancer screening is low among women living with HIV/AIDS in Northwest Ethiopia. Gynecologic Oncol Res Practice. 2017;4(1):1–7.
Ebu NI, Mupepi SC, Siakwa MP, Sampselle CM. Knowledge, practice, and barriers toward cervical cancer screening in Elmina. Southern Ghana Int J Womens Health. 2015;7:31.
Gebru Z, Gerbaba M, Dirar A. Utilization of cervical carcinoma screening service and associated factors among currently married women in Arba Minch Town, Gamo Gofa Zone, Southern Ethiopia 2014.
Chosamata MS, Hong S, Tiraphat S. Determinants of cervical cancer screening utilization among women aged 30–45 years in Blantyre district. Malawi J Public Health Dev. 2015;13(3):19–34.
Bayu H, Berhe Y, Mulat A, Alemu A. Cervical cancer screening service uptake and associated factors among age eligible women in Mekelle Zone, Northern Ethiopia, 2015: a community based study using health belief model. PLoS ONE. 2016;11(3): e0149908.
Muñoz N, Franceschi S, Bosetti C, Moreno V, Herrero R, Smith JS, et al. Role of parity and human papillomavirus in cervical cancer: the IARC multicentric case-control study. Lancet. 2002;359(9312):1093–101.
Kokuro M. Factors affecting the utilisation of cervical cancer screening among women attending health services in the kumasi metropolis of ghana: Stellenbosch: Stellenbosch University; 2017.
Morema EN, Atieli HE, Onyango RO, Omondi JH, Ouma C. Determinants of cervical screening services uptake among 18–49 year old women seeking services at the Jaramogi Oginga Odinga Teaching and Referral Hospital, Kisumu. Kenya BMC Health Serv Res. 2014;14(1):1–7.
Mu L, Mukamal KJ. Alcohol consumption and rates of cancer screening: Is cancer risk overestimated? Cancer Causes Control. 2016;27(2):281–9.
Weiderpass E, Ye W, Tamimi R, Trichopolous D, Nyren O, Vainio H, et al. Alcoholism and risk for cancer of the cervix uteri, vagina, and vulva. Cancer Epidemiol Prev Biomarkers. 2001;10(8):899–901.
Mbaka P, Waihenya R, Oisebe C, Lihana R. Factors affecting the uptake of cervical cancer screening in Mama Lucy Kibaki Hospital, Nairobi. Kenya Cancer Res J. 2018;6:106.
Oba S, Toyoshima M, Ogata H. Association of cervical cancer screening with knowledge of risk factors, access to health related information, health profiles, and health competence beliefs among community-dwelling women in Japan. Asian Pacific J Cancer Prev: APJCP. 2017;18(8):2115.
Leung SS, Leung I. Cervical cancer screening: knowledge, health perception and attendance rate among Hong Kong Chinese women. Int J Womens Health. 2010;2:221.
Geremew AB, Gelagay AA, Azale T. Uptake of pre cervical cancer screening service and associated factors among women aged 30–49 years in Finote Selam town Northwest Ethiopia. Int J Collab Res Intern Med Public Health. 2018;10(2):0-.
Assefa AA, Astawesegn FH, Eshetu B. Cervical cancer screening service utilization and associated factors among HIV positive women attending adult ART clinic in public health facilities, Hawassa town, Ethiopia: a cross-sectional study. BMC Health Serv Res. 2019;19(1):1–11.
Maddux JE, Rogers RW. Protection motivation and self-efficacy: A revised theory of fear appeals and attitude change. Journal of Exp Soc Psych. 1983;19(5):469–79.
Feyisa GC, Temesgen H. Perceived benefits and barriers toward cervical cancer screening among women≥ 15 years in Arsi Zone, Southeastern Ethiopia: Application of the health belief model in a community-based cross-sectional study. J Cancer Res Pract. 2019;6(1):7.
Acknowledgements
We would like to thank the Department of Nursing, College of Medicine and Health Sciences, Mizan Tepi University for giving us this chance to conduct this research. Our grateful thanks also extended to Dr. Yohannes Sisay Molla for his invaluable writing assistance and language editing.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and after ethical clearance was obtained from the research directorate office of the Mizan Tepi University (Ref No: MTU/CHS/16/731/21/13). Written informed consent was obtained from each study participant after explaining the purpose and objectives of the study. For illiterate participants informed consent was taken from their legal guardian after trained interviewers have carefully explained the purpose, benefits, and potential risks before consents were obtained. The interview with study participants was conducted with strict privacy and confidentiality.
Consent for publication
Not applicable.
Competing of Interest
We declare that we have no any conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Belay, A.S., Asmare, W.N. & Kassie, A. Cervical cancer screening utilization and its predictors among women in bench Sheko Zone, Southwest Ethiopia: using health belief model. BMC Cancer 23, 472 (2023). https://doi.org/10.1186/s12885-023-10927-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-10927-x