Abstract
Background
Cancer survivors are able to live much longer today than in the past due to advances in treatment. The promotion of health behaviors is important to address among cancer survivors. Not only can health behaviors reduce the risk of comorbidities, but they may also be key to improving psychological health among cancer survivors, such as psychological distress, perceptions of one’s general health, and distress of cancer mortality (i.e., cancer fatalism). Our overall goal is to 1) determine which individual health behaviors (e.g., fruit consumption, physical activity, and sleep) are associated with psychological health among cancer survivors and 2) determine if the number of health behaviors engaged in is associated with better psychological health among cancer survivors.
Methods
Using data from the HINTS 5 Cycle III survey (N = 856 cancer survivors), we compared whether participants who met guidelines for seven health behaviors (e.g., fruit and vegetable consumption, moderate physical activity, sleep duration) had improved psychological health. Multiple ordinal regression models controlling for sociodemographic variables were used to determine if meeting more recommendations was related to psychological health and then specifically which behaviors were of greatest importance to psychological health.
Results
Meeting guidelines for sleep quality and moderate physical activity was associated with higher general health and meeting guidelines for vegetable intake and better sleep quality was associated with less psychological distress. Although the associations were not significant, cancer survivors who met more of the health behavior guidelines reported higher general health, lower psychological distress, and less distress about what could be done to lower one’s chances to get cancer.
Conclusions
Meeting the guidelines for individual and multiple health behaviors is associated with favorable psychological health among cancer survivors. The findings can contribute to the development of health behavior interventions that focus on multiple health behaviors to improve psychological health and quality of life among cancer survivors.
Similar content being viewed by others
Background
In 2019, the number of cancer survivors was estimated to be 16.9 million, with the number expected to grow past 22 million by 2030 [1]. As the United States lifespan continues to rise, so does the risk of cancer development, particularly among the older adult population [2]. Despite increasing incidence rates in cancer over the past 20 years, survival rates have improved due to improvements in medical treatment [1, 3]. With more people living longer after a cancer diagnosis, improving psychological health among cancer survivors is of the utmost importance since it is linked to adherence to treatment [4] and mortality [5]. Understanding how best to improve psychological health among cancer survivors could indeed improve the quality of life among the growing number of cancer survivors as poor psychological health is common among cancer survivors [1]. Engagement in health behaviors is one way to improve the psychological health of cancer survivors [6]. However, additional research is needed to determine which health behaviors are most beneficial for psychological health among cancer survivors. The goal of the current study is to examine the association between different health behaviors and psychological health among cancer survivors.
In general, many studies and reviews have observed positive associations between various healthy lifestyle behaviors (e.g., physical activity, healthy eating, strength training) and psychological health (e.g., depression, general well-being, distress), in both clinical and nonclinical populations [7,8,9,10]. For instance, Lee and Howard [8] found increased physical activity was associated with positive emotions among older adults. Additionally, Parletta and colleagues [10] measured the effects of a Mediterranean diet intervention (e.g., high consumption of fruits, vegetables, cereals, legumes, and to a lesser extent, fish and dairy products) and found improvements in depressive symptoms over a 6-month period.
Among cancer survivors, healthy lifestyle behaviors have also been shown to be associated with psychological health. In a study of breast cancer survivors, those who engaged in more physical activity reported better health-related quality of life than survivors who were less active [11]. Hawkes and colleagues [12] conducted an intervention targeting multiple health behaviors in colorectal cancer survivors. They found distress was lower in the intervention group compared to a control group. Together, these studies demonstrate an association between healthy lifestyle behaviors and improved psychological health.
Healthy lifestyle behaviors can also be associated with another measure of psychological health: fatalistic beliefs about cancer (i.e., cancer fatalism). Cancer fatalism is the belief that there is little a person can do to prevent cancer or mitigate the health outcomes of cancer [13] and can be considered a specific type of distress. Cross-sectional studies have found that greater cancer fatalism is associated with less engagement with preventive health behaviors (e.g., lower fruit and vegetable intake) [14, 15]. Although no causal assessments have been made, it is possible that the association between cancer fatalism and healthy lifestyle behaviors is bidirectional. Cancer survivors are at risk of cancer recurrence or secondary cancer, so fears related to cancer are still relevant in the cancer survivor population. Being healthy by engaging in physical activity, having a balanced diet, and engaging in other health behaviors could reduce the belief that cancer is a potential “death sentence”, engendering a more optimistic outlook and self-efficacy in coping with the disease. Thus, in addition to examining the association between health behaviors and psychological health, it would be valuable to also better understand the association between health behavior engagement and cancer fatalism.
The purpose of this study is to examine the association between different health behaviors (i.e., fruit and vegetable consumption, sleep quality and duration, moderate physical activity [MPA], strength training, and low sedentary behavior) and psychological health (i.e., psychological distress, general health, and cancer fatalism) among cancer survivors. It is not clear if it is important to target specific health behaviors over others as a means of improving psychological health or if multiple behaviors should be targeted. In a non-cancer survivor cohort, Duncan and colleagues [16] developed an index score consisting of various unhealthy behaviors, such as smoking and physical inactivity and found individuals with higher index scores (i.e., engagement in more unhealthy behaviors) reported poorer health. A similar index could be created for healthy behaviors, such as physical activity and sleep. We hypothesized that meeting health behavior guidelines would be associated with favorable psychological health. The psychological health indicators include psychological distress, general health and cancer fatalism.
Methods
Participants
The data were obtained from the Health Information National Trends Survey (HINTS), a nationally representative sample of American adults that is publicly available for analysis. Data are collected annually, with questions focusing on perceptions of cancer (e.g., It seems like everything causes cancer), health behavior engagement (e.g., About how many cups of vegetables do you eat or drink each day?), health communication (e.g., Used e-mail or the Internet to communicate with a doctor or a doctor’s office), and health information technology (e.g., In the last 12 months, have you used an electronic medical device to monitor or track your health? For example a glucometer or digital blood pressure device). Participants who completed the HINTS 5 Cycle III survey were included in the study, with responses from 5438 participants. Since the focus of the investigation was on cancer survivors, only adults who answered “Yes” (N = 856) to the following question were actually included in the analyses: “Have you ever been diagnosed with having cancer?” See Nelson et al. [17] or the HINTS website (https://hints.cancer.gov/) for additional information on the survey instruments used and the overall methodology. Since the data are publicly available, approval from the Institutional Review Board was not required.
Variables
The outcome variables were psychological distress, general health and cancer fatalism. The Patient Health Questionnaire-4 (PHQ-4) [18], is a 4 item self-report assessment of psychological distress related to both depression and anxiety. Higher scores suggest higher levels of psychological distress, with scores ranging from 0 to 12. There are four categories of psychological distress based on PHQ-4 score: None (0-2), Mild (3-5), Moderate (6-8), and Severe (9-12). Participants were categorized into one of the four groups, with 1 corresponding with “None” and 4 corresponding to “Severe.” General health was measured by the following question: “In general, would you say your health is …” , with participants responding on a 5-point scale from “Poor” to “Excellent.” This measure of health has been used in many previous studies, with evidence of its validity [19, 20].
Cancer fatalism was measured with three items: 1) “It seems like everything causes cancer” 2) “There’s not much you can do to lower your chances of getting cancer” and 3) “There are so many different recommendations about preventing cancer, it’s hard to know which ones to follow.” Participants responded on a 4-point scale from “Strongly agree” to “Strongly disagree” for each item. The cancer fatalism items were reverse coded so that “Strongly disagree” was 1 and “Strongly agree” was 4. Thus, higher scores on the cancer fatalism items suggested more fatalistic views about cancer. Given a relatively low Cronbach’s α of .63 and moderate inter-correlations (i.e., rs ranging from .31 to .42), each item was examined as a separate outcome.
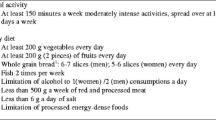
The health behaviors included amount of at least moderate physical activity (MPA), strength training, fruit/vegetable consumption, amount of nightly sleep (henceforth sleep duration), sleep quality, and low sedentary behavior. Participants provided the number of days they engaged in MPA, along with the number of minutes spent engaging in MPA [21]. These two numbers were multiplied together to obtain weekly minutes engaged in MPA. Cancer survivors who exercised for 150 minutes or more a week were categorized as meeting the MPA guideline [22]. Strength training was obtained by asking participants the following: “In a typical week, outside of your job or work around the house, how many days do you do leisure-time physical activities specifically designed to strengthen your muscles?” Participants could provide “None” to “7 days.” Participants who did strength training two or more days a week were categorized as meeting the guideline [22].
For fruit and vegetable consumption, participants answered the following questions: “About how many cups of fruit (including 100% pure fruit juice) do you eat or drink each day?” and “About how many cups of vegetables (including 100% pure vegetable juice) do you eat or drink each day?” Respondents selected from the following options for both questions: “None”, “1/2 cup or less”, “1/2 cup to 1 cup”, “1 to 2 cups”, “2 to 3 cups”, “3 to 4 cups”, or “4 or more cups”. Respondents who reported eating at least “2 to 3 cups” of fruit were categorized as eating sufficient fruit. The same threshold was used for respondents who reported eating at least “2 to 3 cups” of vegetables. These thresholds were chosen according to the United States Department of Agriculture (USDA) as 1½ to 2 cups of fruit and 2 to 3 cups of vegetables are generally recommended [23, 24]. Since those who consume only 1 cup of fruit do not meet the USDA guidelines and half servings were not asked in the survey, it was decided to be more conservative and select 2 to 3 cups of fruit as the cut-off rather than 1 to 2 cups.
Participants reported their sleep quality over the past 7 days using a 4-point scale composed of “Very bad”, “Fairly bad”, “Fairly good”, and “Very good.” There are no specific guidelines for sleep quality, but for consistency with other behaviors we coded “Fairly good” or “Very good” as “good sleep quality”. For sleep duration, participants reported the average hours they slept per night over the past seven days. Participants who reported 7 to 9 hours of sleep were categorized as meeting the guideline for sleep duration [25].
Lastly, participants provided the number of hours they spent sitting. There is no established standard of what constitutes too much sedentary behavior; however, given evidence that many Americans spend half of their day or more sitting [26, 27], 8 hours was selected as the cut-off. Thus, cancer survivors who reported 8 hours or less of time spent sitting were categorized as having low sedentary levels and meeting the low sedentary “recommendation guideline”. Although physical activity and sedentary behavior are correlated, individuals who are physically active can still be too sedentary (“active couch potato”) and experience the negative effects of high levels of sedentary behavior [28]. Since sedentary behavior can be an independent predictor of health even when factoring in physical activity levels, we included it as an independent health behavior.
Basic sociodemographic/control variables were also included: age, gender, income, education, race/ethnicity, urban/rural environment, and time since cancer diagnosis. Given type of cancer can influence the psychological health of cancer survivors, we coded for cancer type: skin (non-melanoma), gynecologic, genitourinary, gastrointestinal, breast, and other. Those who had more than one cancer diagnosis were placed in a “more than one cancer diagnosis” group. Additionally, at-risk health behaviors and physical health problems are likely to be associated with both the predictors and outcomes. We included the number of comorbidities the cancer survivors had by including the following health issues: diabetes, hypertension, lung disease, obesity, and heart condition. A total score was created by summing up the number of comorbidities the cancer survivor had (i.e., scores could range from 0 to 5). We also included smoking status and alcohol consumption. Participants who answered “Every day” and “Some days” to the question “How often do you now smoke cigarettes” were considered current smokers. Participants who consumed alcohol at least once per week over the past 30 days were considered consumers of alcohol.
Data Analysis
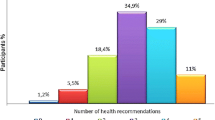
Sample characteristics were calculated for the demographic variables, using survey weights to estimate the national percentage. Means and standard deviations were calculated for all of the variables included in the analyses. For all seven of the health behaviors, meeting a recommended guideline was coded as 1 and not meeting the guideline was coded as 0. The health factor score was computed by adding up each of the guideline behaviors to obtain an overall health factor score with higher scores suggesting engagement in more health behaviors. Scores ranged from 0 to 7. Based on unweighted percentages, 3.1, 10.9, 20.3, 26.3, 18.7, 14.2, 4.5, and 2.0% of participants met the guideline for zero, one, two, three, four, five, six, and seven health behaviors, respectively. The weighted mean of number of guidelines met was 3.17 (SD = 1.51).
Ordinal regression was used to assess the associations between the outcome variables (psychological distress, general health, and three cancer fatalism variables) and the predictor variables (7 lifestyle behaviors as independent variables or as an index) controlling for covariates (age, gender, income, education, race/ethnicity, urban/rural environment, time since cancer diagnosis, overweight/obese, cancer type, comorbidities, smoking status, and alcohol consumption). Given our interest in assessing the associations between the individual health behaviors and the outcome variables and the composite health factor score, ten ordinal regression models were examined. In the first set of five models, each outcome variable (psychological distress, general health, and three cancer fatalism variables) was regressed on the seven health behaviors controlling for the covariates. In the second set of five models, each outcome variable was regressed on the health factor score controlling for the covariates.
It is possible that there is a point of diminishing returns with respect to the number of health behaviors in which people report engaging. In order to test for potential curvilinear relationships, the health factor score was squared and included as an additional predictor. Since the curvilinear term was added, both the health factor and health factor squared terms were mean centered when included in the analyses.
Given HINTS data are collected using a complex sampling method, analyses were conducted using weights provided by the HINTS study. The jackknife replication method was used for the weighted analyses. All descriptive statistics were conducted in R and all regression analyses were conducted in Mplus Version 8.3.
Results
Descriptive Statistics
Table 1 includes sample characteristics of the cancer survivors, while Table 2 includes the mean of the psychological health variables. The average age of the cancer survivors was 63.31 (SD = 16.00). The majority of cancer survivors were female (56.25%). Most cancer survivors were either overweight (38.68%) or obese (30.98%). The average time from cancer diagnosis was 12.29 (SD = 12.09). When examining the health behaviors guidelines, the majority of cancer survivors achieved guidelines for sleep quality, sleep duration, and low sedentary behavior, but not for the other four health behaviors. When considering the individual guidelines, 17.14% met the fruit guideline, 23.22% met the vegetable guideline, 76.60% met the sleep quality guideline, 59.32% met the sleep duration guideline, 31.85% met the MPA guideline, 31.04% met the strength training guideline, and 71.43% met the low sedentary behavior guideline.
Ordinal Regression Results
Tables 3 and 4 includes the ordinal regression results (i.e., odds ratios, 95% confidence intervals, and p-values) of the five models that include the seven health behaviors, controlling for the covariates. As can be seen in Tables 3 and 4, individuals who met the recommended guidelines for vegetable consumption (OR = 0.43, p < 0.001) and sleep quality (OR = 0.54, p = 0.003) reported lower psychological distress scores. Individuals who met the recommended guidelines for sleep quality (OR = 1.73, p = 0.002) and MPA (OR = 1.88, p = < 0.001) reported better general health. Fruit consumption, sleep duration, strength training, and sedentary behavior were not associated with any of the psychological health measures. No significant associations were found between the health behavior guidelines and cancer fatalism, except individuals who met the recommended guidelines for MPA were more likely to report there was not much that could be done to lower one’s chances of getting cancer.
Tables 5 and 6 includes the results of the five models with the overall health factor score, controlling for the covariates. As can be seen, although a higher health factor score was associated with a lower psychological distress score (OR = 0.68, p = 0.084), this association was not significant. The health factor score was also associated with a higher general health score (OR = 1.39, p = 0.055), although this association was also not significant. None of the cancer fatalism variables were significantly associated with the health factor score. However, cancer survivors with a higher health factor score were less likely to agree that there was not much that could be done to lower one’s chances of getting cancer (OR = 0.75, p = 0.082). None of the curvilinear associations tested were significant, which indicated there were linear rather than nonlinear associations.
Discussion
Summary of the findings
Overall, the results show that several of the health behaviors we evaluated were associated with indicators of psychological health. Sleep quality was the only health behavior associated with multiple psychological health indicators, while vegetable consumption was only associated with psychological distress and MPA was only associated with general health. Although sleep duration was not associated with the psychological health indicators, prior research has shown sleep duration and quality are related, but distinct constructs [29]. In fact, in previous research, sleep quality has been shown to generally be a stronger predictor of psychological outcomes than sleep duration [30], which is consistent with our results.
When the health behaviors were combined to create a health factor score, the health factor score was not significantly associated with any of the indicators of psychological health included in the study. However, there were trends in the hypothesized direction for psychological distress and general health, which suggests there could be potential benefits of engaging in multiple health behaviors. However, there was no point of diminishing returns when considering a curvilinear association between the health factor score and the psychological health measures. In other words, cancer survivors can continue to reap benefits of each additional health behavior they engage in, rather than only receive marginal benefits for each health behavior. Given the cross-sectional nature of this data, however, this deserves further study within the context of a randomized controlled trial (RCT). For example, an RCT could include different conditions of varying number of health behaviors. One condition could be focused on only increasing moderate levels of physical activity among cancer survivors, while another condition focuses on increasing engagement in multiple health behaviors, such as simultaneously increasing daily vegetable intake, improving quality of sleep, and increasing moderate levels of physical activity. These conditions can be compared to a control group of cancer survivors who do not change their health behavior engagement.
When considering the health behaviors individually, health behavior engagement was not associated with cancer fatalism in these data, except for the belief that there is not much that could be done to lower one’s chances of getting cancer and MPA. Prior research has found a link between cancer fatalism and health behaviors [14, 15], however, this was observed among individuals without cancer. The null relationships between health behavior engagement and cancer fatalism here may be related to our focus on cancer survivors. Because of their experience, cancer survivors may have a different perspective of what cancer fatalism means to them. Among cancer survivors, even if they have less cancer fatalistic beliefs, they may not change their behavior. They may understand that cancer is not a death sentence or inevitable, but they may not see the point to change their behaviors if they already have cancer, even though they can get an additional diagnosis. It is unclear why those who met the MPA guideline were more likely to believe that there is not much that could be done to lower one’s chances of getting cancer. Given that it was the only health behavior to be associated with any of the cancer fatalistic variables and it was in the opposite hypothesized direction, the finding should be interpreted with caution.
Strengths, Limitations, and Future Directions
There are several limitations that should be considered within the context of the findings. HINTS is a self-report cross-sectional study and the direction of the association (do health behaviors predict psychological health or is it vice versa) is not clear due to possible reverse causality. Self-report studies are also prone to recall bias, particularly when participants are told to recall feelings or behaviors over a period of time [31]. Of the measures included in the analyses, subjective measures of physical activity are known to have validity issues compared to objective measures, such as accelerometers [32]. Even though the dataset was nationally representative, most of the cancer survivors were 51 and older. The results may differ for a study focused on young cancer survivors. Additionally, the cancer fatalism items have been used in past research examining HINTS datasets, but there has been inconsistency in whether researchers combine these items or only use one item in their analysis [33,34,35].
Despite some of these limitations, there are a number of strengths. By analyzing data from a national dataset, the generalizability of the results is higher than if data were collected at only the local or regional level. We included a wide range of confounding variables (e.g., income), that otherwise could have explained the associations between the health behaviors and outcomes. Prior research has typically focused on one or two health behaviors [8,9,10]; we focused on seven different health behaviors in their associations with psychological health. This shows that a wide variety of health behaviors could be beneficial for health. Additionally, sleep is generally understudied compared to other health behaviors; our study included both sleep quality and duration.
While continued research is needed, there are some practical implications worth highlighting. First, there is growing interest in developing interventions to improve psychological health among cancer survivors [36]. Our findings provide evidence that health behaviors and psychological health are related, and that the number of health behaviors a cancer survivor engages in could be positively associated with psychological health. In order to lead to the best improvements in psychological health among cancer survivors, implementation scientists could develop interventions focusing on multiple health behaviors, rather than just one behavior. This also suggests that interventions should really focus on improving the sleep quality of cancer survivors. This can be done by setting up daily routines that can lead to improved sleep quality (e.g., regular sleep and wake times, reducing the use of screen time prior to bedtime).
However, care should be taken when considering the development of interventions to improve sleep quality among cancer survivors. It is possible certain cancer treatments have an influence on both psychological health and health behavior engagement [37,38,39], which we were not able to consider. For example, chemotherapy-induced peripheral neuropathy after treatment has been shown to be associated with less physical activity [40]. Cancer treatment has been shown to increase feelings of depression and anxiety [41, 42], which could interfere with the positive benefits of the health behaviors.
Conclusions
Engaging in health behaviors is positively associated with better psychological health among cancer survivors. This is consistent with prior research showing the long-term benefits of health behaviors on psychological health [43, 44]. This association is not only found when considering the health behaviors individually, but also when considering the health behaviors together (although the findings are non-significant). When considering our findings at a broader level, there are implications for the development of interventions to improve psychological health among cancer survivors.
Availability of data and materials
The dataset analyzed during the current study is available on the NCI HINTS website, https://hints.cancer.gov/data/download-data.aspx
Abbreviations
- MPA:
-
moderate physical activity
- HINTS:
-
Health Information National Trends Survey
- PHQ-4:
-
Patient Health Questionnaire-4
References
Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69(5):363–85. https://doi.org/10.3322/caac.21565.
White MC, Holman DM, Goodman RA, Richardson LC. Cancer risk among older adults: time for cancer prevention to go silver. Gerontologist. 2019;59(S1):S1–6. https://doi.org/10.1093/geront/gnz038.
Brenner H, Bouvier AM, Foschi R, Hackl M, Larsen IK, Lemmens V, et al. Progress in colorectal cancer survival in Europe from the late 1980s to the early 21st century: the EUROCARE study. Int J Cancer. 2012;131(7):1649–58. https://doi.org/10.1002/ijc.26192.
Hurtado-de-Mendoza A, Jensen RE, Jennings Y, Sheppard VB. Understanding breast cancer survivors' beliefs and concerns about adjuvant hormonal therapy: promoting adherence. J Cancer Educ. 2018;33(2):436–9. https://doi.org/10.1007/s13187-017-1180-0.
de Rooij BH, Thong MSY, van Roij J, Bonhof CS, Husson O, Ezendam NPM. Optimistic, realistic, and pessimistic illness perceptions; quality of life; and survival among 2457 cancer survivors: the population-based PROFILES registry. Cancer. 2018;124(17):3609–17. https://doi.org/10.1002/cncr.31634.
Long TM, Rath SR, Wallman KE, Howie EK, Straker LM, Bullock A, et al. Exercise training improves vascular function and secondary health measures in survivors of pediatric oncology related cerebral insult. PLoS One. 2018;13(8):e0201449. Published 2018 Aug 9. https://doi.org/10.1371/journal.pone.0201449.
Mujcic R, Oswald J, A. Evolution of well-being and happiness after increases in consumption of fruit and vegetables. Am J Public Health. 2016;106(8):1504–10. https://doi.org/10.2105/AJPH.2016.303260.
Lee B, Howard EP. Physical activity and positive psychological well-being attributes among U.S. Latino older adults. J Gerontol Nurs. 2019;45(6):44–56. https://doi.org/10.3928/00989134-20190426-01.
Sapranaviciute-Zabazlajeva L, Luksiene D, Virviciute D, Bobak M, Tamosiunas A. Link between healthy lifestyle and psychological well-being in Lithuanian adults aged 45-72: a cross-sectional study. BMJ Open. 2017;7(4):e014240. Published 2017 Apr 3. https://doi.org/10.1136/bmjopen-2016-014240.
Parletta N, Zarnowiecki D, Cho J, Wilson A, Bogomolova S, Villani A, et al. A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized controlled trial (HELFIMED). Nutr Neurosci. 2019;22(7):474–87. https://doi.org/10.1080/1028415X.2017.1411320.
Paxton RJ, Phillips KL, Jones LA, Chang S, Taylor WC, Courneya KS, et al. Associations among physical activity, body mass index, and health-related quality of life by race/ethnicity in a diverse sample of breast cancer survivors. Cancer. 2012;118(16):4024–31. https://doi.org/10.1002/cncr.27389.
Hawkes AL, Pakenham KI, Chambers SK, Patrao TA, Courneya KS. Effects of a multiple health behavior change intervention for colorectal cancer survivors on psychosocial outcomes and quality of life: a randomized controlled trial. Ann Behav Med. 2014;48(3):359–70. https://doi.org/10.1007/s12160-014-9610-2.
Klein WM, Ferrer RA, Graff KA, Kaufman AR, Han PK. Perceived ambiguity, fatalism, and believing cancer is more prevalent than heart disease. Am J Prev Med. 2014;46(4):e45–7. https://doi.org/10.1016/j.amepre.2014.01.003.
Welch JD, Ellis EM. Sex differences in the association of perceived ambiguity, cancer fatalism, and health-related self-efficacy with fruit and vegetable consumption. J Health Commun. 2018;23(12):984–92. https://doi.org/10.1080/10810730.2018.1534905.
Kim HK, Lwin MO. Cultural determinants of cancer fatalism and cancer prevention behaviors among Asians in Singapore. Health Commun. 2021;36(8):940–9. https://doi.org/10.1080/10410236.2020.1724636.
Duncan MJ, Kline CE, Vandelanotte C, Sargent C, Rogers NL, Di Milia L. Cross-sectional associations between multiple lifestyle behaviors and health-related quality of life in the 10,000 Steps cohort. PLoS One. 2014;9(4):e94184. Published 2014 Apr 8. https://doi.org/10.1371/journal.pone.0094184.
Nelson DE, Kreps GL, Hesse BW, Croyle RT, Willis G, Arora NK, et al. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun. 2004;9(5):443–60. https://doi.org/10.1080/10810730490504233.
Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–21. https://doi.org/10.1176/appi.psy.50.6.613.
Garbarski D. Research in and prospects for the measurement of health using self-rated health. Public Opin Q. 2016;80(4):977–97. https://doi.org/10.1093/poq/nfw033.
Maddox GL, Douglass EB. Self-assessment of health: a longitudinal study of elderly subjects. J Health Soc Behav. 1973;14(1):87–93.
Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System 2019. Available from: https://www.cdc.gov/brfss/ index.html. Accessed 27 Jan 2021.
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The Physical Activity Guidelines for Americans. JAMA. 2018;320(19):2020–8. https://doi.org/10.1001/jama.2018.14854.
U.S. Department of Agriculture. Fruits. https://www.choosemyplate.gov/eathealthy/fruits. Accessed September 29, 2020.
U.S. Department of Agriculture. Vegetables. https://www.choosemyplate.gov/eathealthy/vegetables. Accessed September 29, 2020.
Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–3. https://doi.org/10.1016/j.sleh.2014.12.010.
Eanes L. CE: Too much sitting: A newly recognized health risk. Am J Nurs. 2018;118(9):26–34. https://doi.org/10.1097/01.NAJ.0000544948.27593.9b.
Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol. 2008;167(7):875–81.
Lepp A, Barkley JE. Cell phone use predicts being an "active couch potato": results from a cross-sectional survey of sufficiently active college students. Digit Health. 2019;12(5):2055207619844870. https://doi.org/10.1177/2055207619844870.
Pilcher JJ, Ginter DR, Sadowsky B. Sleep quality versus sleep quantity: relationships between sleep and measures of health, well-being and sleepiness in college students. J Psychosom Res. 1997;42(6):583–96. https://doi.org/10.1016/s0022-3999(97)00004-4.
Litwiller B, Snyder LA, Taylor WD, Steele LM. The relationship between sleep and work: a meta-analysis. J Appl Psychol. 2017;102(4):682–99. https://doi.org/10.1037/apl0000169.
Blome C, Augustin M. Measuring change in quality of life: bias in prospective and retrospective evaluation. Value Health. 2015;18(1):110–5. https://doi.org/10.1016/j.jval.2014.10.007.
Reilly JJ, Penpraze V, Hislop J, Davies G, Grant S, Paton JY. Objective measurement of physical activity and sedentary behaviour: review with new data. Arch Dis Child. 2008;93(7):614–9. https://doi.org/10.1136/adc.2007.133272.
Moreno PI, Yanez B, Schuetz SJ, Wortman K, Gallo LC, Benedict C, et al. Cancer fatalism and adherence to national cancer screening guidelines: results from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Cancer Epidemiol. 2019;60:39–45. https://doi.org/10.1016/j.canep.2019.03.003.
Chung JE, Lee CJ. The impact of cancer information online on cancer fatalism: education and eHealth literacy as moderators. Health Educ Res. 2019;34(6):543–55. https://doi.org/10.1093/her/cyz027.
Sinky TH, Faith J, Lindly O, Thorburn S. Cancer fatalism and preferred sources of cancer information: an assessment using 2012 HINTS Data. J Cancer Educ. 2018;33(1):231–7. https://doi.org/10.1007/s13187-016-1115-1.
Berger I, Beck L, Jones J, MacEachen E, Kirsh B. Exploring the needs of cancer survivors when returning to or staying in the workforce. J Occup Rehabil. 2020;30(3):480–95. https://doi.org/10.1007/s10926-020-09877-z.
Daniel LC, Aggarwal R, Schwartz LA. Sleep in adolescents and young adults in the year after cancer treatment. J Adolesc Young Adult Oncol. 2017;6(4):560–7. https://doi.org/10.1089/jayao.2017.0006.
Park H, Jung M, Kim MJ, Min J, Lee CK, Shin SJ, et al. Objectively measured physical activity during chemotherapy in colon cancer patients. Support Care Cancer. 2020;28(6):2597–604. https://doi.org/10.1007/s00520-019-05049-9.
Kelly KM, Bhattacharya R, Dickinson S, Hazard H. Health behaviors among breast cancer patients and survivors. Cancer Nurs. 2015;38(3):E27–34. https://doi.org/10.1097/NCC.0000000000000167.
Mols F, Beijers AJ, Vreugdenhil G, Verhulst A, Schep G, Husson O. Chemotherapy-induced peripheral neuropathy, physical activity and health-related quality of life among colorectal cancer survivors from the PROFILES registry. J Cancer Surviv. 2015;9(3):512–22. https://doi.org/10.1007/s11764-015-0427-1.
Tsaras K, Papathanasiou IV, Mitsi D, Veneti A, Kelesi M, Zyga S, et al. Assessment of depression and anxiety in breast cancer patients: prevalence and associated factors. Asian Pac J Cancer Prev. 2018;19(6):1661–9. Published 2018 Jun 25. https://doi.org/10.22034/APJCP.2018.19.6.1661.
Krebber AM, Buffart LM, Kleijn G, Riepma IC, de Bree R, Leemans CR, et al. Prevalence of depression in cancer patients: a meta-analysis of diagnostic interviews and self-report instruments. Psychooncology. 2014;23(2):121–30. https://doi.org/10.1002/pon.3409.
Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity--a systematic review of longitudinal studies. BMC Public Health. 2013;8(13):813. https://doi.org/10.1186/1471-2458-13-813.
Kim H, Caulfield LE, Rebholz CM. Healthy Plant-Based Diets Are Associated with Lower Risk of All-Cause Mortality in US Adults. J Nutr. 2018;148(4):624–31. https://doi.org/10.1093/jn/nxy019.
Acknowledgements
We would like to thank Jeremy Barsell and Kendall Fugate-Laus, both PhD students at Virginia Commonwealth University, for their feedback and comments on the Background section of the manuscript.
Funding
No specific funding was received for the study. However, the study was supported in part by a National Institute of General Medical Sciences K12 award (2K12GM093857-09) to T.E. Glasgow.
Author information
Authors and Affiliations
Contributions
TEG and BFF conceived the idea for the study. TEG prepared and performed initial analyses. TEG and BFF wrote the initial draft. KPM provided expertise in psychological health among cancer survivors, and edited drafts of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The HINTS dataset is a publicly available dataset that is free for anyone to use. Therefore, Institutional Review Board approval was not required.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Glasgow, T.E., McGuire, K.P. & Fuemmeler, B.F. Eat, sleep, play: health behaviors and their association with psychological health among cancer survivors in a nationally representative sample. BMC Cancer 22, 648 (2022). https://doi.org/10.1186/s12885-022-09718-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09718-7