Abstract
Background
The manner in which bad news is communicated in oncological contexts can affect patients’ engagement, their coping strategies and therapeutic compliance. Although this topic has been broadly investigated since the nineties, to the best of our knowledge, little has been written about Italian patients’ experiences and preferences concerning what the oncologists should disclose and how they should intimate patients about their health conditions in different stages of oncological disease.
Methods
In an attempt to fill this gap, an online self-report questionnaire was administered to a sample of Italian onco-haematological patients. Data were analysed both qualitatively (by a content analysis) and quantitatively (by descriptive analysis and Generalized Linear Mixed Model).
Results
While the majority of patients elected to know the truth during their clinical course, a polarisation between those arguing that the truth be fully disclosed and those claiming that the truth be communicated in a personalised way was observed at the attitude level. Among demographic variables accounted for, age seems to most affect patients’ preferences. Indeed, younger Italian patients decidedly reject concealment of the truth, even when justified by the beneficence principle. This result could be a reaction to some protective and paternalistic behaviours, but it could even reflect a relation according to which the more the age increases the more the fear of knowing rises, or an intergenerational change due to different ways of accessing the information. The qualitative analysis of the final open-ended question revealed three main sources of problems in doctor-patient encounters: scarcity of time, absence of empathy and use of not-understandable language that makes it difficult for patients to assume a more active role.
Conclusions
The results of the present study, which represents a preliminary step in the subject investigation, will be deployed for the construction and validation of a more sophisticated questionnaire. Better awareness of the Italian onco-haematological patients’ preferences concerning bad news communication and truth-telling could be useful in adopting more suitable medical practices and improving doctor-patient relationships.
Similar content being viewed by others
Background
It is known that truth-telling attitudes and practices on breaking bad news during the doctor-patient encounter have been greatly reformed in the past four decades. These have been shifting from full concealment of bad diagnosis or poor prognosis, especially about life-threatening diseases such as cancer, to acknowledgement of the disclosure of health information as every patient’s right. Primarily in oncological contexts, breaking bad news (cancer diagnosis, negative prognosis, relapse post-surgery or treatment, and so on) can significantly impact the patients’ engagement, coping strategies, and therapeutic compliance. Given the importance of this topic—for its clinical, psychological, and social implications—the disclosure of bad news has been broadly investigated since the nineties with respect to physicians’ and patients’ truth-telling preferences and practices.
Thus, doctor-patient negotiation on delivering bad news has been a relevant object of inquiry, through two main research lines: (a) on the one hand, the studies adopting a “medical-centred perspective”, i.e. those mainly focusing on identification and assessment of clinical protocols for communicating bad news [1,2,3,4,5]; and (b) on the other hand, the studies having a “patient-centred perspective”, i.e. those focusing on the patients’ experiences and preferences regarding “what” to know, i.e. what the oncologists should disclose or cover, and “how” to be informed, i.e. how the oncologists should reveal sensitive information [6,7,8,9,10,11,12,13,14,15,16,17,18,19].
Concerning the first line of investigation, three truth-telling models have been identified: non-disclosure, full disclosure and individual disclosure reflecting different relational, communicational and decision-making styles in the doctor-patient relationship [1]. According to Donovan [1], non-disclosure and full-disclosure models can be framed as a paternalistic relationship between physicians and patients, due to the lack of regard for patients’ preferences concerning the timing and the amount of the bad news to be disclosed. Conversely, the individual disclosure model foresees personalised communication between patients and physicians. It implies that patients differ according to the amount of information and time needed to accept and adjust to bad news. Through a negotiation, patients and physicians should clarify the information the patient prefers to know and the best way to communicate it.
Despite the increasing attention towards these communicative aspects as a result of rising awareness of their importance for clinical outcomes, at the onset of the new millennium, contrasts between the physicians’ general attitude and their routine practice in the clinical setting were noted. By investigating the attitudes of a group of physicians regarding truth-telling to cancer patients, Grassi et al. [20 p. 43] discovered that “while about half the sample indicated that, in principle, patients should always be informed of the diagnosis, only one quarter reported that they always disclosed the diagnosis in practice”.
To simplify the arduous task of revealing unpleasant truths, Baile et al. [3] developed one of the best-known protocols for breaking bad news named SPIKES. SPIKES is the acronym for six strategies which, according to the authors, should prove worthwhile in reducing patients’ distress during oncological encounters and which could be used by doctors: Setting up the interview, assessing patients’ Perception (i.e. evaluating their ability to understand), obtaining patients’ Invitation (to be informed or not) and waiting for their possible questions, giving Knowledge and information by avoiding technical terms and pre-announcing bad news, addressing patients’ Emotions with Empathic responses, and sharing Strategy and Summarising. This protocol, as well as other similar ones (e.g. ABCDE [21], and BREAKS [22]), has enjoyed a consistently positive reputation, and it has been utilised for training medical students in breaking bad news [23,24,25,26].
Therefore, where the first line of investigation focuses on how physicians should communicate bad news, the second one pays attention to identifying patients’ preferences. Much research has indeed been carried out with the main purpose of knowing the way in and the extent to which patients prefer to be informed about their cancer, mainly through self-report measures (i.e. questionnaires).Footnote 1 Based on the currently available evidence, it seems fair to suggest that a large majority of patients expect a full disclosure pattern from physicians and pay particular attention to the content of the communication, such as comprehensiveness of the information received or competence of the physicians and, to a lesser extent, to the setting’s aspects, i.e. privacy or time and empathic support [3, 6, 8, 10, 13, 29]. Furthermore, despite the recommendations (see SPIKES), the supportive aspects and physical contact are often evaluated as inappropriate [17]. Similarly, contrary to the expectations, the effects of anticipating bad news (which, at least ideally, should prepare the patient, thus avoiding shocking him/her) do not appear to be significantly associated with a lower degree of patient distress [14].
Although, therefore, much research has been conducted on these topics, most has focused on breaking bad news in general (without explicitly distinguishing between diagnosis and prognosis) and on patient samples mainly from western countries.
On the first aspect, most of these studies deal generically with the communication of bad news, primarily referring to the disclosure of negative diagnoses and disease relapses. Nonetheless, as far as we know, only a few of them explicitly account for the patients’ preferences for communication of undesirable prognosis [14], especially in advanced-stage cancer [30]. This is probably because conveying a bad prognosis is one of the most difficult and complex communicative activities both for patients and for physicians [30,31,32]. These last, as reported by Rodriguez et al. ([33] p. 219), often have difficulties in discussing prognosis because of “the uncertain progression of disease, varied treatment responses, and differences in how patients want to receive this information”, and because of the onerous task of balancing honesty with hope [34]. Regarding the second point, despite the quantum of research just mentioned, to the best of our knowledge, studies on patients from Southern European countries (and more in general on non-western patients) are, at present, fewer in numberFootnote 2; controversial in their results, and, specifically in the Italian context, outdated and mainly focused on patients’ satisfaction [40, 41], demoralisation [42, 43], coping styles [44] etc., i.e. on strictly psychological aspects rather than on communicative preferences.
It is well-known that legal and ethical codes on informed consent and the patient’s right to know have been adopted by many western and eastern countries. Nonetheless, at the practical level, cross-cultural differences seem to resist and influence truth-telling attitudes and acts [3, 45, 46]. This has been observed in the case of Asian countries, such as Japan [47], China [48, 49], Singapore [50, 51]; Middle Eastern countries [52] and Southern European countries, i.e. Greece [53], Spain [54], and Italy [55,56,57].Footnote 3 These nations appear to be characterised by a protective approach to patients; the acceptance of medical authority regarding the decision to reveal the truth or not; the active role attributed to the patient’s family regarding the choice of fully disclosing the truth; and patients’ preferences for partial disclosure concerning bad news, such as poor prognosis or length of survival. Even though the above-mentioned studies seem to confirm the permanence of stereotyped cross-cultural differences, some others appear controversial in their results [16, 32, 58]. Specifically, in the Italian context, Mauri et al. [9 p. 1529] noted some ambiguity among patients “who mostly want to be informed about diagnosis but are confused about this opportunity: the right to be informed in a timely manner to participate in their care is both desired and avoided; a participatory model of relationship that is less asymmetric is not considered as important”.
Since much uncertainty still exists, specifically, about Italian patients’ preferences, the main objectives of this study are (1) to detect their attitudes to the disclosure of the truth about diagnosis and prognosis, and (2) to consider their implications to enhance the communication of bad news within the patient-physician relationship.
This study, which represents a preliminary step in the subject investigation, could shed some light on a poorly investigated topic, thus improving the knowledge of the Italian onco-haematological patients’ preferences concerning bad news communication and truth-telling. Better awareness of these aspects could be beneficial in adopting more suitable medical practices and improving doctor-patient relationships.
Method
Procedures
An exploratory questionnaire made of 20 items has been drafted after five interviews with four physicians (who handle onco-haematological diseases) and two leukaemia patients. The items of the questionnaire (see Table 1 in Section Main Results) have been chosen to identify some relevant dimensions of doctor-patient interaction and are a starting point for building a subsequent questionnaire.
This first version of the questionnaire was administered online (via LimeSurvey, an open-source survey application [59], which limits any possible risk to patients’ confidentiality) in two different periods to six closed Facebook groups of leukaemia patients, who were numerous enough to be representative. The social media site was chosen to speedily recruit the highest possible number of participants afflicted with onco-haematological diseases and then transition to the construction of a new survey.
In the first section of the present questionnaire some information concerning (a) the subjects eligible to compile the questionnaire, i.e. only the patients; (b) the aims of the research; (c) the contacts of one of the researchers (who could be contacted to receive more detailed information about the study and the questionnaire); (d) how the results will be disseminated (scientific publications, workshops, and conferences); and (e) the references to the European and Italian privacy laws and the protection of personal data have been provided.
Since it was an exploratory questionnaire, no pre-test was performed.Footnote 4
After moderators’ approvals, the questionnaire was launched in the first two Facebook groups:
-
1.
“Lotta alla Leucemia, Linfomi e Mieloma, dona il sangue, regala una speranza”/“Fight against Leukemia, Lymphomas and Myeloma, gives blood, gives hope” (a closed group with 7900 members, who are patients and non-patients), and
-
2.
“Trapiantati di midollo, autotrapianto, leucemie, linfomi e mielomi”/“Transplanted marrow, autograft, leukaemia, lymphoma and myeloma” (a closed group with 3330 members. All of those are patients).
The first administration was closed after 2 weeks. A total of 157 patients agreed to participate and completed the questionnaire. Following a common practice, to have a more representative sample, the second administration was shared with other four groups:
-
3.
“Mieloma multiplo Italia esperienze e news”/“Multiple myeloma, Italy experiences and news” (a closed group with 1300 members),
-
4.
“Linfoma non hodgkin” / “Non-hodgkin’s lymphoma” (a closed group with 3200 members)
-
5.
“Linfoma non hodgkin a grandi cellule B mediastino”/“Non-hodgkin’s lymphoma in large B-cell in the mediastinum” (a closed group with 444 members),
-
6.
“Leucemia mieloide cronica”/“Chronic myeloid leukaemia” (a closed group with 303 members).
The second administration was closed after 2 months. A total of 286 patients agreed to participate and completed the questionnaire. Both the choice to run the survey on the other four Facebook groups and to leave it for a longer time had an impact on sample size by increasing the number of respondents and consequently allowing us to better stratify data.
No reminder during the first and the second administration was needed since every time a patient filled the questionnaire and/or added comments, the link for its compilation reappeared among the news of the Facebook groups. We did not offer any prize as an incentive to compile the survey, since it is not a common practice in Italy and as it can also affect the data, by inducing subjects to give socially desirable answers, thus compromising the data reliability [60]. Furthermore, leukaemia patients also seemed to be highly motivated to participate and share their experiences without any prize.
A total of 443 patients completed the questionnaire during the first and second administration. A total of 60 questionnaires have been rejected for lacking one or more demographic responses (age, gender, and level of education). These variables, used as factors in our analyses, are indeed central; therefore, the inclusion of those questionnaires would not have made sense and, on the contrary, it would have been statistically inappropriate. Thus, the final sample included 383 patients.
Data were analysed both quantitatively (through descriptive statistics and GLMM, Generalized Linear Mixed Models) and qualitatively (through a content analysis).
Analysis
Descriptive analysis was performed to detect demographic data, patients’ attitudes, and their experiences. Jasp 0.11.10 software was employed.Footnote 5
Qualitative analysis was applied to the final open-ended question of the questionnaire to know patients’ opinions concerning their views on improvement in patient-physician communication. Specifically, a content analysis was performed on the responses, deriving code categories from the text inductively [63,64,65,66]. Through an initial scoping review of each answer, a first coder (AB, a health sociologist expert in qualitative research and content analysis) created a codebook, with a description of the code system and examples. The coding categories were identified considering the main critical aspects of the patient-doctor communication which emerged from text data. This pilot coding instrument was discussed by two members of the research team (AB and RB), reviewing and resolving discrepancies. In particular, the coders decided to consider in distinct categories the patients who responded that they had no improvement aspects to report and those who pointed out two or more aspects, not classifiable in the other categories identified. Using the finalised codebook, a second coder (RB, a communication psychologist expert in content analysis) coded 21% of the answers (n = 46). Inter-coder reliability was calculated through Cohen’s Kappa, which was on average .83, indicating a high level of reliability.Footnote 6 In order to transform our open-ended responses into nominal-level, we used mlogit.data function of the mlogit package [68] within the R-software (Version 3.6.0, R Core Team, Wien, Austria, 2019).
GLMM (Generalized Linear Mixed Model) was performed, as implemented in the glmer function of the lme4 package [69] within the R-software, to verify if there were significant differences in patients’ responses related to the following demographic variables:
-
gender (male, female),
-
age (18–30; 31–40; 41–50; 51–60; > 60),
-
level of education (junior high school; senior high school; graduate and doctorate).
Every time the variable was dichotomous, therefore, we considered that the statistical distribution was binomial and the link function was “logit”: choice or not choice of a specific response category in interaction with the different levels of the variables under exam. For the multiple comparisons in the post-hoc analysis, we used z-statistic with Bonferroni correction.
The subjects’ identity (ID) has been used since the differences between subjects has been modelled as a random effect. We performed Mixed Model ANOVA Tables via likelihood ratio tests.
The interaction has been limited to two:
-
Gender x Item: male * level 1 vs. female * level 1; male * level 2 vs. female * level 2 etc.
-
Age x Item: “18–30” * level 1 vs. “31–40” * level 1; “18–30” * level 1 vs. “41–50” * level 1 etc.
-
Level of education x Item: junior high school * level 1 vs. secondary school * level 1; junior high school * level 1 vs. degree/graduation and PhD * level 1 etc.
Main results
In the following sections, the results of our analyses will be present separately.
Descriptive statistical analysis
Specifically, in this section, we will present some of the main results of the descriptive analysis. A synopsis is present in Table 1.
As for demographic data, out of 383 patients who fully completed the questionnaire, 279 were women (72.85%) and 104 (27.15%) were men. The mean age was 45.32 years (range 18–83 years). The majority of patients (54.57%) had a secondary school qualification and received the first diagnosis of leukaemia more than a year ago (from when they completed the questionnaire) (80.94%) from the ward physicians (57.70%).
As for patients’ preferences concerning the communication of diagnosis and prognosis (items 6–7) and their attitudes towards doctors’ omission of truth (items 10–11), their answers are slightly different. The sample was split in half concerning the diagnosis communication (item 6), between those who claimed to prefer a full disclosure (192 = 50.13%) and those who claimed to prefer a personalised one (191 = 49.87%). A somewhat different situation was registered for the communication of prognosis (item 7), which, according to a higher percentage of patients (206 = 53.79%), must always be told but in a personalised way. Regarding doctors’ omission of the truth (item 10), almost all patients (321 = 83.81%) claimed that lying is not legitimate behaviour in physicians. Nonetheless, when the physician tells a lie to avoid the patients’ suffering (item 11), the percentage of those who consider this behaviour unjustifiable, and comparable to telling a lie, fell (248 = 64.75%).
As for the patients’ own experiences (items 12–16, 18–20, but also 8–9; see Table 1), the great majority of them (355 = 92.69%) claimed that they always preferred to know the truth (item 12) – because (item 13) it allowed them to better face their illness (263 patients = 74%) – and to have been active and collaborative (299 = 78.07%) during the care pathway (item 16). Nonetheless, most of them also claimed to have been accompanied by one or more people during their first encounter with the doctor (294 = 76.76%), as well as during the subsequent ones (288 = 75.20%) (items 8 and 9, respectively).
Two items (15 and 18; see Table 1) of the questionnaire concerning the patients’ experiences were presented on a Likert scale from 1 to 5 points.
As for item 15, the majority of patients stated that the way used by the physicians to convey information has affected (4 point on a Likert scale) or completely affected (5 point on a Likert scale) their way of coping with illness (122 patients = 31.85% and 151 patients = 39.43%, respectively), recognising, therefore, a central role to the physicians’ communicative styles in managing oncological encounters and in determining their outcomes.
As for item 18, the majority of patients admitted they were satisfied (4 point on the Likert scale = 117 patients = 30.55%) or completely satisfied (5 point on the Likert scale = 136 patients =35.51%) with how the physicians communicated with them.
Finally, as for those aspects that have not worked during the communication with the physicians (item 19), patients could select one or more options from a given list. The majority of them indicated: “the limited time spent during the encounters” (124 patients = 32.38%); “the use of a too technical and/or too difficult language” (79 patients = 20.63%); and “the inability of the physician to comprehend the patient’s needs” (75 patients = 19.58%). Few of them also selected: “the use of a too simplistic language” (20 patients = 5.22%); “the presence of relatives” (19 patients = 4.96%); and “the place for communicating” (16 patients = 4.18%). Specifically, for the “presence of relatives”, although this option was selected by a low percentage of patients, those who chose it were mainly the younger ones (9 out of 19 were 18–30 years old).
Qualitative analysis
The questionnaire concluded with an open-ended question through which the respondents were asked to indicate what could be improved in patient-physician communication. 218 answers were obtained, that is 56,9% of the respondents, among which 162 (74.3%) were females, 56 (25.7%) males, and the median age was 47.12 years.
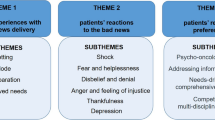
As can be seen from Tables 2, 12 sub-categories have been detected, which include all the answers of patients. Except for “No suggestion” and “Other”, the remaining 10 sub-categories represent the main aspects that should be improved in doctors’ communication from the interviewees’ viewpoint. These sub-categories were subsequently grouped into three categories: Setting, Empathy and Engagement. The three categories were identified considering the content of the answers and grouping together those sub-categories that, by affinity, were addressed to similar communicative, relational or organisational aspects.
The first category Setting (n = 34, 15.6%) includes the sub-categories Time (9.6%) and Organisational setting (6%) and refers to features relating to the setting in which the interaction between doctor and patient takes place. Patients highlight problems such as scarcity of time during medical consultation due to the high number of patients or the absence of a referring physician and the difficulties arising from meeting different doctors every time.
The second category Empathy (n = 57, 26.1%) regards the empathic relationship between patient and physician, and it comprises the sub-categories Understanding (5.5%), Humanity (8.7%) and Empathy (11.9%). This category focuses on patients’ needs for support in their emotional reactions. In the patients’ view, the communication could be ameliorated if the doctor demonstrated more humanity, sympathy, kindness and helpfulness.
Sub-categories that refer to a more active role of patients have been grouped in a third category (“Engagement”, n = 69, 31.7%), which includes the sub-categories Information (9.2%), Engagement (8.3%), Language (6.4%), Listening (4.6%), and Openness (3.2%) and focuses on patients’ involvement in decisions about their condition. These issues directly affect the distribution of knowledge and power within the doctor-patient relationship [70]. Given that technical jargon in a clinical setting can widen the gap in patient-physician understanding and adversely impact patients’ outcomes [71,72,73], patients interviewed prefer a simpler language. Moreover, patients’ demanding to obtain more information, to be heard, to know the truth, and to receive personalised communication could respond to a need for participation in the decision-making process.
Considering the variables gender and level of education, some differences emerged with respect to the categories identified among those who answered the open-ended question (see Table 3). With regard to gender, chi-squared results indicated that differences between women and men were statistically significant (χ2 (4, N = 218) = 20.36, p < .001). Women reported aspects related to both empathy and patient engagement to a greater extent than men, while men felt that there was nothing to improve in doctors’ communication more than women did. Concerning the level of education (χ2 (8, N = 218) = 17.83, p < .05), those with a higher educational qualification identified patients’ engagement and empathy as the main factors for improving the relationship with doctors. Respondents with a junior high school diploma were more inclined not to indicate any aspect of improvement. Instead, there was no significant association between age and the categories identified (χ2 (4, N = 218) = 1.21, p = .876).
GLMM analysis
The GLMM analysis revealed significant differences concerning patients’ experiences and preferences. Specifically, where gender seems to affect mostly patients’ experiences, age and level of education seem to have a higher influence on patients’ preferences, as shown below in detail.
Item (5) the first diagnosis was communicated by the department head, ward doctor, family doctor, doctor undergoing specialised training, other physician, other healthcare worker (nurse), or relative
As shown in Table 1, frequency analyses of the questionnaires show that the communication of the first cancer diagnosis is generally by the ward doctor (221 = 57.7%) and less frequently by department heads (21.41%), family doctors (6.79%), relatives (5.22%), other physicians (4.18%), doctors undergoing specialised training (3.92%), other healthcare workers (0.78%). Nevertheless, the analysis revealed differences statistically significant related to the following:
-
interaction between item 5 levels and levels of education (χ2(12, N = 383) = 21.474, p = .043): specifically, graduate patients more often received the first diagnosis from the department head if compared with junior high school patients (z = 2.555, p = 0.031) and senior high school patients (z = 2.426, p = 0.045); those with low level of education (junior high school certificate) more often received the first diagnosis from one of their own relatives if compared with senior high school certificate (z = 2.499, p = 0.037). Patients with junior school certificate and those with senior high school certificate more often received the first diagnosis by the ward doctor if compared with graduate patients (z = 3.111, p = 0.006) and senior high school patients (z = 3.020, p = 0.007). See Fig. 1(a).
Fig. 1 a Proportion of responses and 95% confidence intervals related to interaction between item 5 levels (The first diagnosis was communicated by department head, ward doctor, family doctor, doctor undergoing specialised training, other physician, other healthcare worker/nurse, or relative) and levels of education: Junior high school, Senior high school, Graduate and doctorate. b Proportion of responses and 95% confidence intervals related to interaction between item 5 levels and age groups: 18–30, 31–40, 41–50, 51–60, > 60. (c) Proportion of responses and 95% confidence intervals related to the interaction between item 6 levels (The truth about diagnosis must be told always and in full or always, but in a personalised way, or never, or other) and levels of education: Junior high school, Senior high school, Graduate and doctorate
-
interaction between item 5 and age (χ2(24, N = 383) = 57.866, p < .001): patients over 60-year-old received more cancer diagnosis from the department head than the other age categories (z = 4.321, p < 0.001 if compared with closest 41–50 years old category). Patients who are between 41 and 50 years old received from the department head cancer diagnosis more often than 18–30, 31–40 and 51–60 age categories (z = 3.907, p < 0.001 if compared with closest 31–40 years old category). Patients over 60-year-old less often than the other age categories received the cancer diagnosis from the ward doctor (z = 4.512, p < 0.001 if compared with closest 41–50 years old category). Patients between 18 and 30 years more often received the cancer diagnosis from one of their relatives than the other age categories (z = 2.588, p = 0.048 if compared with closest 41–50 years old category). See Fig. 1(b).
Item (6) the truth about diagnosis must be told always and in full or always, but in a personalised way, or never, or other
Regarding diagnosis communication, as claimed above (section 3.1), the sample has been split into two parts: on the one hand, those who claimed that the truth must always be told in full (50.1%), and, on the other, those who declared that the truth must always be told, but in a personalised way (49.9%).
The interaction between item 6 and variable level of education seems to significantly affect patients’ responses (χ2(2, N = 383) = 6.715, p = .003). Graduate and doctorate patients (more than others) claimed indeed to believe that truth must always be told, but in a personalised way (z = 2.667, p = 0.022 if compared with closest junior high school category). See Fig. 1(c).
Item (7) the truth about prognosis must be told always and in full; always, but in a personalised way; never; other
Regarding prognosis communication, the analysis did not reveal statistically significant differences related to the interaction between item 7 and gender, age or level of education. Almost all patients claimed to believe that the prognosis must be told (χ2(2, N = 383) = 366.145, p < .001), and the difference with those who claimed that it must be communicated always and in full and those who claimed that it must be communicated in personalised way is not statistically significant. See Fig. 2(a).
a Proportion of responses and 95% confidence intervals related to item 7 levels (The truth about prognosis must be told always and in full; always, but in a personalised way; never; other). b Proportion of responses and 95% confidence intervals related to the interaction between item 8 levels (During the first encounter with the doctor, you were alone or accompanied by one or more people) and gender: Female, Male. c Proportion of responses and 95% confidence intervals related to the interaction between item 9 levels (During the subsequent communication encounter with the doctor you were alone or accompanied by one or more people) and age groups: 18–30, 31–40, 41–50, 51–60, > 60
Item (8) during the first encounter with the doctor, you were alone or accompanied by one or more people
A significant number of patients stated they had gone to the first visit not alone, but accompanied by one or more people. The analysis revealed statistically significant differences related exclusively to the interaction between item 8 and gender (χ2(1, N = 383) = 3.933, p = .047). A significantly higher number of male patients claimed to have gone accompanied by one or more relatives or friends to the first medical encounter if compared with female patients (z = 2.292, p = 0.043). On the contrary, more female than male patients claimed they went alone to the first medical encounter (z = 2.377, p = 0.034). See Fig. 2(b).
Item (9) during the subsequent communication encounter with the doctor you were alone or accompanied by one or more people
Similar to what happened for the first encounter, for the subsequent ones, the majority of patients stated they went with one or more people. Nonetheless, the analysis revealed statistically significant differences related to the following:
-
interaction between item 9 levels and age (χ2(4, N = 383) = 11.810, p = .019): younger patients (18–30) more often claimed to have been accompanied by one or more people during medical visits if compared with patients between 31 and 40 and 41–50 years (z = 2.780, p = 0.027 taking into consideration the closest 41–50 years category). Patients between 51 and 60 stated having been more often accompanied if compared with 31–40 years category (z = 2.678, p = 0.037). See Fig. 2(c).
-
interaction between item 9 levels and level of education (χ2(2, N = 383) = 5.925, p = .050): patients with a low level of education (junior high school certificate) claimed to have been accompanied to medical encounters after the first one more than those with senior high school levels of education (z = 2.481, p = 0.039). See Fig. 3(a).
Fig. 3 a Proportion of responses and 95% confidence intervals related to the interaction between item 9 levels (During the subsequent communication encounter with the doctor you were alone or accompanied by one or more people) and levels of education: Junior high school, Senior high school, Graduate and doctorate. b Proportion of responses and 95% confidence intervals related to the interaction between item 10 levels (Lying to the patient is legitimate or not legitimate) and age groups: 18–30, 31–40, 41–50, 51–60, > 60. c Proportion of responses and 95% confidence intervals related to the interaction between item 11 levels (The doctor who omits a part of the truth to avoid pain to the patient lies or does not lie) and age groups: 18–30, 31–40, 41–50, 51–60, > 60
Item (10) lying to the patient is legitimate or not legitimate
In a statistically significant way, the majority of patients claimed that lying to the patient is not legitimate. Specifically, the interaction between item 10 and variable age significantly affects such a response (χ2(4, N = 383) = 20.068, p < .001). While the younger patients (18–31) claimed that telling a lie to the patients is not a legitimate behaviour, with increasing age, the percentage of those who believe that lying is legitimate also increases. In terms of statistical significance, on the one hand, there are the younger 18–30 and 31–40 years categories, and, on the other hand, there are the other older years categories (z = 2.788, p = 0.026 taking into account the two closest categories, for each of the two age groups, 31–40 and 51–60). See Figu. 3(b).
Item (11) the doctor who omits a part of the truth to avoid pain to the patient lies or does not lie
Similar to our observation for the previous item, also in this case, the majority of patients claimed that the doctor who omits a part of the truth to avoid causing suffering to the patient is telling a lie.
The difference between those patients who claimed that omitting is the same as lying and those who claimed that omitting is different from lying is statically significant and related to the following:
-
interaction between item 11 and age (χ2(4, N = 383) = 37.636, p < .001): for the younger patients (more than the older ones) omitting is the same as lying. The younger patients, more than the older ones, consider omitting part of the truth to be the same as lying. The more the age increases, the more the number of those who consider omitting and lying as the same decreases. In terms of statistical significance, there are two differences, the first between 18 and 30 and all other categories (z = 3.621, p = 0.001 calculated between 18 and 30 and the closest 31–40) and the second between 31 and 40/41–50 and 51–60/> 60 years categories (z = 2.602, p = 0.046 calculated between 41 and 50 and the closest 51–60). See Fig. 3(c).
-
interaction between item 11 and level of education (χ2(2, N = 383) = 5.936, p = 0.05): patients with junior high school certificate considered omitting part of the truth to be the same as lying if compared with graduate and doctorate category (z = 2.542, p = 0.033). See Fig. 4(a).
Fig. 4 a Proportion of responses and 95% confidence intervals related to the interaction between item 11 levels (The doctor who omits a part of the truth to avoid pain to the patient lies or does not lie) and levels of education: Junior high school, Senior high school, Graduate and doctorate. b Proportion of responses and 95% confidence intervals related to the interaction between item 12 levels (During your illness, you have preferred always to know the truth or not always to know the truth) and age groups: 18–30, 31–40, 41–50, 51–60, > 60. c Proportion of responses and 95% confidence intervals related to interaction between item 12 levels and levels of education: Junior high school, Senior high school, Graduate and doctorate
Item (12) during your illness, you have preferred always to know the truth or not always to know the truth
In a statistically significant way, the majority of patients claimed that during their illness they have always preferred to know the truth. The observed differences are related to the following:
-
interaction between item 12 and age (χ2(4, N = 383) = 9.353, p = 0.05): the older patients (> 60) claimed they not always preferred to know the truth if compared with younger categories (z = 2.644, p = 0.041 between > 60 and the closest 18–30 years category). See Fig. 4(b).
-
interaction between item 12 and level of education (χ2(2, N = 383) = 9.381, p = 0.01): patients with lower levels of education (junior high school certificate) have more often claimed that they have not always preferred to know the truth (z = 2.448, p = 0.043 if compared with the closest graduated and doctorate category). See Fig. 4(c).
Item (16) during the care pathway as a patient you have been active and collaborative or passive and non-collaborative or sometimes active and collaborative and sometimes passive and non-collaborative
The majority of patients claimed to have been active and collaborative for the main part of the care pathway. The analysis revealed differences statistically significant related to:
-
interaction between item 16 and age (χ2(12, N = 383) = 53.072, p < 0.001): the more age increases, the more the patients claimed to have been active and collaborative (z = 3.332, p = 0.004 between 18 and 30 and the closest 31–40 years category). Younger patients (18–31) in statistically significant way claimed to have been active and collaborative sometimes only (z = 3.299, p = 0.005 if compared with the closest 31–40 years category). Independent of age, the patients claiming to have been passive and non-collaborative for most of the care pathway are very few in number. See Fig. 5(a).
Fig. 5 a Proportion of responses and 95% confidence intervals related to the interaction between item 16 levels (During care pathway as a patient you have been active and collaborative or passive and non-collaborative or sometimes active and collaborative and sometimes passive and non-collaborative) and age groups: 18–30, 31–40, 41–50, 51–60, > 60. b Proportion of responses and 95% confidence intervals related to the interaction between item 16 levels and gender: Female, Male. c Proportion of responses and 95% confidence intervals related to the interaction between item 16 levels and levels of education: Junior high school, Senior high school, Graduate and doctorate
-
interaction between item 16 and gender (χ2(3, N = 383) = 10.765, p = 0.013): more male patients claimed to have been active and collaborative compared to female patients (z = 2.399, p = 0.033). Female patients more often claimed that they were active and collaborative sometimes only (z = 2.309, p = 0.042). See Fig. 5(b).
-
interaction between item 16 and level of education (χ2(6, N = 383) = 15.436, p = 0.017): a higher number of patients with higher level of education claimed to have been active and collaborative when compared to junior high school level (z = 2.434, p = 0.045 between junior high school and the closest graduate/doctorate level of education). See Fig. 5(c).
Discussion
The present study is a contribution to the ongoing discussions about patients’ preferences for knowing the truth about their health conditions. Particularly, the objective of the paper was to identify onco-haematological Italian patients’ preferences on breaking bad news, regarding the communication of both the diagnosis and the prognosis.
The results of this study revealed an ambiguous stance of Italian patients.
At the practical level, concerning their personal experience, a large majority of the sample chose to know the truth during their clinical course. Despite this, at the attitude level, regarding the way diagnosis and prognosis should be communicated, a polarisation was noted between those who argue for full disclosure and those who prefer to know the truth in a personalised way. As for diagnosis, the individual model is preferred by patients with a higher level of education than those with less education. Concerning the disclosure of prognosis, instead, the desire for an individualised communication increases within the sample, without any significant difference for demographic factors.
Moreover, the legitimisation of concealing the truth presents a dichotomous choice among Italian patients. On the one hand, the majority of the respondents indicate that physicians are not entitled to lie to patients, on the other hand, if the concealment of the truth can avoid causing suffering to patients, the attitudes of the respondents towards the legitimisation of a non-disclosure behaviour increase, especially in older patients. Indeed, Italian younger patients appear to be more inclined to claim a full disclosure style from medical staff, by decidedly rejecting the concealment of the truth, justified by beneficence.
The findings concerning the factor “age” are consistent with previous studies showing that younger patients would seek more engagement in the decision-making process [53, 56, 74,75,76,77]. According to Fujimori and Uchitomi [8], seven of the eight studies examined through a systematic literature review found that younger patients prefer receiving as much information as possible. In general, an explanation of the truth attitudes of younger patients could be related to a stance of sureness, courage and ruthlessness which is believed to exist in young people [53]. Meanwhile, Italian younger patients appear to be subjected to protective attitudes and behaviours from relatives and physicians. For example, this study found that, more often than older patients, younger patients have been accompanied by one or more relatives during medical encounters, and they received the communication of diagnosis more frequently from a relative rather than a physician.
Likewise, our data suggest that older people prefer an individual communication style to a full disclosure model, particularly as far as the communication of prognosis or the omission of information to protect the patient are concerned. There are some likely explanations for the differences between young and older patients. A possible reason for these attitudes may be the growing level of fear and apprehension with increasing age. Meanwhile, the young patients’ clear request for truth could be a reaction to some protective and paternalistic behaviours. This hypothesis seems to be consistent with our data according to which the younger patients, more than the older ones, consider the presence of relatives during medical encounters as a possible communicative barrier. Another explanation for these findings might be related to an intergenerational change taking place between old and young patients. The latter would prefer a full disclosure, by supporting the idea that gathering as much information as possible is a requirement for their own self-determination and autonomy. The older patients’ request for personalised communication may be explained as a demand for greater centrality of the patient as well. Nevertheless, a different motivation could be detected in the desire of older patients not to know all the truth. In other terms, the individual communication model would give to the physician a discretion regarding how much truth to disclose to patients. Although Donovan [1] assumes that the individual model is the best approach to truth-telling practice, it seems possible that in certain cultural contexts such a pattern could reproduce a paternalistic relationship within the doctor-patient encounter.
Actually, many studies demonstrated that Italian physicians and patients have been steeped in an enduring tradition of paternalism for a long time. This paternalistic approach, marked by physicians’ control, family-centred interaction and patients’ disposition to accept the medical control, was reflected in many truth-telling attitudes and practices. Regarding traditional practices of concealment of the truth by physicians, a qualitative research on Italian medical students about the contents conveyed by the hidden curriculum has highlighted that students were exposed to a culture of emotional detachment and partial unveiling of the information to patients, in order to protect them from the harm of knowing too much [78]. Besides, prior studies have noted that Italian physicians believed that not all the truth should be disclosed to the patient and that the latter would not want to know the truth; consequently, a section of the physicians did not break bad news in practice [20, 79, 80]. Indeed, a retrospective survey on caregivers of Italian patients who died of cancer has shown that a small portion of patients (37%) had received information regarding diagnosis and only 13% of people were informed about negative prognosis [56].
Regarding the role of the relatives, further studies have observed that a protective approach of the family is a factor that could explain different attitudes and behaviours towards truth-telling, as is the case in nations traditionally centred on family and community values, such as Eastern [16, 81, 82] and South European countries [83, 84], among which stands Italy [41].
Concerning patients’ disposition to accept medical control, some researches have revealed that individuals living in Southern European Catholic countries show less willingness to be informed on poor prognosis and end-of-life decision making [57, 85]. Comparing these results to the findings of the current study, it can be seen that Italian patients surveyed indicated the rise of a changed attitude towards the patient-physician relationship. The qualitative analysis showed that Italian patients would like to know the whole truth, to be heard, to obtain more information, and to take part in the decision-making process. In contrast to researches that have demonstrated that patients affected by life-threatening diseases prefer to entrust control of the encounter to the physician [86, 87], this study reveals that oncological patients, especially the youngest and highly educated, demand an active role and symmetrical communication.
In this investigation, there are several limitations. The study relies on a convenience sample, which does not allow these results to be generalised. Moreover, the survey is focused on a single type of cancer, and the stage of the disease is not known. The informants are members of patients’ Facebook groups; hence, they could be more active and engaged patients than others. Therefore, the relations identified could vary in significance over different patient populations. Further data collected by a probabilistic sample would be required to determine more accurately how age, educational level or different properties could affect patients’ preferences about the delivery of the truth.
Despite the severe limitations of convenience samples, these findings can enhance the understanding of Italian patients’ preferences.
The results of the present study and specifically those coming from the analysis of the final open-ended item of the questionnaire (see Section 3.2) will be used for the construction and validation of a more sophisticated questionnaire. The new version of the questionnaire will include questions that concern: cancer type, the stage of cancer when diagnosed, the specialize doctor charged with communicating diagnosis and prognosis, etc. (lacking from the present version). It could be administered in presence not only to a sample of Italian onco-haematological patients but also to patients suffering from other types of cancer in order to test if there were significant dissimilarities related to solid or non-solid-type tumours. Furthermore, it could be interesting to adopt a cross-cultural perspective to assess if the above-mentioned contextual differences endure over time or if, on the contrary, as Mauri et al. [9 p. 1527] argued some years ago that something is changing also in “those countries with a well-known attitude of non-disclosure, such as Italy”.
Given the importance of the topic for the patients’ wellbeing, future studies could also focus on pursuing not only descriptive results but also practical changes. In order to attain such a goal, it could be interesting to analyse surveys results and present them to a group of patients and health practitioners and ask them their experiences and recommendations on improving doctor-patient communication around giving the diagnosis and discussing prognosis.
Conclusion
The main aims of our paper were to investigate attitudes of Italian onco-haematological patients to the disclosure of the truth of diagnosis and prognosis, and to take into consideration their implications to enhance the communication of bad news within the patient-physician relationship.
As for patients’ preferences, the descriptive analysis showed some differences concerning the communication of diagnosis and prognosis. Indeed, although almost all of the patients agreed on the need to be informed, i.e. to know the truth of diagnosis and prognosis, the percentage of those who argued that the physicians have to disclose the truth in a personalised way, and not in full, increased in the case of prognosis (suggesting some difficulties in managing possible time-left information, consistent with the results of Harding et al. [57]).
On its part, the GLMM analysis revealed significant differences mainly related to the variables age and level of education. While the younger patients rejected the concealment of the truth, even when it is justified by the beneficence principle, the older ones and those with higher levels of education argued to consider doctors’ omissions—with the non-maleficence principle as a reason—as a behaviour different from lying. Furthermore, patients with higher levels of education agreed in believing that physicians have to communicate also the truth about diagnosis in a personalised way.
The qualitative analysis of the last item of the questionnaire gave us some suggestions concerning the aspects the patients consider important to improve the communication of bad news. These aspects can be reduced to three main dimensions on which doctors should pay more attention: time and setting management, care of the empathic aspects of the relationship, and greater availability towards patients’ requests to be informed, heard, etc. since that can enable them to play a more active role in the decision-making process concerning their health. Therefore, if, on the one hand, the Italian patients seem to have reached a new awareness about the importance of being informed (compared to the past and to the results, for example, of Mauri et al. [9]), on the other, they also believe that the empathic aspects are equally important (consistent with the suggestions of SPIKES and similar protocols).
The results of this preliminary study allowed us to know both the preferences of a sample of Italian onco-haematological patients concerning bad news communication and truth-telling and their opinions (based on their own experience) about how medical practice should change in order to improve doctor-patient relationships. From a pragmatic perspective, this study represents the first step in developing a more suitable tool for knowing Italian oncological patients’ experiences and preferences when they face bad news.
Availability of data and materials
The datasets analysed during the current study are available from the corresponding author on reasonable request.
Notes
“Three countries with the lowest percentage of respondents who would wish to know about time left were Italy, Spain and Portugal. It has been suggested that in traditional Mediterranean Catholic countries, patients are more likely to reject autonomy and that the medical establishment may have a greater paternalism” ([57] p. 2303).
Actually, the two patients, who were interviewed, viewed and completed the questionnaire, giving us their favorable opinion regarding clarity and comprehensibility of the items.
According to Landis and Koch [67], Kappa statistics < 0.00 indicate a poor strength of agreement; 0.00–0.20 slight agreement; 0.21–0.40 fair; 0.41–0.60 moderate; 0.61–0.80 substantial; 0.81–1.00 almost perfect.
Abbreviations
- SPIKES :
-
Stand for the six strategies which, according to Baile et al. (2000), should be useful in reducing patients’ distress during oncological encounters. S (setting), P(patient’s perception), I (patient’s invitation), K (giving knowledge to the patient), E (emphatic responses), S (strategies and summary).
- GLMM :
-
Stands for Generalized Linear Mixed Model
- ANOVA :
-
Stands for Analysis Of Variance
References
Donovan K. Breaking Bad News. In: Communication Bad News. Behavioral Science Learning Modules. Division of Mental Health: World Health Organization; 1993. p. 1–14.
Girgis A, Sanson-Fisher RW. Breaking bad news: consensus guidelines for medical practitioners. J Clin Oncol. 1995;13(9):2449–56. https://doi.org/10.1200/JCO.1995.13.9.2449.
Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES—A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302–11. https://doi.org/10.1634/theoncologist.5-4-302.
Fields SA, Johnson MW. Physician-patient communication: breaking bad news. W V Med J. 2012;108(2):32–6.
Borjalilu S, Karbakhsh M, Mirsharifi R, Davoodzadeh K, Aghili M, Kaviani A. Measuring Attitude and Practice of Physician toward Breaking Bad News to the Breast Cancer Patients: Development and Validation of a Questionnaire. Arch Breast Cancer. 2016;3(2):41–9. https://doi.org/10.19187/abc.20163241-49.
Parker PA, Baile WF, de Moor C, Lenzi R, Kudelka AP, Cohen L. Breaking bad news about Cancer: Patients' preferences for communication. J Clin Oncol. 2001;19(7):2019–56.
Hoff L, Tidefelt U, Thaning L, Hermerén G. In the shadow of bad news - views of patients with acute leukaemia, myeloma or lung cancer about information, from diagnosis to cure or death. BMC Palliat Care. 2007;6(1):1–8. https://doi.org/10.1186/1472-684X-6-1.
Fujimori M, Uchitomi Y. Preferences of Cancer patients regarding communication of bad news: a systematic literature review. Jpn J Clin Oncol. 2009;39(4):201–16. https://doi.org/10.1093/jjco/hyn159.
Mauri E, Vegni E, Lozza E, Parker PA, Moja EA. An exploratory study of the Italian patients' preferences regarding how they would like to be told about their cancer. Support Care Cancer. 2009;17:1523–30. https://doi.org/10.1007/s00520-009-0621-7.
Hillen MA, Koning CCE, Wilmink J, Klinkenbijl JW, Eddes EH, Kallimanis-King BL, et al. Assessing cancer patients' trust in their oncologist: development and validation of the Trust in Oncologist Scale (TiOS). Support Care Cancer. 2012;20(8):1787–95. https://doi.org/10.1007/s00520-011-1276-8.
Hillen MA, Butow PN, Tattersall MH, Hruby G, Boyle FM, Vardy J, et al. Validation of the English version of the Trust in Oncologist Scale (TiOS). Patient Educ Couns. 2013;91(1):25–8. https://doi.org/10.1016/j.pec.2012.11.004.
Hillen MA, Postma RM, Verdam MG, Smets EM. Development and validation of an abbreviated version of the Trust in Oncologist Scale—the Trust in oncologist scale–short form (TiOS-SF). Support Care Cancer. 2017;25(3):855–61. https://doi.org/10.1007/s00520-016-3473-y.
Seifart C, Hofmann M, Bär T, Knorrenschild Riera L, Seifart U, Rief W. (2014). Breaking bad news-what patients want and what they get: evaluating the SPIKES protocol in Germany. Ann Oncol. 2014;25(3):707–11. https://doi.org/10.1093/annonc/mdt582.
Porensky EK, Carpenter BD. Breaking bad news: effects of forecasting. Patient Educ Couns. 2016;99(1):68–76. https://doi.org/10.1016/j.pec.2015.07.022.
Rao A, Sunil B, Ekstrand M, Heylen E, Raju G, Shet A. Breaking bad news: patient preferences and the role of family members when delivering a Cancer diagnosis. Asian Pac J Cancer Prev. 2016;17(4):1779–84. https://doi.org/10.7314/APJCP.2016.17.4.1779.
Zekri J, Karim SM. Breaking Cancer bad news to patients with Cancer: a comprehensive perspective of patients, their relatives, and the public-example from a middle eastern country. J Glob Oncol. 2016;2(5):268–74. https://doi.org/10.1200/JGO.2015.001925.
Mirza RD, Ren M, Agarwal A, Guyatt GH. Assessing patient perspectives on receiving bad news: a survey of 1337 patients with life-changing diagnoses. AJOB Empir Bioeth. 2019;10(1):36–43. https://doi.org/10.1080/23294515.2018.1543218.
Burro R, Savardi U, Annunziata MA, De Paoli P, Bianchi I. The effects of presenting oncologic information in terms of opposites in a medical context. Patient Prefer Adherence. 2018a;12:443–59. https://doi.org/10.2147/PPA.S147091.
Burro R, Savardi U, Annunziata AM, De Paoli P, Bianchi I. The perceived severity of a disease and the impact of the vocabulary used to convey information: using Rasch scaling in a simulated oncological scenario. Patient Prefer Adherence. 2018b;12:2553–73. https://doi.org/10.2147/PPA.S175957.
Grassi L, Giraldi T, Messina EG, Magnani K, Valle E, Cartei G. Physicians' attitudes to and problems with truth-telling to cancer patients. Support Care Cancer. 2000;8(1):40–5. https://doi.org/10.1007/s005209900.
Vandekieft GK. Breaking bad news. Am Fam Physician. 2001;64(12):1975–8.
Narajanan V, Bista B, Koshy C. ‘BREAKS’ protocol for breaking bad news. Indian J Palliat Care. 2010;16(2):61–5. https://doi.org/10.4103/0973-1075.68401.
Buckman RA. Breaking bad news: the SPIKES strategy. Commun Oncol. 2005;2(2):138–42. https://doi.org/10.1016/S1548-5315(11)70867-1.
Pang Y, Tang L, Zhang Y, Song L, Goelz T, Fritzsche K, et al. Breaking bad news in China: implementation and comparison of two communication skills training courses in oncology. Psycho-Oncology. 2015;24(5):608–11. https://doi.org/10.1002/pon.3698.
Dunning R, Laidlaw A. The application of the practitioners in applied practice model during breaking bad news communication training for medical students: a case study. Scott Med J. 2015;60(4):170–5. https://doi.org/10.1177/0036933015608132.
Berney A, Carrard V, Stiefel F, Bourquin C. Individual training at the undergraduate level to promote competence in breaking bad news in oncology. Psycho-Oncology. 2017;26(12):2232–7. https://doi.org/10.1002/pon.4452.
Dégi CL. Non-disclosure of cancer diagnosis: an examination of personal, medical and psychosocial factors. Support Care Cancer. 2009;17(8):1101–7. https://doi.org/10.1007/s00520-008-0568-0.
Fraser B, Korenblum C, Mah K, Watt S, Malfitano C, Rydall A, et al. The experience of medical communication in adults with acute leukemia: impact of age and attachment security. Psycho-Oncology. 2019;28(1):122–30. https://doi.org/10.1002/pon.4919.
Hall MA, Zheng B, Dugan E, Camacho F, Kidd KE, Mishra A, et al. Measuring patients’ trust in their primary care providers. Med Care Res Rev. 2002;59(3):293–318. https://doi.org/10.1177/1077558702059003004.
Hagerty RG, Butow PN, Ellis PM, Dimitry S, Tattersall MH. Communicating prognosis in cancer care: a systematic review of the literature. Ann Oncol. 2005;16(7):1005–53. https://doi.org/10.1093/annonc/mdi211.
Barclay JS, Blackhall L, Tulsky JA. Communication strategies and cultural issues in the delivery of bad news. J Palliat Med. 2007;10(4):958–77. https://doi.org/10.1089/jpm.2007.9929.
Nie X, Ye D, Wang Q, Manyande A, Yang L, Qiu H, et al. Poor-prognosis disclosure preference in cancer patient– caregiver dyads and its association with their quality of life and perceived stress: a cross-sectional survey in mainland China. Psycho-Oncology. 2016;25(9):1099–105. https://doi.org/10.1002/pon.4055.
Rodriguez KL, Gambino FJ, Butow PN, Hagerty RG, Arnold RM. ‘It’s going to shorten your life’: framing of oncologist– patient communication about prognosis. Psycho-Oncology. 2008;17(3):219–25. https://doi.org/10.1002/pon.1223.
Clayton JM, Hancock K, Parker S, Butow PN, Walder S, Carrick S, et al. Sustaining hope when communicating with terminally ill patients and their families: a systematic review. Psycho-Oncology. 2008;17(7):641–59. https://doi.org/10.1002/pon.1288.
Fujimori M, Akechi T, Akizuki NO, Oba A, Sakano Y, Uchitom Y. Good communication with patients receiving bad news about cancer in Japan. Psycho-Oncology. 2005;14(12):1043–51. https://doi.org/10.1002/pon.917.
Fujimori M, Akechi T, Morita T, Inagaki M, Akizuki N, Sakano Y, et al. Preferences of cancer patients regarding the disclosure of bad news. Psycho-Oncology. 2007a;16(6):573–81. https://doi.org/10.1002/pon.1093.
Fujimori M, Parker PA, Akechi T, Sakano Y, Baile WF, Uchitomi Y. Japanese cancer patients’ communication style preferences when receiving bad news. Psycho-Oncology. 2007b;16(7):617–25. https://doi.org/10.1002/pon.1102.
Li J, Yuan XL, Gao XH, Yang XM, Jing P, Yu SY. Whether, when, and who to disclose bad news to patients with cancer: a survey in 150 pairs of hospitalized patients with cancer and family members in China. Psycho-Oncology. 2012;21(7):778–84. https://doi.org/10.1002/pon.1979.
Wuensch A, Tang L, Goelz T, Zhang Y, Stubenrauch S, Song L, et al. Breaking bad news in China – the dilemma of patients’ autonomy and traditional norms. A first communication skills training for Chinese oncologists and caretakers. Psycho-Oncol. 2013;22:1192–5. https://doi.org/10.1002/pon.3112.
Brédart A, Robertson C, Razavi D, Batel-Copel L, Larsson G, Lichosik D, et al. Patients' satisfaction ratings and their desire for care improvement across oncology settings from France, Italy. Poland and Sweden. Psycho-Oncol. 2003;12(1):68–77. https://doi.org/10.1002/pon.620.
Costantini A, Grassi L, Picardi A, Brunetti S, Caruso R, Nanni MG, et al. Awareness of cancer, satisfaction with care, emotional distress, and adjustment to illness: an Italian multicenter study. Psycho-Oncology. 2015;24(9):1088–96. https://doi.org/10.1002/pon.3768.
Grassi L, Costantini A, Kissane D, Brunetti S, Caruso R, Piazza G, et al. The factor structure and use of the demoralization scale (DS-IT) in Italian cancer patients. Psycho-Oncology. 2017;26(11):1965–71. https://doi.org/10.1002/pon.4413.
Nanni MG, Caruso R, Travado L, Ventura C, Palma A, Berardi AM, et al. Relationship of demoralization with anxiety, depression, and quality of life: A Southern European study of Italian and Portuguese cancer patients. Psycho-Oncol. 2018;27(11):2616–22. https://doi.org/10.1002/pon.4824.
Grassi L, Buda P, Cavana L, Annunziata MA, Torta R, Varetto A. Styles of coping with cancer: the Italian version of the mini-mental adjustment to Cancer (mini-MAC) scale. Psycho-Oncology. 2005;14(2):115–24. https://doi.org/10.1002/pon.826.
Mystakidou K, Parpa E, Eleni T, Katsouda E, Vlahos L. Cancer information disclosure in different cultural contexts. Support Care Cancer. 2004;12(3):147–54. https://doi.org/10.1007/s00520-003-0552-7.
Arraras J, Greimel E, Chie W-C, Sezer O, Bergenmar M, Costantini A, et al. (2011). Cross-cultural differences in information disclosure evaluated through the EORTC questionnaires. Psycho-Oncol. 2011;22(2):268–75. https://doi.org/10.1002/pon.2088.
Miyata H, Takahashi M, Saito T, Tachimori H, Kai I. Disclosure preferences regarding cancer diagnosis and prognosis: to tell or not to tell? J Med Ethics. 2005;31(8):447–51. https://doi.org/10.1136/jme.2003.007302.
Li S, Chou LJ. Communication with the cancer patient in China. Ann N Y Acad Sci. 1997;809(1 Communication):243–8. https://doi.org/10.1111/j.1749-6632.1997.tb48087.x.
Liu Y, Yang J, Huo D, Fan H, Gao Y. Disclosure of cancer diagnosis in China: the incidence, patients' situation, and different preferences between patients and their family members and related influence factors. Cancer Manag Res. 2018;10:2173–81. https://doi.org/10.2147/CMAR.S166437.
Tan TK, Teo FC, Wong K, Lim HL. Cancer: to tell or not to tell? Singap Med J. 1993;34(3):202–3.
Lee A, Wu HY. Diagnosis disclosure in cancer patients – when the family says “no!”. Singap Med J. 2002;43(10):533–8.
Khalil RB. Attitudes, beliefs and perceptions regarding truth disclosure of cancer-related information in the Middle East: a review. Palliative Supportive Care. 2013;11(1):69–78. https://doi.org/10.1017/S1478951512000107.
Dalla-Vorgia P, Katsouyanni K, Garanis TN, Touloumi G, Drogari P, Koutselinis A. Attitudes of a Mediterranean population to the truth-telling issue. J Med Ethics. 1992;18(2):67–74. https://doi.org/10.1136/jme.18.2.67.
Arraras JI, Illarramendi JJ, Valerdi JJ, Wright S. Truth-telling to the patient in advanced cancer: family information filtering and prospects for change. Psycho-Oncol. 1995;4(3):191–6. https://doi.org/10.1002/pon.2960040304.
Surbone A, Ritossa C, Spagnolo AG. Evolution of truth-telling attitudes and practices in Italy. Crit Rev Oncol Hematol. 2004;52(3):165–72. https://doi.org/10.1016/j.critrevonc.2004.09.002.
Costantini A, Morasso G, Montella M, Borgia P, Cecioni R, Beccaro M, et al. Diagnosis and prognosis disclosure among cancer patients. Results from an Italian mortality follow-back survey. Ann Oncol. 2006;17(5):853–9. https://doi.org/10.1093/annonc/mdl028.
Harding R, Simms V, Calanzani N, Higginson IJ, Hall S, Gysels M, et al. If you had less than a year to live, would you want to know? A seven-country European population survey of public preferences for disclosure of poor prognosis. Psycho-Oncol. 2013;22:2298–305. https://doi.org/10.1002/pon.3283.
Mitchison D, Butow P, Sze M, Aldridge L, Hui R, Vardy J, et al. Prognostic communication preferences of migrant patients and their relatives. Psycho-Oncology. 2012;21(5):496–504. https://doi.org/10.1002/pon.1923.
Schmitz C. LimeSurvey: An open source survey tool. Hamburg, Germany. URL http://www.limesurvey.org: LimeSurvey Project; 2012.
Pedon A, Gnisci A. Metodologia della ricerca psicologica. Bologna: Il Mulino; 2004.
Goss-Sampson, M. A. Statistical Analysis in JASP 0.9.2: A Guide for Students. https://static.jasp-stats.org/Statistical%20Analysis%20in%20JASP%20v0.9.2%20-%20A%20Students%20Guide.pdf. 2018.
Halter CP. Quantitative analysis with JASP open-source software; 2020.
Krippendorff K. Content analysis: An introduction to its methodology (Vol. 5). Newbury Park, CA: Sage; 1980.
Weber R. Basic content analysis. 2nd ed. Newbury Park, CA: Sage; 1990. https://doi.org/10.4135/9781412983488.
Ryan G, Bernard R. Data management and analysis methods. In: Denzin N, Lincoln Y, editors. Handbook of qualitative research. 2nd ed. Thousand Oaks, CA: Sage; 2000. p. 769–802.
Bernard HR, Ryan GW. Analyzing qualitative data: systematic approaches. Thousand Oaks, CA: Sage; 2010.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74. https://doi.org/10.2307/2529310.
Croissant Y. Estimation of Random Utility Models in R: The mlogit Package. J Stat Software. 2020;95(11):1–41. https://doi.org/10.18637/jss.v095.i11.
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67:1–48.
Nimmon L, Stenfors-Hayes T. The “handling” of power in the physician-patient encounter: perceptions from experienced physicians. BMC Med Educ. 2016;16(1):114. https://doi.org/10.1186/s12909-016-0634-0.
Hadlow J, Pitts M. The understanding of common health terms by doctors, nurses, and patients. Soc Sci Med. 1991;32(2):193–6. https://doi.org/10.1016/0277-9536(91)90059-L.
Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Educ Counsel. 2009;74(3):295–301. https://doi.org/10.1016/j.pec.2008.11.015.
Pieterse AH, Jager NA, Smets EM, Henselmans I. Lay understanding of common medical terminology in oncology. Psycho-Oncology. 2013;22(5):1186–91. https://doi.org/10.1002/pon.3096.
Cassileth BR, Zupkis RV, Sutton-Smith K, March V. Information and participation preferences among cancer patients. Ann Intern Med. 1980;92(2):832–6. https://doi.org/10.7326/0003-4819-92-6-832.
Jenkins V, Fallowfield L, Saul J. Information needs of patients with cancer: results from a large study in UK cancer centres. Br J Cancer. 2001;84(1):48–51. https://doi.org/10.1054/bjoc.2000.1573.
Cox AV, Jenkins V, Catt S, Langridge C, Fallowfield L. Information needs and experiences: an audit of UK cancer patients. Eur J Oncol Nurs. 2006;10(4):263–72. https://doi.org/10.1016/j.ejon.2005.10.007.
Huang B, Chen H, Deng Y, Yi T, Wang Y, Jiang Y. Diagnosis, disease stage, and distress of Chinese cancer patients. Ann Transl Med. 2016;4(4):73. https://doi.org/10.3978/j.issn.2305-5839.2016.02.08.
Lamiani G, Leone D, Meyer EC, Moja EA. How Italian students learn to become physicians: a qualitative study of the hidden curriculum. Medical Teacher. 2011;33(12):989–96. https://doi.org/10.3109/0142159X.2011.577467.
Gordon DR, Paci E. Disclosure practices and cultural narratives: understanding concealment and silence around cancer in Tuscany, Italy. Soc Sci Med. 1997;44(10):1433–52. https://doi.org/10.1016/S0277-9536(96)00198-0.
Vincent JL. Information in the ICU: are we being honest with our patients? The results of a European questionnaire. Intensive Care Med. 1998;24(12):1251–6. https://doi.org/10.1007/s001340050758.
Ozdogan M, Samur M, Artac M, Yildiz M, Savas B, Bozcuk HS. Factors related to truth-telling practice of physicians treating patients with cancer in Turkey. J Palliat Med. 2006;9(5):1114–9. https://doi.org/10.1089/jpm.2006.9.1114.
Wang DC, Guo CB, Peng X, Su YJ, Chen F. Is therapeutic non-disclosure still possible? A study on the awareness of cancer diagnosis in China. Support Care Cancer. 2011;19(8):1191–5. https://doi.org/10.1007/s00520-010-0937-3.
Mystakidou K, Liossi C, Vlachos L, Papadimitriou J. Disclosure of diagnostic information to cancer patients in Greece. Palliat Med. 1996;10(3):195–200. https://doi.org/10.1177/026921639601000303.
Núñez Olarte JM, Guillén DG. Cultural issues and ethical dilemmas in palliative and end-of-life care in Spain. Cancer Control. 2001;8(1):46–54. https://doi.org/10.1177/107327480100800107.
Toscani F, Farsides C. Deception, Catholicism, and hope: understanding problems in the communication of unfavorable prognoses in traditionally-catholic countries. Am J Bioeth. 2006;6(1):W6–W18. https://doi.org/10.1080/15265160500394994.
Arora NK, McHorney CA. Patient preferences for medical decision making: who really wants to participate? Med Care. 2000;38(3):335–41. https://doi.org/10.1097/00005650-200003000-00010.
Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A National Study of public preferences. J Gen Intern Med. 2005;20(6):531–5. https://doi.org/10.1111/j.1525-1497.2005.04101.x.
Acknowledgements
We thank all the patients who agreed to participate and completed the questionnaire, and the moderators of the Facebook groups of leukaemia patients, where the questionnaire was launched.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
The present article has not received prior publication and is not under consideration for publication elsewhere. If accepted, it will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright holder. All Authors listed on the title page have contributed significantly to the work, have read the manuscript, attest to the validity and legitimacy of the data and its interpretation, approve the final manuscript, and agree to its submission to the Journal BMC Public Health. Specifically, LP (Ludovica Piccioni), RB (Ramona Bongelli) and AB (Alessia Bertolazzi) designed the first version of the questionnaire. LP administered it to the Facebook groups of leukaemia patients and collected data; RB (Roberto Burro) performed GLMM analysis; AB (Alessia Bertolazzi) performed the qualitative analysis; RB (Ramona Bongelli) performed descriptive analysis. All the authors discussed data interpretation and contributed equally to writing the draft and final version of the paper.
Authors’ information
RB (Ramona Bongelli), PhD, is Assistant professor in General Psychology at the Department of Political Sciences, Communication and International Relationship of the University of Macerata. Her main research interests concern the pragma-linguistic and epistemic aspects of communication. She was the principal investigator (together with Zuczkowski) of a PRIN project entitled “Certainty and uncertainty in biomedical scientific communication”.
AB (Alessia Bertolazzi), PhD, is Assistant professor of Sociology at the Department of Political Sciences, Communication and International Relationship of the University of Macerata. Her main research interests include sociology of health and illness, health policies, healthcare professions. She has more than 10 years of experience in medical sociology and qualitative research, and she has been involved as experienced researcher in several national researches.
LP (Ludovica Piccioni) is MA student in Organization and Marketing for Corporate Communication at the Department of Political Science, Sociology and Communication (Sapienza University, Roma). When she was BA student in Science of Communication at the Department of Political Science, Communication and International Relations (University of Macerata), she participated in developing and administering the questionnaire presented in this paper.
RB (Roberto Burro), PhD, is Associate professor in General Psychology at the Department of Human Sciences (University of Verona). One of his main research interests concerns the structure of tests and questionnaires for the quantification of psychological variables in order to improve the diagnostic analysis of the patient. Recently, he published two articles concerning the impact of language used to communicate oncologic information.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was conducted according to the APA Ethics Code and following the European and Italian Privacy Law, i.e., EU Reg. 679/2016 (GDPRD) and Legislative Decree n. 196/2003 (Code regarding the protection of personal data).
The Ethic Committee of the Department of Human Sciences, University of Verona (Verona, Italy) approved the present study. Prot. n. 123455.
All the participants were informed by written consent about the research purposes and voluntarily agreed to complete the questionnaire anonymously. The questionnaire compilation and its electronic sending represented participants’ explicit consent to participation in the study and processing of data. The Ethic Committee approved this procedure.
Consent for publication
All the authors have approved the manuscript for submission.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bongelli, R., Bertolazzi, A., Piccioni, L. et al. Italian onco-haematological patients’ preferences in bad news communication: a preliminary investigation. BMC Cancer 21, 555 (2021). https://doi.org/10.1186/s12885-021-08181-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-021-08181-0