Abstract
Background
In recent years, the identification of genetic and phenotypic biomarkers of cancer for prevention, early diagnosis and patient stratification has been a main objective of research in the field. Different multivariable models that use biomarkers have been proposed for the evaluation of individual risk of developing breast cancer.
Methods
This is a case control study based on a population-based cohort. We describe and evaluate a multivariable model that incorporates 92 Single-nucleotide polymorphisms (SNPs) (Supplementary Table S1) and five different phenotypic variables and which was employed in a Spanish population of 642 healthy women and 455 breast cancer patients.
Results
Our model allowed us to stratify two groups: high and low risk of developing breast cancer. The 9th decile included 1% of controls vs 9% of cases, with an odds ratio (OR) of 12.9 and a p-value of 3.43E-07. The first decile presented an inverse proportion: 1% of cases and 9% of controls, with an OR of 0.097 and a p-value of 1.86E-08.
Conclusions
These results indicate the capacity of our multivariable model to stratify women according to their risk of developing breast cancer. The major limitation of our analysis is the small cohort size. However, despite the limitations, the results of our analysis provide proof of concept in a poorly studied population, and opens up the possibility of using this method in the routine screening of the Spanish population.
Similar content being viewed by others
Background
The prevention and early diagnosis of breast cancer is one of the main objectives of cancer research. There are different models to estimate cancer risk based on genetic or non-genetic factors; that is, a high or moderate predisposition [1, 2]. In recent years, the extensive use of genome-wide association studies (GWAS) has led to the identification of low-susceptibility alleles (SNPs). These SNPs are usually combined in a polygenic risk score (PRS), which, in combination with non-genetic factors, reflects the risk of developing breast cancer [3]. We recently described a low-susceptibility SNP polygenic risk score of 76 for breast cancer that allows the general population to be stratified. According to this score, women at a low and high risk of developing breast cancer presented 0.5 and 2.5-fold increased risks, respectively, relative to women in the middle quintile [4]. Previous studies have shown that breast density, familial antecedents and PRS models composed of 77 [5], 83 [6] or, more recently, 313 SNPs [7] determine women at risk. The combination of phenotype and PRS increases the likelihood of identifying women at risk who require personalized follow-up, particularly when an individual exceeds the risk threshold.
Although there are previous studies in Caucasian populations, this is the first to combine a PRS of 92 SNPs with other risk factors, such as mammographic density (MD), reproductive factors, and family history, in a Spanish population of 1097 women. The main objective was to analyze the usefulness of this approach in our population using a multivariable logistic method based on the combination of these variables.
Methods
Study design: description of cohorts
The present study was submitted to and approved by the Clinical Research Ethics Committee (CEIC) of the Hospital Clínico Universitario de Valencia (Spain) - September 29th, 2016 (2016/169) and July 13th, 2018 (2018/139) - and was conducted in compliance with the Helsinki Declaration.
This is case control study compiling full genotyping and phenotypic data for a cohort recruited between January 2017 and December 2018 from two sources: Hospital Clínico Universitario de Valencia and Valencian Community Screening Programme (General Directorate Public Health), both in the Autonomous Community of Valencia (on the Mediterranean Coast). A total of 867 healthy women and 640 breast cancer patients were recruited, with ages in the range of 30–70. Patients had developed breast cancer in a maximum period of 5 years prior to data collection, while controls were women who had not developed breast cancer during the same period. Those that presented incomplete phenotypic data or genotyping failure were excluded from the cohort, which left 1097 participants consisting of 642 healthy women and 455 breast cancer cases.
The patient cohort was composed of 45% Luminal A, 20% Luminal B, 20% Her-2 positive and 15% Triple Negative tumors (approximate percentages).
Data collection
Clinical information was collected for all subjects at recruitment: family history of breast cancer, date of birth, age, age at menarche, age at menopause, age at first pregnancy, and mammographic density (MD). Breast density was assessed from craniocaudal and mediolateral oblique mammographic projections by an experienced radiologist with more than 10 years of experience. The radiologist used the image viewer system (DICOM, from General Electric GIMD company), classifying MD according to Boyd’s semiquantitative scale [8].
SNP selection and genotyping
As in our previous PRS risk analysis [4], we initially selected 76 SNPs from the European Collaborative Oncological Gene Environment Study (COGS) [9]. These SNPs were significant or showed a trend towards significance in our previous validation with Spanish samples. The correlation of the genetic variants analyzed with prediction of breast cancer risk in women of the Spanish population has already been described [4]. In brief, we analyzed the performance of our PRS using the 76 selected SNPs for breast cancer risk prediction in a Spanish case and control cohort. The initial selection was extended to 123 SNPs by including additional SNPs obtained from the OncoArray Project [10]. Of these, 28 SNPs with an OR close to 1 (0.95 < OR < 1.05) and another 3 SNPs with platform genotyping failure were removed. In this way, a total of 92 SNPs [11,12,13,14,15,16] were eventually employed for the current analysis (Online Resource 1).
The genotyping method has been described previously [4]. In short, 10 ml of peripheral blood was collected in an EDTA tube. One μg of Deoxyribonucleic acid (DNA) was used for the genotypic analysis (minimum concentration of 25 ng/μL). Genotyping was performed with the Open Array® Real-Time PCR platform (Life Technologies) using the Acufill® system and Taqman® probes. The data obtained were analyzed using Genotyper software. Samples with a call rate < 0.95 were discarded. SNPs with a genotyping rate < 0.95 and SNPs generating errors in control duplicates were also ruled out.
Statistical analysis
Sample size was calculated with a 95% confidence level (two-tailed test), 80% statistical power, control-case ratio of 1.3 and initial prevalence of breast cancer of 12%; the total number of women necessary for results to be statistically significant was 1138, similar to our case control cohort (1097). In an initial exploratory univariable process, the case/control ratio of each risk factor was compared. During this step, the Wilcoxon-test was used with a two-sided p-value threshold of 0.05.
The PRS was based on a combined effect of 92 SNPs statistically associated with breast cancer. This strategy considers an independent effect of each SNP, ignoring departures from a multiplicative model [17]. The PRS was derived for each study subject using the formula:
where xk is the number of risk alleles (0, 1 or2) based on the ploidy of each SNP. The βk weights are the ORs of the risk alleles associated with breast cancer described in Online Resource 1. This strategy has been used in other studies [5, 6]. The resulting values are normalized using the median PRS value of the control samples of the cohort.
In the phenotypic analysis, the phenotypic categories were transformed into quantitative variables using the ORs described in the Pollan et al. study [8], except for family history, the ORs of which were based on the Pharoah et al. study [18]. In addition, the age of women (age at diagnosis of patients and age at interview of controls) was grouped into five-year periods, similar to in other publications [19], which allowed the groups to be transformed into quantitative variables. The final number of cases and controls in our cohort was 455 and 642, respectively.
For the univariable analysis, logistic regression was applied to each risk factor, which has been adjusted for age and centre. The coefficients of the model were standardized using the reghelper library of R [20]. Additionally, the PRS was adjusted for the first five principal components. The interaction effect between variables was also evaluated using the likelihood ratio test (LRT). All analyses were two-sided and employed a p-value threshold of 0.05.
To confirm the independence of the PRS and other phenotypic risk factors, pairwise Spearman correlations of unaffected controls were evaluated.
For the multivariable study, we performed a logistic regression analysis that incorporated the statistically significant variables obtained in the previous steps, including the interaction terms. Family history and age at menarche were also included in the analyses, even though they were not significant, since they are well-known risk factors. The significance of the final model was evaluated using the Wald Test [21]. To assess the accuracy of the final multivariable model, a global Hosmer-Lemeshow goodness-of-fit test was performed using deciles [22].
To evaluate improvement in risk prediction for the different models and risk factors, the area under the curve (AUC) was evaluated [23] as a measure of discrimination between cases and control women. This calculation was performed using the pROC [24] library of R. To avoid a possible overfitting of the model, the 95% Confidence Interval (CI) of the AUC was assessed using a cross validation strategy [25]. This step was based on the calculation of AUC in 1000 permutations using a random selection of 90% of women as a training set and the remaining 10% as a test set.
Finally, women were stratified into deciles based on their final individual risk factor, obtained from the multivariable model. The ORs of extreme deciles were evaluated using logistic regression with a reference range of 40–60%.
Based on the characteristics of our cohort, the final individual risk factor proposed in this study describes the relative risk of women in the Spanish population of suffering breast cancer in a maximum period of 5 years.
Results
Association of phenotypic risk factors with breast cancer
Age is one of the most important risk factors of breast cancer [26]. To ensure that our analysis was not affected by any bias or confounding effect associated with this risk factor, the distribution of cases and controls was compared using the Wilcoxon test, with no significant differences being detected (p-value of 0.27). The median age of our cohort was 51 years old, with a range of 30 and 70 years in the extreme deciles (Table 1).
The global phenotypic risk factors after comparison between cases and controls in our cohort are detailed in Table 1. Differences between cases and controls in age at menarche and familial antecedents were not statistically significant, with p-values of 0.061 and 0.34, respectively.
Mammographic density presented a clear, statistically significant relationship with breast cancer, with an OR of 1.46 (95% CI: 1.21–1.71) and a p-value of 1.64E-7. The main differences between controls and cases were concentrated in the extremes, with respective proportions of 15% versus 11% in the first category (MD 0–10%) and 10% versus 22% in the last category (MD > 75%).
In our cohort, a higher age at first delivery was associated with an increased risk of development of breast cancer, while age at menarche did not have a statistically significant effect, with p-values of 0.03 and 0.061, respectively. Age at first delivery was associated with an OR of 1.15 (95% CI: 1.02–1.31), and the most marked differences were seen with advanced maternal ages (over 34 years), with a proportion of 11% versus 8% among cases and controls, respectively. In terms of age at menarche, the OR was 0.89 (95% CI: 0.78–1.04). Another reproductive factor we have considered in this study was menopause status, which was associated with an OR of 1.96 (95% CI: 1.72–2.24) and a p-value <2E-16. The greatest difference between cases and controls was observed in the premenopausal category, with values of 46 and 13%, respectively. Regarding family history, cases showed a slightly stronger trend towards more breast cancer antecedents in first- and second-degree family members than controls; however, the logistic regression based on this quantitative variable was not statistically significant, with a p-value of 0.34.The interaction terms identified in our analysis as statistically significant and included in the multivariable model were age with mammary density and age with menopause status, with p-values of 0.004 and 2E-16, respectively. Indeed, the relation between both phenotypes and age has been the subject of study in the field of breast cancer for some time [27,28,29].
The discriminative power of each phenotypic risk factor was compared using ROC curve analysis generated by 10-fold cross-validation (Table 2). The results were concordant with the univariable logistic regression, where age at menarche and family history did not present significant trends and the most discriminant phenotypic variables were menopause status - with an AUC of 0.64 (95% CI: 0.58–0.70) - and mammographic density - with an AUC of 0.60 (95% CI: 0.56–0.66) (Table 2).
Association of PRS92 with breast cancer
The PRS based on 92 SNPs presented an OR per 1 standard deviation (SD) of 1.41, with a 95% CI of 1.24–1.61 and a p-value of 6.30 × 10− 8. For women in the lowest quintile (5%), the PRS distribution presented an OR of 0.38 (95% CI: 0.22–0.63; p-value = 0.0026) with respect to women in the middle quintile (40–60%). On the other hand, the highest quintile (95%) of PRS distribution exhibited an OR of 1.87 (95% CI: 1.16 3.08; p = 0.036) (Fig. 1). The x-axis corresponds with the different deciles and the y-axis reflects the OR using the 40–60% range as reference. The discriminative accuracy of PRS92 was calculated using the area under the curve (AUC). PRS92 (adjusted by age) and the first five principal components presented a discriminative power of 0.62 and a 95% CI of 0.56–0.66 (Table 2). This predictive performance range was one of the most discriminant variables, along with breast mammographic density (0.60) and menopause (0.64).
Multivariable model for breast cancer stratification
All statistically significant univariable risk factors and interaction terms were included in the final multivariable model. Age at menarche and family history were also incorporated into the model based on the scientific literature. The Spearman method did not reveal significant correlations for any other variable (data not shown).
We evaluated the discriminative accuracy of the multivariable model with and without interaction terms (Fig. 2). The median AUC obtained using the interaction model was 0.80 (95% CI: 0.77–0.83), which was higher than that for the model without interactions; 0.74 (95% CI: 0.71–0.77) (Table 2). This difference was statistically significant with a p-value of 5.375E-09. These values are slightly higher than those observed in other previously published methods [30, 31].
AUC-ROC of the multivariable model, with and without interaction terms (blue and pink, respectively). The AUC of the ROC curve of the final multivariable model with interaction was significantly higher than that of the model without interaction: 0.80 (95% CI: 0.77–0.83) versus 0.74 (95% CI: 0.71–0.77). The 95% confidence interval was evaluated using a bootstrap strategy
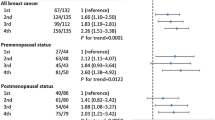
We investigated how individual risk for cases and controls differed when the final multivariable model was used. Figure 3 and Table 3 show the ORs and percentages of cases and controls classified by deciles using the final risk predicted by the multivariable model with interactions. In the first decile, the OR was 0.097 (CI: 95% 0.046–0.184) with a p-value of 1.86E-08. This range contained 9% of controls versus less than 1% of cases. This trend was similar in the next decile, with 8.75 and 1.28% of controls and cases, respectively (OR: 0.29; p = 8.12E-07). At the other extreme, in the last decile, OR was 12.9 (CI: 95% 5.098–23.332; p = 3.43E-07), and the proportion of cases and control was inversed, with 9% of cases and 1% of controls. These results indicate the capacity of the multivariable model to stratify women according to the risk they run of suffering breast cancer.
Discussion
In recent years, there have been various proposals for multivariable models that stratify women who might suffer breast cancer according to their individual risk. Different biomarkers have been analyzed as possible predictors, including phenotypic and non-phenotypic markers, and environmental and genetic factors.
One approach to measuring genetic variables is the polygenic risk score (PRS). This strategy is based on variable numbers of statistically significant low penetrance variants obtained from large GWAS analyses [5, 32].
Our study was based on a relatively small cohort of women adjusted for center of origin in our univariable and multi-variable models.
Employing a specific PRS based on 92 SNPs we obtained an OR of 1.41 (1.24–1.61) that was consistent with the results of other published studies of Caucasian populations using different numbers of SNPs (from 18 to 313) [5, 32,33,34].
The AUC-ROC was 0.62, with a 95% CI of 0.56–0.66, which is also in line with the literature and assigns a range of 0.58 to 0.65 to European populations and one of 0.53 to 0.64 to non-European populations [35].
Regarding univariable phenotypic risk factor analysis, the most statistically significant results in terms of discriminant variables were obtained for menopause status and mammographic density, which once again is consistent with previous studies [28, 29, 36, 37]. Other reproductive factors, such as later age when giving birth for the first time and later age at menarche, have been identified as risk factors for breast cancer [38]. In our study, a significant p-value of 0.03 and an OR of 1.15 were identified for the former risk factor, while the latter was not found to be statistically significant (p-value = 0.061).
The ORs of the risk factors obtained in our cohort present differences with respect to those previously reported. The most evident concern the lack of a statistical significance of family history and age of menarche. However, the direction (positive or negative) of these well-established effects and our results are concordant. On the other hand, the magnitude of OR of mammographic density was lower than that reported in the literature. These differences may be due to the low number of women in our cohort; however, the concordance of the effect, direction and magnitude of the different ORs of our population corroborates the validity of our study as a first proof of concept in a Spanish population.
Additionally, the joint association of our PRS92 with transformed continuous phenotypic variables, such as MD, reproductive factors and family history, was examined in our Spanish population. We did not find any significant correlation between genotypic and phenotypic variables; a multiplicative model would possibly describe this in greater depth and help to improve breast cancer risk estimation.
The precision of the multivariable model increased when we added two statistically significant interaction terms associated with women’s age: menopause and mammographic density. Such interactions have previously been observed, and we detected an increase of AUC-ROC from 0.74 (95% CI: 0.71–0.77) to 0.80 (95% CI: 0.77–0.83) (Table 2), a rise that was statistically significant and offered a final value slightly higher than those of other similar multivariable studies [39].
We were able to stratify the control group within our model (Fig. 3), in which both extremes showed important differences. The last decile included 1% of controls vs 9% of cases, with an OR of 12.9 and a p-value 3.43E-07. In contrast, the first decile presented an inverse proportion (1% of cases and 9% of controls); in this case, the OR was 0.097, with a p-value of 1.86E-08. These results indicate the capacity of the multivariable model to stratify women according to risk of developing breast cancer.
In summary, our results indicate that using the multivariable logistic model and a combination of genetic, phenotypic and interaction variables is an effective approach for stratifying women in the Spanish population according to individual risk of suffering breast cancer within a 5-year period, with a capacity similar to that observed in other studies in European and non-European populations. Due to the nature of our study, different biases could have affected the precision of the results; for example, there may have been selection and length biases. Additionally, the small size of our cohort could have led to overfitting of the model in terms of risk estimation or the over/under representation of a specific tumor type. However, in spite of these limitations, our analysis provides proof of concept in a population that has not been studied until now. Larger series are necessary in order to confirm our data and initiate the use of this type of screening method in the Spanish population.
Conclusions
Our results endorse the capacity of the multivariable model to stratify women according to their risk of developing breast cancer. Some bias could be present in the study and could have affected the precision of our results; however, the analysis provides proof of concept in a poorly studied population and opens up the possibility of its use in the routine screening of the Spanish population.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CNIO:
-
Spanish National Cancer Center
- SNP:
-
Single-nucleotide polymorphism
- OR:
-
Odd ratio
- GWAS:
-
Genome-wide association studies
- PRS:
-
Polygenic risk score
- MD:
-
Mammographic density
- COGS:
-
European Collaborative Oncological Gene Environment Study
- DNA:
-
Deoxyribonucleic acid
- LRT:
-
Likelihood ratio test
- AUC:
-
Area under the curve
- CI:
-
Confidence interval
- SD:
-
Standard deviation
References
Beral V, Bull D, Doll R, Peto R, Reeves G, Skegg D, et al. Familial breast cancer: collaborative reanalysis of individual data from 52 epidemiological studies including 58 209 women with breast cancer and 101 986 women without the disease. Lancet. 2001;358(9291):1389–99.
Antoniou AC, Easton DF. Models of genetic susceptibility to breast cancer. Oncogene. 2006;25(43):5898–905.
Rudolph A, Song M, Brook MN, Milne RL, Mavaddat N, Michailidou K, et al. Joint associations of a polygenic risk score and environmental risk factors for breast cancer in the Breast Cancer Association Consortium. Int J Epidemiol. 2018;47(2):526–36.
Miñambres R, Pita G, Sanchez I, Serra D, Rosar R, Rubio-Solsona E, Palacios S, Llaneza A, Marron P, Hoyas S, Lluch A, Cano A, Gonzalez A, Triviño JC, Benítez J. Prediction of cancer risk based on study of genetic variants in healthy women in the Spanish population. Rev Senol Patol Mamar. 2019;32(3):94–9. https://doi.org/10.1016/j.senol.2019.07.001.
Mavaddat N, Pharoah PDP, Michailidou K, Tyrer J, Brook MN, Bolla MK, et al. Prediction of breast cancer risk based on profiling with common genetic variants. J Natl Cancer Inst. 2015;107(5):djv036.
Vachon CM, Scott CG, Tamimi RM, Thompson DJ, Fasching PA, Stone J, et al. Joint association of mammographic density adjusted for age and body mass index and polygenic risk score with breast cancer risk. Breast Cancer Res. 2019;21(1):68.
Lee A, Mavaddat N, Wilcox AN, Cunningham AP, Carver T, Hartley S, et al. BOADICEA: a comprehensive breast cancer risk prediction model incorporating genetic and nongenetic risk factors. Genet Med. 2019;21(8):1708–18.
Pollán M, Ascunce N, Ederra M, Murillo A, Erdozáin N, Alés-Martínez JE, et al. Mammographic density and risk of breast cancer according to tumor characteristics and mode of detection: a Spanish population-based case-control study. Breast Cancer Res. 2013;15(1):R9.
Michailidou K, Hall P, Gonzalez-Neira A, Ghoussaini M, Dennis J, Milne RL, et al. Large-scale genotyping identifies 41 new loci associated with breast cancer risk. Nat Genet. 2013;45(4):353–61.
Michailidou K, Beesley J, Lindstrom S, Canisius S, Dennis J, Lush MJ, et al. Genome-wide association analysis of more than 120,000 individuals identifies 15 new susceptibility loci for breast cancer. Nat Genet. 2015;47(4):373–80.
Ghoussaini M, Pharoah PDP, Easton DF. Inherited genetic susceptibility to breast cancer: the beginning of the end or the end of the beginning? Am J Pathol. 2013;183(4):1038–51.
Michailidou K, Lindström S, Dennis J, Beesley J, Hui S, Kar S, et al. Association analysis identifies 65 new breast cancer risk loci. Nature. 2017;551(7678):92–4.
Osorio A, Milne RL, Kuchenbaecker K, Vaclová T, Pita G, Alonso R, et al. DNA Glycosylases involved in base excision repair may be associated with cancer risk in BRCA1 and BRCA2 mutation carriers. PLoS Genet. 2014;10(4):e1004256.
Gaudet MM, Kuchenbaecker KB, Vijai J, Klein RJ, Kirchhoff T, McGuffog L, et al. Identification of a BRCA2-specific modifier locus at 6p24 related to breast cancer risk. PLoS Genet. 2013;9(3):e1003173.
Couch FJ, Wang X, McGuffog L, Lee A, Olswold C, Kuchenbaecker KB, et al. Genome-wide association study in BRCA1 mutation carriers identifies novel loci associated with breast and ovarian cancer risk. PLoS Genet. 2013;9(3):e1003212.
Bojesen SE, Pooley KA, Johnatty SE, Beesley J, Michailidou K, Tyrer JP, et al. Multiple independent variants at the TERT locus are associated with telomere length and risks of breast and ovarian cancer. Nat Genet. 2013;45(4):371–84 384e1-2.
Pharoah PDP, Antoniou AC, Easton DF, Ponder BAJ. Polygenes, risk prediction, and targeted prevention of breast cancer. N Engl J Med. 2008;358(26):2796–803.
Pharoah PDP, Day NE, Duffy S, Easton DF, Ponder BAJ. Family history and the risk of breast cancer: a systematic review and meta-analysis. Int J Cancer. 1997;71(5):800–9.
Maas P, Barrdahl M, Joshi AD, Auer PL, Gaudet MM, Milne RL, et al. Breast cancer risk from modifiable and nonmodifiable risk factors among white women in the United States. JAMA Oncol. 2016;2(10):1295–302.
Hughes J. reghelper: helper functions for regression analysis. R package version 0.3.5; 2020.
Draper NR, Smith H. Applied regression analysis. 3rd ed. New York: Wiley; 1998.
Hosmer DW, Lemeshow S, Sturdivant RX. Applied logistic regression: third edition; 2013.
Rosner B, Glynn RJ. Power and sample size estimation for the wilcoxon rank sum test with application to comparisons of C statistics from alternative prediction models. Biometrics. 2009;65(1):188–97.
Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez JC, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics. 2011;12:77.
Tworoger SS, Zhang X, Eliassen AH, Qian J, Colditz GA, Willett WC, et al. Inclusion of endogenous hormone levels in risk prediction models of postmenopausal breast cancer. J Clin Oncol. 2014;32(28):3111–7.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67(1):7–30.
Bertrand KA, Tamimi RM, Scott CG, Jensen MR, Pankratz VS, Visscher D, et al. Mammographic density and risk of breast cancer by age and tumor characteristics. Breast Cancer Res. 2013;15(6):R104.
Tice JA, Miglioretti DL, Li CS, Vachon CM, Gard CC, Kerlikowske K. Breast density and benign breast disease: risk assessment to identify women at high risk of breast cancer. J Clin Oncol. 2015;33(28):3137–43.
Hsieh C-C, Trichopoulos D, Katsouyanni K, Yuasa S. Age at menarche, age at menopause, height and obesity as risk factors for breast cancer: associations and interactions in an international case-control study. Int J Cancer. 1990;46(5):796–800.
Shieh Y, Hu D, Ma L, Huntsman S, Gard CC, Leung JWT, et al. Joint relative risks for estrogen receptor-positive breast cancer from a clinical model, polygenic risk score, and sex hormones. Breast Cancer Res Treat. 2017;166(2):603–12.
Dite GS, Macinnis RJ, Bickerstaffe A, Dowty JG, Allman R, Apicella C, et al. Breast cancer risk prediction using clinical models and 77 independent risk-associated SNPs for women aged under 50 years: Australian breast cancer family registry. Cancer Epidemiol Biomark Prev. 2016;25(2):359–65.
Mavaddat N, Michailidou K, Dennis J, Lush M, Fachal L, Lee A, et al. Polygenic risk scores for prediction of breast cancer and breast cancer subtypes. Am J Hum Genet. 2019;104(1):21–34.
Van Veen EM, Brentnall AR, Byers H, Harkness EF, Astley SM, Sampson S, et al. Use of single-nucleotide polymorphisms and mammographic density plus classic risk factors for breast cancer risk prediction. JAMA Oncol. 2018;4(4):476–82.
Hüsing A, Canzian F, Beckmann L, Garcia-Closas M, Diver WR, Thun MJ, et al. Prediction of breast cancer risk by genetic risk factors, overall and by hormone receptor status. J Med Genet. 2012;49(9):601–8.
Yanes T, Young MA, Meiser B, James PA. Clinical applications of polygenic breast cancer risk: a critical review and perspectives of an emerging field. Breast Cancer Res. 2020;22(1):21.
Tice JA, Cummings SR, Smith-Bindman R, Ichikawa L, Barlow WE, Kerlikowske K. Using clinical factors and mammographic breast density to estimate breast cancer risk: development and validation of a new predictive model. Ann Intern Med. 2008;148(5):337–47.
Hamajima N, Hirose K, Tajima K, Rohan T, Friedenreich CM, Calle EE, et al. Menarche, menopause, and breast cancer risk: individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol. 2012;13(11):1141–51.
Dierssen-Sotos T, Palazuelos-Calderón C, Jiménez-Moleón JJ, Aragonés N, Altzibar JM, Castaño-Vinyals G, et al. Reproductive risk factors in breast cancer and genetic hormonal pathways: a gene-environment interaction in the MCC-Spain project. BMC Cancer. 2018;18(1):280.
Zhang X, Rice M, Tworoger SS, Rosner BA, Eliassen AH, Tamimi RM, et al. Addition of a polygenic risk score, mammographic density, and endogenous hormones to existing breast cancer risk prediction models: a nested case–control study. PLoS Med. 2018;15(9):e1002644.
Acknowledgements
We acknowledge the Spanish National Genotyping Center’s lab (CEGEN) for its technical support and Pablo Fernandez from the Epidemiology Center (Madrid) for his statistical support.
Funding
This study was financed by the own funds of Sistemas Genómicos S.L. Additionally, it was supported by two organizations that provided funds for the execution of the project: IVACE (Instituto Valenciano de competitividad empresarial) and AVI (Agencia Valenciana de Innovación). IVACE grant numbers: IMIDTA/2016/75 and IMIDTA/2018/7; AVI programme grant number; INNTAL21/197002.
Author information
Authors and Affiliations
Contributions
JCT, AC, ER, RM, RB, AGN, AGV, AMA, BB, PE, JI, DS conceived experiments. DS, ISG, GR, GP, SD, AJ, AL carried out experiments. JCT, AC, MC, GL, RR, JLD analysed data. JCT, AC, ER, RM, JB, LB, AL, AC conceived the study, participated in its design and coordination and wrote the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The present study was submitted to and approved by the Clinical Research Ethics Committee (CEIC) of the Hospital Clínico Universitario de Valencia (Spain), September 29th, 2016 (2016/169) and July 13th, 2018 (2018/139), and was conducted in compliance with the Helsinki Declaration.
Informed consent: Written informed consent was obtained from all the participants included in the study at the time of recruitment. Patient information was anonymized and de-identified.
This study was approved by the Ethical Committee of Hospital Clínico Universitario de Valencia (Comité Ético de Investigación Clínica) on 29th September 2016 and was assigned the internal project code 2016/169.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Triviño, J.C., Ceba, A., Rubio-Solsona, E. et al. Combination of phenotype and polygenic risk score in breast cancer risk evaluation in the Spanish population: a case –control study. BMC Cancer 20, 1079 (2020). https://doi.org/10.1186/s12885-020-07584-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-020-07584-9