Abstract
Background
Although surgical resection provides a cure for patients with intrahepatic cholangiocarcinoma (ICC), the risk of mortality and recurrence remains high. Several biomarkers are reported to be associated with the prognosis of ICC, including Beclin-1, ARID1A, carbonic anhydrase IX (CA9) and isocitrate dehydrogenase 1 (IDH1), but results are inconsistent. Therefore, a histopathological retrospective study was performed to simultaneously investigate the relationship of these four potential biomarkers with clinicopathological parameters and their prognostic values in patients with ICC.
Methods
A total of 113 patients with ICC were enrolled from Cancer Hospital of Chinese Academy of Medical Sciences between January 1999 and June 2015. The expression of Beclin-1, ARID1A, IDH1 and CA9 were determined by immunohistochemical staining. The prognostic values of the four biomarkers were analyzed by Cox regression and the Kaplan-Meier method.
Results
Beclin-1, ARID1A, CA9 and IDH1 were highly expressed in ICC tumor tissues. Higher mortality was positively associated with Beclin-1 expression (HR = 2.39, 95% CI = 1.09–5.24) and higher recurrence was positively associated with ARID1A expression (HR = 1.71, 95% CI = 1.06–2.78). Neither CA9 nor IDH1 expression was significantly associated with mortality or disease recurrence. Kaplan-Meier survival curves showed that ICC patients with higher Beclin-1 and ARID1A expression had a lower survival rate and a worse recurrence rate than patients with low Beclin-1 and ARID1A expression (p < 0.05).
Conclusions
High Beclin-1 and ARIDIA expression are strongly associated with poor prognosis in ICC patients, and thus Beclin-1 and ARID1A should be simultaneously considered as potential prognostic biomarkers for ICC patients.
Similar content being viewed by others
Background
Intrahepatic cholangiocellular carcinoma (ICC) is an aggressive cancer that arises from the epithelial bile ducts in the liver and has a very poor prognosis [1]. ICC accounts for 5 to 30% of all primary liver malignancies, and its incidence has been rising over the past few decades [2]. ICC often occurs in cirrhotic and non-cirrhotic livers because of chronic hepatitis, metabolic syndrome and the lack of clear etiological risk factors [3, 4]. Although the reported incidence of ICC is about one to two cases per 100,000 patients in the Western world [5,6,7], the cancer-related mortality of ICC is increasing, and the 5-year survival rate is less than 20% [8, 9]. Currently, surgical resection is the regular treatment for patients with ICC. However, postoperative resection, conventional chemotherapy and radiotherapy do not significantly improve long-term survival, and there remains a high recurrence rate and metastasis [10,11,12,13,14]. Thus, in past studies, many potential biomarkers for the diagnosis of ICC have been identified. In addition, several studies identified clinicopathological risk factors for ICC recurrence or mortality, such as age, tumor size, number of tumors, lymph node metastasis, vascular invasion, positive margins and pre-existing liver disease [15,16,17]. However, few studies have systematically and simultaneously investigated the prognostic values of these biomarkers through histopathology.
The disease staging and prognosis of ICC are mainly based on the pathological features of the tumor. Although surgical resection combined with cytotoxic chemotherapy is the standard treatment for ICC, prognosis remains poor, with a median survival of about 1 year [18]. Thus, new and effective molecular targets to identify ICC are urgently needed. Recent studies suggested that tumor cells activate autophagy in response to cellular stress [19,20,21] shed new light on potential targets for ICC. In addition to inhibiting autophagy by pharmacological agents such as chloroquine [22], it is also important to target potential autophagic biomarkers. In addition to autophagy, several reports which analyzed ICC tissues found significant differences in biomarkers between intrahepatic and extrahepatic cholangiocarcinoma, such as ARID1A, IDH1 and TP53 [23,24,25].
Autophagy, a major intracellular degradation system, is involved in many pathological and physiological functions of organisms. However, its promoting and suppressing effects in tumorigenesis, inflammatory responses, apoptosis and reactive oxygen species generation make autophagy a double-edged sword in the cancer setting [26,27,28,29]. Autophagy has been reported to promote tumor cell survival, tumor progression and metastatic tumor recurrence [30, 31]. The mammalian autophagy gene Beclin-1 plays an important role in the localization of autophagic proteins to a pre-autophagosomal structure, and thus Beclin-1 can coordinately regulate the autophagy activation and endocytic trafficking of autophagosomes [32]. However, recent studies found that Beclin-1 was negatively correlated with disease progression in cholangiocarcinoma patients [33, 34]. Lower Beclin-1 expression was associated with poor overall survival (OS) and progression-free survival (PFS). This association suggests that, in addition to Beclin-1, a variety of biological markers should be considered simultaneously in the identification of cancer prognosis and treatment, particularly ICC.
Recently, several biological markers were also reported to be associated with the prognosis of ICC, such as AT-rich interactive domain 1A (ARID1A), hypoxia-regulated carbonic anhydrase IX (CA9) and isocitrate dehydrogenase 1 (IDH1). ARID1A is generally considered as a tumor-suppressor gene because reduced expression of ARID1A has been found in a variety of tumors and correlated with tumor progression. Lower ARID1A expression was associated with a lower OS rate and lower disease-free survival rate in ICC [35]. CA9 is a known prognostic marker for many cancers, such as ovarian cancer [36, 37], esophageal and gastric adenocarcinomas [38], breast cancer [39] and rectal cancer [40, 41], as well as ICC [42]. CA9 is a transmembrane protein that contributes to microenvironmental acidification and subsequently augments the metastatic potential. Interestingly, CA9 can be released into the circulation by ectodomain shedding, which then influence its biological function [43]. Isocitrate dehydrogenases (IDH) are crucial in cellular metabolism, particularly in tumor cells [44]. IDH1 is responsible for generating NADPH from NADP+ by catalyzing the oxidative decarboxylation of isocitrate to 2-ketoglutarate. IDH1 mutation has been identified in a variety of tumor types, such as glioma [45], acute myelogenous leukemia [46, 47], central and periosteal cartilaginous tumors [48] and ICC [49, 50]. IDH1 mutation is associated with a good prognosis in patients with glioma [51, 52] but with a worse prognosis in ICC patients [53].
The study represents the results of a histopathological retrospective study of 113 patients with ICC, and the first simultaneous examination of the expression of Beclin-1, ARID1A, IDH1 and CA9 and their association with ICC. The aim of this study was to elucidate whether Beclin-1, ARID1A, IDH1 and CA9 can be simultaneously used to determine prognosis in ICC.
Methods
Patients and tissue specimens
The histopathological retrospective study enrolled 113 patients who received ICC surgery from Cancer Hospital of Chinese Academy of Medical Sciences (CAMS) between January 1999 and June 2015. The study population included patients with complete ICC tumor resection; postoperative pathological confirmation that the tumor was ICC; preoperative image confirmation of no distal metastasis and completed follow-up; and availability of paraffin-embedded tissue samples for subsequent immunohistochemistry analysis. We excluded patients with mixed types of liver cancer, other malignancies, those who died during the perioperative period and those who died of a cause unrelated to cancer. All tumor specimens were collected from Cancer Hospital, CAMS from January 1999 to June 2015. The study was performed in accordance with the Declaration of Helsinki and the protocol and study were approved by the Ethics Committee of CAMS. Informed written consent was obtained from all patients.
Pre-surgery clinicopathological characteristics
Prior to surgery, the following characteristics were evaluated: gender, age, hepatitis B surface antigen, pre-operative γ-glutamyl transpeptidase, pre-operative total bilirubin, pre-operative alkaline phosphatase, pre-operative tumor markers (CA19–9, CEA and AFP), extent of tumor differentiation, tumor type, number of tumor foci, maximum diameter of the tumor, lymph node metastasis, vascular involvement, intravascular cancer embolus, nerve involvement, involvement of the hepatic capsule, extra-hepatic involvement, tumor necrosis, mucus and hepatic cirrhosis.
Post-surgery follow-up
Follow-up post-surgery was conducted through hospital and/or telephone visits. Patients were followed until death or October 8, 2015. Patients had chest X-ray, enhanced computed tomography (CT) and analysis of the presence of tumor markers (CA19–9, CEA and AFP) every three months during the first two years following surgery. If abnormalities were observed or recurrence was assessed by imaging and the presence of tumor markers, biopsy or surgery was performed to confirm diagnosis. The treatment strategy for recurrence was mainly based on the comprehensive consideration of the tumor characteristics, liver function and the patient’s general condition. Local curative treatment consisted of re-hepatectomy and radiofrequency ablation (RFA) and systemic palliative treatment, such as molecular targeted therapy and chemotherapy were performed as alternative methods for recurrence treatment. RFS was defined as the time from the date of surgery to the date of detected recurrence or last follow up. OS was defined as the time from the date of surgery to the date of death or last follow up.
Score of immunohistochemistry staining
Immunohistochemistry was performed on paraffin embedded tissue samples. Briefly, tissues were sectioned into 5 μm thickness. After deparaffinization and hydration, antigen retrieval was performed by incubating with 3% hydrogen peroxide to block endogenous peroxidase. After washing and bovine serum albumin blocking, the specimen was incubated with the primary antibody at 4 °C overnight. Primary antibodies used in this study included the following: for Beclin-1, sc-11,427 H300 (1:100, Santa-Cruz Biotechnology, Santa-Cruz, CA, USA), for ARIDIA, sc-32,761 PSG3 (1:200, Santa-Cruz Biotechnology), for IDH1, Clone OTI24A2 (1:150, Origene Technologies, Rockville, MD, USA) and for CA9, Clone OTI1G7 (1:150, Origene Technologies). Sections were then washed with phosphate-buffered saline, incubated with a PV-9000 Polymer Detection System (PV-9000, GBI Labs, Mukilteo, WA, USA) and color-related with 3,3′-diaminobenzidine solution (ZLI-9018, Zhongshan, Beijing, China). The staining intensity and proportion of positive cells were determined in the same section. Positive cells had light yellow or brown granules. Staining intensity was determined according to the staining characteristics of most cells (contrast to the background) and was scored as follows: no staining, 0 (None); light yellow, 1 (Weak); brown yellow, 2 (Moderate); brown, 3 (Strong). Ten fields were randomly selected at a high magnification (400×), 300 cells were counted in each field and the proportion of positive cells was determined and scored as follows: 0, 0–10% positive cells; 1, 11–25% positive cells; 2, 26–50% positive cells; 3, > 50% positive cells. The staining intensity and proportion of positive cells were determined for each field, and the total score was the sum of both scores: 0, negative (grade 0); 1–2, weakly positive (grade 1); 3–4, moderate positive (grade 2); 5–6; strong positive (grade 3). All sections were scored independently by two experienced pathologists.
Statistics analysis
All demographic and cancer characteristics were presented as categorical variables, and the differences in Beclin-1, ARID1A, IDH1 and CA9 expression by groups were analyzed by Pearson’s chi-squared test. Death and disease recurrence rates were estimated according to Beclin-1, ARID1A, IDH1 and CA9 expression. Cox’s proportional hazards regression model was constructed to estimate the association of death or disease recurrence with each demographic and cancer characteristics according to Beclin-1, ARID1A, IDH1, and CA9 expression. Demographic and cancer features with significantly higher crude hazard ratios (HRs) for death or recurrence risk were further included in the multiple regression model to explore the adjusted HRs for the different factors. Survival curves for OS and RFS were presented using the Kaplan-Meier approach. Log-rank tests were performed to examine differences in OS and RFS rates by levels of expression of Beclin-1 and ARID1A.
Results
Higher Beclin-1 expression is associated with higher mortality and recurrence
A total of 113 tissue samples from ICC patients were separately stained with specific antibodies to examine the expression levels of Beclin-1, ARIDIA, CA9 and IDH1. Representative examples of positive and negative immunohistochemical staining of Beclin-1, ARID1A, CA9 and DH1 were shown in Fig. 1. The distribution of staining intensities among the four grades were shown in Table 1. Results of immunohistochemical staining showed that the four biomarkers were highly expressed in ICC tumor tissues. A total of 97 (85.9%) and 77 (68.2%) tumor tissues exhibited positive immunohistochemical staining for Beclin-1 and ARID1A, respectively; 96 (85.0%) and 105 (92.9%) samples stained positive for CA9 and IDH1, respectively.
To investigate the relationship between clinical prognosis and the four biomarkers, the above 113 cases of ICC patients were followed up. There was no significant association between ICC mortality and the expression of ARID1A, CA9 or IDH1 (Table 2). However, a higher mortality rate was associated with Beclin-1 expression (HR = 2.39, 95% Confidence Interval [CI]: 1.09–5.24). Compared with grade 0, ICC patients with histologic grade 2 of Beclin-1 expression had a 3.02-fold higher risk of mortality (95% CI: 1.32–6.91); those with histological grade 3 had a 2.95-fold higher risk of mortality (95% CI: 1.22–7.12). We further examined the association of disease recurrence and the four biomarkers (Table 3). There was a 2.75- and 3.19-fold increased risk of recurrence in grade 2 and grade 3 Beclin-1 expression, respectively (grade 2, 95% CI: 1.26–6.00; grade 3, 95% CI: 1.38–7.37). In addition to Beclin-1, ARID1A expression was associated with a 1.71-fold higher risk of recurrence (95% CI: 1.06–2.78). No significant association was found between risk of disease recurrence and the expression of CA9 and IDH1.
Association of clinical features with the expression of Beclin-1 and ARID1A
The patients’ demographic characteristics and the expression of Beclin-1 and ARID1A were listed in Additional file 1: Table S1. The distribution of most baseline characteristics was similar between the Beclin-1 negative and Beclin-1 positive group and between the ARID1A negative and ARID1A positive group. The clinical variables considered as potential predictors of risk of death and recurrence in ICC patients were listed in Additional file 1: Table S2. A multivariate analysis was performed to analyze the independent association of Beclin-1 and ARID1A with the risk of death or disease recurrence in ICC patients. As shown in Table 4, Beclin-1 expression was strongly associated with the risk of death (adjusted HR = 2.51, 95% CI = 1.05–5.99), while ARID1A was significantly correlated with the risk of death (adjusted HR = 1.95, 95% CI = 1.09–3.47) and the risk of disease recurrence (adjusted HR = 2.08, 95% CI = 1.23–3.51).
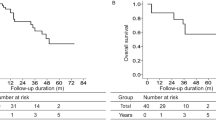
Association of Beclin-1 and ARID1A expression with prognosis
Kaplan-Meier survival curves showed that high levels of Beclin-1 were associated with poor prognosis. The OS rate for those with high levels of Beclin-1 expression was significantly shorter than that for those with low levels of Beclin-1 expression (p < 0.05; Fig. 2a). In contrast, the OS rate for those with high levels of ARID1A expression was lower than that of those with low ARID1A expression, but the difference was not statistically significant (p = 0.07; Fig. 2b). On the other hand, high levels of expression of both Beclin-1 and ARID1A were significantly associated with lower RFS rates when compared with low Beclin-1 and ARID1A expression (p < 0.05; Fig. 2c and d). Taking all cases together, we found that ICC patients with high levels of expression of both Beclin-1 and ARID1A had the lowest OS rate (Fig. 3a) and the highest disease recurrence rate (Fig. 3b). The expression of CA9 and IDH1 in these double positive Beclin-1 and ARID1A patients was further analyzed. Interestingly, we found that IDH1 and CA9 were both positively expressed in most patients with positive Beclin-1 and ARID1A. Of the 70 patients with double positive expression of Beclin-1 and ARID1A, 59 showed positive expression of IDH1 and CA9. However, the difference with other groups was not statistically significant (p = 0.732 for mortality and p = 0.505 for recurrence). Collectively, the study indicated that Beclin-1 and ARID1A, but not CA9 or IDH1, can be used simultaneously as prognostic factors for clinical outcomes in ICC patients.
Discussion
ICC is a malignant neoplasm in the biliary duct system with a high mortality rate. Despite continuous improvement in surgical techniques, the prognosis for ICC remains poor. Even after combined surgical resection, radiotherapy and adjuvant chemotherapy, the recurrence rate is still high because of regional invasiveness and distant metastasis. Although several valuable biomarkers have been reported to be associated with the prognosis of ICC, few studies have systematically explored the prognostic value of these biomarkers. These potential biomarkers include serum carbohydrate antigen 19–9 (CA19–9), interleukin-6 (IL-6), Beclin-1, ARID1A, CA9 and IDH1. However, we found that levels of CA19–9 and IL-6 were easily influenced by factors other than the presence of ICC. The serum level of CA19–9 was also increased in patients with other tumors such as gastric cancer or pancreatic cancer. Although the inflammatory cytokine IL-6 was increased in ICC patients, it is easily elevated in response to other inflammatory stimuli. Thus, this study excluded CA19–9 and IL-6, and conducted a histopathological retrospective study to assess simultaneously the prognostic value of Beclin-1, ARIDIA, IDHA and CA9 in the OS and disease recurrence of patients with ICC.
Our study found that ICC patients with higher Beclin-1 expression had a greater risk of mortality and disease recurrence. Interestingly, Beclin-1 is an essential protein for autophagy which play multiple roles in tumor progression and suppression. Existing reports on the prognostic role of autophagy or autophagy-associated proteins such as Beclin-1 in tumor progression are often contradictory. Higher Beclin-1 expression was suggested to be a positive prognostic factor for patients with colorectal cancers [54], oral tongue squamous cell carcinoma [55] and natural killer T-cell lymphoma [56]. However, other reports found higher expression of Beclin-1 associated with a poor prognosis in endometrial adenocarcinomas [57] or nasopharyngeal carcinoma [58]. As to the association of Beclin-1 and cholangiocarcinoma, our histopathological retrospective study found that higher expression of Beclin-1 was significantly associated with a poor OS rate and recurrence-free rate. However, the result is different from that of Dong et al., who reported that lower Beclin-1 expression was associated with worse OS [34]. Although our study included more patients, this difference in results may arise from differences in the included patient characteristics, therapeutic surgery used or the influence of other prognostic factors. Thus, in addition to Beclin-1, other potential prognostic markers such as ARID1A should be included simultaneously in the histopathological determination of OS or RFS.
ARID1A, a member of the switching defective/sucrose non-fermenting complexes, is generally considered a tumor suppressor gene in breast cancer [59], hepatocellular carcinoma [60] and pancreatic cancer [61]. However, recent studies demonstrated that ARID1A has dual roles in both oncogenicity and tumor suppression [62, 63]. ARID1A can promote tumor initiation through CYP450-mediated oxidative damage. Consistent with our study, we found that increased expression of ARID1A was associated with a higher risk of mortality and disease recurrence in ICC patients. However, Yang et al. reported that low expression of ARIDIA correlated with poor prognosis in patients with ICC. The difference may be due to their small number of patients, only 57 ICC patients. In addition, the dual roles of ARID1A may contribute to the difference in results between studies. Therefore, using multiple prognostic factors, especially for contradictory prognostic factors, may avoid inconsistencies.
Recently, CA9 and IDH1 were reported to be diagnostic factors for cholangiocarcinoma [42, 49, 50]. However, our study showed no significant relationship between CA9 or IDH1 and risk of mortality or disease recurrence in ICC patients. Although the expression of IDH1 was largely increased in ICC patients (8 negative vs. 105 positive), IDH1 level was not associated with mortality (HR = 1.05; 95% CI: 0.42–2.61) or disease recurrence (HR = 1.29; 95% CI: 0.52–3.2). It is likely that IDH1 gene mutation, but not the protein level, is the crucial factor contributing to ICC pathogenesis, mortality and disease recurrence. Mutation in the IDH1 gene might not significant alter the protein level; thus, histological staining for IDH1 could not be used to diagnose ICC. On the other hand, the hypoxia-regulated CA9 is not only expressed on the cell surface, but also released into the circulation by ectodomain shedding and functions as an indicator of therapeutic outcome. Of interest, the results of Hektoen et al. demonstrated that an increase in circulating CA9 was associated with a better PFS rate in patients with rectal cancer. In contrast to Korkeila’s immunohistochemical analysis of CA9 [40], disease-free survival was significantly shorter in patients with moderate/strong CA9 staining intensity. This discrepancy may indicate that intracellular and circulating CA9 may contribute to different prognostic outcomes. Thus, it is possible that the level of circulating CA9 may not indicate the prognostic value of immunohistochemical CA9 in ICC patients. This issue warrants further investigation.
Since the results of this study, especially for Beclin-1, contradict those of other studies [33, 34], we should point out that the recognition epitopes of the antibodies used may have led to the observed contradictory findings. However, the Beclin-1 antibody in this study was the same as in the study by Wang et al. (Santa Cruz, sc-11,427 H300). Although Dong et al. used a different Beclin-1 antibody, the antibody was generated by using the same immunogenic region of Beclin-1 (aa 1–300). Thus, the observed contradictory findings of Beclin-1 were likely not caused by the recognition epitope of the Beclin-1 antibody. Of interest, the antibodies used by Korkeila et al. and Gu et al. were generated by aa 359–459 (Abcam, ab15086) and aa 200–300 (Abcam, ab108351) of CA9, respectively [40, 42]. However, the CA9 antibody used in this study (Origene, OTI1G7) was generated from a full-length CA9 immunogen. Structurally, CA9 consists of a transmembrane segment, an N-terminal proteoglycan-like domain, a catalytic domain and an intracytoplasmic portion [64]. Of interest, the immunogenic region used in these studies was the extracellular region of CA9. Whether the recognized epitopes other than the transmembrane segment of CA9 are related to the observed contradictory findings warrants further investigation.
Conclusion
In summary, to determine the biomarkers associated with mortality and disease recurrence in ICC, the study simultaneously evaluated four controversial prognostic factors: Beclin-1, ARID1A, CA9 and IDH1. Although CA9 and IDH1 did not show great prognostic effects in the risk of mortality and disease recurrence of ICC, both Beclin-1 and ARID1A were highly correlated with poor prognosis in ICC patients. Of importance, patients with high expression of both Beclin-1 and ARID1A had very poor OS and RFS rates. Collectively, the result of this study showed that Beclin-1 and ARIDIA can be simultaneously used as prognostic indicators to predict disease recurrence and mortality in ICC patients.
Abbreviations
- ARID1A:
-
AT-rich interactive domain 1A
- CA9:
-
carbonic anhydrase IX
- CAMS:
-
Cancer Hospital of Chinese Academy of Medical Sciences
- CT:
-
Computed tomography
- ICC:
-
Intrahepatic cholangiocarcinoma
- IDH1:
-
Isocitrate dehydrogenase 1
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- RFA:
-
Radiofrequency ablation
References
Endo I, Gonen M, Yopp AC, Dalal KM, Zhou Q, Klimstra D, D'Angelica M, DeMatteo RP, Fong Y, Schwartz L, et al. Intrahepatic cholangiocarcinoma: rising frequency, improved survival, and determinants of outcome after resection. Ann Surg. 2008;248(1):84–96.
Nathan H, Aloia TA, Vauthey JN, Abdalla EK, Zhu AX, Schulick RD, Choti MA, Pawlik TM. A proposed staging system for intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2009;16(1):14–22.
Palmer WC, Patel T. Are common factors involved in the pathogenesis of primary liver cancers? A meta-analysis of risk factors for intrahepatic cholangiocarcinoma. J Hepatol. 2012;57(1):69–76.
Welzel TM, Graubard BI, Zeuzem S, El-Serag HB, Davila JA, McGlynn KA. Metabolic syndrome increases the risk of primary liver cancer in the United States: a study in the SEER-Medicare database. Hepatology. 2011;54(2):463–71.
Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part III: liver, biliary tract, and pancreas. Gastroenterology. 2009;136(4):1134–44.
Shin HR, Oh JK, Masuyer E, Curado MP, Bouvard V, Fang Y, Wiangnon S, Sripa B, Hong ST. Comparison of incidence of intrahepatic and extrahepatic cholangiocarcinoma--focus on east and south-eastern Asia. Asian Pac J Cancer Prev. 2010;11(5):1159–66.
Singal AK, Vauthey JN, Grady JJ, Stroehlein JR. Intra-hepatic cholangiocarcinoma--frequency and demographic patterns: thirty-year data from the M.D. Anderson Cancer center. J Cancer Res Clin Oncol. 2011;137(7):1071–8.
Briggs CD, Neal CP, Mann CD, Steward WP, Manson MM, Berry DP. Prognostic molecular markers in cholangiocarcinoma: a systematic review. Eur J Cancer. 2009;45(1):33–47.
Khan SA, Thomas HC, Davidson BR, Taylor-Robinson SD. Cholangiocarcinoma. Lancet. 2005;366(9493):1303–14.
Puhalla H, Schuell B, Pokorny H, Kornek GV, Scheithauer W, Gruenberger T. Treatment and outcome of intrahepatic cholangiocellular carcinoma. Am J Surg. 2005;189(2):173–7.
Shinohara ET, Mitra N, Guo M, Metz JM. Radiation therapy is associated with improved survival in the adjuvant and definitive treatment of intrahepatic cholangiocarcinoma. Int J Radiat Oncol Biol Phys. 2008;72(5):1495–501.
Tamandl D, Herberger B, Gruenberger B, Puhalla H, Klinger M, Gruenberger T. Influence of hepatic resection margin on recurrence and survival in intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2008;15(10):2787–94.
Yedibela S, Demir R, Zhang W, Meyer T, Hohenberger W, Schonleben F. Surgical treatment of mass-forming intrahepatic cholangiocarcinoma: an 11-year Western single-center experience in 107 patients. Ann Surg Oncol. 2009;16(2):404–12.
Zografos GN, Farfaras A, Zagouri F, Chrysikos D, Karaliotas K. Cholangiocarcinoma: principles and current trends. Hepatobiliary Pancreat Dis Int. 2011;10(1):10–20.
Hyder O, Marques H, Pulitano C, Marsh JW, Alexandrescu S, Bauer TW, Gamblin TC, Sotiropoulos GC, Paul A, Barroso E, et al. A nomogram to predict long-term survival after resection for intrahepatic cholangiocarcinoma: an eastern and Western experience. JAMA Surg. 2014;149(5):432–8.
Sakamoto Y, Kokudo N, Matsuyama Y, Sakamoto M, Izumi N, Kadoya M, Kaneko S, Ku Y, Kudo M, Takayama T, et al. Proposal of a new staging system for intrahepatic cholangiocarcinoma: analysis of surgical patients from a nationwide survey of the liver Cancer study Group of Japan. Cancer. 2016;122(1):61–70.
Zhou H, Jiang X, Li Q, Hu J, Zhong Z, Wang H, Wang H, Yang B, Hu H. A simple and effective prognostic staging system based on clinicopathologic features of intrahepatic cholangiocarcinoma. Am J Cancer Res. 2015;5(5):1831–43.
Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A, Madhusudan S, Iveson T, Hughes S, Pereira SP, et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010;362(14):1273–81.
Carew JS, Medina EC, Esquivel JA 2nd, Mahalingam D, Swords R, Kelly K, Zhang H, Huang P, Mita AC, Mita MM, et al. Autophagy inhibition enhances vorinostat-induced apoptosis via ubiquitinated protein accumulation. J Cell Mol Med. 2010;14(10):2448–59.
Thorburn A, Thamm DH, Gustafson DL. Autophagy and cancer therapy. Mol Pharmacol. 2014;85(6):830–8.
Huang CC, Lee CC, Lin HH, Chen MC, Lin CC, Chang JY. Autophagy-regulated ROS from xanthine oxidase acts as an early effector for triggering late mitochondria-dependent apoptosis in Cathepsin S-targeted tumor cells. PLoS One. 2015;10(6):e0128045.
Jia B, Xue Y, Yan X, Li J, Wu Y, Guo R, Zhang J, Zhang L, Li Y, Liu Y, et al. Autophagy inhibitor chloroquine induces apoptosis of cholangiocarcinoma cells via endoplasmic reticulum stress. Oncol Lett. 2018;16(3):3509–16.
Churi CR, Shroff R, Wang Y, Rashid A, Kang HC, Weatherly J, Zuo M, Zinner R, Hong D, Meric-Bernstam F, et al. Mutation profiling in cholangiocarcinoma: prognostic and therapeutic implications. PLoS One. 2014;9(12):e115383.
Ross JS, Wang K, Gay L, Al-Rohil R, Rand JV, Jones DM, Lee HJ, Sheehan CE, Otto GA, Palmer G, et al. New routes to targeted therapy of intrahepatic cholangiocarcinomas revealed by next-generation sequencing. Oncologist. 2014;19(3):235–42.
Zou S, Li J, Zhou H, Frech C, Jiang X, Chu JS, Zhao X, Li Y, Li Q, Wang H, et al. Mutational landscape of intrahepatic cholangiocarcinoma. Nat Commun. 2014;5:5696.
He Y, She H, Zhang T, Xu H, Cheng L, Yepes M, Zhao Y, Mao Z. p38 MAPK inhibits autophagy and promotes microglial inflammatory responses by phosphorylating ULK1. J Cell Biol. 2018;217(1):315–28.
Huang CC, Chen KL, Cheung CHA, Chang JY. Autophagy induced by cathepsin S inhibition induces early ROS production, oxidative DNA damage, and cell death via xanthine oxidase. Free Radic Biol Med. 2013;65:1473–86.
White E, DiPaola RS. The double-edged sword of autophagy modulation in cancer. Clin Cancer Res. 2009;15(17):5308–16.
Qian M, Fang X, Wang X. Autophagy and inflammation. Clin Transl Med. 2017;6(1):24.
Vera-Ramirez L, Vodnala SK, Nini R, Hunter KW, Green JE. Autophagy promotes the survival of dormant breast cancer cells and metastatic tumour recurrence. Nat Commun. 2018;9(1):1944.
Degenhardt K, Mathew R, Beaudoin B, Bray K, Anderson D, Chen G, Mukherjee C, Shi Y, Gelinas C, Fan Y, et al. Autophagy promotes tumor cell survival and restricts necrosis, inflammation, and tumorigenesis. Cancer Cell. 2006;10(1):51–64.
Kang R, Zeh HJ, Lotze MT, Tang D. The Beclin 1 network regulates autophagy and apoptosis. Cell Death Differ. 2011;18(4):571–80.
Wang TT, Cao QH, Chen MY, Xia Q, Fan XJ, Ma XK, Lin Q, Jia CC, Dong M, Ruan DY, et al. Beclin 1 deficiency correlated with lymph node metastasis, predicts a distinct outcome in intrahepatic and extrahepatic cholangiocarcinoma. PLoS One. 2013;8(11):e80317.
Dong LW, Hou YJ, Tan YX, Tang L, Pan YF, Wang M, Wang HY. Prognostic significance of Beclin 1 in intrahepatic cholangiocellular carcinoma. Autophagy. 2011;7(10):1222–9.
Yang SZ, Wang AQ, Du J, Wang JT, Yu WW, Liu Q, Wu YF, Chen SG. Low expression of ARID1A correlates with poor prognosis in intrahepatic cholangiocarcinoma. World J Gastroenterol. 2016;22(25):5814–21.
Hynninen P, Vaskivuo L, Saarnio J, Haapasalo H, Kivela J, Pastorekova S, Pastorek J, Waheed A, Sly WS, Puistola U, et al. Expression of transmembrane carbonic anhydrases IX and XII in ovarian tumours. Histopathology. 2006;49(6):594–602.
Choschzick M, Oosterwijk E, Muller V, Woelber L, Simon R, Moch H, Tennstedt P. Overexpression of carbonic anhydrase IX (CAIX) is an independent unfavorable prognostic marker in endometrioid ovarian cancer. Virchows Arch. 2011;459(2):193–200.
Driessen A, Landuyt W, Pastorekova S, Moons J, Goethals L, Haustermans K, Nafteux P, Penninckx F, Geboes K, Lerut T, et al. Expression of carbonic anhydrase IX (CA IX), a hypoxia-related protein, rather than vascular-endothelial growth factor (VEGF), a pro-angiogenic factor, correlates with an extremely poor prognosis in esophageal and gastric adenocarcinomas. Ann Surg. 2006;243(3):334–40.
Hussain SA, Ganesan R, Reynolds G, Gross L, Stevens A, Pastorek J, Murray PG, Perunovic B, Anwar MS, Billingham L, et al. Hypoxia-regulated carbonic anhydrase IX expression is associated with poor survival in patients with invasive breast cancer. Br J Cancer. 2007;96(1):104–9.
Korkeila E, Talvinen K, Jaakkola PM, Minn H, Syrjanen K, Sundstrom J, Pyrhonen S. Expression of carbonic anhydrase IX suggests poor outcome in rectal cancer. Br J Cancer. 2009;100(6):874–80.
Hektoen HH, Flatmark K, Andersson Y, Dueland S, Redalen KR, Ree AH. Early increase in circulating carbonic anhydrase IX during neoadjuvant treatment predicts favourable outcome in locally advanced rectal cancer. BMC Cancer. 2015;15:543.
Gu M. CA9 overexpression is an independent favorable prognostic marker in intrahepatic cholangiocarcinoma. Int J Clin Exp Pathol. 2015;8(1):862–6.
Zatovicova M, Pastorekova S. Modulation of cell surface density of carbonic anhydrase IX by shedding of the ectodomain and endocytosis. Acta Virol. 2013;57(2):257–64.
Al-Khallaf H. Isocitrate dehydrogenases in physiology and cancer: biochemical and molecular insight. Cell Biosci. 2017;7:37.
Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, Kos I, Batinic-Haberle I, Jones S, Riggins GJ, et al. IDH1 and IDH2 mutations in gliomas. N Engl J Med. 2009;360(8):765–73.
Green CL, Evans CM, Hills RK, Burnett AK, Linch DC, Gale RE. The prognostic significance of IDH1 mutations in younger adult patients with acute myeloid leukemia is dependent on FLT3/ITD status. Blood. 2010;116(15):2779–82.
Ward PS, Patel J, Wise DR, Abdel-Wahab O, Bennett BD, Coller HA, Cross JR, Fantin VR, Hedvat CV, Perl AE, et al. The common feature of leukemia-associated IDH1 and IDH2 mutations is a neomorphic enzyme activity converting alpha-ketoglutarate to 2-hydroxyglutarate. Cancer Cell. 2010;17(3):225–34.
Amary MF, Bacsi K, Maggiani F, Damato S, Halai D, Berisha F, Pollock R, O'Donnell P, Grigoriadis A, Diss T, et al. IDH1 and IDH2 mutations are frequent events in central chondrosarcoma and central and periosteal chondromas but not in other mesenchymal tumours. J Pathol. 2011;224(3):334–43.
Borger DR, Tanabe KK, Fan KC, Lopez HU, Fantin VR, Straley KS, Schenkein DP, Hezel AF, Ancukiewicz M, Liebman HM, et al. Frequent mutation of isocitrate dehydrogenase (IDH)1 and IDH2 in cholangiocarcinoma identified through broad-based tumor genotyping. Oncologist. 2012;17(1):72–9.
Saha SK, Parachoniak CA, Ghanta KS, Fitamant J, Ross KN, Najem MS, Gurumurthy S, Akbay EA, Sia D, Cornella H, et al. Mutant IDH inhibits HNF-4alpha to block hepatocyte differentiation and promote biliary cancer. Nature. 2014;513(7516):110–4.
Sonoda Y, Kumabe T, Nakamura T, Saito R, Kanamori M, Yamashita Y, Suzuki H, Tominaga T. Analysis of IDH1 and IDH2 mutations in Japanese glioma patients. Cancer Sci. 2009;100(10):1996–8.
Parsons DW, Jones S, Zhang X, Lin JC, Leary RJ, Angenendt P, Mankoo P, Carter H, Siu IM, Gallia GL, et al. An integrated genomic analysis of human glioblastoma multiforme. Science. 2008;321(5897):1807–12.
Jiao Y, Pawlik TM, Anders RA, Selaru FM, Streppel MM, Lucas DJ, Niknafs N, Guthrie VB, Maitra A, Argani P, et al. Exome sequencing identifies frequent inactivating mutations in BAP1, ARID1A and PBRM1 in intrahepatic cholangiocarcinomas. Nat Genet. 2013;45(12):1470–3.
Yang Z, Ghoorun RA, Fan X, Wu P, Bai Y, Li J, Chen H, Wang L, Wang J. High expression of Beclin-1 predicts favorable prognosis for patients with colorectal cancer. Clin Res Hepatol Gastroenterol. 2015;39(1):98–106.
Hu Z, Zhong Z, Huang S, Wen H, Chen X, Chu H, Li Q, Sun C. Decreased expression of Beclin1 is significantly associated with a poor prognosis in oral tongue squamous cell carcinoma. Mol Med Rep. 2016;14(2):1567–73.
Huang JJ, Li HR, Huang Y, Jiang WQ, Xu RH, Huang HQ, Lv Y, Xia ZJ, Zhu XF, Lin TY, et al. Beclin 1 expression: a predictor of prognosis in patients with extranodal natural killer T-cell lymphoma, nasal type. Autophagy. 2010;6(6):777–83.
Giatromanolaki A, Koukourakis MI, Koutsopoulos A, Chloropoulou P, Liberis V, Sivridis E. High Beclin 1 expression defines a poor prognosis in endometrial adenocarcinomas. Gynecol Oncol. 2011;123(1):147–51.
Wan XB, Fan XJ, Chen MY, Xiang J, Huang PY, Guo L, Wu XY, Xu J, Long ZJ, Zhao Y, et al. Elevated Beclin 1 expression is correlated with HIF-1alpha in predicting poor prognosis of nasopharyngeal carcinoma. Autophagy. 2010;6(3):395–404.
Mamo A, Cavallone L, Tuzmen S, Chabot C, Ferrario C, Hassan S, Edgren H, Kallioniemi O, Aleynikova O, Przybytkowski E, et al. An integrated genomic approach identifies ARID1A as a candidate tumor-suppressor gene in breast cancer. Oncogene. 2012;31(16):2090–100.
He F, Li J, Xu J, Zhang S, Xu Y, Zhao W, Yin Z, Wang X. Decreased expression of ARID1A associates with poor prognosis and promotes metastases of hepatocellular carcinoma. J Exp Clin Cancer Res. 2015;34:47.
Zhang L, Wang C, Yu S, Jia C, Yan J, Lu Z, Chen J. Loss of ARID1A expression correlates with tumor differentiation and tumor progression stage in pancreatic ductal adenocarcinoma. Technol Cancer Res Treat. 2018;17:1533034618754475.
Otto JE, Kadoch C. A two-faced mSWI/SNF subunit: dual roles for ARID1A in tumor suppression and Oncogenicity in the liver. Cancer Cell. 2017;32(5):542–3.
Sun X, Wang SC, Wei Y, Luo X, Jia Y, Li L, Gopal P, Zhu M, Nassour I, Chuang JC, et al. Arid1a has context-dependent oncogenic and tumor suppressor functions in liver Cancer. Cancer Cell. 2018;33(1):151–2.
Opavsky R, Pastorekova S, Zelnik V, Gibadulinova A, Stanbridge EJ, Zavada J, Kettmann R, Pastorek J. Human MN/CA9 gene, a novel member of the carbonic anhydrase family: structure and exon to protein domain relationships. Genomics. 1996;33(3):480–7.
Acknowledgments
The authors would like to thank Dr. Yiling Zheng for give some advice during the revision stage.
Funding
This work was supported by the Beijing Hope Run Special Fund of Cancer Foundation of China (LC2018A15), the PUMC Fund of the Funds for the Central Universities (3332018193) and National Natural Science Foundation (81641113).
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
CB and ML conceptually designed the experiments, analyzed and interpreted the data, and drafted the manuscript. WR performed part of the experiments and provided technical support. FW, YZ and YL performed the clinical studies and data acquisition. SL performed the literature search and analysis of the clinical data. JW developed the concept for this study and provided approval of the investigation. LW performed statistical analysis and provided critical revision of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Review Committee reviewed and approved the protocol (#81641113). Written informed consent was obtained from all study participants.
Consent for publication
Not Applicable.
Competing interests
All authors declare no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Table S1. Demographic and clinical characteristics of ICC patients with the expression of Becin-1 and ARID1A (n = 113).Table S2. Death and recurrence risk with baseline characteristics for patients with intrahepatic cholangiocarcinoma (n = 113). (DOCX 32 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bi, C., Liu, M., Rong, W. et al. High Beclin-1 and ARID1A expression corelates with poor survival and high recurrence in intrahepatic cholangiocarcinoma: a histopathological retrospective study. BMC Cancer 19, 213 (2019). https://doi.org/10.1186/s12885-019-5429-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-019-5429-3