Abstract
Background
The key-stone-pathogen, Porphyromonas gingivalis associates not only with periodontal diseases but with a variety of other chronic diseases such as cancer. We previously reported an association between the presence of Porphyromonas gingivalis in esophageal squamous cell carcinoma (ESCC) and its progression. We now report the diagnostic and prognostic potential of serum immunoglobulin G and A antibodies (IgG/A) against Porphyromonas gingivalis for ESCC.
Methods
An enzyme-linked immunosorbent assay (ELISA) was used to determine the serum levels of Porphyromonas gingivalis IgG and IgA in 96 cases with ESCC, 50 cases with esophagitis and 80 healthy controls.
Results
The median serum levels of IgG and IgA for P. gingivalis were significantly higher in ESCC patients than non-ESCC controls. P. gingivalis IgG and IgA in serum demonstrated sensitivities/specificities of 29.17%/96.90% and 52.10%/70.81%, respectively, and combination of IgG and IgA produced a sensitivity/specificity of 68.75%/68.46%. The diagnostic performance of serum P. gingivalis IgA for early ESCC was superior to that of IgG (54.54% vs. 20.45%). Furthermore, high serum levels of P. gingivalis IgG or IgA were associated with worse prognosis of ESCC patients, in particular for patients with stage 0-IIor negative lymphnode metastasis, and ESCC patients with high levels of both IgG and IgA had the worst prognosis. Multivariate analysis revealed that lymph node status, IgG and IgA were independent prognostic factors.
Conclusions
The IgG and IgA for P. gingivalis are potential serum biomarkers for ESCC and combination of IgG and IgA improves the diagnostic and prognostic performance. Furthermore, serum P. gingivalis IgG and IgA can detect early stage ESCC.
Similar content being viewed by others
Background
Esophageal squamous cell carcinoma (ESCC) remains the predominant histological subtype of esophageal carcinoma and ranks as the fourth most common cancer in terms of both incidence and mortality in China [1, 2]. Although significant advances in diagnostic and therapeutic modalities have improved the prognosis of ESCC patients, the overall 5-year survival rate still ranges from 25% to 30%, mainly due to advanced stage at initial presentation [1, 3,4,5,6,7]. On the other hand, accurate staging and prognosis is difficult to assess at diagnosis, which hampers ESCC tailoring therapy, treatment efficiency and recurrence monitoring. It is, therefore, imperative to identify novel biomarkers for early detection, metastasis and recurrence to reduce ESCC-related morbidity and mortality.
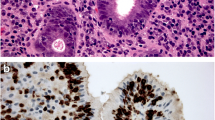
A number of epidemiological and clinical studies have reported a positive association between the conditions of oral microbiome, periodontal disease or tooth loss and the progression of multiple cancers [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25], and even gastric precancerous lesions [26, 27]. The oral microbiome inhabiting the oral cavity contains multiple species in a complex community that generally exist in a balanced immunoinflammatory state with the host [28]. Disruption of this equilibrium has deleterious effects on the mucosal lining, surrounding tissues and even distant organs and systems of human body through the combined effects of a dysbiotic microbial community and a dysregulated immune response [12, 13, 29]. Porphyromonas gingivalis has become regarded as a key-stone pathogen and is closely associated with periodontal diseases, a variety of presumably unrelated chronic diseases and multiple cancers [30, 31]. Although the self-reported tooth loss may have a microbial basis in the case of esophageal cancer [16, 17], there is no convincing evidence of direct and specific microbial etiologic agents until our recent findings, which revealed a higher frequency (61%) of P. gingivalis presence in ESCC [18].
As P. gingivalisis is an important periodontal pathogen in various types of periodontal disease, numerous studies have reported that antibody responses to P. gingivalis correlate with severity and progression of periodontitis, extent of attachment loss and treatment effects [32,33,34,35,36]. In a cohort study of NHANES III, not only the increasing severity of periodontitis but the higher serum IgG for P. gingivalis was associated with increased orodigestive cancer mortality [25]. In another European prospective cohort study, high levels of antibodies to P. gingivalis rendered a > 2-fold increased risk to pancreatic cancer [21]. In clinical settings, serum tumor biomarkers take priority over other measures for screening, diagnosis and clinical management of cancer. However, conventional serum markers for ESCC, such as squamous cell carcinoma antigen (SCCA), carcinoembryonic antigen (CEA), CYFRA21-1 and carbohydrate antigen (CA)19-9, lack sufficient sensitivity and specificity for the early detection and progression of ESCC [37,38,39,40,41].
On the grounds of our recent study establishing the association between the infection of P. gingivalis in esophageal epithelium and progression of ESCC, herein we investigate the serum levels of immunoglobulin G and A (IgG and IgA) for P. gingivalis and their clinical significance for the diagnosis and postoperative prognosis of ESCC.
Methods
Patients
The first cohort of 96 preoperative serum samples were recruited from ESCC patients, who underwent curative esophagectomy at the First Affiliated Hospital of Henan University of Science & Technology and Anyang people’s hospital. None of ESCC patients received preoperative neoadjuvant chemoradiotherapy. The clinical stage of ESCC was classified in accordance with the seventh edition of AJCC and early stage was defined as AJCC stage 0 + I + IIA. Another cohort of 50 serum samples were collected from patients with esophagitis, who underwent gastroscopy. In addition, 80 healthy individuals without evidence of comorbid disease were recruited as healthy controls from the physical examination center of our hospital.
Enzyme-linked immunosorbent assay
P. gingivalis ATCC 33277, used as the antigen in our experiment, was cultured and prepared as previously described. For enzyme-linked immunosorbent assay (ELISA), 100 ul of reconstituted protein extracts of P. gingivalis (10 μg/ml) was used to coat microtiter plates followed by incubation with 1:200 diluted serum incubation, 1: 1000 biotin-conjugated anti-human IgG and IgA, and 1:400 avidin-conjugated peroxidase. Antibodies levels were expressed as ELISA units (EUs) with the use of a reference serum pool [42].
Statistical analysis
The statistical analyses were performed using SPSS 19.0 software package (SPSS, Chicago, IL, USA). Data are expressed as mean ± standard deviation (SD). Comparisons between groups were performed using t tests. The receiver operating characteristic (ROC) was used to determine the optimal cut-off value of IgG and IgA. The accuracy, sensitivity, specificity, false negative rate (FNR), false positive rate (FPR) and area under the ROC (AUC) were used to assess the classification efficiency. Overall survival (OS) was defined as the interval between the date of surgery and the date of death or the date of last follow-up. Follow-up data was available for 80 ESCC patients with a median follow-up interval of 10.5 months (3.0-42.6 months). Clinical stage and lymph node metastasis were available for 78 ESCC patients. Survival curves were plotted using the Kaplan-Meier method and differences between curves were tested by log-rank tests. The significance of prognostic factors on survival was studied by Cox regression model.
Results
Levels of serum IgG and IgA for P. gingivalis in ESCC
The details of ESCC characteristics are presented in Table 1. Figure 1 shows the frequency distributions of IgG and IgA for P. gingivalis across the three cohorts. As there were no significant differences between healthy controls and non-ESCC patients with esophagitis with regards to serum levels of P. gingivalis IgG or IgA, we combined these two cohorts as non-ESCC controls hereafter. The median serum levels of IgG and IgA for P. gingivalis were significantly higher in ESCC patients than in non-ESCC controls (150.69 EU vs. 109.13 EU, P < 0.001 for IgG; 33.16 EU vs. 19.14 EU, P < 0.01 for IgA). However, no significant correlation was found between serum levels of P. gingivalis IgG and IgA (r2 = 0.03, P > 0.05, data not shown).
Enzyme-linked immunosorbent assay (ELISA) of serum IgG and IgA antibodies to P. gingivalis in healthy controls (n = 80), patients with esophagitis (n = 50) and ESCC (n = 96). a Scatter plots of ELISA units (EUs) of P. gingivalis IgG antibody in serum of healthy controls, patients with esophagitis and ESCC. b Scatter plots of ELISA units (EUs) of P. gingivalis IgA antibody in serum of healthy controls, patients with esophagitis and ESCC
Seeking to determine the diagnostic potential of P. gingivalis IgG and IgA, ROC curves were plotted to distinguish 96 patients of ESCC from 130 non-ESCC controls. As shown in Fig. 2a, AUCs of IgG and IgA for P. gingivalis were 0.612 and 0.632, with optimal cut-off values of 189.17 EU and 21.25 EU, respectively. The specificity for IgG was higher (96.90%) than that of IgA (70.81%) but not the sensitivity (29.17% vs. 52.10%, Fig. 2b). Combination of IgG and IgA, i.e. seropositivity for at least one subtype of IgG or IgA antibody, produced an AUC of 0.686 with a sensitivity of 68.75% and a specificity of 68.46%, respectively (Fig. 2a). Figure 2b shows the diagnostic performance of IgG, IgA, and combination of IgG and IgA in terms of accuracy, sensitivity, specificity, FNR and FPR.
Receiver operating characteristic (ROC) curves and clinical performances of P. gingivalis IgG and IgA. a ROC curves of IgG, IgA and combination of IgG and IgA for P. gingivalis as a diagnostic marker for discrimination of ESCC and non-ESCC controls. b Clinical performances of IgG, IgA and combination of IgG and IgA for P. gingivalis as a diagnostic marker for discrimination of ESCC and non-ESCC controls in terms of accuracy, sensitivity, specificity, false negative rate (FNR), false positive rate (FPR). c Time-dependent ROC curves of IgG, IgA and combination of IgG and IgA for P. gingivalis as predictors of ESCC-related 3-year survival rates. d Clinical performances of IgG, IgA and combination of IgG and IgA for P. gingivalis predictors of ESCC-related 3-year survival rates in terms of accuracy, sensitivity, specificity, false negative rate (FNR), false positive rate (FPR)
Diagnostic value of IgG and IgA for P. gingivalis in early stage of ESCC.
There were 44 patients with early stage disease in our cohort of ESCC. The mean value of P. gingivalis IgA in early stage ESCC was lower (32.08 EU) than that of late stage ESCC (41.76 EU) without statistical significance (P = 0.29), whereas the mean IgG value was marginally higher in early stage ESCC (114.35 EU vs. 113.62 EU, P = 0.058). The sensitivity of P. gingivalis IgA for detection of early stage ESCC was 54.54% (24/44) with a specificity of 70.82%, and was far better than that of IgG (20.45%, (9/44)).
Associations between P. gingivalis IgG and IgA with clinicopathological features and overall survival of ESCC
The associations between clinicopathological features of ESCC and serum levels of IgG or IgA for P. gingivalis were determined by t test. No significant associations were observed between any clinicopathological features with IgG or IgA serum levels. Likewise, ROCs were plotted to predict the 3-year OS rate of ESCC. Figure 2c shows the time-dependent ROC curves of P. gingivalis antibodies as predictors of ESCC-related 3-year survival rates and the AUCs were 0.595 and 0.719 with optimal cut-off values of 125.08 EU and 37.12 EU for IgG and IgA, respectively. The sensitivity of P. gingivalis IgA was higher than that of IgG (86.25% vs. 47.82%) but not the specificity (57.54% vs. 71.92%, Fig. 2d). Likewise, combination of IgG and IgA produced a maximal AUC (0.746), a maximal sensitivity (87.16%) but a modest specificity (62.07%) in comparison with individual IgG or IgA (Fig. 2d).
Figure 3a shows the postoperative survival of 80 ESCC patients with a median survival time of 31.58 months, 61 surviving patients and 19 ESCC-related deaths at the last clinical follow-up (Fig. 3a). Using the optimal cut-off value of 138.23 EU, Kaplan-Meier survival analysis revealed that ESCC patients with higher serum level of P. gingivalis IgG had a significantly worse prognosis than ESCC with lower serum level (log-rank test, x2 = 4.852, P = 0.028, median OS of 26.25 (n = 19) months vs. 33.68 months (n = 61), Fig. 3b). The prognostic effect of P. gingivalis IgA resembled that of IgG (log-rank test, x2 = 6.800, P = 0.006, median OS of 19.59 months (n = 16) vs. 34.15 months (n = 64), Fig. 3c). In 50 ESCC patients with lower IgG or IgA serum level, the median OS was 36.12 months compared with 25.89 months of their counterparts (log-rank test, x2 = 7.208, P = 0.007, Fig. 3d). Furthermore, 5 ESCC patients with higher levels of both IgG and IgA had the worst prognosis and the median OS for these 5 patients was 16.62 months versus 32.93 months of the other 75 patients (log-rank test, x2 = 8316, P = 0.004, Data now shown).
Kaplan-Meier survival curves of ESCC patients. a The 3-year OS rate of 80 ESCC patients was 52.23%. b The 3-year OS rates in ESCC patients with IgG < 138.23 EU (n = 61) and IgG > 138.23 EU (n = 19) were 70.145% and 32.68%, respectively, with a significant difference (P = 0.028). c The 3-year OS rates in ESCC patients with IgA < 56.56 EU (n = 64) and IgG > 56.56 EU (n = 16) were 60.82% and 18.83%, respectively, with a significant difference (P = 0.006). d The 3-year OS rates in ESCC patients with IgG < 138.23 EU or IgA < 56.56 (n = 50) and IgG > 138.23 EU or IgA > 56.56 (n = 30) were 76.38% and 34.04%, respectively, with a significant difference (P = 0.007)
The prognostic values of histopathological features were also evaluated by Kaplan-Meier method and log-rank test. With regards to clinical TNM stage, stage I–II ESCC patients (stage I–II, 63.75%, n = 51) survived longer than stage III–IV ESCC cases (Stage III–IV, 36.25%, n = 27, Additional file 1: Figure S1A). For the subgroup ESCC patients with early clinical stage, a significant benefit in OS was observed in patients with low serum level of P. gingivalis IgA but non-significant for IgG than in patients with high level (log-rank test, x2 = 9.141, P = 0.003, Additional file 1: Figure S1B & D), and neither IgG nor IgA was associated with OS of late stage ESCC (Additional file 1: Figure S1C &E). In addition, lymph node metastasis was significantly associated with shorter OS ((log-rank test, x2 = 5.61, P = 0.018, Additional file 2: Figure S2A). In ESCC patients with negative lymph node metastasis, those with high levels of P. gingivalis IgG or IgA had worse OS than patients with low IgG or IgA serum level (log-rank test, x2 = 6.097/6.097, P = 0.014/0.011, Additional file 2: Figure S2B & D), whereas no significant differences were observed between P. gingivalis IgG or IgA and OS in positive lymph node metastasis (Additional file 2: Figure S2C & E).
To identify independent prognostic factors for ESCC patients, clinicopathological factors were assessed by univariate and multivariate Cox regression models. Univariate Cox proportional hazard regression analysis revealed that N-stage (Hazard ratio = 3.169, 95% CI = 1.175 – 8.545, P = 0.023), IgG (Hazard ratio = 3.039, 95% CI = 1.148 – 8.041, P = 0.025) and IgA (Hazard ratio = 3.588, 95% CI = 1.368 – 9.409, P = 0.009) were significant prognostic predictors for OS of ESCC patients (Table 2). When N-stage, IgG and IgA were analysed by multivariate analysis using Cox’s proportional hazards model, N-stage (Hazard ratio = 12.292, 95% CI = 1.399 – 108.003, P = 0.024), IgG (Hazard ratio = 4.910, 95% CI = 1.473– 16.364, P = 0.010) and IgA (Hazard ratio = 4.686, 95% CI = 1.492 – 14.722, P = 0.008) were independent prognostic factors of ESCC (Table 2).
Discussion
Early diagnosis remains one of the key determinants to improve the long-term survival of patients with ESCC. The majority of patients with ESCC present at an advanced stage and have limited treatment options, resulting in dismal prognosis [1, 3,4,5,6,7]. Although gastroscopy with biopsy offers an efficient method for diagnosis of patients with ESCC, poor compliance of gastroscopy in asymptomatic patients precludes early detection. Compared with gastroscopy, blood testing is less invasive and cost-effective. Therefore, serum biomarkers have the priority over other measures for clinical application to detect ESCC at an early stage [43].
First and foremost, the present study demonstrates that serum antibody levels against P. gingivalis have the potential for diagnosis of ESCC. Although inflammation plays a key role in esophageal carcinogenesis, our results revealed that morphological esophagitis harboring inflammatory cells without transformed cells in esophageal mucosa failed to show increased IgG and IgA antibody response to P. gingivalis. This finding indicates that P. gingivalis may not be involved in the process of esophagitis, but do not rule out the possibility that P. gingivalis or host responses against P. gingivalis contribute to the development and progression of ESCC. In sharp contrast, titers of IgG and IgA against P. gingivalis in serum of patients with ESCC increased remarkably compared to patients with esophagitis and healthy controls, which provides direct evidence that P. gingivalis is implicated in the pathogenesis of ESCC. Using an optimal diagnostic cut off value of 425 EU, individual IgA had the highest sensitivity (52.1%) for discrimination of ESCC from non-ESCC controls compared with conventional serum markers for ESCC, such as SCCA, CYFRA21-1, CEA, CA19-9 [37,38,39,40,41], whereas the specificity was low (70.8%). However, ELISA results of SCCA1, SCCA2, CYFRA21-1 and CEA did not show diagnostic value in our cohort (data not shown). Growing evidence indicates that combination of several individual biomarkers is superior to any single biomarker [44]. Combination of IgG and IgA for P. gingivalis had an increased AUC (0.671) compared with an individual IgG or IgA.
For detection of early stage ESCC, conventional serum biomarkers of ESCC have little diagnostic benefit. For instance, the positive frequencies of both CYFRA21-1 and SCCA in patients with early stage ESCC (stage 0-II) varied from 4.7% to 24% [37, 40]. In contrast, the diagnostic performance of serum P. gingivalis IgA for early ESCC was superior as evidenced by a sensitivity of 54.54% in our study. Although the specificity of single IgA was not sufficient, combination of IgG and IgA produced a specificity of 91.5%.
Mounting clinical evidence indicates a positive association between P. gingivalis or periodontal disease and an increased risk for a variety of cancers and even poor prognosis [11, 12, 18, 21, 25]. In normal distal esophagus, bacterial colonization was not uncommon [45]. Furthermore, the global esophageal microbiome in both esophagitis and Barrett’s esophagus altered from typeI bacteria in normal esophageal mucosa to typeIIbacteria, many of which are Gram-negative anaerobes/microaerophiles and putative pathogens of periodontal disease [46]. Our previous study demonstrated that P. gingivalis infection in ESCC was prevalent (61%) and negatively correlated with OS of ESCC [18]. In the present study, we looked into the prognostic potential of human immune response to P. gingivalis in terms of IgG and IgA. In line with the presence of P. gingivalis in ESCC, higher serum levels of P. gingivalis IgG and IgA were associated with worse prognosis of patients with ESCC. In particular for early stage ESCC, i.e. ESCC with stage 0-II or negative lymphnode metastasis, patients with high level of P. gingivalis IgG or IgA had a significantly lower OS relative to ESCC patients with low level, and patients with high level of both IgG and IgA had the worst prognosis. Multivariate analysis identified lymph node status, IgG and IgA as independent prognostic factors. Therefore, IgG and IgA were combined and we found that the combination produced higher predictive accuracy than an individual IgG or IgA.
Conclusions
To our knowledge, we are the first to report that the human immune response against P. gingivalis is implicated in the malignant progression of ESCC. IgG and IgA for P. gingivalis are potential serum biomarkers for ESCC and combination of IgG and IgA improves the diagnostic and prognostic performance. Furthermore, serum IgG and IgA for P. gingivalis could differentiate early stage ESCC patients. Further investigations are warranted to compare or combine with current serum biomarkers for ESCC, to identify the optimal panel for clinical application.
Abbreviations
- AUC:
-
Area under the ROC curve
- ESCC:
-
Esophageal squamous cell carcinoma
- IgG/A:
-
Immunoglobulin G/A
- ROC:
-
Receiving operating characteristic
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90.
Lin Y, Totsuka Y, He Y, Kikuchi S, Qiao Y, Ueda J, Wei W, Inoue M, Tanaka H. Epidemiology of esophageal cancer in Japan and China. J Epidemiol. 2013;23(4):233–42.
Enzinger PC, Mayer RJ. Esophageal cancer. N Engl J Med. 2003;349(23):2241–52.
Pennathur A, Gibson MK, Jobe BA, Luketich JD. Oesophageal carcinoma. Lancet. 2013;381(9864):400–12.
Shimada H, Nabeya Y, Okazumi S, Matsubara H, Shiratori T, Gunji Y, Kobayashi S, Hayashi H, Ochiai T. Prediction of survival with squamous cell carcinoma antigen in patients with resectable esophageal squamous cell carcinoma. Surgery. 2003;133(5):486–94.
Tang KH, Dai YD, Tong M, Chan YP, Kwan PS, Fu L, Qin YR, Tsao SW, Lung HL, Lung ML, et al. A CD90(+) tumor-initiating cell population with an aggressive signature and metastatic capacity in esophageal cancer. Cancer Res. 2013;73(7):2322–32.
Falk GW. Risk factors for esophageal cancer development. Surg Oncol Clin N Am. 2009;18(3):469–85.
Nagy KN, Sonkodi I, Szoke I, Nagy E, Newman HN. The microflora associated with human oral carcinomas. Oral Oncol. 1998;34(4):304–8.
Mager DL, Haffajee AD, Devlin PM, Norris CM, Posner MR, Goodson JM. The salivary microbiota as a diagnostic indicator of oral cancer: a descriptive, non-randomized study of cancer-free and oral squamous cell carcinoma subjects. J Transl Med. 2005;3:27.
Katz J, Onate MD, Pauley KM, Bhattacharyya I, Cha S. Presence of Porphyromonas gingivalis in gingival squamous cell carcinoma. Int J Oral Sci. 2011;3(4):209–15.
Whitmore SE, Lamont RJ. Oral bacteria and cancer. PLoS Pathog. 2014;10(3):e1003933.
Hooper SJ, Wilson MJ, Crean SJ. Exploring the link between microorganisms and oral cancer: a systematic review of the literature. Head Neck. 2009;31(9):1228–39.
Ahn J, Chen CY, Hayes RB. Oral microbiome and oral and gastrointestinal cancer risk. Cancer Causes Control. 2012;23(3):399–404.
Groeger S, Domann E, Gonzales JR, Chakraborty T, Meyle J. B7-H1 and B7-DC receptors of oral squamous carcinoma cells are upregulated by Porphyromonas gingivalis. Immunobiology. 2011;216(12):1302–10.
Tezal M, Sullivan MA, Hyland A, Marshall JR, Stoler D, Reid ME, Loree TR, Rigual NR, Merzianu M, Hauck L, et al. Chronic periodontitis and the incidence of head and neck squamous cell carcinoma. Cancer Epidemiol Biomark Prev. 2009;18(9):2406–12.
Hiraki A, Matsuo K, Suzuki T, Kawase T, Tajima K. Teeth loss and risk of cancer at 14 common sites in Japanese. Cancer Epidemiol Biomark Prev. 2008;17(5):1222–7.
Abnet CC, Qiao YL, Mark SD, Dong ZW, Taylor PR, Dawsey SM. Prospective study of tooth loss and incident esophageal and gastric cancers in China. Cancer Causes Control. 2001;12(9):847–54.
Gao S, Li S, Ma Z, Liang S, Shan T, Zhang M, Zhu X, Zhang P, Liu G, Zhou F, et al. Presence of Porphyromonas gingivalis in esophagus and its association with the clinicopathological characteristics and survival in patients with esophageal cancer. Infect Agent Cancer. 2016;11:3.
Abnet CC, Kamangar F, Dawsey SM, Stolzenberg-Solomon RZ, Albanes D, Pietinen P, Virtamo J, Taylor PR. Tooth loss is associated with increased risk of gastric non-cardia adenocarcinoma in a cohort of Finnish smokers. Scand J Gastroenterol. 2005;40(6):681–7.
Watabe K, Nishi M, Miyake H, Hirata K. Lifestyle and gastric cancer: a case-control study. Oncol Rep. 1998;5(5):1191–4.
Michaud DS, Izard J, Wilhelm-Benartzi CS, You DH, Grote VA, Tjonneland A, Dahm CC, Overvad K, Jenab M, Fedirko V, et al. Plasma antibodies to oral bacteria and risk of pancreatic cancer in a large European prospective cohort study. Gut. 2013;62(12):1764–70.
Michaud DS. Role of bacterial infections in pancreatic cancer. Carcinogenesis. 2013;34(10):2193–7.
Stolzenberg-Solomon RZ, Dodd KW, Blaser MJ, Virtamo J, Taylor PR, Albanes D. Tooth loss, pancreatic cancer, and helicobacter pylori. Am J Clin Nutr. 2003;78(1):176–81.
Michaud DS, Joshipura K, Giovannucci E, Fuchs CS. A prospective study of periodontal disease and pancreatic cancer in US male health professionals. J Natl Cancer Inst. 2007;99(2):171–5.
Ahn J, Segers S, Hayes RB. Periodontal disease, Porphyromonas gingivalis serum antibody levels and orodigestive cancer mortality. Carcinogenesis. 2012;33(5):1055–8.
Salazar CR, Sun J, Li Y, Francois F, Corby P, Perez-Perez G, Dasanayake A, Pei Z, Chen Y. Association between selected oral pathogens and gastric precancerous lesions. PLoS One. 2013;8(1):e51604.
Salazar CR, Francois F, Li Y, Corby P, Hays R, Leung C, Bedi S, Segers S, Queiroz E, Sun J, et al. Association between oral health and gastric precancerous lesions. Carcinogenesis. 2012;33(2):399–403.
Hajishengallis G, Lamont RJ. Beyond the red complex and into more complexity: the polymicrobial synergy and dysbiosis (PSD) model of periodontal disease etiology. Mol Oral Microbiol. 2012;27(6):409–19.
Jenkinson HF. Beyond the oral microbiome. Environ Microbiol. 2011;13(12):3077–87.
Meyer MS, Joshipura K, Giovannucci E, Michaud DS. A review of the relationship between tooth loss, periodontal disease, and cancer. Cancer Causes Control. 2008;19(9):895–907.
Atanasova KR, Yilmaz O. Looking in the Porphyromonas gingivalis cabinet of curiosities: the microbium, the host and cancer association. Mol Oral Microbiol. 2014;29(2):55–66.
Tribble GD, Kerr JE, Wang BY. Genetic diversity in the oral pathogen Porphyromonas gingivalis: molecular mechanisms and biological consequences. Future Microbiol. 2013;8(5):607–20.
Naito Y, Okuda K, Takazoe I. Detection of specific antibody in adult human periodontitis sera to surface antigens of Bacteroides Gingivalis. Infect Immun. 1987;55(3):832–4.
Ebersole JL, Taubman MA, Smith DJ, SocranskySS. Humoral immune responses and diagnosis of human periodontal disease. J Periodontal Res. 1982;17(5):478–80.
Vincent JW, Falkler WA Jr, Cornett WC, Suzuki JB. Effect of periodontal therapy on specific antibody responses to suspected periodontopathogens. J Clin Periodontol. 1987;14(7):412–7.
Mooney J, Adonogianaki E, Riggio MP, Takahashi K, Haerian A, Kinane DF. Initial serum antibody titer to Porphyromonas gingivalis influences development of antibody avidity and success of therapy for chronic periodontitis. Infect Immun. 1995;63(9):3411–6.
Kosugi S, Nishimaki T, Kanda T, Nakagawa S, Ohashi M, Hatakeyama K. Clinical significance of serum carcinoembryonic antigen, carbohydrate antigen 19-9, and squamous cell carcinoma antigen levels in esophageal cancer patients. World J Surg. 2004;28(7):680–5.
Shimada H, Nabeya Y, Tagawa M, Okazumi S, Matsubara H, Kadomatsu K, Muramatsu T, Ikematsu S, Sakuma S, Ochiai T. Preoperative serum midkine concentration is a prognostic marker for esophageal squamous cell carcinoma. Cancer Sci. 2003;94(7):628–32.
Mealy K, Feely J, Reid I, McSweeney J, Walsh T, Hennessy TP. Tumour marker detection in oesophageal carcinoma. Eur J Surg Oncol. 1996;22(5):505–7.
Shimada H, Nabeya Y, Okazumi S, Matsubara H, Miyazawa Y, Shiratori T, Hayashi H, Gunji Y, Ochiai T. Prognostic significance of CYFRA 21-1 in patients with esophageal squamous cell carcinoma. J Am Coll Surg. 2003;196(4):573–8.
Zheng X, Xing S, Liu XM, Liu W, Liu D, Chi PD, Chen H, Dai SQ, Zhong Q, Zeng MS, et al. Establishment of using serum YKL-40 and SCCA in combination for the diagnosis of patients with esophageal squamous cell carcinoma. BMC Cancer. 2014;14:490.
Ogawa T, Kusumoto Y, Hamada S, McGhee JR, Kiyono H. Bacteroides Gingivalis-specific serum IgG and IgA subclass antibodies in periodontal diseases. Clin Exp Immunol. 1990;82(2):318–25.
Hsu FM, Cheng JC, Chang YL, Lee JM, Koong AC, Chuang EY. Circulating mRNA profiling in esophageal Squamous cell carcinoma identifies FAM84B as a biomarker in predicting pathological response to Neoadjuvant Chemoradiation. Sci Rep. 2015;5:10291.
Xu YW, Peng YH, Chen B, Wu ZY, Wu JY, Shen JH, Zheng CP, Wang SH, Guo HP, Li EM, et al. Autoantibodies as potential biomarkers for the early detection of esophageal squamous cell carcinoma. Am J Gastroenterol. 2014;109(1):36–45.
Pei Z, Bini EJ, Yang L, Zhou M, Francois F, Blaser MJ. Bacterial biota in the human distal esophagus. Proc Natl Acad Sci U S A. 2004;101(12):4250–5.
Yang L, Lu X, Nossa CW, Francois F, Peek RM, Pei Z. Inflammation and intestinal metaplasia of the distal esophagus are associated with alterations in the microbiome. Gastroenterology. 2009;137(2):588–97.
Acknowledgements
We thank Dr. Huizhi Wang and Dr. David A. Scott from Department of Oral Immunology and Infectious Diseases, University of Louisville School of Dentistry, for providing P. gingivalis protein extract for ELISA assay.
Funding
This study was supported by the National Natural Science Foundation of China (81,472,234, U1604191), Science and Technology Innovation Team Program for Universities of Henan (15IRTSTHN024), Science and Technology Major Project of Henan (161100311200). The funding body had no role in the design of the study, collection, analysis, and interpretation of data or in writing the manuscript.
Availability of data and materials
All datasets supporting our conclusions are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
SGG and XSF conceived and designed the study. YJQ drafted the manuscript. ZKM and XY collected the blood samples and performed ELISA assays. HW collected part of blood samples and JQY collected the follow-up data of ESCC patients. JQY, CZ and GCW were responsible for statistical analyses. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Henan University of Science and Technology. All ESCC patients and non-ESCC controls gave informed written consents prior to sample collection. This study was conducted in accordance with the Declaration of Helsinki and the ethical standards of the committee on human experimentation of the institution.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1: Figure S1.
Kaplan-Meier survival curves of ESCC patients with regards to clinical stage. A The 3-year OS rates in ESCC patients with TNMI-II (n = 51) and patients with TNM III-IV (n = 27) were 59.95% and 33.26%, respectively (P = 0.069). B The 3-year OS rates in ESCC patients with IgG < 138.23 EU (n = 59) and IgG > 138.23 EU (n = 19) were 77.59% and 37.65%, respectively, in early clinical stage (P = 0.055). B The 3-year OS rates in ESCC patients with IgG < 138.23 EU (n = 59) and IgG > 138.23 EU (n = 19) were 44.63% and 20.89%, respectively, in late clinical stage (P = 0.055). D The 3-year OS rates in ESCC patients with IgA < 56.56 EU (n = 62) and IgA > 56.56 EU (n = 16) were 68.95% and 23.34%, respectively, in early clinical stage (P = 0.003). D The 3-year OS rates in ESCC patients with IgA < 56.56 EU (n = 62) and IgA > 56.56 EU (n = 16) were 41.45% and 0, respectively, in late clinical stage (P = 0.48). (DOC 334 kb)
Additional file 2: Figure S2.
Kaplan-Meier survival curves of ESCC patients with regards to lymph node stage. A The 3-year OS rates in ESCC patients without lymph node metastasis (n = 44) and patients with lymph node metastasis (n = 34) were 63.87% and 27.85%, respectively (P = 0.018). B The 3-year OS rates in ESCC patients with IgG < 138.23 EU (n = 59) and IgG > 138.23 EU (n = 19) were 87.19% and 37.64%, respectively, in negative lymph node metastasis (P = 0.014). C The 3-year OS rates in ESCC patients with IgG < 138.23 EU (n = 59) and IgG > 138.23 EU (n = 19) were 29.43% and 20.80%, respectively, in lymph node metastasis (P = 0.293). D The 3-year OS rates in ESCC patients with IgA < 56.56 EU (n = 62) and IgA > 56.56 EU (n = 16) were 72.91% and 25.96%, respectively, in negative lymph node metastasis (P = 0.011). E The 3-year OS rates in ESCC patients with IgA < 56.56 EU (n = 62) and IgA > 56.56 EU (n = 16) were 34.52% and 0, respectively, in lymph node metastasis (P = 0.092). (DOC 355 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Gao, SG., Yang, JQ., Ma, ZK. et al. Preoperative serum immunoglobulin G and A antibodies to Porphyromonas gingivalis are potential serum biomarkers for the diagnosis and prognosis of esophageal squamous cell carcinoma. BMC Cancer 18, 17 (2018). https://doi.org/10.1186/s12885-017-3905-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-017-3905-1