Abstract
Background
Chronic hepatitis B (CHB) virus infection is a major cause of hepatocellular carcinoma (HCC), as late diagnosis is the main factor for the poor survival of patients. There is an urgent need for accurate biomarkers for early diagnosis of HCC. The aim of the study was to explore the serum lipidome profiles of hepatitis B-related HCC to identify potential diagnostic biomarkers.
Methods
An ultraperformance liquid chromatography mass spectrometry (UPLC-MS) lipidomic method was used to characterize serum profiles from HCC (n = 32), liver cirrhosis (LC) (n = 30), CHB (n = 25), and healthy subjects (n = 34). Patients were diagnosed by clinical laboratory and imaging evidence and all presented with CHB while healthy controls had normal liver function and no infectious diseases.
Results
The UPLC-MS-based serum lipidomic profile provided more accurate diagnosis for LC patients than conventional alpha-fetoprotein (AFP) detection. HCC patients were discriminated from LC with 78 % sensitivity and 64 % specificity. In comparison, AFP showed sensitivity and specificity of 38 % and 93 %, respectively. HCC was differentiated from CHB with 100 % sensitivity and specificity using the UPLC-MS approach. Identified lipids comprised glycerophosphocolines, glycerophosphoserines and glycerophosphoinositols.
Conclusions
UPLC-MS lipid profiling proved to be an efficient and convenient tool for diagnosis and screening of HCC in a high-risk population.
Similar content being viewed by others
Background
Hepatitis B virus (HBV) infection is one of the main causes of chronic liver disease worldwide. It is estimated that 240 million individuals are chronically infected with HBV [1]. Depending on the presence of co-factors, progression to liver cirrhosis (LC) may occur at a rate of 2 to 10 % per year, whereas hepatocellular carcinoma (HCC) may develop in 2–4 % of patients per year. HBV is estimated to be responsible for 30 % of cirrhosis- and 45 % of HCC-related deaths [2].
In Brazil, HBV accounts for 13–25 % of HCC cases in most geographical regions, reaching 40 % of HCC cases in the Mid-west [3].
HCC is a complex and heterogeneous tumor with several genomic alterations and its incidence has been increasing worldwide. It is the sixth most common cancer and the second cause of cancer-related death. When diagnosed at an early stage, surgical options such as resection or liver transplantation, or local ablative therapies, can be applied with intent to cure HCC. However, until now, no effective serum or plasma biomarkers have been found for accurate screening or diagnosis of HCC [4, 5].
HCC diagnosis is most commonly performed by ultrasound examination, CT scan and/or magnetic resonance. Histopathology confirmation may also be necessary in some cases. However, there are some limitations related to risk of complications and feasibility of the biopsy due to tumor location. Moreover, the effectiveness of ultrasound for early detection of HCC is highly dependent on the stage of liver fibrosis, the quality of the equipment and the expertise of the operator [4].
Alpha-fetoprotein (AFP) is the most widely used biomarker for HCC. However, its sensitivity is only up to 60 % and elevated AFP levels are also common in LC and chronic liver disease [6]. Thus, there is an urgent need to identify better HCC biomarkers.
The ideal biomarker should be specific and able to discriminate HCC from regenerative nodules irrespective of the stage of liver disease. Furthermore, the biomarker should be sensitive, allowing detection at an early stage, and should be easily measurable, reproducible, and minimally invasive.
Recently developed mass spectrometry (MS)-based techniques such as lipidomics are promising tools for the discovery and subsequent identification of molecules associated with various diseases. Separation techniques, like ultraperformance liquid chromatography (UPLC), coupled to MS enable the analysis of complex samples such as plasma or serum with very high sensitivity and accuracy [7, 8].
Once lipid biomarkers are identified through UPLC-MS, they can be later investigated in clinical laboratory routine using simple and accessible colorimetric and/or enzymatic techniques. Nonetheless, studies on lipid profiling and fingerprinting of HCC are still scarce [9–12].
The aim of this study was to assess the serum lipid patterns of HCC by performing UPLC-MS to search for potential biomarkers for diagnosis in HBV chronic infected patients (HBV-HCC).
Methods
Study design, sample and data collection
A total of 87 patients with chronic hepatitis B (CHB) were enrolled from 2012 to 2014 at the Hospital das Clínicas of the University of Sao Paulo School of Medicine, including 32 patients with HBV-HCC, 30 patients with HBV-LC and 25 patients with CHB. Additionally, 34 eligible blood donors with normal liver function and no infectious diseases were recruited at COLSAN Beneficent Association for Blood Collection to serve as healthy controls. CHB was diagnosed based on the presence of HBsAg for at least 6 months. LC was diagnosed by histopathology, clinical features and/or elastography and HCC was diagnosed using imaging or histopathology techniques, in accordance with guidelines of the Brazilian Society of Hepatology.
Blood samples were obtained by venipuncture and drained into blood collection tubes. The samples were centrifuged immediately after collection and serum was stored at −80 °C until analysis.
Demographic, clinical and laboratory data were collected from medical records. The study was approved by the ethics committee of human research of the Federal University of Sao Paulo and the University of São Paulo School of Medicine (2012/81656 and 2014/569922) and all patients gave written informed consent.
Extraction of lipids
Lipids were extracted from each sample using a modified Bligh-Dyer protocol [13]. Immediately after thawing, 100 μL of serum were dissolved in 850 μL of a mixture of water/chloroform/methanol (1:2.5:5, v/v) and vortexed well for 5 min. After vortexing, 250 μL of chloroform were added and the tubes were agitated for 15 min at 700 rpm. Then, 200 μL of deionized water were added and the tubes were centrifuged at 14,000 rpm for 15 min at room temperature. Following this protocol a 2-phase system (aqueous top, organic bottom) was achieved. The bottom phase containing lipids was gently recovered using a micropipette, dried, and resuspended in 350 μL of acetonitrile/water (3:2, v/v). All chemicals were of analytical reagent grade and used as received.
UPLC-MS analysis
Reversed-phased analysis was performed on a Waters ACQUITY IClass UPLC system equipped with a Waters Acquity CSH C18 1.7 μm x 2.1 × 100 mm column coupled to a Waters Synapt-MS hidrid quadrupole-time of flight mass spectrometer operating in the positive ion electrospray mode. A mass scan range of 200 to 1,200 mass-to-charge ratio (m/z) was set for data acquisition in continuous mode with optimized parameters for ionization and mass transmission. Acetonitrile/water (3:2, v/v) was used as mobile phase A and isopropanol/acetonitrile (9:1, v/v) was used as mobile phase B, both with 10 mM ammonium formate and 0.1 % formic acid as additives. The flow rate was set at 600 μL/min and the injection volume was 10 μL. A binary gradient was optimized as follows: the composition of mobile phase B was changed from 15 % to 30 % in 2 min, then to 48 % in 30 s and reached 82 % in 8.5 min. Subsequently, it was changed to 99 % in 30 s, held for another 30 s and then dropped to 15 % in 6 s prior to being held until a total run time of 15 min. The mass spectrometer was previously calibrated with 0.1 % phosphoric acid in water/acetonitrile (1:1, v/v) and a solution of 0.5 ng/μL leucine enkephalin in water/acetonitrile (1:1, v/v) with 0.1 % formic acid infused in the reference probe at a flow rate of 5 μL/min was used as lock mass spray at a 30 s frequency for accurate mass determination. All analyses were acquired using the lock spray and the instrument was recalibrated every 4 run-hours to ensure accuracy and reproducibility. Furthermore, a quality control of pool plasma samples was analyzed after every 10 runs, and 10 peaks well distributed from 200 to 1,200 m/z were assessed.
Data pretreatment and statistical data analyses
All data obtained from the UPLC-MS analyses were processed with the Waters Progenesis software (Manchester, UK). This step included mass correction, chromatograms and spectra alignment and peak detection using default parameters. After attribution, the matrix of the features characterized by their m/z and retention time (RT) was uploaded into the MetaboAnalyst 3.0 (The Metabolomics Innovation Centre, Canada). For normalization, data was mean-centered and divided by the square root of standard deviation of each variable (Pareto scaling).
For multivariate analysis, the unsupervised principal component analysis (PCA) was first utilized in all samples (Additional file 1). Supervised partial least-squares-latent structure discriminate analysis (PLS-DA) was then performed to identify biomarkers that contributed to the clustering. Validation with a permutation test and 100 repetitions was performed to prevent model overfitting. Potential biomarkers that differentiated HCC from LC, CH and healthy subjects (HS) were selected based on the variable importance in the projection (VIP) values and univariate statistical significance after Mann–Whitney test and fold-change analyses. Receiver operating characteristic (ROC) curves were performed to evaluate the accuracy of the potential biomarkers and the proposed model using the ROCCET (The Metabolomics Innovation Centre, Canada).
Statistical analyses of demographic, clinical and laboratory data of subjects were performed using SPSS version 11.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics consisted of the characterization of the studied population (demographic, clinical and laboratory characteristics) through the respective percentages or mean/median and standard deviation (SD) for continuous variables. Bivariate analysis consisted of Fisher exact test to compare categorical values. For continuous variables, Student’s t-test was use to compare means of normally distributed variables, while non-normally distributed variables were subjected to Mann–Whitney U test. Statistical significance level was P < 0.050. All reported values are 2-tailed.
A tentative identification of the differentiating lipids was performed on the LIPID MAPS and HMDB databases.
Results
The mean age of patients was 59.0 years old in the HCC group, 56.8 in the LC group, and 37.1 in the CHB group. The mean age of the HS was 42.6 years. In the HCC group 81.3 % of patients were males, while in the LC, CH and HS groups they were 66.7, 68.0 and 38.2 %, respectively (Table 1).
Clinical and laboratory data analyses were performed for the HCC and LC groups (Table 2). In summary, the mean levels of AFP, alkaline phosphatase (ALP), and gamma-glutamyl transpeptidase (GGT) were significantly higher in the HCC group, while prothrombin time (PT) was lower. Nonetheless, the Child-Pugh score distribution was only slightly different between the LC and the HCC groups, which presented 4 and 2 patients with B and C scores, respectively. Twenty-eight of the 32 HCC patients (87.5 %) presented with LC. HCC was classified as BCLC—Barcelona Clínic Liver Cancer staging system very early or early stage in 19 of the 32 cases (59.4 %), intermediate stage in 10 (31.2 %) and advanced or terminal stage in only 3 (9.4 %) cases (Additional file 2.).
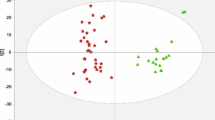
A total of 2,698 ions were detected using the UPLC-MS method in this study. Figure 1 shows the PLS-DA score plot for the 4 groups evaluated. The separate PLS-DA score plots for inter-group comparisons are shown in Fig. 2.
PLS-DA scores plot based on the UPLC-MS profiling data for the studied groups. Detailed legend: The score plots show the first, second and third latent variables. Each dot in the plot represents a patient according to its group. HCC, hepatocellular carcinoma; LC, liver cirrhosis; CH, chronic hepatitis; HS, healthy subjects
PLS-DA scores plot based on the UPLC-MS profiling data for (a) HCC versus HS; (b) HCC versus CH; (c) HCC versus LC; (d) LC versus CH versus HS. Detailed legend: The score plots show the first, second and third latent variables for each plot. Each dot in the plot represents a patient according to its group. HCC, hepatocellular carcinoma; LC, liver cirrhosis; CH, chronic hepatitis; HS, healthy subjects
Hepatocellular carcinoma versus liver cirrhosis
Four lipids independently predicted HCC from LC with 65.6–84.4 % sensitivity, and 60.0–76.7 % specificity. Figure 3 shows the intensities and ROC curves of the 4 lipids in patients with HCC and LC.
ROC curves and intensities of the differential ions in the UPLC-MS 4-peak model by RT and m/z. Detailed legend: ROC curves and intensities of the differential ions in the ULC-MS 4-peak model in HCC (red boxes) and LC (green boxes) patients for the ions (a) RT 1.30_498.8315 m/z; (b) RT 1.32_497.5731 m/z; (c) RT 1.30_496.6721 m/z; (d) RT 4.26_540.4255 m/z. AUC, area under the curve; HCC, hepatocellular carcinoma; LC, liver cirrhosis; CH, chronic hepatitis; HS, healthy subjects
Based on the efficiency of the ROC curves, cutoff values were determined for each ion. The number of “positive” ions in each sample was used to generate a 4-peak algorithm with cutoff value of at least 2 “positive” biomarkers, defined by ROC curve analysis and posterior univariate statistical validation (Fig. 4a). The 4-peak algorithm generated distinguished HCC from LC with an accuracy of 71.0 % (95 % CI 58.7–80.1 %), a sensitivity of 78.1 % (95 % CI 61.2–89.0 %), and a specificity of 63.6 % (95 % CI: 45.4–78.1 %). This algorithm successfully detected 25 of 32 HCC cases when applied to discriminate HCC from LC.
Conversely, AFP detected only 12 of 32 HCC cases from LC when cutoff value was set as 20 ng/mL, showing an accuracy of 64.5 % (95 % CI 52.1–75.3 %), a sensitivity of 37.5 % (95 % CI 22.9–54.8 %), and a specificity of 93.3 % (95 % CI: 78.7–98.2 %). In the range of 200 ng/mL, AFP detected 6 of 32 HCC cases, performing with an accuracy of 58.1 % (95 % CI 45.7–69.5 %), a sensitivity of 18.8 % (95 % CI: 8.9–35.3 %), and a specificity of 100 % (95 % CI 88.7–100.0 %) (Table 3).
The accuracy, sensitivity and specificity of HCC detection of the 4-peak algorithm was not compromised when the 6 HCC patients with Child-Pugh scores B and C were excluded from the analysis. Likewise, the HCC detection rate of the algorithm did not vary significantly when patients were stratified according to the BCLC staging system (P = 0.463). Very early or early HCC was detected with a sensitivity of 73.7 % (95 % CI: 51.2–88.2 %), and a specificity of 63.3 % (95 % CI: 45.5–78.1 %).
The combination of the 4-peak UPLC-MS algorithm with AFP in the range of 20 ng/mL was able to distinguish HCC from LC with an accuracy of 79.0 % (95 % CI 67.4–87.3 %), a sensitivity of 75 % (95 % CI 57.9–86.8 %), and a specificity of 83.3 % (95 % CI: 66.4–92.7 %).
Hepatocellular carcinoma versus chronic hepatitis B
The 4 peaks independently predicted HCC from CHB with 52–90.6 % sensitivity and 68.8–86.7 % specificity. The intensities and ROC curves of the 4 lipids in patients with HCC and CHB are shown in Additional file 3. The 4-peak algorithm distinguished HCC from CHB with an accuracy of 87.1 % (95 % CI 76.6–93.3 %), a sensitivity of 93.8 % (95 % CI 79.9–98.3 %), and a specificity of 80.0 % (95 % CI 62.7–90.5 %) (Table 3).
As the ion RT 4.26_540.4255 m/z did not perform well in this comparison, we also tested the performance of the model using different combinations of the 4 ions. The best model was a combination of the ion RT 1.30_498.8315 m/z and RT 1.32_497.5731 m/z, which with a cutoff of at least 1 “positive” ion, detected 31 of the 32 HCC cases and distinguished HCC and CHB with an accuracy of 88.7 % (95 % CI 78.5–94.4 %), a sensitivity of 96.9 % (95 % CI 84.26–99.5 %), and a specificity of 80.0 % (95 % CI 62.7–90.5 %) (Fig. 4b).
We also looked at the whole lipidomic profile of HCC and CHB and, interestingly, 7 peaks independently predicted HCC from CHB with 100 % sensitivity and specificity (Additional file 4).
Tentative identification of potential biomarkers
Table 4 shows the main classes and subclasses associated with the differentiating lipids found in this study.
Discussion
Diagnosis of HCC at an early stage is essential for disease prognosis as it allows the application of curative treatments and improves patient survival.
In the present study, an UPLC-MS-based lipidomic expression signature successfully distinguished HBV-HCC cases from HBV-LC with 78.1 % sensitivity and 63.6 % specificity and provided a more precise diagnostic instrument for cirrhotic patients than conventional non-invasive biomarker detection (AFP). Our results also show that the UPLC-MS lipidomic fingerprinting discriminated serum lipidomic expression patterns among patients with HBV-HCC, HBV-LC, and CHB.
Studies on lipidomic profiling of HCC are still scarce. Moreover, key data are lacking in the few published studies, such as comprehensive description and assessment regarding patient and background liver disease characterization, group allocation and controls adequacy, and proper performance assessment of the diagnostic model, among others [14].
The results presented herein are innovative, as this study performs a robust evaluation of patients enrolled in a well-established HCC surveillance program. These patients are, therefore, well characterized as to their clinical and laboratory parameters, which ensures the adequacy of the study groups and controls, and allows an unbiased interpretation of the proposed biomarkers and their intra-group level variations.
When used as a diagnostic biomarker, AFP is expected to misdiagnose up to 40 % of HCC cases with a 20 ng/mL cutoff value [4]. In this study, however, while the UPLC-MS-based 4-peak model accurately diagnosed 25 of 32 HCC cases from LC patients, AFP performed poorly, detecting only 12 of 32 cases with a sensitivity of 37.5 % and 93.3 % specificity.
When applied to differentiate HCC in the early stages, the UPLC-MS signature detected very early or early stage HCC with 73.7 % sensitivity and 63.3 % specificity. These data show the potential applicability of UPLC-MS for screening biomarkers for early diagnosis of HCC.
Patients at high risk of HCC development should be screened semi annually using ultrasonography (US). It is known, however, that in most cases US has only acceptable diagnosis accuracy with sensitivity ranging from 58 to 89 % and specificity greater than 90 % [4, 15, 16]. Furthermore, US effectiveness for detecting early-stage HCC is even lower, with a sensitivity of only 63 % [17]. The accuracy of the proposed UPLC-MS 4-peak model for HCC screening and the actual gain in the detection rate need to be further evaluated on larger studies. Nonetheless, the use of this model might improve HCC surveillance and diagnosis, especially in resource-limited regions where patients may have difficult access to US and higher resolution imaging techniques such as CT scan and magnetic resonance. A lipidomic biomarker and/or profile could be, in turn, detected through a simple, inexpensive and widely accessible enzyme immunoassay or chemiluminescence assay, which would represent a significant reduction on HCC screening costs.
HBV infection can lead to HCC in the absence of cirrhosis. Although little is known about the clinical and epidemiological aspects of HCC in Brazil [18], data from other regions show that 20 to 30 % of patients with HBV-related HCC do not present with LC [19]. In this study the rate of HCC in the absence of cirrhosis was 12.5 %. The UPLC-MS 4-peak detected HCC from CHB patients with of 93.8 % sensitivity and a specificity of 80.0 %. Furthermore, it was observed that some peaks not included in the first model could differentiate HCC and CHB with 100 % sensitivity and specificity.
We performed a tentative and preliminary identification of the differentially expressed peaks. At this point we have identified 3 glycerophosphoserines, 1 glycerophosphocholine and 1 glycerophosphoinositol, all in significantly lower levels in HCC patients.
Previous studies also have shown lower levels of glycerophosphocolines in HCC patients, which are the most abundant phospholipid in mammalian cellular membranes [11]. This under expression may result from the inflammatory response and consequent higher consumption of these lipids [20, 21]. CHB infection has been associated with alterations in lipid metabolism and a recent study showed that HBV infection altered the metabolic gene expression in a human liver-chimeric mouse model by altering bile acid and cholesterol metabolism as a consequence of impaired bile acid uptake [22].
Conclusions
Our findings suggest that UPLC-MS lipidomic fingerprinting may be a powerful tool for the identification of diagnostic biomarkers and models for hepatitis B virus-related HCC. These data showed that the lipid fingerprinting in HCC patients selected a number of lipids that should be functionally investigated to elucidate the pathogenesis of the disease. This technique and the selected peaks show a great potential to improve HCC surveillance in patients with LC and CHB.
References
Ott JJ, Stevens GA, Groeger J, Wiersma ST. Global epidemiology of hepatitis B virus infection: new estimates of age-specific HBsAg seroprevalence and endemicity. Vaccine. 2012;30:2212–9.
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917.
Carrilho FJ, Kikuchi L, Branco F, Gonçalves CS, Mattos AA, Brazilian HCC Study Group. Clinical and epidemiological aspects of hepatocellular carcinoma in Brazil. Clinics (Sao Paulo). 2010;65:1285–90.
European Association For The Study Of The Liver and European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908–43.
McGlynn KA, Petrick JL, London WT. Global Epidemiology of Hepatocellular Carcinoma: An Emphasis on Demographic and Regional Variability. Clin Liver Dis. 2015;19:223–38.
Bruix J, Sherman M. AASLD Practice Guideline. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–2.
Wenk MR. The emerging field of lipidomics. Nat Rev Drug Discov. 2005;4:594–610.
Hu C, van der Heijden R, Wang M, van der Greef J, Hankemeier T, Xu G. Analytical strategies in lipidomics and applications in disease biomarker discovery. J Chromatogr B Analyt Technol Biomed Life Sci. 2009;877:2836–46.
Diamond DL, Syder AJ, Jacobs JM, Sorensen CM, Walters KA, Proll SC, et al. Temporal Proteome and Lipidome Profiles Reveal Hepatitis C Virus-Associated Reprogramming of Hepatocellular Metabolism and Bioenergetics. PLoS Pathog. 2010;6:e1000719. doi:10.1371/journal.ppat.1000719.
Patterson AD, Maurhofer O, Beyoglu D, Lanz C, Krausz KW, Pabst T, et al. Aberrant Lipid Metabolism in Hepatocellular Carcinoma Revealed by Plasma Metabolomics and Lipid Profiling. Cancer Res. 2011;71:6590–600.
Wang B, Chen D, Chen Y, Hu Z, Cao M, Xie Q, et al. Metabonomic profiles discriminate hepatocellular carcinoma from liver cirrhosis by ultraperformance liquid chromatography-mass spectrometry. J Proteome Res. 2012;11:1217–27.
Zhou L, Wang Q, Yin P, Xing W, Wu Z, Chen S, et al. Serum metabolomics reveals the deregulation of fatty acids metabolism in hepatocellular carcinoma and chronic liver diseases. Anal Bioanal Chem. 2012;403:203–13.
Bligh EG, Dyer WJ. A rapid method of total lipid extraction and purification. Can J Biochem Physiol. 1959;37:911–7.
Kimhofer T, Fye H, Taylor-Robinson S, Thursz M, Holmes E. Proteomic and metabonomic biomarkers for hepatocellular carcinoma: a comprehensive review. Br J Cancer. 2015;112:1141–56.
Kim CK, Lim JH, Lee WJ. Detection of hepatocellular carcinomas and dysplastic nodules in cirrhotic liver: accuracy of ultrasonography in transplant patients. J Ultrasound Med. 2001;20:99–104.
Bolondi L. Screening for hepatocellular carcinoma in cirrhosis. J Hepatol. 2003;39:1076–84.
Singal A, Volk ML, Waljee A, Salgia R, Higgins P, Rogers MA, et al. Meta-analysis: surveillance with ultrasound for early-stage hepatocellular carcinoma in patients with cirrhosis. Aliment Pharmacol Ther. 2009;30:37–47.
Kikuchi L, Chagas AL, Alencar RS, Paranaguá-Vezozzo DC, Carrilho FJ. Clinical and epidemiological aspects of hepatocellular carcinoma in Brazil. Antivir Ther. 2013;18:445–9.
El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365:1118–27.
Sullentrop F, Moka D, Neubauer S, Haupt G, Engelmann U, Hahn J, et al. 31P NMR spectroscopy of blood plasma: determination and quantification of phospholipid classes in patients with renal cell carcinoma. NMR Biomed. 2002;15:60–8.
Lewen Jia JC, Yin P, Lu X, Guowang X. Serum metabonomics study of chronic renal failure by ultra performance liquid chromatography coupled with Q-TOF mass spectrometry. Metabolomics. 2008;4:183–9.
Oehler N, Volz T, Bhadra OD, Kah J, Allweiss L, Giersch K, et al. Binding of hepatitis B virus to its cellular receptor alters the expression profile of genes of bile acid metabolism. Hepatology. 2014;60:1483–93.
Acknowledgements
The Fleury SA Group supported this work and AMPC received a doctorate scholarship from Fundação de Amparo à Pesquisa do Estado de São Paulo – FAPESP (no. 2013/03701-0). The funding agencies did not interfere in the scientific aspects of the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AMPC, VMC, KHMC, JRRP, FJC and CFHG were responsible for study conception and design. AMPC, LC, ALC, MSGG, FM and ACSSN recruited the patients, collected the blood samples and clinical and laboratory data and performed data analysis and interpretation. AMPC, VMC and KHMC performed mass-spectrometry analysis and interpretation of data. AMPC performed the statistical analysis and drafted the manuscript. All authors participated in the critical revision, read and approved the final manuscript.
Author’s information
AMPC is currently at her final semester as a PhD Student at the Federal University of Sao Paulo. She has been awarded a highly competitive merit PhD scholarship from Fundação de Amparo à Pesquisa do Estado de São Paulo and two awards for best oral presentation at the Brazilian Congress of Virology. Moreover, the preliminary results of her PhD study have been awarded twice during international conferences. First she received a Student Travel Stipend for oral presentation by the Human Proteome Organisation for the HUPO 11th Annual World Congress and second, she received a Full Young Investigator Bursary for oral presentation of high quality abstract by the European Association for the Study of the Liver for oral presentation at the EASL 50th The International Liver Congress. Furthermore, during the short six years since she graduated as a Pharmacist and Biochemist, she has published 15 scientific articles which have been cited a total of 58 times in SCOPUS.
Additional files
Additional file 1:
PCA scores plot based on the UPLC-MS profiling data for the studied groups. The score plots show the first, second and third principal components. Each dot in the plot represents a patient according to its group. HCC, hepatocellular carcinoma; LC, liver cirrhosis; CH, chronic hepatitis; HS, healthy subjects. (TIF 1120 kb)
Additional file 2:
Distribution of HCC patients according to BCLC staging system. (TIF 62 kb)
Additional file 3:
ROC curves and intensities of the differential ions in the UPLC-MS 4-peak model by RT and m/z. ROC curves and intensities of the differential ions in HCC (red boxes) and CH (green boxes) for (A) RT 1.30_498.8315 m/z; (B) RT 1.32_497.5731 m/z; (C) RT 1.30_496.6721 m/z; (D) RT 4.26_540.4255 m/z. AUC, area under the curve; HCC, hepatocellular carcinoma; LC, liver cirrhosis; CH, chronic hepatitis; HS, healthy subjects. (TIF 4244 kb)
Additional file 4:
ROC curves and intensities of the differential ions by RT and m/z. ROC curves and intensities of the differential ions in HCC (red boxes) and CH (green boxes) for (A) RT 3.40_773.5478n; (B) RT 4.23_851.6090 m/z; (C) RT 3.59_770.5691 m/z; (D) RT 3.45_822.5670 m/z; (E) RT 6.25_369.3538 m/z; (F) RT 1.87_534.3902 m/z; (G) RT 3.99_826.5920 m/z. AUC, area under the curve; HCC, hepatocellular carcinoma; LC, liver cirrhosis; CH, chronic hepatitis; HS, healthy subjects. (TIF 7531 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Passos-Castilho, A.M., Carvalho, V.M., Cardozo, K.H.M. et al. Serum lipidomic profiling as a useful tool for screening potential biomarkers of hepatitis B-related hepatocellular carcinoma by ultraperformance liquid chromatography–mass spectrometry. BMC Cancer 15, 985 (2015). https://doi.org/10.1186/s12885-015-1995-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-015-1995-1