Abstract
Background
Definitive, percutaneous irradiation of the prostate and the pelvic lymph nodes in high-risk prostate cancer is the alternative to prostatectomy plus lymphadenectomy. To date, the role of whole pelvis radiotherapy (WPRT) has not been clarified especially taking into consideration the benefits of high conformal IMRT (intensity modulated radiotherapy) of complex-shaped target volumes.
Methods
From 2009 to 2012, 40 patients of high-risk prostate cancer with an increased risk of microscopic lymph node involvement were enrolled into this prospective phase II trial. Patients received at least two months of antihormonal treatment (AT) before radiotherapy continuing for at least 2 years. Helical IMRT (tomotherapy) of the pelvic lymph nodes (51.0 Gy) with a simultaneous integrated, moderate hypofractionated boost (single dose of 2.25 Gy) to the prostate (76.5 Gy) was performed in 34 fractions. PSA levels, prostate-related symptoms and quality of life were assessed at regular intervals for 24 months.
Results
Of the 40 patients enrolled, 38 finished the treatment as planned. Overall acute toxicity rates were low and no acute grade 3 or 4 gastrointestinal (GI) and genitourinary (GU) toxicity occurred. 21.6 % of patients experienced acute grade 2 but no late grade ≥2 GI toxicity. Regarding GU side effects, results showed 48.6 % acute grade 2 and 6.4 % late grade 2 toxicity. After a median observation time of 23.4 months the PLATIN 1 trial can be considered as sufficiently safe meeting the prospectively defined aims of the trial. With 34/37 patients free of a PSA recurrence it shows promising efficacy.
Conclusion
Tomotherapy of the pelvic lymph nodes with a simultaneous integrated boost to the prostate can be performed safely and without excessive toxicity. The combined irradiation of both prostate and pelvic lymph nodes seems to be as well tolerated as the irradiation of the prostate alone.
Trial registration
Trial Numbers: ARO 2009–05, ClinicalTrials.gov: NCT01903408.
Similar content being viewed by others
Background
Percutaneous irradiation of locally advanced prostate cancer is the alternative therapy to radical prostatectomy (RP). A direct and valid comparison between radiation therapy (RT) and RP is not possible on the basis of existing studies due to the lack of prospective clinical trials [1–3]. When comparing retrospectively the clinical outcome of external beam radiotherapy (EBRT) with case series for RP, similar rates of the five-year (5y) biochemical progression free survival (bPFS) and the 5y- and 10y-disease-specific survival (DSS) were observed for EBRT, while the 10y-bPFS and the 10y-overall survival (OS) were slightly higher in favor of RP. However, this weak evidence does not allow a prioritization of one of the two treatments for locally advanced prostate cancer.
The addition of pelvic lymph nodes to the radiation field raised concerns regarding possible increased side effects. Acute gastrointestinal (GI) and genitourinary (GU) toxicities were more frequently reported in patients treated with WPRT [4, 5]. Late complications were also more frequently seen in the whole pelvis (WP)RT group compared to postoperative radiotherapy (PORT) [6–8]. IMRT can reduce acute and late toxicities using smaller irradiated volumes of bladder, small bowels and rectum [9, 10]. Moderately hypofractionated RT has become routine over the years due to area-wide implementation of image guided (IG)RT and better knowledge of tumor radiation biology [11–13]. Hence, in the present study we combined both, advanced IMRT/IGRT techniques for a better tolerability, and a moderate hypofractionated simultaneous integrated boost (SIB) to the prostate for a probably higher biological effectiveness.
The PLATIN (Prostate and Lymph Node Irradiation with Integrated-Boost-IMRT after NHT) phase II trial evaluates an optimized WPRT in patients with locally advanced prostate cancer. Due to image guided IMRT even inhomogeneous dose distributions can be applied accurately. Initiated in 2009, the study was designed to prospectively investigate safety and feasibility of five prostate and lymph node irradiation concepts, each enrolling n = 40 patients. Pelvic lymph nodes are simultaneously irradiated with an integrated boost to either the prostate (PLATIN 1), the prostate and macroscopic lymph nodes (PLATIN 2), the prostate bed (PLATIN 3), the prostate bed and macroscopic lymph nodes (PLATIN 4), or to macroscopic lymph nodes in patients with prior PBRT (PLATIN 5). Secondary objectives were a detailed characterization of the toxicity profiles, and the evaluation of quality of life during treatment. Results of the PLATIN 3 arm were published by Katayama et al. [14].
In this article we report on safety and efficacy data applying IMRT treatment of the pelvic lymph nodes with a SIB to the prostate (PLATIN 1).
Methods
From May 2009 to December 2012, 40 patients were enrolled prospectively in the PLATIN 1 trial. Eligibility criteria were, among others, a histological proven prostate carcinoma without lymph node metastases but with an estimated risk of lymph node involvement >20 % according to the Roach formula [15]. In case of a diagnostic lymphadenectomy, a minimum number of ten lymph nodes had to be surgically removed.
Before trial initiation, ethical consent was obtained from the ethics committee of the University of Heidelberg (permit S-034/2009). All patients gave written informed consent before trial enrollment. All reported data were conducted in accordance with the Helsinki Declaration and with national guidelines. Patients received at least 2 months of neoadjuvant AT (bicalutamide or LHRH analogue). With good tolerability AT was continued for at least 2 years after irradiation.
For treatment planning, CT scans with 3 mm slice thickness at full bladder and empty rectum were performed. PTV-P (planning target volume - prostate) covered the prostate (CTV-P) + 6 mm including the seminal vesicles. PTV-L (planning target volume - lymph nodes) included the obturatory, internal and external iliac, common iliac and presacral (down to S3) lymph nodes with a 5 mm margin [16]. Pararectal lymph nodes were not included in the PTV-L. Inverse treatment planning was performed using the Tomotherapy® treatment planning software (Accuray, USA). A total dose of 51.0 Gy was prescribed to 95 % of PTV-L with a SIB of 76.5 Gy to 95 % of PTV-P in 34 fractions. The dose prescription to the lymph nodes of 51 Gy in 1.5 Gy fractions is biologically equivalent to 43.7 Gy, assuming a α/β of 1.5 Gy for prostate cancer; and 48.2 Gy, assuming a α/β of 7 Gy for small bowel. Treatment was performed with full bladder and empty rectum under daily IGRT.
Prostate-specific symptoms and treatment toxicity, using the criteria of the NCI CTC AE version 3.0, were recorded before treatment, weekly during treatment, at the end of treatment, and at 2.5, 6, 12, 18 and 24 months follow-up. For calculation of toxicity rates, only patients with available data at the respective time points were considered. Cumulative GI toxicity was defined as the cumulative incidence of diarrhea, enteritis and proctitis. To facilitate comparison with other publications, only cystitis was included in the calculation of cumulative GU toxicity, as most scoring systems do not include incontinence and erectile dysfunction. Nevertheless, incontinence and erectile dysfunction were recorded.
Quality of life was assessed using the EORTC QLQ-C30 questionnaire before treatment and during follow-up after 6, 12 and 24 months.
PSA levels were measured before radiotherapy and then every 3 months afterwards, starting from week 10. Biochemical failure was established according to the Phoenix criteria [17].
A primary endpoint, the safe treatment application rate (STR) was chosen. STR was defined as the proportion of patients receiving treatment as planned and without grade 3–4 toxicity and calculated as the ratio of the number of patients fulfilling this criteria divided by the size of the Intention-to-treat (ITT) population. The ITT population consisted of all patients giving informed consent, fulfilling the inclusion and exclusion criteria and receiving planned treatment for a minimum of 4 weeks after initiation. Based on a one-stage phase II type design, STR of 80 % (null-hypothesis SDR ≤80 %) was tested against the alternative of being at least as large as 95 % in a one-stage phase-II type design using the exact binomial test at the significance level of 0.1 % with a power of 90 %. The null hypothesis would be rejected when SDR would be at least 87.7 %.
Results
Patient characteristics
Among all 40 patients (identical with the ITT population), median follow-up was 23.4 months (range: 2.8 – 31.7 months). Median age at inclusion was 70 years (range: 51 – 75 years); all patients were high-risk according to the D‘Amico risk categories [18]. One patient underwent laparoscopic resection of lymph nodes but rejected prostatectomy. Indication for WPRT was seen by reason of lymph node affection (pN+) without remaining macroscopic lymph node metastasis in situ. All other patients had an estimated risk of lymph node involvement >20 % according to the Roach formula. Both LHRH and antiandrogen therapy were permitted as antihormonal therapies.
Twenty-seven patients received LHRH analogue therapy, seven patients received bicalutamide and six patients both (complete androgen deprivation). Most of the patients still had antihormonal therapy prescribed by their urologist as they were seen in the Department of Radiooncology. Radiotherapy was performed as definitive treatment in 38 patients. Two patients had PSA elevation during NHT and were thus excluded from the study. One patient died 7 months after radiotherapy diagnosed with a metastasized esophageal cancer. For further patient characteristics see Table 1.
Treatment characteristics
Average beam on time of the 38 evaluated radiation plans was 477 ± 78 s. The intended target coverage could be met. 95 % of the PTV-P received 75 ± 2.5 Gy (median dose: 78.5 ± 0.5 Gy) and 95 % of the PTV-L received 50.7 ± 0.5 Gy (median dose: 53.8 ± 1.1 Gy).
Plan quality in terms of organ at risk sparing is shown in Table 2. The anterior rectal wall received a maximum dose of 72.8 ± 1.3 Gy. The rectum received doses ≥60 Gy (9.5 %) and ≥70 Gy (1.6 %). Dose to the small bowel could be kept low in the segmented parts with 9.4 % of the small bowel exposed to ≥40 Gy and a maximum dose of 52.7 Gy. Most of the bladder could be spared from high dose exposure with 6.3 % of the bladder receiving ≥70 Gy.
Treatment safety
After a median observation time of 23.4 months one patient out of 38 died seven months after irradiation suffering from metastasized esophageal cancer. No patient showed acute toxicity ≥grade 3. We defined acute toxicity as side effects within 6 months after therapy. Therefore, at the time of evaluation the PLATIN 1 trial met the prospectively defined statistical criteria of a successful treatment with an SDR of at least 87.7 %.
Gastrointestinal toxicity
Cumulative incidence of acute GI toxicity was 56.8 % (grade 1) and 21.6 % (grade 2). No acute grade 3 or 4 GI toxicity occurred. During treatment, patients suffered from diarrhea in 18.9 % (grade 1) and 2.7 % (grade 2). Proctitis was reported in 13.5 % (grade 1) and 5.4 % (grade 2) of all cases. Enteritis grade 1 occurred in 15.4 % and grade 2 in 2.7 %.
Cumulative late GI toxicity was 6.1 % (grade 1). No patient suffered from late enteritis of any grade. Only one patient experienced late proctitis grade 1 at 12 months of follow-up, and one late diarrhea grade 1 at 18 months was observed (see Table 3).
Genitourinary toxicity
The incidence of acute GU toxicity is comparable to other published data with 78.4 % (grade 1) and 48.6 % (grade 2). Cumulative incidence of late GU toxicity was 12.3 % (grade 1) and 6.4 % (grade 2). No patient developed acute or late GU toxicity grade 3/4.
Acute cystitis was reported in 35.1 % (grade 1) and 18.9 % (grade 2) of all patients (see Table 4). Two patients reported stress incontinence grade 1 (occasional, no pads necessary) at the beginning of radiation therapy, which regressed about 12 months thereafter. Four other patients reported on stress incontinence grade 1 in one follow-up. In all cases, the symptoms resolved until the following visit.
One patient required urinary catheterization (for 8 days) during follow-up (6 days after the end of radiotherapy) due to urinary retention. As no other intervention was required, it was rated as grade 2 toxicity. For all other patients the urinary flow has hardly changed during and after therapy. At 24 months of follow-up, all patients were catheter-free.
Urge incontinence increased after treatment within the first 6 months from 8.1 to 20.5 % (grade 1) and from 2.7 to 2.9 % (grade 2). At 24 months, urge incontinence decreased to 7.4 % (grade 1) and 0 % (grade 2).
Within the study, we also evaluated the incidence of adverse effects on libido and erectile dysfunction. However, since hormonal therapy is running within the first 2 years, toxicity analysis is reasonable only after discontinuation of AHT.
Quality of life
Overall health as assessed by the “Global Health Score” of the EORTC QLQ-C30 questionnaire remained almost unchanged at 6, 12 and 24 months follow-up compared to baseline (see Table 5). Scores were on a similar level as the EORTC reference value of prostate cancer patients over all disease stages.
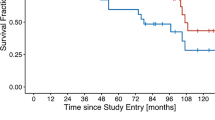
Biochemical control and survival
During follow-up, three patients experienced PSA recurrences. All three had discontinued AT after radiotherapy resulting in an actuarial biochemical progression free survival of 91.9 % after 2 years (see Fig. 1a). In one patient, PSA recurrence coincided with the diagnosis of bone metastases; for the other two patients, the localization of recurrence could not be determined. Ten patients quit AT after completion of radiotherapy due to reported intolerance and side effects. At the time of analysis, 15 patients still received AT. Average duration of AT was 13.6 months for the 38 patients remaining in the trial after the end of radiotherapy. At a median of 24 months follow-up, 37 patients were alive resulting in an actuarial overall survival (OS) of 97.3 % (see Fig. 1b).
Discussion
The procedure of EBRT for prostate cancer has undergone many changes in the past decade. Recently, dose escalation, hypofractionation and the use of IMRT and IGRT became a standard method. Hence, outcome data are slowly emerging. The necessity of prophylactic radiotherapy of the pelvic lymph nodes remains controversial. Many radiation oncology centers electively treat the pelvic lymph nodes because of publications on surgical lymph node sampling and nanoparticle-enhanced MRI studies that revealed a high proportion of occult lymph node metastases [19, 20]. In contrast, other centers avoid WPRT because of concerns about excessive toxicity. For more clarity, the effect of WPRT was tested in large prospective trials. Unfortunately, the long-term PFS showed no significant differences between WPRT and PORT [21–23]. However, these trials were designed before the dose-escalation era [6, 7, 24, 25]. With a dose-escalation up to 75.6 Gy to the prostate, Aizer et al. could prove the superiority of WPRT [8]. Especially in high-risk situations a benefit with reduced rates of failure were seen in patients treated with doses higher than 75 Gy [26, 27].
The present phase II study shows good tolerability of IMRT-based treatment of the prostate and pelvic lymph nodes. We revealed a reduced incidence of toxicities compared to conventionally fractionated schemes. The RTOG 94–13 trial showed late grade ≥3 GI and GU toxicities at 5 years of 3.0 and 4.3 %, respectively, using conventionally fractionation of 1.8 Gy (50.4 Gy WPRT + 19.8 Gy boost to the prostate bed). The GETUG-01 trial applied doses to the prostate and whole pelvis of 66 – 72 Gy à 1.8 – 2.25 Gy and 45–46.8 Gy à 1.8 Gy. Here, 37.7 % of patients developed late grade ≥2 GU toxicity and 31.7 % developed late grade ≥2 GI toxicity. In our trial, the observed rates of late toxicity compare favorably to the mentioned studies with no grade ≥2 GI toxicity, and 6.4 % grade 2 and no grade 3 or 4 GU toxicity. On the one hand, the lower rates of side effects could be attributed to the modern IMRT/IGRT technique; on the other hand, the moderate hypofractionation could have an important impact: the α/β ratio of prostate cancer is supposed to be lower than the surrounding healthy tissue of rectum and bladder resulting in a probably lower rate of late side effects.
In our trial, patients received at least 2 months of neoadjuvant AT. With good tolerability AT was continued for at least 2 years after irradiation. The addition of antihormonal treatment (AT) in patients with clinically localized intermediate or high-risk prostate cancer showed superior results (bPFS, DSS, OS) in a number of prospective randomized trials [28–31]. The question of the right timing of adjuvant hormonal treatment (AHT) is still under debate and lasts from 4 months in the RTOG 86–10 trial to 3 years in the EORTC trial [32–35]. Bolla et al. demonstrated a significantly lower overall mortality in patients under neoadjuvant hormonal treatment (NHT) plus 3 years AHT compared to 6 months AHT [36]. Most randomized phase III trials used short-term NHT in combination with EBRT and showed an improvement either in absence of PSA failure or OS [33, 37, 38]. One of the possible effects of NHT is the immune modulation of AT resulting in T-cell infiltration of the prostate, which can increase apoptosis [39]. Most studies using long-term AHT for high-risk patients added whole pelvis radiotherapy (WPRT) [30, 32, 40]. The RTOG 92–02 trial proved that NHT combined with long-term AHT is superior to NHT for locally advanced/high-risk patients [40]. While it is still unclear whether an additional WPRT is beneficial compared to prostate irradiation alone [21, 22, 41, 42], the mentioned studies also showed no significant improvement of relevant clinical endpoints (OS, bPFS, DSS). The RTOG 94–13 trial planned to evaluate the timing of AT. The role of WPRT became rather complex as the authors found an interaction between field size and timing of AT. No benefit could be found in the trial testing WPRT vs. prostate only RT (PORT) in combination with AHT vs. NHT [21]. However, the results suggest that if a patient chooses NHT, WPRT appears beneficial compared to PORT. The risk of high-grade (> grade 3) GI toxicity is potentially higher under additional WPRT and AT compared to PORT.
The evaluation of erectile function and libido based on patient-reported data is prone to reporting bias. Nevertheless, we documented the incidence of adverse effects on libido and erectile dysfunction as well. At this stage evaluation is too early, as for most patients AT is still running within the first 2 years of follow-up. Toxicity analysis is only reasonable if AT is completed.
Our study has shown both safety and efficacy using helical tomotherapy. At the point of analysis, 34 of 37 patients were free from PSA recurrence. However, it is important to note the limitations of our first analysis. The patient number is relatively small. For a reliable evaluation of efficacy, a median follow-up of 23.4 months is rather short. A longer follow-up period is needed to detect differences especially in late toxicity. Also, it will provide more significant reports on biochemical control.
Conclusion
While the role of WPRT of prostate cancer remains to be fully explored, we could demonstrate in the prospective PLATIN 1 trial that prophylactic radiotherapy of the pelvic lymph nodes with a SIB to the prostate can be performed without excessive toxicity. The combined irradiation of both prostate and pelvic lymph nodes seems to be as well tolerated as the irradiation of the prostate alone.
References
Akakura K, Suzuki H, Ichikawa T, Fujimoto H, Maeda O, Usami M, et al. A randomized trial comparing radical prostatectomy plus endocrine therapy versus external beam radiotherapy plus endocrine therapy for locally advanced prostate cancer: results at median follow-up of 102 months. Jpn J Clin Oncol. 2006;36(12):789–93.
Edamura K, Saika T, Senoh T, Koizumi F, Manabe D, Ebara S, et al. Long-term clinical outcomes of 420 consecutive prostate cancer patients in a single institute. Acta Med Okayama. 2005;59(5):195–9.
Saito T, Kitamura Y, Komatsubara S, Matsumoto Y, Sugita T, Hara N. Outcomes of locally advanced prostate cancer: a single institution study of 209 patients in Japan. Asian J Androl. 2006;8(5):555–61.
Mameghan H, Fisher R, Mameghan J, Watt WH, Tynan A. Bowel complications after radiotherapy for carcinoma of the prostate: the volume effect. Int J Radiat Oncol Biol Phys. 1990;18(2):315–20.
Perez CA, Lee HK, Georgiou A, Lockett MA. Technical factors affecting morbidity in definitive irradiation for localized carcinoma of the prostate. Int J Radiat Oncol Biol Phys. 1994;28(4):811–9.
Hanks GE, Hanlon AL, Epstein B, Horwitz EM. Dose response in prostate cancer with 8–12 years’ follow-up. Int J Radiat Oncol Biol Phys. 2002;54(2):427–35.
Zelefsky MJ, Leibel SA, Gaudin PB, Kutcher GJ, Fleshner NE, Venkatramen ES, et al. Dose escalation with three-dimensional conformal radiation therapy affects the outcome in prostate cancer. Int J Radiat Oncol Biol Phys. 1998;41(3):491–500.
Aizer AA, Yu JB, McKeon AM, Decker RH, Colberg JW, Peschel RE. Whole pelvic radiotherapy versus prostate only radiotherapy in the management of locally advanced or aggressive prostate adenocarcinoma. Int J Radiat Oncol Biol Phys. 2009;75(5):1344–9.
Ashman JB, Zelefsky MJ, Hunt MS, Leibel SA, Fuks Z. Whole pelvic radiotherapy for prostate cancer using 3D conformal and intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2005;63(3):765–71.
Jani AB, Su A, Milano MT. Intensity-modulated versus conventional pelvic radiotherapy for prostate cancer: analysis of acute toxicity. Urology. 2006;67(1):147–51.
Kupelian PA, Willoughby TR, Reddy CA, Klein EA, Mahadevan A. Hypofractionated intensity-modulated radiotherapy (70 Gy at 2.5 Gy per fraction) for localized prostate cancer: Cleveland Clinic experience. Int J Radiat Oncol Biol Phys. 2007;68(5):1424–30.
Guckenberger M, Lawrenz I, Flentje M. Moderately hypofractionated radiotherapy for localized prostate cancer: long-term outcome using IMRT and volumetric IGRT. Strahlenther Onkol. 2014;190(1):48–53.
Thomson D, Merrick S, Swindell R, Coote J, Kelly K, Stratford J, et al. Dose-escalated hypofractionated intensity-modulated radiotherapy in high-risk carcinoma of the prostate: outcome and late toxicity. Prostate Cancer. 2012;2012:450246.
Katayama S, Habl G, Kessel K, Edler L, Debus J, Herfarth K, et al. Helical intensity-modulated radiotherapy of the pelvic lymph nodes with integrated boost to the prostate bed - initial results of the PLATIN 3 Trial. BMC Cancer. 2014;14:20.
Roach 3rd M, Marquez C, Yuo HS, Narayan P, Coleman L, Nseyo UO, et al. Predicting the risk of lymph node involvement using the pre-treatment prostate specific antigen and Gleason score in men with clinically localized prostate cancer. Int J Radiat Oncol Biol Phys. 1994;28(1):33–7.
Lawton CA, Michalski J, El-Naqa I, Buyyounouski MK, Lee WR, Menard C, et al. RTOG GU radiation oncology specialists reach consensus on pelvic lymph node volumes for high-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2009;74(2):383–7.
Horwitz EM, Thames HD, Kuban DA, Levy LB, Kupelian PA, Martinez AA, et al. Definitions of biochemical failure that best predict clinical failure in patients with prostate cancer treated with external beam radiation alone: a multi-institutional pooled analysis. J Urol. 2005;173(3):797–802.
D’Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280(11):969–74.
Partin AW, Kattan MW, Subong EN, Walsh PC, Wojno KJ, Oesterling JE, et al. Combination of prostate-specific antigen, clinical stage, and Gleason score to predict pathological stage of localized prostate cancer. A multi-institutional update. JAMA. 1997;277(18):1445–51.
Ross RW, Zietman AL, Xie W, Coen JJ, Dahl DM, Shipley WU, et al. Lymphotropic nanoparticle-enhanced magnetic resonance imaging (LNMRI) identifies occult lymph node metastases in prostate cancer patients prior to salvage radiation therapy. Clin Imaging. 2009;33(4):301–5.
Lawton CA, DeSilvio M, Roach 3rd M, Uhl V, Kirsch R, Seider M, et al. An update of the phase III trial comparing whole pelvic to prostate only radiotherapy and neoadjuvant to adjuvant total androgen suppression: updated analysis of RTOG 94–13, with emphasis on unexpected hormone/radiation interactions. Int J Radiat Oncol Biol Phys. 2007;69(3):646–55.
Pommier P, Chabaud S, Lagrange JL, Richaud P, Lesaunier F, Le Prise E, et al. Is there a role for pelvic irradiation in localized prostate adenocarcinoma? Preliminary results of GETUG-01. J Clin Oncol. 2007;25(34):5366–73.
Roach 3rd M, DeSilvio M, Lawton C, Uhl V, Machtay M, Seider MJ, et al. Phase III trial comparing whole-pelvic versus prostate-only radiotherapy and neoadjuvant versus adjuvant combined androgen suppression: Radiation Therapy Oncology Group 9413. J Clin Oncol. 2003;21(10):1904–11.
Pollack A, Zagars GK, Smith LG, Lee JJ, von Eschenbach AC, Antolak JA, et al. Preliminary results of a randomized radiotherapy dose-escalation study comparing 70 Gy with 78 Gy for prostate cancer. J Clin Oncol. 2000;18(23):3904–11.
Valicenti R, Lu J, Pilepich M, Asbell S, Grignon D. Survival advantage from higher-dose radiation therapy for clinically localized prostate cancer treated on the Radiation Therapy Oncology Group trials. J Clin Oncol. 2000;18(14):2740–6.
Peeters ST, Heemsbergen WD, Koper PC, van Putten WL, Slot A, Dielwart MF, et al. Dose–response in radiotherapy for localized prostate cancer: results of the Dutch multicenter randomized phase III trial comparing 68 Gy of radiotherapy with 78 Gy. J Clin Oncol. 2006;24(13):1990–6.
Jacob R, Hanlon AL, Horwitz EM, Movsas B, Uzzo RG, Pollack A. The relationship of increasing radiotherapy dose to reduced distant metastases and mortality in men with prostate cancer. Cancer. 2004;100(3):538–43.
Granfors T, Modig H, Damber JE, Tomic R. Long-term followup of a randomized study of locally advanced prostate cancer treated with combined orchiectomy and external radiotherapy versus radiotherapy alone. J Urol. 2006;176(2):544–7.
Roach 3rd M, Bae K, Speight J, Wolkov HB, Rubin P, Lee RJ, et al. Short-term neoadjuvant androgen deprivation therapy and external-beam radiotherapy for locally advanced prostate cancer: long-term results of RTOG 8610. J Clin Oncol. 2008;26(4):585–91.
Bolla M, Collette L, Blank L, Warde P, Dubois JB, Mirimanoff RO, et al. Long-term results with immediate androgen suppression and external irradiation in patients with locally advanced prostate cancer (an EORTC study): a phase III randomised trial. Lancet. 2002;360(9327):103–6.
Bolla M, Van Tienhoven G, Warde P, Dubois JB, Mirimanoff RO, Storme G, et al. External irradiation with or without long-term androgen suppression for prostate cancer with high metastatic risk: 10-year results of an EORTC randomised study. Lancet Oncol. 2010;11(11):1066–73.
Pilepich MV, Winter K, Lawton CA, Krisch RE, Wolkov HB, Movsas B, et al. Androgen suppression adjuvant to definitive radiotherapy in prostate carcinoma—long-term results of phase III RTOG 85–31. Int J Radiat Oncol Biol Phys. 2005;61(5):1285–90.
Pilepich MV, Winter K, John MJ, Mesic JB, Sause W, Rubin P, et al. Phase III radiation therapy oncology group (RTOG) trial 86–10 of androgen deprivation adjuvant to definitive radiotherapy in locally advanced carcinoma of the prostate. Int J Radiat Oncol Biol Phys. 2001;50(5):1243–52.
Lawton CA, Winter K, Grignon D, Pilepich MV. Androgen suppression plus radiation versus radiation alone for patients with stage D1/pathologic node-positive adenocarcinoma of the prostate: updated results based on national prospective randomized trial Radiation Therapy Oncology Group 85–31. J Clin Oncol. 2005;23(4):800–7.
Tyrrell CJ, Payne H, See WA, McLeod DG, Wirth MP, Iversen P, et al. Bicalutamide (‘Casodex’) 150 mg as adjuvant to radiotherapy in patients with localised or locally advanced prostate cancer: results from the randomised Early Prostate Cancer Programme. Radiother Oncol. 2005;76(1):4–10.
Bolla M, de Reijke TM, Van Tienhoven G, Van den Bergh AC, Oddens J, Poortmans PM, et al. Duration of androgen suppression in the treatment of prostate cancer. N Engl J Med. 2009;360(24):2516–27.
Christie D, Denham J, Steigler A, Lamb D, Turner S, Mameghan H, et al. Delayed rectal and urinary symptomatology in patients treated for prostate cancer by radiotherapy with or without short term neo-adjuvant androgen deprivation. Radiother Oncol. 2005;77(2):117–25.
D’Amico AV, Loffredo M, Renshaw AA, Loffredo B, Chen MH. Six-month androgen suppression plus radiation therapy compared with radiation therapy alone for men with prostate cancer and a rapidly increasing pretreatment prostate-specific antigen level. J Clin Oncol. 2006;24(25):4190–5.
Mercader M, Bodner BK, Moser MT, Kwon PS, Park ES, Manecke RG, et al. T cell infiltration of the prostate induced by androgen withdrawal in patients with prostate cancer. Proc Natl Acad Sci U S A. 2001;98(25):14565–70.
Hanks GE, Pajak TF, Porter A, Grignon D, Brereton H, Venkatesan V, et al. Phase III trial of long-term adjuvant androgen deprivation after neoadjuvant hormonal cytoreduction and radiotherapy in locally advanced carcinoma of the prostate: the Radiation Therapy Oncology Group Protocol 92–02. J Clin Oncol. 2003;21(21):3972–8.
Pilepich MV, Krall JM, Johnson RJ, Sause WT, Perez CA, Zinninger M, et al. Extended field (periaortic) irradiation in carcinoma of the prostate--analysis of RTOG 75–06. Int J Radiat Oncol Biol Phys. 1986;12(3):345–51.
Asbell SO, Martz KL, Shin KH, Sause WT, Doggett RL, Perez CA, et al. Impact of surgical staging in evaluating the radiotherapeutic outcome in RTOG #77-06, a phase III study for T1BN0M0 (A2) and T2N0M0 (B) prostate carcinoma. Int J Radiat Oncol Biol Phys. 1998;40(4):769–82.
Acknowledgements
The PLATIN trial is supported by the Klaus Tschira Foundation (project number 00.153.2009). The PLATIN trial is conducted in collaboration with the ARO (Trial Number: 2009–5). We cordially thank Renate Haselmann and Alexandros Gioules for her thorough work.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interest
The Department of Radiation Oncology, University Hospital Heidelberg, has a research collaboration with Accuray Inc., who is the manufacturer of Tomotherapy® machines and software.
Authors’ contributions
GH performed patient treatment and follow up and data acquisition and drafted the manuscript. SK and MU performed treatment and follow up. KK was responsible for data management. LE planned the trial statistics. JD revised the manuscript. KH was the principal investigator and revised the trial protocol and the manuscript. FS designed the trial protocol, was responsible for patient treatment and follow up and revised the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Habl, G., Katayama, S., Uhl, M. et al. Helical intensity-modulated radiotherapy of the pelvic lymph nodes with a simultaneous integrated boost to the prostate - first results of the PLATIN 1 trial. BMC Cancer 15, 868 (2015). https://doi.org/10.1186/s12885-015-1886-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-015-1886-5