Abstract
Background
Previous studies have examined that a range of optimal serum P level during the implantation period was associated with optimal live birth rates. However, those results obtained with vaginal or intramuscular route of progesterone administration for luteal phase support (LPS) alone. Is there a relationship between the serum progesterone (P) on the day of frozen-thawed embryo transfer (FET) with the likelihood of a live birth (LB) in artificial cycles (AC) when using a combination of oral dydrogesterone and vaginal progesterone for LPS?
Methods
This was a retrospective study of 3659 FET cycles with artificial endometrial preparation in a Chinese tertiary-care academic medical centre from January 2015 to February 2017. Endometrial preparation was performed using estradiol (E2) valerate (Fematon-red tablets) 8 mg/d beginning on day 3 of the cycle, followed by administration of P both orally (8 mg/d Fematon-yellow tablets) and vaginally (400 mg/d; Utrogestan). The primary endpoint was live birth rate (LBR). The association between the serum P level on the embryo transfer day and pregnancy outcomes was evaluated by univariable and multivariable logistic regression analysis.
Results
The LBRs according to the serum P quartiles were as follows: Q1: 35.7%; Q2: 37.4%; Q3: 39.1% and Q4: 38.9%. Logistic regression analysis showed that the odds of a LB were not significantly different between the low (P < 7.9 ng/mL) and high (P ≥ 7.9 ng/mL) progesterone groups before or after adjustment (crude OR = 0.89, 95% CI: 0.76–1.04; adjusted OR = 0.89, 95% CI: 0.75–1.04).
Conclusion
The present study suggests that the serum P levels on the day of embryo transfer (ET) do not correlate with the likelihood of a LB in artificial cycles when using a combination of oral dydrogesterone and vaginal progesterone for luteal phase support.
Similar content being viewed by others
Background
Since the first live birth by frozen-thawed embryo transfer (FET) in 1983, embryonic cryopreservation and FET procedures have progressively advanced and become essential tools in the treatment of infertility [1, 2]. Elective embryo cryopreservation was mainly developed to prevent ovarian hyperstimulation syndrome in women who were at risk [2,3,4], but its use has been extended to cycles with preimplantation diagnoses and embryo-endometrial asynchrony [5, 6]. FET is performed using different cycle regimens: spontaneous ovulatory (natural) cycles; cycles in which the endometrium is artificially prepared with oestrogen and progesterone hormones, commonly known as hormonally substituted artificial cycles (AC); and cycles in which ovulation is induced by drugs (ovulation induction FET cycles) [7]. However, the most effective method to prepare the endometrium prior to FET is still a matter of debate. Hormonally substituted AC-FET is commonly used, requires less monitoring than other FET protocols and thus offers flexibility in terms of the timing of the thaw and transfer of the embryo [8].
The importance of progesterone in the establishment and maintenance of pregnancy has been proven by interventional studies in early pregnancy, which showed that progesterone deficiency caused by a lutectomy or by blocking the actions of progesterone (using a progesterone antagonist) lead to pregnancy loss [9, 10]. In AC-FET, administration of oestrogen and progesterone is necessary due to the lack of a corpus luteum and endogenous sex steroid production [8].
Multiple routes of P administration are available. Over the last few decades, vaginal and intramuscular routes have been preferentially used, whereas oral P has been generally avoided due to poor bioavailability and inferior assisted reproductive technology (ART) outcomes [11,12,13]. Surveys have indicated that when given the choice, most patients prefer vaginal over intramuscular P administration for a variety of reasons, including greater convenience, ease of use, and less pain [14, 15]. Dydrogesterone is a synthetic progestin with enhanced oral bioavailability that is highly selective for the progesterone receptor [16, 17]. Furthermore, data from prospective trials for luteal phase support in IVF show that oral dydrogesterone is as effective as micronized vaginal progesterone (MVP), is well tolerated overall, and has a higher patient satisfaction rate than MVP [16, 18].
Recently, it has been reported that a range of serum progesterone concentrations during the implantation period is associated with an optimal live birth rate [19,20,21,22,23,24,25]. Although these results are controversial, they suggest an optimal serum P threshold for the LBR of artificial cycles when using intravaginal or intramuscular progesterone; however, different cut-off levels have been suggested. Our in vitro fertilization (IVF) centre applies a combination of oral dydrogesterone and vaginal progesterone for LPS in AC-FET. We are interested in determining whether the findings are consistent under the combination of oral dydrogesterone and vaginal progesterone administration. Given this background, the present study aimed to examine whether serum P levels on the day of ET are related to the live birth rate for artificial cycles when using a combination of oral dydrogesterone and vaginal progesterone for LPS.
Methods
Study design and patients
This retrospective cohort study was conducted at the Department of Assisted Reproduction of the Ninth People’s Hospital of Shanghai Jiao Tong University School of Medicine (Shanghai, China) from January 2017 to February 2019. It was approved by the Ethics Committee (Institutional Review Board) of the Ninth People’s Hospital of Shanghai. All participants provided informed consent after counselling for infertility treatments and routine IVF procedures. All patients underwent artificial endometrial preparation with a combination of oral dydrogesterone and vaginal progesterone for LPS only. Inclusion criteria were as follows: 19 < age < 50 years; BMI < 30 kg/m2; and no systemic diseases. Due to the potential bias from recurrent implantation failure (the failure of clinical pregnancy after 4 good quality embryo transfers, with at least three fresh or frozen IVF cycles in women under the age of 40) [26], analysis was limited only to patients undergoing their first or second FET cycles. The exclusion criteria were recurrent miscarriages (the loss of three or more consecutive pregnancies (< 28 weeks of gestation), infertility due to severe male factors (e.g., oligozoospermia, cryptozoospermia and azoospermia), uterine diseases (e.g., fibroids, polyps, and previously diagnosed Müllerian abnormalities) or the presence of hydrosalpinx, women whose triple-line endometrium of < 7 mm thickness after as many days as 21 E2 administration. Likewise, records with missing data were excluded. Therefore, a final cohort of 3659 cycles was analysed.
Protocol of endometrial preparation and embryo transfer
Details on endometrial preparation procedures have been described in our previous study [27]. Endometrial preparation was induced with sequential provision of oral E2 (Fematon-red tablets, Abbott Biological, USA) 8 mg/d from cycle day 3 onwards. After 12–14 days of oestrogen therapy, a blood sample was collected, and a vaginal ultrasound were performed for measurements of oestradiol, LH, and progesterone levels and endometrial thickness, respectively. If the endometrial thickness was < 7 mm, oestrogen therapy was extended for as long as 7 days if required. If a triple-line endometrium of ≥ 7 mm thickness was observed with serum progesterone concentrations < 1.0 ng/ml, P was administered both orally (40 mg dydrogesterone and 8 mg E twice per day; Fematon-yellow tablets, Abbott Biologicals, USA) and vaginally (400 mg/d; Utrogestan, Besins Manufacturing, Belgium). If a triple-line endometrium of ≥ 7 mm thickness was observed with serum progesterone concentrations ≥ 1.0 ng/ml, the FET cycle should be cancelled due to premature ovulation. The time of thaw and transfer was set as the 3rd or 5th day after P administration depending on the embryo stage. The maximum number of embryos transferred was two per patient in each FET cycle. Given the absence of corpora lutea, exogenous P4 administration was continued until 10-week gestation. A blood sample was obtained between 7 and 8 am on the day of frozen-thawed embryo transfer for serum oestradiol and progesterone measurements. Embryos were generated from either IVF or intracytoplasmic sperm injection cycles and were vitrified and warmed as previously described [28, 29] on day 3 or at the blastocyst stage. In brief, the Cummins criteria and the Gardner and Schoolcraft grade system were used to grade D3 embryos and blastocysts respectively [30, 31]. We defined top-quality embryo as grade I 7–10 cells on Day 3 and grade 4BB or higher on Day 5/6. All embryo transfers were performed under ultrasound guidance. The number of transferred embryos and the stage of the embryo were recorded. A human chorionic gonadotrophin (HCG) test was measured 12 or 14 days after embryo transfer and ultrasound examination was routinely performed 28 days after embryo transfer.
Serum hormonal assays
Hormone levels were measured by chemiluminescence (Abbott Biologicals B.V.). Intra- and inter-assay coefficients of variation were 7.9 and 10% for P. The synthetic progestogens used (dydrogesterone) did not have any cross-reaction with the progesterone assay.
Outcome measures
The primary endpoint was the relationship between progesterone levels on the embryo transfer day and the live birth rate per cycle. Secondary endpoints included the implantation rate, positive β-HCG test rate, clinical pregnancy rate, ongoing pregnancy rate at 12 weeks of gestation and early miscarriage (first-trimester pregnancy loss) rate. A human chorionic gonadotrophin (hCG) test was considered positive if HCG was > 10 IU/l. The clinical pregnancy rate (CPR) was defined as the proportion of patients diagnosed by ultrasonographic visualization of one or more gestational sacs or definitive clinical signs of pregnancyafter ET among all transfer cycles. The implantation rate was defined as the number of gestational sacs divided by the number of embryos transferred. The early miscarriage rate was defined as the proportion of patients with spontaneous pregnancy termination before the gestational age of 12 weeks. The ongoing pregnancy rate (OPR) was defined as the proportion of patients with a gestational sac with foetal heart activity assessed by ultrasound examination at 12 weeks of gestation among all transfer cycles.
The live birth rate (LBR) was defined as the proportion of the number of deliveries that resulted in at least one live birth among all transfer cycles. The main neonatal outcomes of the study included preterm birth (PTB), low birthweight (LBW), and major congenital malformations. PTB was defined as a birth takes place after 22 weeks and before 37 completed weeks of gestation. LBW was defined as a birthweight below 2500 g [32, 33]. Major congenital malformations were defined and coded according to the Q codes (Q00–Q99) of the International Classification of Diseases, 10th Revision (ICD-10) [34].
Statistical analysis
Serum P on the day of ET was classified into four quartiles according to the 25th, 50th and 75th percentiles. Continuous variables were presented as the mean plus/minus standard deviation, and the Kruskal-Wallis test was used to compare continuous variables. Categorical variables were described as the frequency with the rate, and between-group differences were assessed by chi-square test or Fisher’s exact test, as appropriate. The association between serum P on the day of ET and pregnancy outcome was evaluated by univariable and multivariable logistic regression analysis. All potential confounders were introduced into the regression equation for adjustment by the entry method, whether significant differences between groups were observed. These included maternal age (continuous), maternal BMI (continuous), duration of infertility (continuous), type of infertility (primary, secondary), infertility diagnosis (tubal factor, male factor, ovulatory, endometriosis, unexplained or combined), ovarian stimulation protocol (GnRH-a short, mild stimulation or progestin-primed ovarian stimulation (PPOS)), fertilization method (IVF, ICSI or IVF + ICSI), duration of estrogen use (continuous), endometrial thickness (continuous), progesterone level on embryo transfer day, number of embryos transferred (single or double), embryo stage at transfer (cleavage or blastocyst), transfer of ≥ 1 top-quality embryos and duration of embryo cryopreservation (continuous).
All P values were based on two-sided tests, and P < 0.05 was considered statistically significant. Statistical analysis was performed with the Statistical Package for the Social Sciences (version 20.0; SPSS Inc., USA).
Results
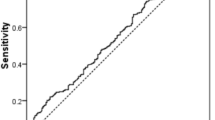
A total of 3659 cycles were analysed in terms of demographic characteristics and reproductive outcomes. Serum P on the day of ET was 10.30 ± 3.88 ng/ml. Supplementary Fig. 1 shows the 5th, 10th, 25th, 50th, 75th, 90th and 95th percentile values. The serum P intervals for each quartile were as follows: Q1, < 7.9 ng/ml; Q2, 7.9–9.6 ng/ml; Q3, 9.7–12 ng/ml; and Q4, ≥ 12.1 ng/ml. The baseline characteristics according to the serum P level on the day of ET are shown in Table 1. The four groups differed significantly in terms of the proportions for ovarian stimulation protocol (P < 0.001), endometrial thickness (P = 0.002) and embryo stage at transfer (P = 0.01). No significant differences were found when maternal age, BMI, duration of infertility, infertility diagnosis, fertilization method, number of embryos transferred or duration of embryo cryopreservation were analysed. The mean serum P values on the day of ET were 6.3 ± 1.4, 8.8 ± 0.5, 10.8 ± 0.7 and 15.3 ± 3.8 ng/ml in the Q1, Q2, Q3 and Q4 groups, respectively (P < 0.001).The patients with serum P levels on the day of ET that were < 7.9 ng/ml (Q1) had a significantly lower positive β-HCG test rate before or after adjustment relative to the high progesterone group (Q2-Q4) ((429/905,47.4%) versus (1461/2754,53.0%) (P = 0.003); adjusted OR = 0.79, 95% CI: 0.67–0.92, P = 0.003). The low progesterone group (Q1) also had a significantly lower CPR and OPR than the other patients (Q2–Q4): (393/905,43.4%) versus (1310/2754,47.6%) (P = 0.03); (333/905,36.8%) versus (1115/2754,40.5%) (P = 0.049). However, the odds of OPR between the two groups did not show a significant difference after adjustment (adjusted OR = 0.85, 95% CI: 0.72-1.00). In addition, for women in the low progesterone group (Q1), the odds of a LB did not show a significant difference before or after adjustment relative to the high progesterone group (Q2-Q4) (crude odds ratio [OR] = 0.89, 95% confidence interval [CI]: 0.76–1.04; adjusted OR = 0.89, 95% CI: 0.75–1.04). Furthermore, there was no statistically significant difference in the adjusted odds of early miscarriage between the low and high progesterone groups (Table 2; Fig. 1).
In the multivariable analysis, the factors significantly associated with live birth rate were maternal age (adjusted OR = 0.91, 95% CI: 0.90–0.93, P < 0.001), maternal BMI (adjusted OR = 0.98, 95% CI: 0.95-1.00, P = 0.045), infertility diagnosis for males (adjusted OR = 1.40, 95% CI: 1.07–1.82, P = 0.014), duration of estrogen use (adjusted OR = 0.96, 95% CI: 0.94–0.99, P = 0.002), endometrial thickness (adjusted OR = 1.07, 95% CI: 1.02–1.11, P = 0.002), number of embryos transferred (adjusted OR = 2.01, 95% CI: 1.65–2.44, P < 0.001), and embryo stage at transfer (adjusted OR = 1.54, 95% CI: 1.21–1.97, P = 0.001) (Table 3).
Table 4 demonstrates the neonatal outcomes grouped by the serum P level on the day of ET. We did not find statistically significant differences in the neonatal outcomes, such as PTB, LBW, major congenital malformations and early neonatal death, across the serum P quartiles for either singletons or twins.
Discussion
The results of the present study showed that there was no association between serum P levels on the day of ET and the live birth rate in artificial cycles when using a combination of oral dydrogesterone and vaginal progesterone for LPS. After adjusting for all potential confounders, the relationship between serum P on the day of ET and the likelihood of a live birth was not present.
The importance of luteal P for the establishment and maintenance of pregnancy is undebatable, and it is well accepted that the success of frozen embryo transfer is crucially dependent on sufficient luteal phase support [35]. However, the optimal luteal P level following frozen embryo transfer is poorly understood and has not been consistent until now. There have been conflicting results when using intramuscular P. A recent study by Brady et al. indicated that P values lower than 20 ng/ml on the day of embryo transfer are associated with lower live birth and clinical pregnancy rates in donor recipient cycles [19]. Conversely, Kofinas et al. reported that P levels > 20 ng/ml on the day of transfer (during frozen single euploid embryo transfer cycles) were associated with a decreased OPR/LBR [23]. When using intravaginal P, different cut-off levels have been suggested. In a previous study [20], the optimal progesterone range needed to achieve a live birth was found to be 22-31ng/ml, while values outside this range were significantly related to lower pregnancy rates. Furthermore, two very recent studies found that there is an optimal serum P value around the time of ET (≥ 10 ng/ml) and on the day of the pregnancy test (≥ 11ng/ml) [21, 24]. In line with the above two studies, one study [22] showed that patients with serum P < 9.2 ng/ml on the day of ET after an artificial endometrial preparation cycle with vaginal micronized P had a significantly reduced OPR, which was observed in the oocyte donation cycle context. In the abovementioned studies using intravaginal P, although there are variations in the optimal serum P level, these results suggest that a minimal threshold of serum P on the day of ET needs to be reached.
Our endometrial preparation protocol is quite different in that it combines oral dydrogesterone and vaginal progesterone. Although 40 mg of dydrogesterone daily seems to be an enough dose for covering the needing of LPS in artificial cycles, it is not properly defined so far. That is why we are still combining the vaginal route. It is widely used in most IVF units in China [36, 37]. Therefore, we are interested in determining whether there is also an optimal serum P level when using a combination of oral dydrogesterone and vaginal progesterone. Consequently, the present study was designed, and we observed that there was no association between serum P levels on the day of ET and the live birth rate in artificial cycles when using a combination of oral dydrogesterone and vaginal progesterone for LPS.
In this study, we used dydrogesterone, which is an orally administered synthetic progestogen that has been successfully used for luteal phase support in stimulated IVF cycles over the past decade [16, 18, 38,39,40]. However, limited data are available about its use in artificial frozen–thawed cycles, which have different underlying endocrinological issues [41, 42]. Due to its unique molecular structure, dydrogesterone has a more selective binding capacity to the natural progesterone receptor. Therefore, much lower doses are required for dydrogesterone than for micronized progesterone [43]. Furthermore, because of the structural differences with progesterone, it cannot be quantified by any commonly used diagnostic test for measuring progesterone levels [16]. Consequently, the serum progesterone levels in this study only reflected vaginal progesterone administration. The P levels widely varied in this study, which were also observed in previous studies [20,21,22, 24]. Although all women receive the same dose of vaginal progesterone, the uptake, absorption and metabolism of each hormone can vary among women [20]. One study [41] reported comparable pregnancy rates between the oral dydrogesterone and micronized vaginal progesterone groups, using equivalent doses of 40 mg and 800 mg, respectively. In line with Rashidi’s research, our IVF unit administered 40 mg dydrogesterone orally. Therefore, the orally administered dydrogesterone probably covers the minimal threshold of serum P. Consequently, it may explain the results of the present study in which there was no association between serum P levels on the day of ET and the live birth rate in artificial cycles using a combination of oral dydrogesterone and vaginal progesterone for LPS. To our knowledge, this is the first study to estimate the association between serum P levels on the day of ET and the live birth rate using a combination of oral dydrogesterone and vaginal progesterone for LPS. The oral route of administration is thought to be a more patient-friendly regimen that lacks the side effects of vaginal or intramuscular administration. However, whether only 40 mg dydrogesterone is adequate in AC-FET for LPS remains to be determined. Although two small clinical studies have investigated the use of 30 or 40 mg oral dydrogesterone for luteal phase support in programmed frozen-thawed cycles [42, 44], there is also lack of randomized controlled trials at least at the national level for determining the required dose for oral dydrogesterone. Our luteal phase support protocol reduces the vaginal dose to a level that is more comfortable for patients, also ensures progesterone support for patients with poor vaginal absorption. There is much literature showing the relevance of measuring serum P in artificial cycles when using vaginal progesterone. But in this study it cannot be appreciated that if there is any impact of the levels of serum P according to the vaginal administration because all patients were already receiving dydrogesterone and thus, “protected” to the possible situation of bad absorption of vaginal progesterone.
Previous studies have reported that a high BMI, advanced maternal age or prolonged estrogen treatment are associated with a lower live birth rate, which in line with our study [45,46,47]. The main limitation of our study is the retrospective nature of the data. Although we adjusted our analysis to minimize the likelihood of confounding, selection bias could not be completely ruled out. Additionally, embryo aneuploidy is one of the main aspects related to implantation failure, so we have not ruled out the impact of embryo quality on this finding. Moreover, there may be a serious confounding bias in the results of this study in which there was no association between serum P levels on the day of ET and the live birth rate in artificial cycles using a combination of oral dydrogesterone(40 mg/d) and vaginal progesterone(400 mg/d) for LPS because patients were supported with combination of oral dydrogesterone and vaginal progesterones, but serum progesterone levels responded only to the latter. In other words, the orally administered 40 mg dydrogesterone probably covers the minimal threshold of serum P. So different findings may be observed if the amount of oral dydrogesterone is reduced.
Conclusions
This is the first study to estimate the association between serum P levels on the day of ET and live birth in artificial cycles using a combination of oral dydrogesterone(40 mg/d) and vaginal progesterone(400 mg/d) for LPS. We found that the serum P levels on the day of ET do not correlate with live birth using the combination progesterone for LPS. In addition, prospective, randomized, controlled, blinded trials are merited to determine the optimal dosing regimen for oral dydrogesterone in in AC-FET for LPS.
Data Availability
The data used and analyzed during the study are available from the corresponding author if the request is reasonable.
Abbreviations
- P:
-
Progesterone
- FET:
-
Frozen-thawed embryo transfer
- ET:
-
Embryo transfer
- LB:
-
Live birth
- AC:
-
Artificial cycles
- LPS:
-
Luteal phase support
- E2:
-
Estradiol
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- ART:
-
Assisted reproductive technology
- IVF:
-
In vitro fertilization
- ICSI:
-
Intracytoplasmic sperm injection
- MVP:
-
Micronized vaginal progesterone
- hCG:
-
Human chorionic gonadotrophin
- CPR:
-
Clinical pregnancy rate
- OPR:
-
Ongoing pregnancy rate
- PTB:
-
Preterm birth
- LBW:
-
Low birthweight
- PPOS:
-
Progestin-primed ovarian stimulation
References
Mackens S, Santos-Ribeiro S, van de Vijver A, Racca A, Van Landuyt L, Tournaye H, et al. Frozen embryo transfer: a review on the optimal endometrial preparation and timing. Hum Reprod. 2017;32(11):2234–42.
Chen ZJ, Shi Y, Sun Y, Zhang B, Liang X, Cao Y, et al. Fresh versus frozen embryos for infertility in the polycystic ovary syndrome. N Engl J Med. 2016;375(6):523–33.
Devroey P, Polyzos NP, Blockeel C. An OHSS-Free clinic by segmentation of IVF treatment. Hum Reprod. 2011;26(10):2593–7.
Montagut M, Santos-Ribeiro S, De Vos M, Polyzos NP, Drakopoulos P, Mackens S, et al. Frozen-thawed embryo transfers in natural cycles with spontaneous or induced ovulation: the search for the best protocol continues. Hum Reprod. 2016;31(12):2803–10.
Yarali H, Polat M, Mumusoglu S, Yarali I, Bozdag G. Preparation of endometrium for frozen embryo replacement cycles: a systematic review and meta-analysis. J Assist Reprod Genet. 2016;33(10):1287–304.
Maheshwari A, Bell JL, Bhide P, Brison D, Child T, Chong HY, et al. Elective freezing of embryos versus fresh embryo transfer in IVF: a multicentre randomized controlled trial in the UK (E-Freeze). Hum Reprod. 2022;37(3):476–87.
Ghobara T, Gelbaya TA, Ayeleke RO. Cycle regimens for frozen-thawed embryo transfer. Cochrane Database Syst Rev. 2017;7:CD003414.
Ortega I, Garcia Velasco JA. Progesterone supplementation in the frozen embryo transfer cycle. Curr Opin Obst Gynecol. 2015;27(4):253–7.
Toner JP. The corpus luteum is more than progesterone. Fertil Steril. 2021;115(6):1432.
Christin-Maitre S, Bouchard P, Spitz IM. Medical termination of pregnancy. N Engl J Med. 2000;342(13):946–56.
van der Linden M, Buckingham K, Farquhar C, Kremer JA, Metwally M. Luteal phase support for assisted reproduction cycles.The Cochrane database of systematic reviews. 2015(7):CD009154.
Leonard PH, Hokenstad AN, Khan Z, Jensen JR, Stewart EA, Coddington CC. Progesterone support for frozen embryo transfer: intramuscular versus vaginal suppository demonstrates no difference in a cohort. J Reprod Med. 2015;60(3–4):103–8.
Almohammadi A, Raveendran A, Black M, Maheshwari A. The optimal route of progesterone administration for luteal phase support in a frozen embryo transfer: a systematic review.Arch Gynecol Obstet. 2022.
Devine K, Richter KS, Widra EA, McKeeby JL. Vitrified blastocyst transfer cycles with the use of only vaginal progesterone replacement with endometrin have inferior ongoing pregnancy rates: results from the planned interim analysis of a three-arm randomized controlled noninferiority trial. Fertil Steril. 2018;109(2):266–75.
Warren MP. Vaginal progesterone and the vaginal first-pass effect. Climacteric. 2018;21(4):355–7.
Griesinger G, Blockeel C, Sukhikh GT, Patki A, Dhorepatil B, Yang DZ, et al. Oral dydrogesterone versus intravaginal micronized progesterone gel for luteal phase support in IVF: a randomized clinical trial. Hum Reprod. 2018;33(12):2212–21.
Tataru C, Dessapt AL, Pietin-Vialle C, Pasquier M, Bry-Gauillard H, Massin N. [Dydrogesterone versus micronized vaginal progesterone as luteal phase support after fresh embryo transfer in IVF]. Gynecol Obstet Fertil Senol. 2022;50(6):455–61.
Tournaye H, Sukhikh GT, Kahler E, Griesinger G. A phase III randomized controlled trial comparing the efficacy, safety and tolerability of oral dydrogesterone versus micronized vaginal progesterone for luteal support in in vitro fertilization. Hum Reprod. 2017;32(10):2152.
Brady PC, Kaser DJ, Ginsburg ES, Ashby RK, Missmer SA, Correia KF, et al. Serum progesterone concentration on day of embryo transfer in donor oocyte cycles. J Assist Reprod Genet. 2014;31(5):569–75.
Yovich JL, Conceicao JL, Stanger JD, Hinchliffe PM, Keane KN. Mid-luteal serum progesterone concentrations govern implantation rates for cryopreserved embryo transfers conducted under hormone replacement. Reprod Biomed Online. 2015;31(2):180–91.
Cedrin-Durnerin I, Isnard T, Mahdjoub S, Sonigo C, Seroka A, Comtet M, et al. Serum progesterone concentration and live birth rate in frozen-thawed embryo transfers with hormonally prepared endometrium. Reprod Biomed Online. 2019;38(3):472–80.
Labarta E, Mariani G, Holtmann N, Celada P, Remohi J, Bosch E. Low serum progesterone on the day of embryo transfer is associated with a diminished ongoing pregnancy rate in oocyte donation cycles after artificial endometrial preparation: a prospective study. Hum Reprod. 2017;32(12):2437–42.
Kofinas JD, Blakemore J, McCulloh DH, Grifo J. Serum progesterone levels greater than 20 ng/dl on day of embryo transfer are associated with lower live birth and higher pregnancy loss rates. J Assist Reprod Genet. 2015;32(9):1395–9.
Alsbjerg B, Thomsen L, Elbaek HO, Laursen R, Povlsen BB, Haahr T, et al. Progesterone levels on pregnancy test day after hormone replacement therapy-cryopreserved embryo transfer cycles and related reproductive outcomes. Reprod Biomed Online. 2018;37(5):641–7.
Gaggiotti-Marre S, Martinez F, Coll L, Garcia S, Alvarez M, Parriego M, et al. Low serum progesterone the day prior to frozen embryo transfer of euploid embryos is associated with significant reduction in live birth rates. Gynecol endocrinology: official J Int Soc Gynecol Endocrinol. 2019;35(5):439–42.
Coughlan C, Ledger W, Wang Q, Liu F, Demirol A, Gurgan T, et al. Recurrent implantation failure: definition and management. Reprod Biomed Online. 2014;28(1):14–38.
Huang J, Lu X, Xie Q, Lin J, Cai R, Kuang Y. Timing of frozen-thawed embryo transfer after controlled ovarian stimulation in a non-elective freeze-all policy. Ann Transl Med. 2019;7(23):752.
Yu S, Long H, Chang HY, Liu Y, Gao H, Zhu J, et al. New application of dydrogesterone as a part of a progestin-primed ovarian stimulation protocol for IVF: a randomized controlled trial including 516 first IVF/ICSI cycles. Hum Reprod. 2018;33(2):229–37.
Kuang Y, Chen Q, Fu Y, Wang Y, Hong Q, Lyu Q, et al. Medroxyprogesterone acetate is an effective oral alternative for preventing premature luteinizing hormone surges in women undergoing controlled ovarian hyperstimulation for in vitro fertilization. Fertil Steril. 2015;104(1):62–70e3.
Cummins JM, Breen TM, Harrison KL, Shaw JM, Wilson LM, Hennessey JF. A formula for scoring human embryo growth rates in in vitro fertilization: its value in predicting pregnancy and in comparison with visual estimates of embryo quality. J In Vitro Fert Embryo Transf. 1986;3(5):284–95.
Gardner DK, Lane M, Schoolcraft WB. Physiology and culture of the human blastocyst. J Reprod Immunol. 2002;55(1–2):85–100.
Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, et al. The International Glossary on Infertility and Fertility Care, 2017. Fertil Steril. 2017;108(3):393–406.
Du T, Wang Y, Fan Y, Zhang S, Yan Z, Yu W, et al. Fertility and neonatal outcomes of embryos achieving blastulation on Day 7: are they of clinical value? Hum Reprod. 2018;33(6):1038–51.
Bonduelle M, Liebaers I, Deketelaere V, Derde MP, Camus M, Devroey P, et al. Neonatal data on a cohort of 2889 infants born after ICSI (1991–1999) and of 2995 infants born after IVF (1983–1999). Hum Reprod. 2002;17(3):671–94.
Shapiro D, Boostanfar R, Silverberg K, Yanushpolsky EH. Examining the evidence: progesterone supplementation during fresh and frozen embryo transfer. Reprod Biomed Online. 2014;29(Suppl 1):1–14. quiz S5-6.
Shi Y, Sun Y, Hao C, Zhang H, Wei D, Zhang Y, et al. Transfer of fresh versus frozen embryos in ovulatory women. N Engl J Med. 2018;378(2):126–36.
Wei D, Liu JY, Sun Y, Shi Y, Zhang B, Liu JQ, et al. Frozen versus fresh single blastocyst transfer in ovulatory women: a multicentre, randomised controlled trial. Lancet. 2019;393(10178):1310–8.
Chakravarty BN, Shirazee HH, Dam P, Goswami SK, Chatterjee R, Ghosh S. Oral dydrogesterone versus intravaginal micronised progesterone as luteal phase support in assisted reproductive technology (ART) cycles: results of a randomised study. J Steroid Biochem Mol Biol. 2005;97(5):416–20.
Ganesh A, Chakravorty N, Mukherjee R, Goswami S, Chaudhury K, Chakravarty B. Comparison of oral dydrogestrone with progesterone gel and micronized progesterone for luteal support in 1,373 women undergoing in vitro fertilization: a randomized clinical study. Fertil Steril. 2011;95(6):1961–5.
Salehpour S, Tamimi M, Saharkhiz N. Comparison of oral dydrogesterone with suppository vaginal progesterone for luteal-phase support in in vitro fertilization (IVF): a randomized clinical trial. Iran J Reprod Med. 2013;11(11):913–8.
Rashidi BH, Ghazizadeh M, Tehrani Nejad ES, Bagheri M, Gorginzadeh M. Oral dydrogesterone for luteal support in frozen-thawed embryo transfer artificial cycles: a pilot randomized controlled trial. Asian Pac J Reprod. 2016;5(6):490–4.
Zarei A, Sohail P, Parsanezhad ME, Alborzi S, Samsami A, Azizi M. Comparison of four protocols for luteal phase support in frozen-thawed embryo transfer cycles: a randomized clinical trial. Arch Gynecol Obstet. 2017;295(1):239–46.
Schindler AE. Progestational effects of dydrogesterone in vitro, in vivo and on the human endometrium. Maturitas. 2009;65(Suppl 1):3–11.
Guo W, Chen X, Ye D, He Y, Li P, Niu J, et al. [Effects of oral dydrogesterone on clinical outcomes of frozen-thawed embryo transfer cycles]. Nan fang yi ke da xue xue bao = Journal of Southern Medical University. 2013;33(6):861–5.
Arabipoor A, Ashrafi M, Hemat M, Zolfaghari Z. The Effects of maternal and paternal body Mass Index on live birth rate after intracytoplasmic sperm injection cycles. Int J fertility Steril. 2019;13(1):24–31.
Zhu Q, Chen Q, Wang L, Lu X, Lyu Q, Wang Y, et al. Live birth rates in the first complete IVF cycle among 20 687 women using a freeze-all strategy. Hum Reprod. 2018;33(5):924–9.
Bourdon M, Santulli P, Kefelian F, Vienet-Legue L, Maignien C, Pocate-Cheriet K, et al. Prolonged estrogen (E2) treatment prior to frozen-blastocyst transfer decreases the live birth rate. Hum Reprod. 2018;33(5):905–13.
Acknowledgements
The authors thank all staff of the department of assisted reproduction and the infertile couples who participated in this study.
Funding
This study was funded by the National Nature Science Foundation of China (Grant no.81903324) and Science and Technology Plan Project of Wenzhou(no.Y20220054).
Author information
Authors and Affiliations
Contributions
J.Z. and X.F.H conceived and designed this study. Q.Q.Z. and J.L.H. drafted the manuscript. Q.Q.Z., J.L.H., Y.L. and L.Y.J contributed to the data analysis. J.Z., Q.Q.Z. and J.L.H. were responsible for the collection of the data. J.Z revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
This study conformed to the guidelines of the Declaration of Helsinki, and the study procedures were reviewed and approved by the Ethics Committee (Institutional Review Board) of the Ninth People’s Hospital of Shanghai.
Informed consent
All participants provided informed consents after counseling for infertility treatments and routine IVF procedures.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhu, Q., Huang, J., Lin, Y. et al. Association between serum progesterone levels on the day of frozen-thawed embryo transfer and pregnancy outcomes after artificial endometrial preparation. BMC Pregnancy Childbirth 23, 401 (2023). https://doi.org/10.1186/s12884-023-05596-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05596-4