Abstract
Background
Opioid exposure during pregnancy has increased alarmingly in recent decades. However, the association between prenatal opioid exposure and congenital malformation risk has still been controversial. We aim to assess the association between opioid exposure during pregnancy and the risk of congenital malformations.
Method
PubMed, Embase, and Cochrane library of clinical trials were systematically searched to September 13th, 2021. Cohort studies reporting risk of congenital malformation after opioid exposure compared with non-exposure during pregnancy were included. Risk of studies was appraised with the ROBINS-I tool. Meta-analysis was conducted using the random-effects model. Subgroup analyses were conducted for the primary outcome based on indication, exposed period, whether adjusted data was used, and risk of bias assessment. Meta-regression was performed to evaluate the relation of publication year.
Main results
Eighteen cohort studies with 7,077,709 patients were included. The results showed a significant increase in the risk of overall congenital malformation (RR = 1.30, 95%CI: 1.11–1.53), major malformation (RR = 1.57, 95%CI:1.11–2.22), central nervous system malformation (RR = 1.36, 95% CI:1.19–1.55), and limb malformation (RR = 2.27, 95%CI:1.29–4.02) with opioid exposure during pregnancy. However, the predictive interval conveyed a different result on overall congenital malformation (95%PI: 0.82–2.09) and major malformation (95%PI: 0.82–2.09). No association between opioid exposure and overall congenital malformation in the first trimester (RR = 1.12, 95%CI:0.97–1.31) and prescribed for analgesic or antitussive treatment (RR = 1.03, 95%CI:0.94–1.13) were observed. In subgroups that study provided data adjusted for confounders (RR = 1.06, 95%CI:0.93–1.20) or identified moderate or serious risk of bias (RR = 1.00, 95%Cl: 0.85–1.16; RR = 1.21, 95%Cl: 1.60–2.68), no association was found.
Conclusion
Opioid exposed in the first trimester or prescribed for analgesic or antitussive treatment did not increase the risk of overall congenital malformation. The findings should be discussed in caution considering the situation of individual patients and weigh out its potential risk of congenital malformation.
Trial registration
Registration number: CRD42021279445.
Similar content being viewed by others
Introduction
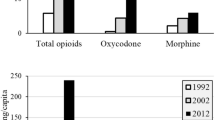
Opioid is frequently prescribed for pain, such as lower back pain and pelvic joint pain, to reduce perception of pain during pregnancy. Also, opioid medications, such as methadone and buprenorphine, are used to treat opioid use disorder [1]. Opioid exposure during pregnancy has increased alarmingly in recent decades [2,3,4,5,6,7,8]. It was reported that 21.6% of women receive an opioid prescription during pregnancy in the US, which meant up to one of five pregnant women filled an opioid prescription [4]. The prescriptions were widespread in either commercial insurance or Medicaid [5, 9]. A 2019 self-reported study found that about 7% of women reported using prescription opioid pain relievers during pregnancy [7]. On the other hand, increasing opioid use among reproductive-age women has also been widespread [9, 10]. Since unplanned pregnancies are not uncommon and many pregnancies are not recognized until a few weeks after conception [11], all women prescribed opioid at reproductive age were at potential risk [12].
The association between prenatal opioid exposure and congenital malformation risk has still been controversial. Two studies funded by the Centers for Disease Control and Prevention have set off an upsurge in studying the relationship between opioid use during pregnancy and congenital malformations [13, 14]. Some studies reported an increased risk of congenital malformations in relation to maternal opioid use [13, 15,16,17], while other studies have found no association [18, 19]. Specially, a systematic review from the CDC in the US reported some potential higher risk of congenital malformations related to opioid exposure during pregnancy, such as congenital malformations overall, cardiovascular malformations, oral cleft, and clubfoot [20]. However, they still reported uncertainty regarding the teratogenicity of opioids. Recently, two large population-based cohort studies have been conducted to explore the gestational opioid exposure and risk of congenital malformations in Europe and the US [21, 22]. Bateman et al. [21] reported that prescription opioids used in early pregnancy are not associated with a substantial increase in risk for most of the malformation types considered except oral clefts. Wen [22] found no excess risk for major birth defects in infants with opioid exposure in the first trimester. In contrast, a higher risk of minor congenital malformations associated with opioid use in the third trimester was found.
These findings call for the safety re-evaluation of opioid exposure during pregnancy to inform clinical practice. Therefore, we performed a meta-analysis using data from real-world cohort studies to assess the association between opioid exposure during pregnancy and the risk of congenital malformations.
Methods
Protocol and registration
We followed the Meta-analysis of Observational Studies in Epidemiology [23] to perform the meta-analysis. The study protocol was registered at https://www.crd.york.ac.uk/prospero/ (registration number CRD42021279445) before searching articles.
Eligibility criteria
We used PICOS model to select the population. The inclusion criteria were: (1) cohort studies; (2) investigated opioid use during pregnancy; (3) reported both opioids-exposed and -unexposed group; (4) reported on any congenital malformations and specific congenital malformation at birth; (5) reported available data, such as odds ratio (OR), adjusted OR, risk ratio (RR), adjusted RR, hazard ratio (HR), or data to calculate RR; (6) reported outcomes including any congenital malformations, major congenital malformation, and/or sub-categories of congenital malformations. The exclusion criteria were: (1) review, systematic review and meta-analysis, conference abstract, and case report; (2) not human studies; (3) did not clarify the exposure of opioid during pregnancy; (4) overlapped data source is included.
Search strategy
We systematically searched PubMed, Embase, and Cochrane library of clinical trials up to September 13th, 2021. The search terms were attached in Table S1.
Selection of studies and data extraction
Two reviewers (X.W, Y.W) independently screened titles and abstracts through Endnote (version 9.3.2). Duplications were removed through Endnote and manually. We also screened the references lists of relevant reviews and articles. Any disagreement was resolved by discussion until consensus was reached or by consulting a third author (X.F).
Data were independently extracted by two investigators (X.W and Y.W) for eligible studies. Disagreements were discussed and resolved by a third author (X.F). The data obtained for each study included first author, year of publication, study setting, drug used, exposure measurement, exposed period, outcome assessment, indication, sample size, congenital malformations with their risk estimates, 95% confidence interval (CI) and 95% prediction interval (PI). The primary outcome was overall congenital malformations. The secondary outcome was organ-specific congenital malformations.
Quality assessment
We assessed the risk of bias for each study included using the ROBINS-I tool [24], which is developed for evaluating risk of bias of interventions for non-randomized studies. The quality of each study was evaluated for the risk of bias in seven domains: (1) bias due to confounding; (2) bias in selection of participants into the study; (3) bias in classification of intervention; (4) bias due to deviations from intended interventions; (5) bias due to missing data; (6) bias in measurement of outcomes; (7) bias in selection of the reported result. The interpretations of domain level and overall judgment for risk of bias are classified as low, moderate, serious, or critical.
We evaluated the level of evidence for each outcome using Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach [25]. The results were classified as high, moderate, low, or very low.
Statistical analysis
The meta-analysis was conducted with R (version 4.0.5). For the expected high heterogeneity in terms of the enrolled populations, DerSimonian and Laird random-effect models was used to pool RRs along with the corresponding 95% CIs. Due to the low prevalence of congenital malformation in the general population, we proposed RR, HR, and OR to be comparable. For those studies that did not report the RRs of congenital malformations, we used other risk measures, including ORs or HRs, as an approximation to the RRs. Therefore, we summarized them together using meta-analysis methods. The adjusted effect sizes were selected to pool the risk estimates preferentially. Statistical heterogeneity among studies was tested using Cochran’s Q test and the I2 statistic. I2 > 50% or P < 0.05 was considered to indicate significant heterogeneity. We also addressed heterogeneity by calculating the 95% prediction interval for the pooled unadjusted OR, which gives an estimate of the point at which the true effects are to be expected for 95% of similar studies that might be conducted in the future [26]. The Egger test was used to assess the funnel plot for asymmetry, indicating possible publication biases.
To explore the sources of heterogeneity, subgroup analyses were run for primary outcome based on indication (analgesic or antitussive treatment, opioid abuse or opioid abuse treatment), exposed period (first trimester, all trimesters), risk of bias assessment (moderate, serious, critical), and whether adjusted data was used (yes, no). Due to the large span of publication year of included studies, we performed random-effects meta-regression analyses by the empirical Bayes method to estimate the between-study variance and the method by Hartung and Knapp was used to adjust statistics and evaluate the relation of covariates (year of publication) on the primary outcome. To evaluate the stability of the results, sensitivity analyses were performed with the leave-one-out method.
Results
One thousand one hundred seventeen studies were identified after database searching. 18 additional records were identified manually through references lists of relevant articles. After removing the duplications, 1030 studies were excluded by screening titles and abstracts. Only 18 studies [15, 16, 19, 21, 22, 27,28,29,30,31,32,33,34,35,36,37,38,39] were eligible for meta-analysis after full-text assessment (Fig. 1). Characteristics of the included studies are presented in Table 1. The included studies were published between 1976 and 2021. According to the results of risk of bias assessment using ROBIN-I tool, the risk of bias of each included study ranged from moderate to critical. The results of all domains of quality assessment are summarized in Table S2. In addition, according to the GRADE approach, the overall level of evidence among all outcomes ranged from very low to moderate (Table 2).
Opioid indications were analgesic or antitussive treatment, opioid abuse, and opioid abuse treatment. The total sample size of these studies ranged from 96 to 2,780,256. Kallen 2015 and Kallen 2013 were both from the Swedish Medical Birth Register and the time covered were overlapped. Therefore, we included Kallen 2013 (reported all opioids exposure) for statistical analysis in most outcomes. Kallen 2015 were included for analysis for urogenital malformation, where Kallen 2013 did not provide available data. Sensitivity analysis and subgroup analysis was conducted only for overall congenital malformations for the few studies included in different specific congenital malformations.
Overall congenital malformation
Thirteen studies [15,16,17, 19, 21, 28,29,30,31,32, 35,36,37] reported overall congenital malformation. The results showed a significant increase in the risk of congenital malformations with opioid exposure during pregnancy (RR = 1.30, 95%CI: 1.11–1.53); however, the 95% predictive interval (95%PI: 0.82–2.09) did not show the same effect. This indicates the uncertainty of the estimates and in the conclusions, given the observed between-study heterogeneity (P<0.001, I2 = 82%) (Fig.2). No evident asymmetry in the funnel plot (Fig. S1).
Organ-specific congenital malformations
The summary of meta-analysis of 13 estimates, which analyzed organ-specific congenital malformations, was shown in Fig. 3. The interpretation of major malformation (RR = 1.57, 95%CI:1.11–2.22), central nervous system (CNS) malformation (RR = 1.36, 95%CI:1.19–1.55) and limb malformation (RR = 2.27, 95%CI:1.29–4.02) using the confidence interval shows a statistically significant treatment effect, whereas the predictive interval conveyed a different result on major malformation (95%PI: 0.82–2.09). No significant relationship between opioid use and cardiovascular malformation, gastrointestinal malformation, ear, face, and neck malformation, respiratory malformation, musculoskeletal malformation, urogenital malformation, orofacial clefts, neural tube defects, gastroschisis, and clubfoot were found (Fig. S2–14).
Sensitivity analysis and meta-regression
The sensitivity analyses revealed no substantial change in the pooled risk estimates upon excluding of any single study (Fig. 4). Meta-regression analysis based on the year of publication showed no significant relationship (Fig. S15).
Subgroup analysis
We performed subgroup analyses regarding exposed period, indication, adjusted for confounders, and risk of bias assessment by ROBINS-I (Fig. S16–20). The results were summarized in Table 3. There was no significant increased risk of overall congenital malformation among studies that specifically examined exposure to opioids in the first trimester (RR = 1.12, 95%Cl:0.97–1.31). In contrast, studies reported opioid exposure during pregnancy, no significant result was observed. When stratified by indication, studies that use opioid abuse or opioid abuse treatment as a reason for opioid exposure, the risk (RR = 2.09, 95%Cl:1.74–2.52) was significantly increased. No difference was found for those opioid use for analgesic or antitussive treatment (RR = 1.03, 95%Cl:0.94–1.13). In addition, a significant association was found in studies that used unadjusted data (RR = 2.07, 95%CI:1.60–2.68), but not in studies that provided adjusted data (RR = 1.06, 95%CI:0.93–1.20). Furthermore, studies with moderate or serious risk of bias showed no significant difference between opioid exposure and overall congenital malformation (RR = 1.00, 95%Cl: 0.85–1.16; RR = 1.21, 95%Cl: 0.90–1.63).
Discussion
The overall result of this meta-analysis included 18 cohort studies and demonstrated opioid exposure during pregnancy with a 1.3-fold risk of congenital malformations. Additionally, opioid use was associated with increased risks of major malformation, CNS malformation, and limb malformation with an increase of 57, 36, and 127%, respectively. We found no significant relationship between opioid use and cardiovascular malformation, gastrointestinal malformation, ear, face, and neck malformation, respiratory malformation, musculoskeletal malformation, urogenital malformation, orofacial clefts, neural tube defects, gastroschisis, and clubfoot were found. No association in subgroups that opioid was exposed in the first trimester or prescribed for analgesic or antitussive treatment. However, the positive findings were only observed in subgroups that studies provided data unadjusted for confounders or identified critical risk of bias assessment. In subgroups that study provided data adjusted for confounders or identified moderate or serious risk of bias, no association of opioid exposure and overall congenital malformation was found between exposed and not exposed group.
Opioids can compound act on the endogenous opioid system, which comprises four G protein-coupled receptors and four major peptide families. They can regulate neuronal function and neurotransmission in human brain, brain stem and other tissues, to effectively prevent the sensation of pain from being transmitted to the brain [40]. Pregnant women would experience various physiological changes in the body, such as changes in renal blood flow, gastric emptying speed, plasma protein level and apparent distribution volume, making it difficult to predict the pharmacokinetic metabolism of opioids. For instance, maternal hepatic metabolism altered in pregnancy [41, 42], affecting the pharmacokinetics of several opioids metabolized through these pathways [43]. The increase of tidal volume and respiratory rate during pregnancy may also promote the absorption of drugs into the system through the alveoli, which could amplify fetal drug exposure to inhaled opioids [44]. Moreover, the plasma albumin of pregnant women will gradually decrease and reach stabilization at the end of the first trimester in pregnancy, which will make the free fraction of high plasma protein binding drugs such as oxycodone, methadone, and fentanyl higher than non-pregnant women [45, 46]. Zagon [47] found that the opioid exposure of rats during pregnancy will reduce DNA synthesis in three germ layer organ cells which leads to fetal congenital malformation. It was proposed that exogenous opioids during the critical period might destroy the normal development process and lead to fetal congenital malformations. Nevertheless, we found a significantly increased risk of congenital malformation during pregnancy while no difference in the first trimester. More research exploring the biological mechanism of opioid exposure and congenital malformation were needed.
When stratified by opioid indications, we found opioid use for analgesic or antitussive treatment did not associate with a higher risk of congenital malformation compared with no exposure. On the contrary, patients who use opioids for abuse or opioid-dependent treatment were more likely to give birth to babies with congenital malformations. The cumulative dose of drug used varied between these indications may explain one of the reasons, which might cause increased blood drug level and risk of congenital malformations. Given that those who were addicted to opioids were at greater risk of misusing prescription opioids and might use more opioids, which is way higher than the therapeutic safe boundary [48]. Only two studies reported the dose-response relationship between opioid and congenital malformations. Wen [22] observed that overall minor birth defects showed significant dose responses in trimester 3. No evidence of increasing risk with higher cumulative opioid exposure was found for any of the primary outcomes as demonstrated by Bateman [21]. The higher dosage range of these studies varied from ≥42.25 cumulative morphine milligram equivalent (MME) to > 300 MME. More research assessing the dose-response relationship between opioid use and the risk of congenital malformations should be pursued.
After stratified by whether the study controlled for potential confounders to avoid unpredictable bias introduced by other confounders, we found significant heterogeneity between subgroups. The confounding factors included baseline characteristic such as maternal age, obesity, tobacco use, parity, and so on. Alternatively, the result of confounders adjusted studies showed no association between opioid use and overall congenital malformations, which is different from the pooled result. The potential confounders adjusted in these studies were not consistent. For example, Bateman [21] and Nezvalová-Henriksen [19] adjusted for concomitant medication use while others did not. Furthermore, in both subgroup of moderate and serious risk of bias, most of which adjusted for confounders, the result showed no association between opioid exposure and overall congenital malformation. The results still provide reasonable doubt that after adjusting some potential confounders, opioid itself did not contribute to a higher risk of overall congenital malformations.
Our findings provide evidence for health professionals to weigh the benefit of opioid along with its potential risks. Also, pregnant women, women intended to get pregnant, or reproductive-aged women at risk of any unintended pregnancy could evaluate the potential risk of opioid during pregnancy. Still, the use of opioid in some situations, especially medication assisted therapy for the treatment of substance use disorder, might provide far greater benefits than risks [49]. Our results should be treated with caution by pregnancy opioids users or potential opioid users to make the safest choice. Besides, since we detected raised risk of major congenital malformation, CNS malformation, and limb malformation, exposed pregnant women could take ultrasound examinations more frequently to detect the fetus growth, especially for CNS growth and limb growth.
Our study has several strengths. To date, this is the first meta-analysis evaluating the association between opioid exposure and the risk of congenital malformations. The meta-analysis included a large sample size of 7,077,709 patients and only cohort studies to reduce recall and selection bias. We also did comprehensive subgroup analyses to evaluate the relationship between opioid use and congenital malformations.
Our findings are also subject to several limitations. Firstly, the publication year of the studies included ranged from 1976 to 2021 and might contribute to methodologic bias. However, no significance was observed on meta-regression evaluating the relation of publication year and overall congenital malformations. Secondly, high heterogeneity was detected in most of the outcomes. The reason might be that all included studies are retrospective studies, with the potential for confounding. We performed subgroup analyses to reduce the possible influence. Besides, included studies reported congenital malformations based on several kinds of opioids. Some contained only methadone, and some investigated opioid prescriptions, including hydrocodone, oxycodone, codeine. This might contribute to the heterogeneity of the results. Thirdly, the evaluation of the prediction interval revealed that the current 95%CI produces a positive biased estimate of the overall congenital malformation and major malformation, probably due to the between-study heterogeneity, or to the very low certainty of evidence for the two outcomes. Therefore, large size studies with higher level evidence are needed. Fourthly, most of the studies considered the pregnancies as opioid-exposed by referring to prescriptions during pregnancy, it might be possible that though prescriptions were dispensed while opioids were not taken. Well-designed prospective studies are needed to affirm the findings. Fifthly, few studies reported organ-specific malformations, and the categories of malformations reported were inconsistent. For example, Cleary [15] reported 10/13 of the organ-specific malformations, Kelty [16] reported 8/13, and Brown [27] only reported 2/13. Hence, we were unable to carry subgroup analyses. More studies were needed to provide data classified by specific organs to assess the association between opioid exposure and the risk of organ-specific malformations.
Conclusion
In conclusion, we found that maternal opioid exposure in pregnancy was associated with increased risk of major malformation, CNS malformation, and limb malformation. Opioid exposed in the first trimester or prescribed for analgesic or antitussive treatment did not increase the risk of overall congenital malformation. In studies with moderate or serious risk of bias or studies adjusted for confounders, no association was found between opioid exposure and overall congenital malformation. Therefore, the results should be interpreted in caution.
Availability of data and materials
All data are available within the manuscript and supplemental materials.
References
Donohue JM, Jarlenski MP, Kim JY, Tang L, Ahrens K, Allen L, et al. Use of medications for treatment of opioid use disorder among US Medicaid enrollees in 11 states, 2014-2018. Jama. 2021;326(2):154–64. https://doi.org/10.1001/jama.2021.7374.
Engeland A, Bjørge T, Klungsøyr K, Hjellvik V, Skurtveit S, Furu K. Trends in prescription drug use during pregnancy and postpartum in Norway, 2005 to 2015. Pharmacoepidemiol Drug Saf. 2018;27(9):995–1004. https://doi.org/10.1002/pds.4577.
Daw JR, Mintzes B, Law MR, Hanley GE, Morgan SG. Prescription drug use in pregnancy: a retrospective, population-based study in British Columbia, Canada (2001-2006). Clin Ther. 2012;34(1):239–49.e2. https://doi.org/10.1016/j.clinthera.2011.11.025.
Desai RJ, Hernandez-Diaz S, Bateman BT, Huybrechts KF. Increase in prescription opioid use during pregnancy among Medicaid-enrolled women. Obstet Gynecol. 2014;123(5):997–1002. https://doi.org/10.1097/aog.0000000000000208.
Bateman BT, Hernandez-Diaz S, Rathmell JP, Seeger JD, Doherty M, Fischer MA, et al. Patterns of opioid utilization in pregnancy in a large cohort of commercial insurance beneficiaries in the United States. Anesthesiology. 2014;120(5):1216–24. https://doi.org/10.1097/aln.0000000000000172.
Jones CM, Logan J, Gladden RM, Bohm MK. Vital signs: demographic and substance use trends among heroin users - United States, 2002-2013. MMWR Morb Mortal Wkly Rep. 2015;64(26):719–25.
Ko JY, D'Angelo DV, Haight SC, Morrow B, Cox S, Salvesen von Essen B, et al. Vital signs: prescription opioid pain reliever use during pregnancy - 34 U.S. jurisdictions, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(28):897–903. https://doi.org/10.15585/mmwr.mm6928a1.
Epstein RA, Bobo WV, Martin PR, Morrow JA, Wang W, Chandrasekhar R, et al. Increasing pregnancy-related use of prescribed opioid analgesics. Ann Epidemiol. 2013;23(8):498–503. https://doi.org/10.1016/j.annepidem.2013.05.017.
Gallagher BK, Shin Y, Roohan P. Opioid prescriptions among women of reproductive age enrolled in Medicaid - New York, 2008-2013. MMWR Morb Mortal Wkly Rep. 2016;65(16):415–7. https://doi.org/10.15585/mmwr.mm6516a2.
Miller AM, Sanderson K, Bruno RB, Breslin M, Neil AL. Chronic pain, pain severity and analgesia use in Australian women of reproductive age. Women Birth. 2019;32(2):e272–e8. https://doi.org/10.1016/j.wombi.2018.06.013.
Moreira LR, Ewerling F, Dos Santos IS, Wehrmeister FC, Matijasevich A, Barros AJD, et al. Trends and inequalities in unplanned pregnancy in three population-based birth cohorts in Pelotas. Brazil Int J Public Health. 2020;65(9):1635–45. https://doi.org/10.1007/s00038-020-01505-0.
Auerbach SL, Agbemenu K, Ely GE, Lorenz R. A review of unintended pregnancy in opioid-using women: implications for nursing. J Addict Nurs. 2021;32(2):107–14. https://doi.org/10.1097/jan.0000000000000396.
Broussard CS, Rasmussen SA, Reefhuis J, Friedman JM, Jann MW, Riehle-Colarusso T, et al. Maternal treatment with opioid analgesics and risk for birth defects. Am J Obstet Gynecol. 2011;204(4):314.e1–11. https://doi.org/10.1016/j.ajog.2010.12.039.
Yazdy MM, Mitchell AA, Tinker SC, Parker SE, Werler MM. Periconceptional use of opioids and the risk of neural tube defects. Obstet Gynecol. 2013;122(4):838–44. https://doi.org/10.1097/AOG.0b013e3182a6643c.
Cleary BJ, Donnelly JM, Strawbridge JD, Gallagher PJ, Fahey T, White MJ, et al. Methadone and perinatal outcomes: a retrospective cohort study. Am J Obstet Gynecol. 2011;204(2):139.e1–9. https://doi.org/10.1016/j.ajog.2010.10.004.
Kelty E, Hulse G. A retrospective cohort study of birth outcomes in neonates exposed to naltrexone in utero: a comparison with methadone. Buprenorphine- Non-opioid-Exposed Neonates Drugs. 2017;77(11):1211–9. https://doi.org/10.1007/s40265-017-0763-8.
Nørgaard M, Nielsson MS, Heide-Jørgensen U. Birth and neonatal outcomes following opioid use in pregnancy: a Danish population-based study. Subst Abuse. 2015;9(Suppl 2):5–11. https://doi.org/10.4137/sart.S23547.
Jumah NA, Edwards C, Balfour-Boehm J, Loewen K, Dooley J, Gerber Finn L, et al. Observational study of the safety of buprenorphine+naloxone in pregnancy in a rural and remote population. BMJ Open. 2016;6(10):e011774. https://doi.org/10.1136/bmjopen-2016-011774.
Nezvalová-Henriksen K, Spigset O, Nordeng H. Effects of codeine on pregnancy outcome: results from a large population-based cohort study. Eur J Clin Pharmacol. 2011;67(12):1253–61. https://doi.org/10.1007/s00228-011-1069-5.
Lind JN, Interrante JD, Ailes EC, Gilboa SM, Khan S, Frey MT, et al. Maternal use of opioids during pregnancy and congenital malformations: a systematic review. Pediatrics. 2017;139(6). https://doi.org/10.1542/peds.2016-4131.
Bateman BT, Hernandez-Diaz S, Straub L, Zhu Y, Gray KJ, Desai RJ, et al. Association of first trimester prescription opioid use with congenital malformations in the offspring: population based cohort study. BMJ (Clinical research ed). 2021;372:n102. https://doi.org/10.1136/bmj.n102.
Wen X, Belviso N, Murray E, Lewkowitz AK, Ward KE, Meador KJ. Association of Gestational Opioid Exposure and Risk of major and minor congenital malformations. JAMA Netw Open. 2021;4(4):e215708. https://doi.org/10.1001/jamanetworkopen.2021.5708.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in EpidemiologyA proposal for reporting. JAMA. 2000;283(15):2008–12. https://doi.org/10.1001/jama.283.15.2008.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ (Clinical research ed). 2016;355:i4919. https://doi.org/10.1136/bmj.i4919.
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6. https://doi.org/10.1016/j.jclinepi.2010.07.015.
IntHout J, Ioannidis JP, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016;6(7):e010247. https://doi.org/10.1136/bmjopen-2015-010247.
Brown HL, Britton KA, Mahaffey D, Brizendine E, Hiett AK, Turnquest MA. Methadone maintenance in pregnancy: a reappraisal. Am J Obstet Gynecol. 1998;179(2):459–63. https://doi.org/10.1016/S0002-9378(98)70379-5.
Ellwood DA, Sutherland P, Kent C, O'Connor M. Maternal narcotic addiction: pregnancy outcome in patients managed by a specialized drug-dependency antenatal clinic. Aust N Z J Obstet Gynaecol. 1987;27(2):92–8. https://doi.org/10.1111/j.1479-828x.1987.tb00952.x.
Fishman B, Daniel S, Koren G, Lunenfeld E, Levy A. Pregnancy outcome following opioid exposure: a cohort study. PLoS One. 2019;14(7):e0219061. https://doi.org/10.1371/journal.pone.0219061.
Greig E, Ash A, Douiri A. Maternal and neonatal outcomes following methadone substitution during pregnancy. Arch Gynecol Obstet. 2012;286(4):843–51. https://doi.org/10.1007/s00404-012-2372-9.
Jumah NA, Edwards C, Balfour-Boehm J, Loewen K, Dooley J, Finn LG, et al. Observational study of the safety of buprenorphine+naloxone in pregnancy in a rural and remote population. BMJ Open. 2016;6(10). https://doi.org/10.1136/bmjopen-2016-011774.
Källén B, Borg N, Reis M. The use of central nervous system active drugs during pregnancy. Pharmaceuticals (Basel). 2013;6(10):1221–86. https://doi.org/10.3390/ph6101221.
Källén B, Reis M. Use of tramadol in early pregnancy and congenital malformation risk. Reprod Toxicol. 2015;58:246–51. https://doi.org/10.1016/j.reprotox.2015.10.007.
Nørgaard M, Nielsson MS, Heide-Jørgensen U. Birth and neonatal outcomes following opioid use in pregnancy: a danish population-based study. Subst Abuse. 2015;9:5–11. https://doi.org/10.4137/SaRt.S23547.
Saleh Gargari S, Fallahian M, Haghighi L, Hosseinnezhad-Yazdi M, Dashti E, Dolan K. Maternal and neonatal complications of substance abuse in Iranian pregnant women. Acta Med Iran. 2012;50(6):411–6.
Stimmel B, Adamsons K. Narcotic dependency in pregnancy. Methadone maintenance compared to use of street drugs. Jama. 1976;235(11):1121–4. https://doi.org/10.1001/jama.235.11.1121.
Vucinovic M, Roje D, Vucinovic Z, Capkun V, Bucat M, Banovic I. Maternal and neonatal effects of substance abuse during pregnancy: our ten-year experience. Yonsei Med J. 2008;49(5):705–13. https://doi.org/10.3349/ymj.2008.49.5.705.
Wilson GS, Desmond MM, Wait RB. Follow-up of methadone-treated and untreated narcotic-dependent women and their infants: health, developmental, and social implications. J Pediatr. 1981;98(5):716–22. https://doi.org/10.1016/s0022-3476(81)80830-x.
Ostrea EM, Chavez CJ. Perinatal problems (excluding neonatal withdrawal) in maternal drug addiction: a study of 830 cases. J Pediatr. 1979;94(2):292–5. https://doi.org/10.1016/s0022-3476(79)80847-1.
Corder G, Castro DC, Bruchas MR, Scherrer G. Endogenous and exogenous opioids in pain. Annu Rev Neurosci. 2018;41:453–73. https://doi.org/10.1146/annurev-neuro-080317-061522.
Ke AB, Nallani SC, Zhao P, Rostami-Hodjegan A, Isoherranen N, Unadkat JD. A physiologically based pharmacokinetic model to predict disposition of CYP2D6 and CYP1A2 metabolized drugs in pregnant women. Drug Metab Dispos. 2013;41(4):801–13. https://doi.org/10.1124/dmd.112.050161.
Ke AB, Nallani SC, Zhao P, Rostami-Hodjegan A, Unadkat JD. Expansion of a PBPK model to predict disposition in pregnant women of drugs cleared via multiple CYP enzymes, including CYP2B6, CYP2C9 and CYP2C19. Br J Clin Pharmacol. 2014;77(3):554–70. https://doi.org/10.1111/bcp.12207.
Madadi P, Avard D, Koren G. Pharmacogenetics of opioids for the treatment of acute maternal pain during pregnancy and lactation. Curr Drug Metab. 2012;13(6):721–7. https://doi.org/10.2174/138920012800840392.
Price HR, Collier AC. Analgesics in pregnancy: an update on use, safety and pharmacokinetic changes in drug disposition. Curr Pharm Des. 2017;23(40):6098–114. https://doi.org/10.2174/1381612823666170825123754.
Wood M, Wood AJ. Changes in plasma drug binding and alpha 1-acid glycoprotein in mother and newborn infant. Clin Pharmacol Ther. 1981;29(4):522–6. https://doi.org/10.1038/clpt.1981.73.
Dean M, Stock B, Patterson RJ, Levy G. Serum protein binding of drugs during and after pregnancy in humans. Clin Pharmacol Ther. 1980;28(2):253–61. https://doi.org/10.1038/clpt.1980.158.
Zagon IS, Wu Y, McLaughlin PJ. Opioid growth factor and organ development in rat and human embryos. Brain Res. 1999;839(2):313–22. https://doi.org/10.1016/s0006-8993(99)01753-9.
Frieden TR, Houry D. Reducing the Risks of Relief--The CDC Opioid-Prescribing Guideline. N Engl J Med. 2016;374(16):1501–4. https://doi.org/10.1056/NEJMp1515917.
Tran TH, Griffin BL, Stone RH, Vest KM, Todd TJ. Methadone, buprenorphine, and naltrexone for the treatment of opioid use disorder in pregnant women. Pharmacotherapy. 2017;37(7):824–39. https://doi.org/10.1002/phar.1958.
Acknowledgements
None.
Funding
This study is supported by Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (code: ZYLX202119).
Author information
Authors and Affiliations
Contributions
X. W conceived the research idea and designed the search strategy. X. W and Y. W performed the search, study screening, data extraction and data analysis. B. T performed statistical analysis. X. W and Y. W developed figures and wrote the manuscript with revisions based on B. T and X. F’s comments. X. F was the arbiter for unresolved conflicts and responsible for supervision. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1 Table S1.
Search terms. Table S2. Summary of risk of bias assessment using ROBINS-I tool. Fig. S1. Eggers’s test of studies examining the association between opioids exposure and the risk of congenital malformations. Fig. S2. Forest plot of association between opioid exposure and major congenital malformation. Fig. S3. Forest plot of association between opioid exposure and central nervous system malformation. Fig. S4. Forest plot of association between opioid exposure and limb malformation. Fig. S5. Forest plot of assoxiation between opioid exposure and cardiovascular malformation. Fig. S6. Forest plot of association between opioid exposure and gastrointestinal malformation. Fig. S7. Forest plot of association between opioid exposure and ear, face, and neck malformation. Fig. S8. Forest plot of association between opioid exposure and respiratory malformation. Fig. S9. Forest plot of association between opioid exposure and musculoskeletal malformation. Fig. S10. Forest plot of association between opioid exposure and urogenital malformation. Fig. S11. Forest plot of association between opioid exposure and orofacial malformation. Fig. S12. Forest plot of association between opioid exposure and neural tube defects. Fig. S13. Forest plot of association between opioid exposure and gastroschisis. Fig. S14. Forest plot of association between opioid exposure and clubfoot. Fig. S15. Meta-regression according to the year of publication. Fig. S16. Forest plot of subgroup analysis of exposed period. Fig. S17. Forest plot of subgroup analysis of indication. Fig. S18: Forest plot of subgroup analysis of adjusted for confounders. Fig. S19. Forest plot of subgroup analysis of risk of bias assessment.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, X., Wang, Y., Tang, B. et al. Opioid exposure during pregnancy and the risk of congenital malformation: a meta-analysis of cohort studies. BMC Pregnancy Childbirth 22, 401 (2022). https://doi.org/10.1186/s12884-022-04733-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-04733-9