Abstract
Background
To determine whether severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2, the cause of COVID-19 disease) exposure in pregnancy, compared to non-exposure, is associated with infection-related obstetric morbidity.
Methods
We conducted a multicentre prospective study in pregnancy based on a universal antenatal screening program for SARS-CoV-2 infection. Throughout Spain 45 hospitals tested all women at admission on delivery ward using polymerase-chain-reaction (PCR) for COVID-19 since late March 2020. The cohort of positive mothers and the concurrent sample of negative mothers was followed up until 6-weeks post-partum. Multivariable logistic regression analysis, adjusting for known confounding variables, determined the adjusted odds ratio (aOR) with 95% confidence intervals (95% CI) of the association of SARS-CoV-2 infection and obstetric outcomes. Main outcome measures: Preterm delivery (primary), premature rupture of membranes and neonatal intensive care unit admissions.
Results
Among 1009 screened pregnancies, 246 were SARS-CoV-2 positive. Compared to negative mothers (763 cases), SARS-CoV-2 infection increased the odds of preterm birth (34 vs 51, 13.8% vs 6.7%, aOR 2.12, 95% CI 1.32–3.36, p = 0.002); iatrogenic preterm delivery was more frequent in infected women (4.9% vs 1.3%, p = 0.001), while the occurrence of spontaneous preterm deliveries was statistically similar (6.1% vs 4.7%). An increased risk of premature rupture of membranes at term (39 vs 75, 15.8% vs 9.8%, aOR 1.70, 95% CI 1.11–2.57, p = 0.013) and neonatal intensive care unit admissions (23 vs 18, 9.3% vs 2.4%, aOR 4.62, 95% CI 2.43–8.94, p < 0.001) was also observed in positive mothers.
Conclusion
This prospective multicentre study demonstrated that pregnant women infected with SARS-CoV-2 have more infection-related obstetric morbidity. This hypothesis merits evaluation of a causal association in further research.
Similar content being viewed by others
Key message
This prospective multicentre study revealed that pregnant women infected with SARS-CoV-2 have more infection-related obstetric morbidity (Preterm birth, premature rupture of membranes at term and neonatal intensive care unit admissions).
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), identified in December 2019, is the cause of the illness named COVID-19 [1, 2]. With more than 249,000 confirmed cases and more than 28,700 deaths by 20th August 2020, Spain remains one of the European countries most severely affected by the ongoing COVID-19 pandemic [3, 4]. Spain also established a universal screening programme for pregnancies in light of the higher disease exposure. We observed that obstetric intervention may influence the clinical course of the disease [5,6,7]. The cohort of pregnant women assembled through this programme lends itself to evaluation of concerns about obstetric outcomes.
The majority of non-pregnant patients with SARS-CoV-2 infection have uncomplicated or mild illness (81%), some will develop severe illness associated with cytokine-mediated inflammation phenomena such as IL-6 associated with the need for mechanical ventilation [8]. Initial studies have reported similar involvement in pregnant patients [9]. The inflammatory mediators associated SARS-CoV-2 infection have previously been related to poor perinatal outcomes [10, 11]. This background naturally leads to the question as to whether SARS-CoV-2 infection affects pregnancy adversely.
We hypothesised that SARS-CoV-2 infection in pregnancy, compared to non-infection, would increase infection-related obstetric morbidity including preterm birth and premature rupture of membranes which in turn would increase the admissions of the neonate to intensive care units. We tested the hypothesis in a multivariable logistic regression analysis, adjusting for the effect of known confounding variables.
Methods
This was a multicentre prospective study of consecutive cases of SARS-CoV-2 infection in a pregnancy cohort registered by the Spanish Obstetric Emergency group in 45 hospitals [12]. The registry’s objective updates were approved by the coordinating hospital’s Medical Ethics Committee on March 23rd, 2020 (reference number: PI 55/20); each collaborating center subsequently obtained protocol approval locally. The registry protocol is available in ClinicalTrials.gov, identifier: NCT04558996, and in Additional File 1. A complete list of the centers contributing to the study is provided in Supplementary Table 1, Additional File 2. Upon recruitment, given the contagiousness of the disease and the lack of personal protection equipment, mothers consented by either signing a document (Additional File 3), when possible, or by giving permission verbally which was recorded in the patient’s chart. A specific database was designed for recording information regarding SARS-CoV-2 infection in pregnancy. Data were entered by the lead researcher for each center after delivery, with a follow-up of 6-weeks postpartum in order to detect complications or symptomatic infections. We developed an analysis plan using recommended contemporaneous methods and followed existing guidelines for reporting our results (Supplementary Table 2, Additional File 2) [13].
Infected group
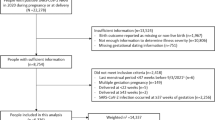
We included infected obstetric patients detected by routine screening for SARS-CoV-2 infection, which was carried out in every pregnant at admission on delivery ward during the study period from the 23rd of March to the 31st of May 2020 (Fig. 1). SARS-CoV-2 infection was diagnosed by positive double-sampling polymerase-chain-reaction (PCR) from nasopharyngeal swabs. All identified cases were included in the study, irrespective of clinical signs and symptoms or the result of another serological test. In those cases, with a clinical presentation of SARS-CoV-2 infection, it was classified following the WHO division for adults: mild symptoms, mild-moderate pneumonia, severe pneumonia and septic shock [14].
Non-infected comparison group
Non-infected patients were those defined by a negative PCR in the routine screening carried out in every pregnant at admission on delivery ward. Among these PCR negative mothers, each center identified 2–3 pregnancies delivered immediately before and/or after delivery of each SARS-CoV-2 infected mother (Fig. 1). This method of identifying mothers not exposed to SARS-CoV-2 infection was deployed to adjusted for center conditions at the time of delivery and decreased the risk of bias.
Study information
Hospitals collected the encoded information in two separate phases: during the enrolment period that occurred at the time of the SARS-CoV-2 test during pregnancy and within 6 weeks after birth. Information regarding the demographic characteristics of each pregnant woman, comorbidities and current obstetric history was extracted from the clinical history and from the interview with the patient; subsequently, age and race were categorized following the classification used by the CDC [15]. Definitions of obstetric conditions followed international criteria [16,17,18]. Perinatal events, medical and obstetric complications were recorded. Preterm deliveries were classified as spontaneous onset (including those resulting from a PPROM), induced labour/C-section due to PPROM and iatrogenic (not associated with PPROM). Patients were followed until six weeks postpartum. Neonatal events were recorded until 14 days postpartum. Recorded variables are listed in Supplementary Table 1, Additional File 1. A total of 33 dropout cases were recorded from the beginning of the registry; the reasons were incomplete information in the registry database, did not participate in the six-week postpartum follow-up and/or voluntary withdrawal of the patient.
Data analysis
We estimated that a sample size of 246 SARS-CoV-2 positive pregnancies with a ratio 1:3 of negative pregnancies would detect a 6% difference in proportions between groups with a power of 80% at a significance level of 5%, assuming a 7% event rate of preterm deliveries in the non-infected group [19]. This level of event rate also permitted us to build logistic regression models without overfitting using the 10:1 event per variable rule.
For the descriptive analysis of the data, absolute and relative frequencies were used in the case of categorical variables and means and ranges in the case of quantitative variables. The possible association of both the characteristics of the patients and the outcomes collected with SARS-CoV-2 infection was analysed using the Pearson’s Chi-square test or Fisher’s exact test and the Mann-Whitney U test (after checking the absence of normality of the data using the Kolmogorov-Smirnov test). Statistical tests were two-sided and were performed with SPSS V.20 (IBM Inc., Chicago, Il, USA); statistically significant associations were considered to exist when the p value was less than 0.05.
For computing measures of association of the outcomes of interest that were statistically significant in the univariate analysis (and with enough number of events) with SARS-CoV-2 infection, the influence of known and suspected measured confounding factors was controlled for multivariable logistic regression modelling in order to derive adjusted odds ratios (aOR) with 95% confidence intervals (95% CI). Models were built for each outcome separately, incorporating a range of independent variables appropriate for the adjustment of the association between SARS-CoV-2 infection and that outcome. The selection process for variables was driven by causal knowledge for the adjustment of confounding, based on previous findings and clinical constraints [11, 14,15,16,17,18]. Besides SARS-CoV-2 positivity, the preterm delivery model included Ethnicity [categorized as white European, Latin American and other ethnic groups (black non-Hispanic, Asian non-Hispanic and Arab)], multiple pregnancy, in vitro fertilization, gestational hypertensive disorders (moderate or severe preeclampsia and HELLP), miscarriage risk and clinical and ultrasound prematurity screening; the spontaneous preterm delivery model included ethnicity (categorized as above), multiple pregnancy, miscarriage risk and clinical and ultrasound prematurity screening; the premature rupture of membranes at term (PROM) model included multiple pregnancy, miscarriage risk, cough, obesity (BMI > 30 kg/m2) and smoking [categorized as smokers (actual and ex-smokers) and non-smokers]; the preterm premature rupture of membranes (PPROM) model included multiple pregnancy and miscarriage risk; and the neonate intensive care unit (NICU) admission model included multiple pregnancy, gestational hypertensive disorders and clinical and ultrasound prematurity screening as independent variables.
A complete list of the final set of covariates is provided with each model in the results section. The modelling was conducted after excluding cases with missing data. A prematurity screening program was not established in all participating hospitals and that variable had 11.3% of missing values, whereas the remaining variables had less than 1.2% of missing values. Regression analyses were carried out using lme4 package in R, version 3.4 (RCoreTeam, 2017) [20].
Results
One thousand and nine (1009) patients were analysed. 246 pregnant women in the infected group and 763 in the non-infected group. Of the 246 positive cases, 88.6% (n = 218) were asymptomatic at delivery while 11.4% (n = 28) were symptomatic. Of the asymptomatic women, 44 (20.2%) had previously presented symptoms and 174 (79.8%) were totally asymptomatic. On the other hand, of the pregnant women who showed symptoms at the time of delivery, 24 (85.7%) cases corresponded to mild symptoms (being the most prevalent, cough 33.3%, and anosmia 20.8%, followed by fatigue/discomfort, fever and dyspnoea), 2 (7.1%) pregnant women presented mild-moderate pneumonia and another 2 (7.1%) pregnant women had developed severe pneumonia. No case of septic shock or maternal death was recorded in pregnant women with SARS-CoV-2 infection included in the study.
The demographic characteristics, comorbidities and current obstetric history of the positive cohort and the subsample of negative patients concurrent in time deliveries (246 vs 763) are shown in Table 1. The only variable in which statistically significant differences were observed was ethnicity, being significantly higher the proportion of Latin American women in the infected cohort compared to the non-infected group (p < 0.001; OR = 2.85, 95% CI: 1.96–4.15), while the opposite was true for White European patients (p < 0.001, OR = 0.49, 95% CI: 0.36–0.67).
When the possible association of perinatal and neonatal events with SARS-CoV-2 infection was analysed by univariate and multivariable logistic regression using complete case analyses (without imputation for missing values) (Tables 2 and 3), twice as many deliveries with less than 37 weeks of gestation were observed in the infected cohort (13.8%) than in the negative group (6.7%) (p = 0.002), with an adjusted OR equal to 2.12 (95% CI: 1.32–3.36), although no statistically significant differences had been observed in the clinical and ultrasound screening for prematurity between both groups (p = 0.461) (Table 1). Among preterm deliveries, iatrogenic preterm delivery (not associated with PPROM) was practically four times more frequent in infected by SARS-CoV-2 pregnant women than in the non-infected group (4.9% vs 1.3%, p = 0.001), while the occurrence of spontaneous preterm deliveries was not affected by SARS-CoV-2 infection status (p = 0.760, adjusted OR = 1.10, 95% CI: 0.57–2.06) (Table 3). In the positive group, symptomatic SARS-CoV-2 infection were present in 5 (42%) out of 12 iatrogenic preterm deliveries, while this was the case in only 3 (20%) out of 15 spontaneous preterm deliveries.
Similarly, a higher risk of premature rupture of membranes, at term (PROM) and preterm (PPROM), was observed in the infected group (p = 0.009 and p = 0.031, respectively) (Table 2). In the case of PROM, the finding of multivariable logistic regression was consistent with the above result, with a 70% increase of occurrence in infected patients compared to non-infected (adjusted OR = 1.70, 95% CI: 1.11–2.57) (Table 3).
No maternal deaths were recorded in the 1009 patients in the study, but there were intrauterine fetal deaths, with the proportion of these being considerably higher in patients in the positive group than in the subsample of negative patients (1.2% vs 0.1%, p = 0.047) (Table 2).
When the information regarding the neonate was analysed (Tables 2 and 3), those born to mothers with SARS-CoV-2 infection were admitted to the NICU significantly more often than those born to non-infected mothers (p < 0.001, adjusted OR = 4.62, 95% CI: 2.43–8.94). Prematurity and respiratory distress were the main causes of NICU admission (Table 2), while none of these admissions were due to SARS-CoV-2 infection in newborns. In 189 (76.8%) of the SARS-CoV-2 infection cases, a PCR analysis was performed on nasopharyngeal and/or oropharyngeal samples of the newborns; 147 were performed during the first 12 h of life, three of which were positive, and another 42 were performed until 48 h of life, all resulting negative. The 3-initial positive newborns were retested at 48 h, with final negative results.
Discussion
Main findings
Through a multicentre prospective study, we analysed the relationship between SARS-CoV-2 exposure and infection-related obstetric outcomes. We found, using multivariable models adjusting for confounding factors, that the pregnant women with SARS-CoV-2 infection had more preterm births, premature rupture of membranes at term and NICU admissions compared to the pregnant woman who were not exposed.
Strengths and weaknesses
Ours is a study with a group of positive mothers carried out during a difficult pandemic situation whose continuing objective is to investigate the influence of SARS-CoV-2 infection on delivery and the puerperium. We wish to obtain the best epidemiological information in the shortest possible time with a follow-up 6 weeks after delivery. Patient recruitment continues in our registry and this is an initial analysis. Our work is one of the first multicentre prospective studies to analyse the relationship between SARS-CoV-2 infection and prematurity. The relationship that we establish with premature rupture of membranes raises future lines of research.
The most important limitation of our work is the inability to compare infected patients with uninfected patients from the beginning due to the lack of diagnostic tests and the health sector crisis that occurred. When a screening system was established, there were not as many patients with severe symptoms and the number of events reduced the ability to analyse some effects of symptomatic SARS-CoV-2 infection. Many cases of obstetric severe preeclampsia, haemorrhage, pulmonary thromboembolism and abruptio occurred mainly in the months of March and April before many centres started screening programmes and the cohort study began, so no distinction has been made between the different clinical presentations of the disease. We could not do a multivariable analysis of such conditions.
No serological test was performed on patients who had a negative PCR test, either because the tests were not available at the time of recruitment or because they did not have a proven sensitivity. In some cases, these patients may have already had the disease. No serology was performed during those months on asymptomatic PCR-positive patients to confirm their disease and immune response. Our study is best understood if the results are interpreted under this premise and therefore our group continues to recruit patients to seek more associations, explanations and causations. This work reflects the conditions of patients with SARS-CoV-2 infection at the time of delivery and the puerperium. It has not analysed the course of the disease during pregnancy, nor has it recorded late abortions, vertical transmission, or causes of intrauterine mortality.
In addition, we acknowledge as a limitation the absence of the complete cohort screened from analysis. In this sense our study has a hybrid design. The PCR negative comparison group was a subsample of the screen negative cohort from all 45 hospitals that had PCR positive mothers. The concurrent method applied for selection of non-infected cohort allowed for a comparison unaffected by difference in time of exposure and outcome assessment.
Comparison with other studies
The symptoms of the patients in our study do not differ from those already published [21, 22]. Although most did not have any symptoms, we did find an increase in obstetric pathology in these patients, which in our opinion indicates that in the pregnant woman with asymptomatic SARS-CoV-2 infection there is a specific obstetric pathology that needs to be recognised. In the same way as other authors, we have also found a demographic factor, such as ethnicity, that increases the possibility that a patient has SARS-CoV-2 infection [15, 23]. It is necessary to know if there is a component of genetic susceptibility or if there are social factors that explain this association. There are already studies that relate this situation to less access to healthcare resources or the possibility of confinement which complies with healthcare measures [24].
Patients with SARS-CoV-2 infection are at increased risk of preterm delivery associated with increased iatrogenic preterm delivery. The explanation for this risk is the need to end the pregnancy due to maternal diseases, such as severe pre-eclampsia and pneumonia, which are more frequent in these patients and lead to more labour inductions. A unique and novel finding in our study is the association between premature rupture of membranes at term and SARS-CoV-2 infection. PROM may result in immediate risks and subsequent problems including maternal or neonatal infection [25]. One of the possible explanations we found for this association is the activation of a series of mediators and biochemical pathways of inflammation in the premature rupture of membranes and premature delivery that are also found in SARS-CoV-2 infection, such as macrophages or IL-6 [26]. The studies demonstrating the influence of IL-6 on preterm delivery are a strong basis for studying this association [27]. Cytokines are vital in regulating immunological and inflammatory responses. Among them, IL-6 is of major importance because there is evidence that circulating IL-6 levels are closely linked to the severity of the SARS-CoV-2 infection [28]. There are already treatments that are indicated based on these findings [29].
We observed a significant increase in the stillbirth rate in the univariate analysis alone. The role of inflammation mediators in these deaths could be the subject of a line of research because it is known that women without SARS-CoV-2 infection who have a pregnancy loss, have significantly higher amniotic fluid IL-6 concentration levels than those with a normal outcome [30]. We found no differences in mortality or early or late neonatal morbidity related to SARS-CoV-2 exposure in our study, unlike reports from other series [31, 32]. .There is a higher risk that the children of SARS-CoV-2 infection mothers enter the NICU, with prematurity being one of the determining factors. All newborns were followed for at least 14 days by the different neonatology units of the participating hospitals, without any case of neonatal SARS-CoV-2 infection being detected in that period.
To date, there has been indirect evidence on placental involvement which would explain our findings [33, 34]. Our results derived using multivariable analyses confirm those of the cases series published at the beginning of the pandemic that described preterm deliveries and premature rupture of the membranes [21, 31, 35].
Conclusion
Pregnant SARS-CoV-2 infection patients are a population at risk of suffering preterm deliveries, and the disease has an impact on NICU admissions. Premature rupture of membranes at term and preterm are more frequent in patients with SARS-CoV-2 infection.
Availability of data and materials
The data that support the findings of this study are available from the Institute of Health-Carlos III and the Spanish Ministry of Health (registry protocol in ClinicalTrials.gov: NCT04558996) and has been previously published by Encinas Pardilla et al. [12]. Data are however available from the authors upon reasonable request and with permission of the Institute of Health-Carlos III and the Spanish Ministry of Health.
Abbreviations
- OR:
-
Odds ratio
- aOR:
-
Adjusted odds ratio
- NICU:
-
Neonate intensive care unit
- PCR:
-
Polymerase-chain-reaction
- PROM:
-
Premature rupture of membranes at term
- PPROM:
-
Premature rupture of membranes at term
References
Zhu N, Zhang D, Wang W, Xingwang L, Bo Y, Jingdong S, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–33. https://doi.org/10.1056/NEJMoa2001017.
Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. 2020;222(5):415–26. https://doi.org/10.1016/j.ajog.2020.02.017 Epub 2020.
Panel Covid-19 en España [Internet]. Madrid: Centro Nacional de Epidemiología/Instituto de Salud Carlos III; 2001 [updated 2020 Jul 17; cited 2020 Jul 20]. Available from: https://cnecovid.isciii.es/covid19/
COVID-19 situation update worldwide. [Internet] Stockholm: European Centre for Disease Prevention and Control; 2005 [updated 2020 Jul 18; cited 2020 Jul 20]. Available from: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases.
Martínez-Perez O, Vouga M, Cruz Melguizo S, et al. Association between mode of delivery among pregnant women with COVID-19 and maternal and neonatal outcomes in Spain. JAMA. Epub June 08, 2020. 2020. https://doi.org/10.1001/jama.2020.10125.
Silveira Campos L, Peixoto Caldas JM. Increasing maternal mortality associated with COVID-19 and shortage of intensive care is a serious concern in low-resource settings. Acta Obstet Gynecol Scand. 2020;99(10):1421. https://doi.org/10.1111/aogs.13975.
Westgren M, Pettersson K, Hagberg H, Acharya G. Severe maternal morbidity and mortality associated with COVID-19: the risk should not be downplayed. Acta Obstet Gynecol Scand. 2020;99(7):815–6. https://doi.org/10.1111/aogs.13900.
WHO. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Geneva; 16-24 February 2020. Avalaible from https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
Khalil A, von Dadelszen P, Draycott T, Ugwumadu A, O’Brien P, Magee L. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA. Epub July 10, 2020. 2020. https://doi.org/10.1001/jama.2020.12746.
Romero R, Munoz H, Gomez R, Sherer DM, Ghezzi F, Gibbs RS, et al. Two thirds of spontaneous abortion/fetal deaths after genetic amniocentesis are the result of a pre-existing sub-clinical inflammatory process of the amniotic cavity. Am J Obstet Gynecol. 1995;172:S261.
Zaigham M, Andersson O. Maternal and perinatal outcomes with COVID-19: a systematic review of 108 pregnancies. Acta Obstet Gynecol Scand. 2020;99(7):823–9. https://doi.org/10.1111/aogs.13867.
Encinas Pardilla MB, Caño Aguilar Á, Marcos Puig B, Sanz Lorenzana A, Rodríguez de la Torre I, Hernando López de la Manzanara P, Fernández Bernardo A, Martínez Pérez O. Registro español de cribado de Covid-19 en gestantes asintomáticas. Rev Esp Salud Pública. 2020; 94. In press.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9. https://doi.org/10.1016/j.ijsu.2014.07.013.
WHO. Clinical Management of COVID-19. Interim Guidance 27 May 2020. Geneva; 2020. WHO/2019-nCoV/clinical/2020.5. Available from: https://www.who.int/publications/i/item/clinical-management-of-covid-19
Ellington S, Strid P, Tong Van T, Woodworth K, Galang RG, Zambrano LD et al. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status. MMWR Morb Mortal Wkly Rep 2020; 69(25): 769–775. Available from https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6925-H.pdf. https://doi.org/10.15585/mmwr.mm6925a1
Prelabor Rupture of Membranes. ACOG practice bulletin summary, number 217. Obstet Gynecol. 2020;135(3):e80–97. https://doi.org/10.1097/AOG.0000000000003700.
Thomson AJ, on behalf of the Royal College of Obstetricians and Gynaecologists. Care of Women Presenting with suspected preterm Prelabour rupture of membranes from 24+ 0 to 36+ 6 weeks of gestation. BJOG. 2019;126(9):e152–66. Available from https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg73/. https://doi.org/10.1111/1471-0528.15803.
Brown MA, Magee LA, Kenny LC, Karumanchi AS, McCarthy FP, Saito S, et al. Hypertensive Disorders of Pregnancy, ISSHP Classification, Diagnosis, and Management Recommendations for International Practice. Hypertension. 2018;72(1):24–43. https://doi.org/10.1161/HYPERTENSIONAHA.117.10803.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75–84. https://doi.org/10.1016/S0140-6736(08)60074-4.
Bates D, Maechler M, Bolker B, Walker S. Fitting Linear Mixed-Effects Models Using lme4. J Stat Software. 2015;67(1):1–48. https://doi.org/10.18637/jss.v067.i01.
Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 395(10226):809–15. https://doi.org/10.1016/S0140-6736(20)30360-3.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City. JAMA. 2020;323(20):2052–9. https://doi.org/10.1001/jama.2020.6775.
Knight M, Bunch K, Vousden N, Morris E, Simpson N, Gale C, et al. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population-based cohort study Obstetric Surveillance System SARS-CoV. BMJ. 2020;369:m2107. https://doi.org/10.1136/bmj.m2107.
WM, Napoles A, Pérez-Stable E. COVID-19 and Racial/Ethnic Disparities. JAMA. 2020;323(24):2466–7. https://doi.org/10.1001/jama.2020.8598.
Alexander JM, Cox SM. Clinical course of premature rupture of the membranes. Semin Perinatol. 1996;20(5):369–74. https://doi.org/10.1016/s0146-0005(96)80003-6 PMID: 8912990.
Lannon SMR, Vanderhoeven JP, Eschenbach DA, Gravett MG, Adams Waldorf KA. Synergy and interactions among biological pathways leading to preterm premature rupture of membranes. Reprod.Sci. 2014;21(10):1215–27. https://doi.org/10.1177/1933719114534535.
Romero R, Yoon BH, Kenney JS, Gomez R, Allison AC, Sehgal PB. Amniotic fluid interleukin-6 determinations are of diagnostic and prognostic value in preterm labor. Am J Reprod Immunol. 1993;30(2–3):167–83. https://doi.org/10.1111/j.1600-0897.1993.tb00618.x PMID: 8311926.
Aziz M, Fatima R, Assaly R. Elevated interleukin-6 and severe COVID-19: A meta-analysis. J Med Virol. 2020;28. https://doi.org/10.1002/jmv.25948 Epub ahead of print. PMID: 32343429; PMCID: PMC7267383.
Naqvi M, Zakowski P, Glucksman L, Smithson S, Burwick RM. Tocilizumab and Remdesivir in a pregnant patient with coronavirus disease 2019 (COVID-19). Obstet Gynecol. 2020;136(5):1025–9. https://doi.org/10.1097/AOG.0000000000004050. PMID: 32618794.
Wenstrom KD, Andrews WW, Tamura T, DuBard MB, Johnston KE, Hemstreet GP. Elevated amniotic fluid interleukin-6 levels at genetic amniocentesis predict subsequent pregnancy loss. Am J Obstet Gynecol. 1996;175(4):830–3. https://doi.org/10.1016/S0002-9378(96)80007-X.
Zhang L, Jiang Y, Wei M, Cheng BH, Zhou XC, Li J, et al. Analysis of the pregnancy outcomes in pregnant women with COVID-19 in Hubei Province. Zhonghua Fu Chan Ke Za Zhi. 2020;55(3):166–71. https://doi.org/10.3760/cma.j.cn112141-20200218-00111 PMID: 32145714. Chinese.
Chen Y, Peng H, Wang L, Zhao Y, Zeng L, Gao H, et al. Infants born to mothers with a new coronavirus (COVID-19). Front Pediatr. 2020;8:1–5. https://doi.org/10.3389/fped.2020.00104.
Prochaska E, Minyoung J, Burd I. COVID-19 in pregnancy: Placental and neonatal involvement. Am J Reprod Immunol. 2020;17:e13306. https://doi.org/10.1111/aji.13306.
Shanes ED, Mithal LB, Otero S, Azad HA, Miller, Goldstein JA. Placental Pathology in COVID-19. Am J Clin Pathol. 2020;154:23–32. https://doi.org/10.1093/ajcp/aqaa089.
Zhu H, Wang L, Fang C, et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. 2020;9(1). https://doi.org/10.21037/tp.2020.02.06.
Acknowledgements
Authors thank José Montes (Effice Research) for his support with the statistics, Professor Khalid Khan (Department of Preventive Medicine and Public Health, University of Granada) and Dr. Mar Gil Mina (Hospital Universitario de Torrejón) for their scientific advice, and Meisys for their support with the manuscript writing.
Funding
This project was supported by public funds obtained in competitive calls: Grant COV20/00021 from the Institute of Health - Carlos III and co-financed with Fondo Europeo de Desarrollo Regional (FEDER) funds. The funding body had no role in the study design, collection, analysis or interpretation of data, nor on manuscript writing.
Author information
Authors and Affiliations
Consortia
Contributions
OMP contributed with the design and coordination of the study, interpretation of results and writing of the manuscript; PPR and JASB contributed with the interpretation of results and writing of the manuscript; MMH, MBEP, NPP, MRVH, AVY, ONV, PGBF, LFA, CMOL, AMV, BMA, MSA, LFR, CMD, MJJF, MAA-M, CCP, OAM, CLH, JCWA, RBV, MMB, CAC, ASM, LPA, RAS, MLR, MCBL, MRMC, OVR, EMA, MJNV, CFF, ATN, AMCG, CBL, SSP, IGA, JAG, MTG, APP, ROS, MPGM, MCC, EFP collected and curated the data, and did the critical revision of the manuscript; ACA centralized and cleansed the screening data and MLCC did the statistical analysis of data and writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures were approved by the Drug Research and Clinical Research Ethics Committee of the Puerta de Hierro University Hospital (Madrid, Spain) on 23rd March 2020 (protocol registration number, 55/20); each collaborating center subsequently obtained protocol approval locally (Ethics Committees of the participant hospitals, listed in the Supplementary Table 1 of the Additional File 2). Upon recruitment, mothers consented to participate in the study by either signing a document, when possible, or by giving permission verbally which was recorded in the patient’s chart in the electronic clinical recording system. The possibility of verbal consent was approved by the Ethics Committees during the first three months of the pandemic, given the contagiousness of the disease and the lack of personal protection equipment; afterwards, written consent (using the Patient Consent Form, Additional File 3) was collected from every patient who had previously given permission verbally.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
Registry Protocol. Table S1. List of variables in the Registry (Appendix 5 of Registry Protocol).
Additional file 2: Table S1
. List of hospitals included in the study (n = 45); and Table S2. STROBE Statement—checklist of items that should be included in reports of observational studies.
Additional file 3.
Patient Consent Form.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Martinez-Perez, O., Prats Rodriguez, P., Muner Hernandez, M. et al. The association between SARS-CoV-2 infection and preterm delivery: a prospective study with a multivariable analysis. BMC Pregnancy Childbirth 21, 273 (2021). https://doi.org/10.1186/s12884-021-03742-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-021-03742-4